Abstract
We compared differential reinforcement plus escape extinction to noncontingent reinforcement plus escape extinction to treat food selectivity exhibited by a young child with autism. The interventions were equally effective for increasing bite acceptance and decreasing problem behaviors. However, a social validity measure suggested that noncontingent reinforcement was preferred by the child's caregiver.
Key words: autism, differential reinforcement, escape extinction, food selectivity, noncontingent reinforcement
Escape extinction (EE) may be a necessary component for treatments aimed at increasing food acceptance and decreasing mealtime-related problem behavior (Piazza, Patel, Gulotta, Sevin, & Layer, 2003). Piazza et al. showed that, when used alone, differential reinforcement was ineffective at increasing bite acceptance and mouth clean (a product measure of swallowing). Escape extinction was necessary to increase acceptance and mouth clean. Reed et al. (2004) found similar results with noncontingent reinforcement (NCR); that is, food consumption increased only when therapists implemented EE, regardless of whether NCR was present or absent.
Although previous research has shown that EE may be necessary to increase consumption, extinction often produces side effects such as aggression and emotional behavior. The addition of differential reinforcement (Piazza et al., 2003) and NCR (Reed et al., 2004) has decreased problem behavior for some participants. However, no study has compared differential reinforcement with EE to NCR with EE directly to determine which is more effective at increasing acceptance and decreasing problem behavior in children with autism who exhibit food selectivity; this was the purpose of the current study.
METHOD
Participant, Setting, and Materials
Cam was a 3-year-old boy with a diagnosis of autism; he had been referred for food selectivity. He ate several flavors of applesauce and Stage 3 baby food. Trained therapists conducted sessions in a room equipped with a one-way observation window at an autism treatment center. Food, a high chair, and eating utensils were present during all sessions, and toys were available during some conditions. The therapists wore different-colored shirts and used a corresponding colored placemat during the various conditions of the functional analysis and treatment evaluation to promote Cam's discrimination of the different conditions.
Response Measurement and Reliability
Observers scored acceptance, latency to accept, problem behavior, and negative vocalizations using personal digital assistants equipped with data-collection software. We scored the occurrence of acceptance when the therapist deposited the entire bolus of food in the participant's mouth. Observers scored latency to accept by activating a timer when the therapist presented the spoon within 3 cm of the child's lips and deactivating the timer when the therapist deposited the entire bite into the child's mouth; this measure did not include the time it took the therapist to present the spoon and deposit the bite during re-presentation. The frequency of problem behavior was scored when the participant (a) turned his head 45 degrees away from the spoon or (b) hit or blocked the therapist's feeding hand, arm, or spoon while the spoon was within 10 cm of the child's lips. The duration of negative vocalizations was scored when the participant cried or whined for at least 3 s. Acceptance data were converted to a percentage by dividing the number of acceptances by the number of bite presentations (i.e., each time the therapist placed the spoon within 3 cm of the child's lips, not including placement of the spoon at the lips during re-presentation). Data on problem behavior were converted to a rate by dividing the number of occurrences by the amount of time the spoon was at the child's lips (i.e., total duration of spoon within 10 cm of child's lips). Data on negative vocalizations were converted to a percentage by dividing the duration of negative vocalizations by the duration of the session.
A second observer collected data on 40% and 34% of sessions during the functional analysis and treatment evaluation, respectively. To obtain interobserver agreement for acceptance and problem behavior, the smaller frequency was divided by the larger frequency on an interval-by-interval basis and the result was converted to a percentage. For negative vocalizations, the smaller duration was divided by the larger duration on an interval-by-interval basis and the result was converted to a percentage.
During the functional analysis, interobserver agreement for acceptance and negative vocalizations was 100%. Interobserver agreement for problem behavior was 90%. During the treatment evaluation, interobserver agreement was 100% for acceptance, 82% for problem behavior, and 86% for negative vocalizations.
Procedure
We conducted a paired-stimulus preference assessment (Fisher et al., 1992) to identify five highly preferred toys (i.e., those chosen on at least 66% of trials) that were used during the functional analysis and treatment evaluation. Therapists conducted 5 to 10 sessions per day, 2 to 3 days per week. During each session, the therapist presented a half level bolus of food on a toddler spoon once every 30 s (with the exceptions noted below) for 5 min. The order of food presentation within the session was determined randomly. Foods were randomly selected for each session; no two foods were used consecutively across sessions. Presented foods were mashed potatoes, wet-ground carrots, apple sauce, and Stage 2 macaroni and cheese; these foods had been refused previously. The therapist said “good” after acceptance and after mouth clean. The therapist checked for a mouth clean with an empty spoon 30 s after the bite initially entered the child's mouth using a three-step prompting procedure. A verbal prompt to “swallow” was delivered if the participant had food in his mouth at the 30-s mouth check. The therapist repeated the mouth check and prompt to swallow every 30 s until there was no food present in his mouth. The therapist then presented the next bite. If the participant had food in his mouth 5 min after the session began, the therapist did not present additional bites of food, and the session continued until the child had no food in his mouth or until 20 min had elapsed. If the session ended and the child had food in his mouth, the therapist removed the food with an empty spoon. No differential consequences were delivered after vomiting.
Functional analysis
We conducted a pairwise functional analysis in which control and escape conditions were randomly alternated to identify the variables that maintained problem behavior (Bachmeyer et al., 2009). Across both conditions, the spoon with food remained where the therapist initially presented it for 30 s if the child did not accept the bite and was followed by a new bite presentation. No differential consequences were delivered after expulsion. During the control condition, no differential consequences were provided for problem behavior. The participant had access to preferred items identified via the preference assessment and therapist attention throughout the session. During the escape condition, if the participant engaged in problem behavior, the therapist removed the bite for 20 s and presented the next bite after the escape interval had elapsed.
Treatment evaluation
A combination multielement and ABAB reversal design was used to evaluate the effects of differential reinforcement of alternative behavior (i.e., acceptance, DRA) plus EE versus NCR plus EE on acceptance, problem behavior, and negative vocalizations. The therapist used five preferred toys identified via the stimulus preference assessment during treatment. Baseline of the treatment evaluation was identical to the escape condition of the functional analysis. Prior to each DRA or NCR treatment session, we conducted a brief preference assessment with the five toys described above to identify the two toys to be used in that session. During DRA plus EE, the bite remained at the child's lips until the therapist could deposit it into his mouth. The therapist presented 30-s access to the preferred toy and high-quality praise and interaction contingent on acceptance. The next bite was presented after the 30-s reinforcement interval if Cam had a mouth clean. The therapist delivered no differential consequences for problem behavior but blocked it if necessary. Expelled bites were re-presented until the child swallowed or 20 min elapsed. NCR plus EE was identical to the DRA plus EE condition except that the same preferred items and therapist attention were available throughout the entire session. At the conclusion of the study, Cam's mother completed a seven-question social validity questionnaire that had been created for this study. Each question included a 5-point Likert scale. Questions addressed the extent to which Cam's parents would be likely to implement each procedure, the acceptability of each procedure, and preference for each procedure.
RESULTS AND DISCUSSION
Cam exhibited higher rates of problem behavior in the escape condition (M = 30) of the functional analysis (Figure 1, top) than in the control condition (M = 4). He did not accept any bites and did not exhibit any negative vocalizations during the functional analysis (data not shown). The second panel shows that both treatments increased bite acceptance from 0% in the escape condition to 100%. The third panel shows that both treatments decreased problem behavior relative to the escape condition (Ms = 30 and 30.4 per minute during the first and second escape conditions, respectively). Problem behavior decreased to 10.7 and 7 responses per minute during the first and second treatment phases, respectively, of DRA plus EE and to 9.4 and 4.6 responses per minute during the first and second treatment phases, respectively, of NCR plus EE. During both escape conditions, negative vocalizations did not occur and increased in the first treatment phase to 23.2% in DRA plus EE and 32.7% in NCR plus EE and in the second treatment phase to 6.2% in DRA plus EE and 1.7% in NCR plus EE (bottom panel). Bite rate and intake were equivalent across the two conditions.
Because observers scored acceptance any time the bite entered the child's mouth, acceptance was always 100% during EE, unless the therapist was unable to deposit a bite before the session ended. Therefore, to demonstrate that Cam's behavior changed during EE, data on latency to accept illustrate that acceptance occurred within seconds after bite presentation. Mean latency to accept bites was 3.8 s and 2.5 s during the first and second DRA plus EE treatment phases, respectively. Mean latency to accept bites was 2.6 s and 1.6 s during the first and second NCR plus EE treatment phases, respectively. These data indicate that the interventions not only increased Cam's acceptance, but that acceptance occurred within seconds after bite presentation across both conditions.
Cam's problem behavior was maintained by negative reinforcement. DRA plus EE and NCR plus EE were equally effective at increasing bite acceptance, reducing problem behavior, and minimizing negative vocalizations. Given that the interventions worked and were mostly equally effective, caregiver preference for the two interventions might be the most important determinant of which to use. The social validity questionnaire revealed that Cam's mother preferred NCR plus EE over DRA plus EE. In fact, she rated NCR plus EE as more acceptable, easier to implement, and as a better fit for her child's needs. In addition, she said that she would feel more comfortable implementing NCR plus EE at home and in public settings. After discharge, Cam's mother reported that she and her husband implemented the NCR plus EE intervention at home. NCR may have been more preferred because it was easier to implement. She mentioned that she felt continuous access to preferred toys was more “comforting” to her child than providing toys contingent on acceptance.
One limitation of this study is that EE was not evaluated separately from DRA or NCR. Thus, it is possible that EE alone would have produced similar results. Although other studies have shown that escape extinction may be necessary to increase bite acceptance and may be effective regardless of whether DRA or NCR is also present, the focus of the current study was on which of these two reinforcement procedures produced greater decreases in problem behavior and was more socially acceptable to caregivers. In addition, when asked at intake, Cam's mother did not approve the use of EE alone, so we were unable to include that comparison. Future studies might evaluate the acceptability of EE alone relative to EE plus positive reinforcement procedures such as DRA or NCR.
Footnotes
Action Editor, Cathleen Piazza
Figure 1.
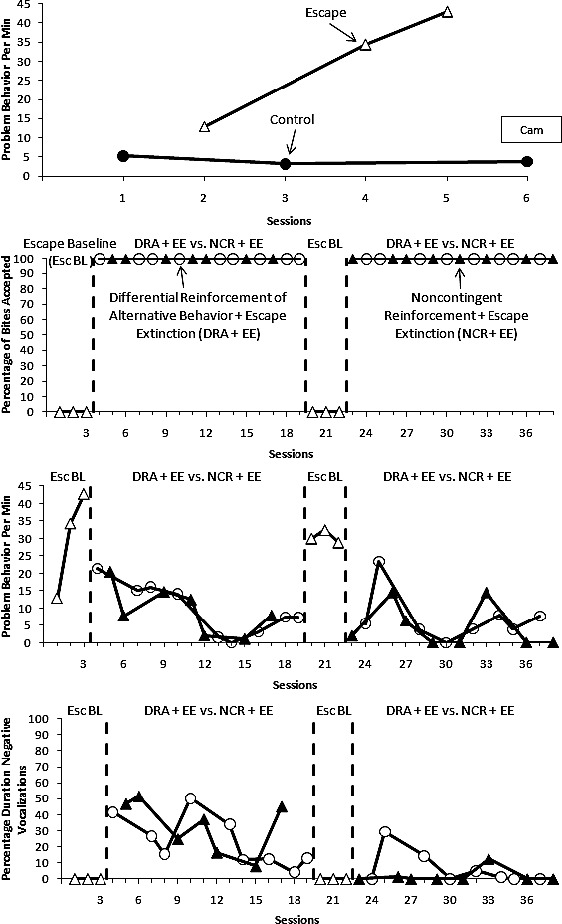
Problem behavior per minute during the functional analysis (top panel) and percentage of bites accepted (second panel), problem behavior per minute (third panel), and percentage of negative vocalizations (bottom panel) during the treatment evaluation.
REFERENCES
- Bachmeyer M. H, Piazza C. C, Fredrick L. D, Reed G. K, Rivas K. D, Kadey H. J. Functional analysis and treatment of multiply controlled inappropriate mealtime behavior. Journal of Applied Behavior Analysis. 2009;42:641–658. doi: 10.1901/jaba.2009.42-641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher W, Piazza C. C, Bowman L. G, Hagopian L. P, Owens J. C, Slevin I. A comparison of two approaches for identifying reinforcers for persons with severe and profound disabilities. Journal of Applied Behavior Analysis. 1992;25:491–498. doi: 10.1901/jaba.1992.25-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza C. C, Patel M. R, Gulotta C. S, Sevin B. M, Layer S. A. On the relative contribution of positive reinforcement and escape extinction in the treatment of food refusal. Journal of Applied Behavior Analysis. 2003;36:309–334. doi: 10.1901/jaba.2003.36-309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed G. K, Piazza C. C, Patel M. R, Layer S. A, Bachmeyer M. H, Bethke S. D, et al. On the relative contributions of noncontingent reinforcement and escape extinction in the treatment of food refusal. Journal of Applied Behavior Analysis. 2004;37:27–41. doi: 10.1901/jaba.2004.37-27. [DOI] [PMC free article] [PubMed] [Google Scholar]


