Abstract
Few studies have examined the effects of the high-probability instructional sequence in the treatment of food selectivity, and results of these studies have been mixed (e.g., Dawson et al., 2003; Patel et al., 2007). The present study extended previous research on the high-probability instructional sequence by combining this procedure with low-probability demand fading with 2 boys with autism (9 and 10 years old) who had a history of food selectivity and engaged in active food refusal behaviors when presented with novel foods. Response requirements were faded gradually from responses the child would tolerate (e.g., touching the food) to the final requirement of chewing and swallowing the food. The antecedent-based intervention was implemented in the absence of escape extinction and was effective in increasing food consumption for both participants. Possible mechanisms responsible for the effectiveness of the intervention are discussed along with directions for future research.
Key words: food selectivity, noncompliance, high-p instructional sequence, demand fading
Food selectivity has been conceptualized as a form of noncompliance in which the child refuses to eat a sufficient variety of food (Dawson et al., 2003). Selective food preferences may result in inadequate daily nutritional intake even though the child may maintain his or her weight by eating a sufficient quantity of preferred foods. Furthermore, children with an autism spectrum disorder (ASD) may be especially at risk for developing abnormal eating behaviors of this type (Ahearn, Castine, Nault, & Green, 2001). Several authors have suggested that feeding problems result from a combination of environmental, behavioral, and physical factors (Ahearn, Kerwin, Eicher, & Lukens, 2001; Freeman & Piazza, 1998).
Although the etiology of feeding disorders varies across children, feeding problems often persist as a result of environmental factors. Research has suggested that reinforcement plays a large role in the development and maintenance of inappropriate mealtime behaviors (Freeman & Piazza, 1998; Kern & Marder, 1996). For example, refusing food may be positively reinforced when parents offer their child a reward contingent on refusal behaviors rather than setting up a contingency prior to presenting the meal (e.g., a parent might tell the child “If you eat your apple, you can watch a video”). Alternatively, inappropriate mealtime behavior may be negatively reinforced when the child is allowed to leave the meal early contingent on such behaviors. When attempts to introduce new foods to the child are met with resistance, noncompliance, or tantrums, Kern and Marder (1996) noted that many parents often resort to offering the child a preferred food to abate the negative behavior. Based on this learning history, parents of selective eaters may stop introducing new foods and provide their children with only preferred foods to avoid these negative mealtime behaviors.
Although complete food refusal requires intensive, and often invasive, treatment procedures provided by a team of experienced medical professionals, research suggests that less intrusive treatment procedures may be effective for children who struggle with food selectivity (Bachmeyer, 2009; Patel et al., 2007). As mentioned previously, food selectivity has been conceptualized as a form of noncompliance (Dawson et al., 2003); therefore, the focus of the current study was to evaluate two antecedent interventions that have been previously shown to be effective in increasing compliance. Specifically, the current study examined a high-probability (high-p) instructional sequence and demand fading. Instructions with a higher probability of compliance were issued prior to an instruction with a lower probability of compliance, and the difficulty of low-probability (low-p) instructions was increased gradually until the terminal response requirement was met.
Although research has demonstrated the effectiveness of the high-p instructional sequence for increasing compliance (e.g., Mace et al., 1988), few studies have evaluated the effects of the high-p instructional sequence for the treatment of noncompliance in the form of food selectivity. Dawson et al. (2003) evaluated the effects of the high-p sequence alone and combined with escape extinction (EE) relative to EE alone in a young girl with a history of food refusal and gastrostomy-tube dependence. Results showed that the high-p instructional sequence was ineffective when escape was delivered contingent on noncompliance. Acceptance occurred only during the conditions in which EE was implemented, regardless of the delivery of high-p instructions. The authors suggested that the high-p sequence was ineffective without an EE component because the positive reinforcement available for compliance did not compete with the negative reinforcement provided for escape behavior. However, a potential limitation of this study was that high-p instructions required simple fine motor responses that were not related to eating, and the low-p instructions required multiple responses (i.e., opening the mouth, chewing the food, swallowing, and retaining the food).
Patel et al. (2007) further evaluated the effects of high-p instructional sequences without EE in the treatment of feeding-related noncompliance. Prior to treatment, a compliance assessment was conducted to demonstrate that the child's acceptance of an empty spoon was a high-p response. The effects of the high-p sequence were evaluated using an ABAB reversal design. In Phase A, the therapist presented low-p instructions every 30 s; the therapist placed a spoonful of food in a bowl in front of the participant and delivered up to two verbal instructions to take a bite before removing the bite. Verbal praise and light physical touch (e.g., high fives) were provided contingent on compliance. A 20-s escape period was provided contingent on inappropriate behavior (e.g., turning head, spitting). The procedures in Phase B were identical to those in Phase A, except the therapist presented an empty spoon three times rapidly (i.e., high-p instruction) before presenting the low-p instruction. Results showed zero compliance when the low-p instructions were presented in isolation and 100% compliance when the high-p sequence preceded the low-p instruction. Furthermore, the child's mother was taught to implement the intervention during mealtimes following treatment. Unlike Dawson et al. (2003), the high-p and low-p responses in this study were topographically similar (both involved accepting a spoon); in addition, the participant in this study engaged in what the authors referred to as passive refusal (i.e., not responding to bite presentations in the absence of problem behavior) whereas the participant in Dawson et al. displayed active refusal (noncompliance that co-occurred with problem behavior). These discrepancies may account for why the high-p sequence was found to be effective in Patel et al. but not in Dawson et al.
Demand fading, in which the number of requests to take a bite is increased gradually (also known as bite fading), is another antecedent intervention that has been shown to be effective in the treatment of feeding difficulties. Najdowski, Wallace, Doney, and Ghezzi (2003) evaluated a large magnitude of reinforcement for the acceptance of bites in conjunction with bite fading and EE. Initially, an entire plate of high-preference food was provided when the child accepted one bite of nonpreferred food; with each increase in bite requirement, the magnitude of reinforcement was decreased until the child reached his terminal bite requirement and the plate of high-preference foods was faded completely.
Penrod, Wallace, Reagon, Betz, and Higbee (2010) extended Najdowski et al. (2003) by further evaluating the effects of bite fading as one component of treatment in a sequential component analysis. For two participants, results were similar to those of Najdowski et al.; food consumption increased when bite fading was implemented in conjunction with a large reinforcer and EE. However, for one participant, bite fading combined with a large reinforcer was effective in increasing food consumption without the use of EE.
Although results of studies evaluating the high-p instructional sequence and bite fading are promising, these antecedent interventions may be germane to some children only. For children who may not tolerate even being in the presence of certain foods or engage in active refusal, these procedures may not be effective when implemented in the absence of EE. Therefore, the purpose of the current study was to extend previous research by evaluating the high-p instructional sequence and demand fading in the treatment of food selectivity in two boys who exhibited active refusal. The effectiveness of the high-p instructional sequence was evaluated when combined with demand fading in which response requirements consisted of graduated approximations to the final response requirement of consumption. More specifically, the difficulty of the low-p instructions was increased gradually. High-p instructions that required physical contact with the target foods (e.g., touching the food, smelling the food) preceded low-p instructions, which involved increasingly closer approximations to the terminal desired response of chewing and swallowing the food (similar to a shaping procedure).
METHOD
Participants and Setting
Two children, both with a diagnosis of ASD and a history of food selectivity, participated. Cole was a 9-year-old boy, and Colin was a 10-year-old boy. Participants were recruited from the Autism Center for Excellence at California State University, Sacramento (CSUS). Children selected as participants were required to have at least an imitative repertoire (i.e., the ability to copy or mimic another person's actions) and some listener skills (e.g., the ability to follow one-step instructions). The children also had to have a limited food repertoire within at least one primary food group (i.e., fruit or vegetable, protein, dairy, and starch), and they had to be resistant to trying new foods. Parents were asked to complete the Behavioral Feeding Assessment Parent Interview to identify potential participants (Budd et al., 1992). Parents also were interviewed to identify 12 foods that their children did not prefer from one or more of the food groups listed above. Prior to the start of the study, Cole's food repertoire was limited to dairy, starches, and some proteins (e.g., grilled cheese sandwiches, waffles, and hamburgers). Colin's food repertoire was limited to starches and proteins (e.g., pancakes, bacon, and hot dogs). Both participants engaged in gagging, spitting, or vomiting when presented with novel foods.
All treatment sessions took place in the pediatric behavior research laboratory (measuring approximately 3.7 m by 4.6 m) on the CSUS campus. The treatment room was equipped with a table, chairs, and items relevant to the feeding session (e.g., preferred and nonpreferred foods, napkins, utensils). Two to four consecutive sessions (i.e., alternating baseline and treatment sessions described below), with 5-min breaks in between, were conducted 2 to 3 days per week. Sessions were trial based (described below) rather than time based, but were approximately 10 min in duration; on average, four sessions were completed within approximately 60 min (including breaks between sessions and time for setup and cleanup).
Design and Response Measurement
A multielement design was used that alternated between two food groups, one associated with baseline and the other associated with treatment. The dependent variable was the percentage of bites consumed as well as the percentage of compliance with low-p instructions. Bite consumption was defined as a clean mouth after 5 s of food acceptance, and compliance was defined as the participant following through with an instruction after the first or second prompt (further described below). Data on both child and therapist behaviors were recorded on a trial-by-trial basis using prepared data sheets. Child behaviors included consumption and compliance, and therapist behaviors included prompting and reinforcer delivery. Percentage of bites consumed was calculated by dividing the total number of bites consumed by 12 (the total number of trials [each trial consisted of two high-p instructions and one low-p instruction] presented during the session) and converting the result to a percentage. Percentage of compliance was calculated by dividing instances of compliance with the low-p instruction by 12 (the total number of low-p instructions issued within one session) and converting the result to a percentage. Data were analyzed by graphing the percentage of compliance with low-p instructions as well as the percentage of bites consumed for each session.
Procedural integrity data were collected on all trials for therapist prompting and reinforcer delivery and were calculated as the total number of correct implementations divided by the sum of correct plus incorrect implementations; the result was converted to a percentage. Procedural integrity for prompting averaged 100% and 99% (range, 97% to 100%) for Cole and Colin, respectively. Procedural integrity for reinforcer delivery was 94% (range, 92% to 100%) and 99% (range, 97% to 100%) for Cole and Colin, respectively.
Two independent observers collected interobserver agreement data for compliance with low-p requests, bites consumed, and procedural integrity measures for 36% of Cole's sessions and 52% of Colin's sessions. Interobserver agreement was calculated by dividing the total number of agreements by the sum of agreements plus disagreements and converting the result to a percentage. Agreement for compliance to low-p requests was defined as both observers scoring the same behavior (compliance following the first prompt, compliance following the second prompt, or noncompliance) for each trial. Agreement for bites consumed was defined as both observers marking the trial in the same way (either by marking a plus to indicate the child swallowed [defined as a clean mouth following acceptance] or by marking a minus to indicate noncompliance). Agreement for procedural integrity was defined as both observers marking the trial in the same way for both procedural integrity measures (marking either a plus or a minus to indicate correct or incorrect implementation of therapist prompting and reinforcer delivery; observers had to agree on both measures in order for the trial to count as an agreement). Interobserver agreement was 100% for compliance with low-p requests, 100% for bites consumed, and 99% (range, 94% to 100%) for procedural integrity across both participants.
Pretreatment Preference Assessment
Prior to the start of treatment, parents were asked to choose two nonpreferred foods from each food group. Four foods were targeted during treatment, and four foods were used for baseline measures. A single-stimulus preference assessment (Pace, Ivancic, Edwards, Iwata, & Page, 1985) was conducted to ensure that foods chosen by the parent were truly nonpreferred by the participant. Prior to the assessment, the participant was prompted to sample each food. Each trial consisted of presenting one food item to the participant for 5 s. If he approached the food (e.g., reached toward the food and touched it) within the time allowed, that item was made available for an additional 5 s. If he failed to approach the food within 5 s, he was prompted to “try the food.” If he refused the food item during the next 5 s, the food was removed and the next trial began. For both participants, each of the foods included in baseline and treatment were never approached and consumed. Each food included in the assessment was presented a total of three times.
Following the single-stimulus preference assessment, a paired-choice preference assessment (Fisher et al., 1992) was conducted to evaluate relative preferences for high-preference (HP) foods that could be used as response-dependent reinforcement throughout each phase. Seven items identified as preferred by the participants' parents were presented in pairs, and the participant was prompted to “pick one.” The assessment continued until each food had been paired with every other food once, and the two to three food items selected and consumed most often were delivered contingent on compliance during each phase. Parents were asked to restrict access to the chosen HP food outside the treatment sessions.
Baseline
During the initial baseline, the food group for treatment (Group A) and the food group for baseline (Group B) were alternated, with each session consisting of 12 trials (i.e., four foods each presented three times). Foods were presented in small bite-sized pieces (e.g., a cucumber cut into six equal pieces). In addition, each condition was associated with a different therapist. One bite of food at a time was placed in front of the participant. If he did not take a bite of food within 5 s of the presentation, the therapist delivered a verbal instruction (e.g., “Colin, take a bite”). If the participant failed to take a bite within 5 s of the first verbal instruction, the therapist delivered another verbal instruction. If he did not take a bite within 5 s of the second verbal instruction, the therapist removed the bite and presented the next bite approximately 20 s later. The therapist ignored food refusal (i.e., made neither eye contact with the child nor any statements about the refusal behavior), removed the bite of food, and began the next trial approximately 20 s later. Food refusal was defined as the participant vocally refusing the food at any time after it was placed in front of him (e.g., by saying “no”), gagging either with or without food in the mouth (i.e., making a choking noise or thrusting the tongue forward as if to expel or vomit food), food expulsion (i.e., spitting food out after accepting it past the plane of the lips), or vomiting (either before or after a bite presentation). The participant received praise contingent on compliance following the first or second instruction.
Instructional Procedure
Responses observed during the initial baseline determined the starting phase for each participant. For example, if during baseline, the participant licked the food after being instructed to “take a bite,” this was the starting phase at the onset of treatment. The initial low-p instruction for Colin was “kiss the food,” and the initial low-p instruction for Cole was “balance the food on your tongue.” It should be noted that, in baseline, the only instruction presented was to “take a bite.”
To establish a motivating operation for compliance, the participant was permitted 10 s of noncontingent access to the HP food at the start of the session. Each session consisted of 12 trials with three instructions for each of four targeted foods. Each instruction was issued in conjunction with a model prompt (e.g., “Touch the food” [while the therapist touched the food] or “Do this” [while touching the food]; “Eat your watermelon” [while the therapist demonstrated chewing and swallowing a bite of watermelon]). Both high-p and low-p instructions were issued with model prompts. If compliance did not occur after the first instruction, the therapist repeated the instruction; if compliance still did not occur, the therapist removed the bite of food and presented the next target food approximately 20 s later. Further, the same procedures described in baseline were followed for refusal. Compliance with the first two high-p instructions resulted in praise from the therapist, and compliance with the last instruction (low-p) resulted in praise plus a small portion (two to three small bites) of the HP food. Low-p instructions were issued immediately after the delivery of high-p instructions. The criterion for moving from one phase to the next was at least three consecutive sessions with 100% compliance with all instructions; however, if the participant engaged in food refusal (specifically, gagging or vomiting), phase changes were postponed until food refusal no longer occurred.
It should be noted that previous low-p instructions were issued as high-p instructions as low-p instructions were faded in. For example, two high-p instructions, “touch the food” and “smell the food,” might be issued prior to the delivery of the low-p instruction, “kiss the food”; once the child consistently complied with the low-p instruction, “kiss the food,” in the absence of food refusal for at least three consecutive sessions, the next low-p instruction would be introduced in a subsequent phase and the first high-p instruction from the previous phase would be dropped. Instructions were presented in the same sequence such that the previous low-p instruction would be issued as the second high-p instruction (i.e., “smell the food,” “kiss the food” [previous low-p instruction], and “lick the food” [new low-p instruction]). The instructional sequence introduced across phases was as follows: (a) touch the food, (b) smell the food, (c) kiss the food (initial low-p instruction for Colin), (d) lick the food, (e) balance the food on tongue (initial low-p instruction for Cole), (f) bite the food into two pieces, (g) eat one of the pieces, (h) chew the food (i.e., one of the pieces) into little pieces (this was a remedial phase added for both participants after an unsuccessful transition to eating one of the pieces; they were required to chew the food until the therapist indicated it was safe to swallow, at which point the participant spit out the chewed food), and finally (i) swallow the chewed food (both pieces). The initial low-p instruction for Cole was to balance the food on his tongue, which was preceded by the instruction to kiss the food and lick the food; hence, Cole was never given the first two instructions listed above (touch the food and smell the food). It should be noted that the demand fading steps were not selected based on a standard instructional sequence but rather on the primary investigator's previous clinical experience.
Once participants reached 100% compliance with eating each bite of the target foods for three sessions in a row, the therapist increased the bite requirement to six bites of each target food (a total of 24 bites of food per session). At this point, high-p instructions no longer preceded the terminal low-p instruction to consume each bite of food. It was observed that both participants immediately began eating the target foods as soon as they were presented; therefore, it was decided that the high-p instructions were no longer necessary. The criterion for completion of treatment was three sessions of eating six bites of each of the target foods in the absence of refusal. Next, treatment sessions for Group A foods were alternated between the therapist and the research assistant who had been associated previously with baseline to ensure that compliance was not trainer specific and was, instead, under control of the treatment procedures.
Posttreatment Assessment
A posttreatment preference assessment was conducted with the baseline foods (Group B) to determine the extent to which accepting and swallowing generalized to other nonpreferred foods that were not specifically targeted during treatment. The single-stimulus preference assessment and procedures used during the pretreatment preference assessment were conducted as described previously. Each food was presented to the participant for 5 s. If he approached the food, it was made available for an additional 5 s; however, if he did not approach the food within the time allowed, the therapist presented the high-p and low-p instructions until the participant stopped complying.
Follow-up
Follow-up sessions were scheduled after completion of the treatment sessions as an additional evaluation of generalization and maintenance outside the experimental setting. Follow-up sessions were conducted at the participant's home with the experimenter and parent present, and the parent was taught to implement the treatment procedure with the baseline foods (Group B). The starting instruction for baseline foods was determined by the level of compliance observed with the low-p instructions during the posttreatment preference assessment. Follow-up sessions occurred 3, 6, and 12 weeks after completion of treatment.
RESULTS
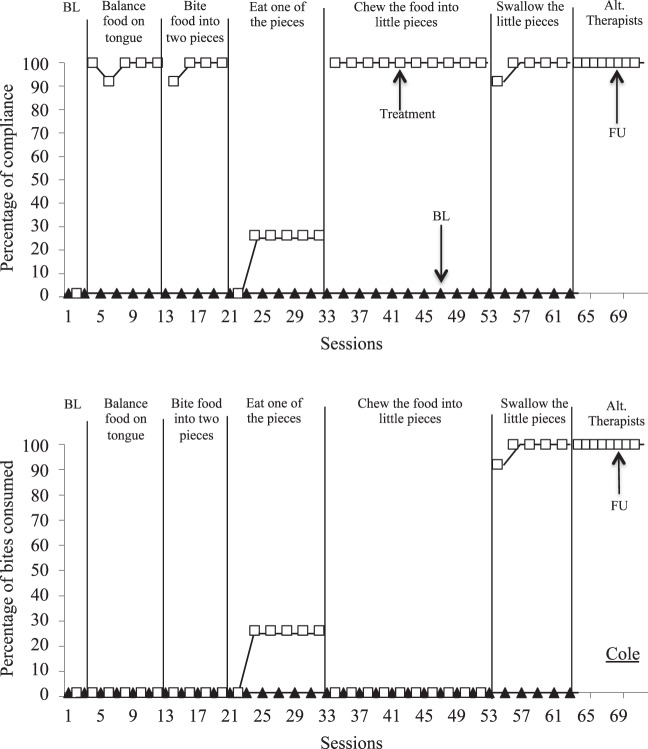
Figure 1 (top) depicts Cole's compliance to low-p requests across baseline and treatment phases. Compliance remained at zero during baseline when the low-p instruction (i.e., take a bite) was presented in isolation and increased only when demand fading was employed in combination with the high-p sequence preceding low-p instructions. Compliance decreased when the therapist presented the low-p instruction to eat one of the pieces of food; therefore, a subsequent remedial phase was added in which the therapist instructed Cole to chew the bite of food into little pieces. When the remedial phase was introduced, compliance returned to 100% and remained high for the remainder of treatment sessions. Once Cole was chewing and swallowing each of the four target foods, the therapist associated with baseline alternated conducting treatment sessions with the experimenter (with the same Group A foods); compliance and bite consumption (Figure 1) remained at 100% with this therapist, demonstrating that the increase in consumption was not trainer specific.
Figure 1.
Percentage of compliance (top) and percentage of bites consumed (bottom) for Cole during baseline and treatment.
Figure 1 (bottom) depicts Cole's bite consumption across phases. During the first two phases following baseline, Cole was not required to consume any of the food. In the third phase, when the low-p instruction to “eat one of the pieces” was introduced, consumption increased to and remained at 25%. With the introduction of the remedial phase (low-p instruction to chew the food into little pieces), bite consumption decreased to zero until Cole was instructed to swallow the chewed pieces. Once this phase was introduced, bites consumed increased to 100% within two treatment sessions.
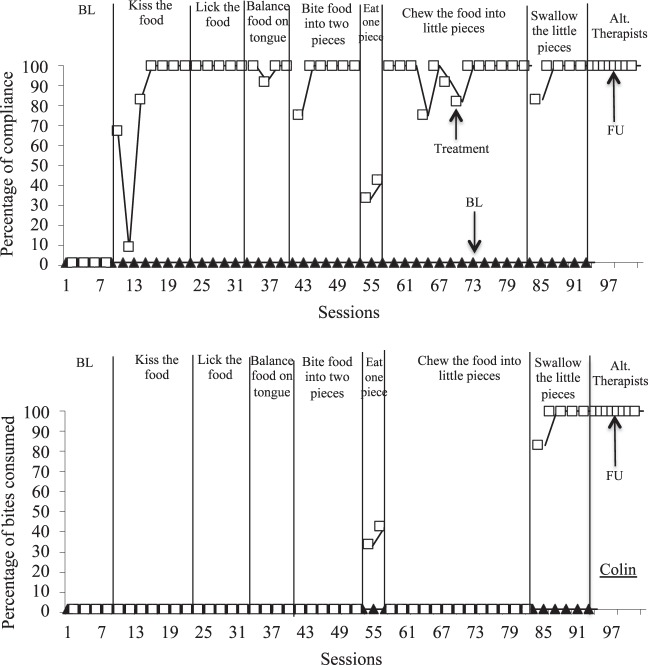
Figure 2 (top) depicts Colin's compliance to low-p instructions across both baseline and treatment phases. Compliance remained at zero during baseline sessions and increased only when demand fading was employed in combination with the high-p sequence preceding low-p instructions. Compliance decreased when the therapist presented the low-p instruction to eat one of the pieces of food; therefore, a remedial phase was implemented in which the therapist instructed Colin to chew the bite of food into little pieces. When the remedial phase was introduced, compliance returned to 100% and remained high for the remainder of treatment sessions. Similar to Cole, once Colin was chewing and swallowing each of the four target foods, the therapist associated with baseline also conducted treatment sessions (with the same Group A foods); compliance and bite consumption (Figure 2) remained at 100% with this therapist, demonstrating that the increase in consumption was not trainer specific.
Figure 2.
Percentage of compliance (top) and percentage of bites consumed (bottom) for Colin during baseline and treatment.
Figure 2 (bottom) depicts Colin's bite consumption across phases. He was not required to consume any of the food until Session 54, when consumption increased to 42%; however, with the introduction of the remedial phase (low-p instruction to chew the food into little pieces), bite consumption decreased to zero until he was instructed to swallow the chewed pieces. Once this phase was introduced, bites consumed increased to and remained at 100% within two treatment sessions.
Although data on the frequency of specific refusal behaviors were not collected, anecdotally, both boys primarily engaged in vocal protests during baseline. During treatment, when compliance was at 100%, refusal generally did not occur. For both participants, when the instruction to eat one of the pieces was introduced, compliance dramatically decreased and there was a concomitant increase in refusal; during this phase, gagging and, on occasion, vomiting were observed in conjunction with vocal protests.
Prior to completion of treatment, bite requirements were expanded systematically by increasing the volume of food required for consumption prior to receiving reinforcement. At the end of treatment, Cole was eating one slice of watermelon, six kernels of corn, two strawberries, and one slice of cucumber per session. Colin was eating nine bites of chicken, nine noodles, four baby carrots, and nine bites of banana per session. For both participants, two treatment sessions were conducted each day.
During the posttreatment assessment with Group B foods, neither participant consumed any of the foods presented, suggesting that preference for and generalization to nontargeted foods did not occur. Therefore, each food in this group was presented to the child following the aforementioned instructional sequence. The first instruction at which compliance no longer occurred was the starting point for parent training. The starting instructions for Cole and Colin were “balance food on tongue” and “lick the food,” respectively. During three follow-up visits, both Cole's and Colin's mothers were taught to implement treatment during mealtimes at home. Compliance and bite consumption for both participants remained at 100% during parent implementation of treatment.
DISCUSSION
This study sought to examine the effects of a proactive feeding intervention that used high-p instructional sequences in combination with low-p demand fading in the absence of EE. Results corroborated those of Patel et al. (2007), suggesting that antecedent-based treatments may increase food consumption in the absence of EE or physical guidance. The study also extends previous research on the high-p instructional sequence. The feeding intervention increased consumption for both Cole and Colin despite active refusal (e.g., spitting, gagging, and vomiting), which had not been observed by Patel et al. Active refusal was observed by Dawson et al. (2003), and the high-p instructional sequence was not effective in increasing food consumption in the absence of EE. This led the authors to suggest that antecedent-based treatments are ineffective when escape is provided for refusal.
As noted previously, a possible reason for the discrepant results between Dawson et al. (2003) and Patel et al. (2007) is that the high-p instructional sequence used in Dawson et al. involved motor responses that were not related to eating, whereas the low-p response was a more complex behavior that involved multiple steps associated with eating (i.e., opening the mouth, chewing the food, and swallowing). As in Patel et al., our high-p and low-p instructions were both related to eating; however, our high-p responses required physical contact with the target foods. In addition, demand fading was implemented in conjunction with the high-p instructional sequence; specifically, high-p and low-p instructions built on each other as the participants moved across phases. With the introduction of each low-p instruction, a closer approximation to the terminal response of chewing and swallowing was required. This may have been a contributing factor to the acquisition of eating observed in the current study. In other words, it is possible that the procedure responsible for the increase in food consumption was the demand fading component and not the high-p instructional sequence. Future research should evaluate the relative effects of demand fading alone and in combination with the high-p instructional sequence.
An important finding of the current study was that the increase in food consumption was maintained across people and environments. Cole's compliance and consumption remained at 100% when his mother was taught to implement the treatment procedure at home. This is promising given that there are more opportunities to conduct treatment sessions throughout the day when at home (e.g., at each mealtime), whereas the number of treatment sessions per day may be limited in a clinical setting. In addition, because this feeding intervention did not require EE and was not time consuming, teachers or clinicians may be successful in implementing this treatment in a school setting, again increasing the child's opportunity to contact novel foods.
Although this study adds to the literature on the use of the high-p instructional sequence in the treatment of food selectivity, several limitations should be addressed in future research. First, the hierarchy of instructions was selected somewhat arbitrarily. The starting phase for treatment was based on behaviors observed in baseline following the instruction to “take a bite”; however, the escape contingency for noncompliance may have prevented opportunities to observe other behaviors. It is possible that participants may have complied with later steps in the hierarchy of instructions in spite of noncompliance with earlier steps; future research should conduct a compliance assessment for each step prior to selecting the starting phase for treatment. In addition, the last fading step was not probed prior to advancing phases; therefore, some of the fading steps may not have been needed.
The total quantity of food consumed during treatment sessions may seem negligible given the number of sessions to complete treatment. Participants were given only a limited amount of food. Initially, 12 small bites were presented (three bites of four different foods) during each session. Although the bite requirement was increased from 12 bites to 24 bites (six bites of four different foods) per session, the size of the bites was not increased. It is possible that participants would have consumed a greater quantity of food if given the opportunity. The bite sizes were not increased to avoid the possibility of satiation because more than one treatment session was conducted per day.
Other limitations include procedural differences across baseline and treatment conditions that make it difficult to draw definitive conclusions regarding the procedures responsible for increased compliance and food consumption. One procedural difference was that only vocal instructions were presented in baseline whereas in treatment, both high-p and low-p instructions were delivered in conjunction with a model prompt; thus, it is possible that modeling may have played a role in the increase in food consumption observed during treatment. In addition, HP foods were delivered for compliance with low-p instructions in treatment but only social praise was delivered contingent on compliance during baseline. Thus, it is possible that the increase in compliance and food consumption during treatment was a result of reinforcement in the form of HP foods.
Finally, a possible mechanism of behavior change may have been repeated exposure to novel foods. Participants had greater exposure to the treatment foods during treatment than during baseline. Specifically, during baseline, foods were presented directly in front of the participant. Contingent on refusal, the foods were removed and placed off to the side such that they were only peripherally visible. In treatment, foods also were removed and placed off to the side contingent on refusal; however, the foods remained directly in front of the participant after compliance with both high-p and low-p instructions. Given that compliance never occurred in baseline, one might argue that the participants had more direct exposure to the treatment foods. Furthermore, during treatment, participants were asked to engage in behaviors that simulated aspects of eating the food, which may have desensitized them to the actual behavior of eating rather than just tolerating being in the presence of the food. Anecdotal observations, however, indicated that participants often played with the baseline foods (e.g., touching, rolling, picking apart), which suggests that they were no less desensitized to the treatment foods than they were to the baseline foods.
Footnotes
Action Editor, Jennifer Zarcone
The research presented in this article was completed in partial fulfillment of thesis requirements for the MA degree by the second author. We thank Caio Miguel for his comments on a previous version of this manuscript and Shu Wing Fu for her assistance in conducting this project.
REFERENCES
- Ahearn W, Castine T, Nault K, Green G. An assessment of food acceptance in children with autism or pervasive developmental disorder not otherwise specified. Journal of Autism and Developmental Disorders. 2001;31:505–511. doi: 10.1023/a:1012221026124. [DOI] [PubMed] [Google Scholar]
- Ahearn W. H, Kerwin M. E, Eicher P. S, Lukens C. T. An ABAC comparison of two intensive interventions for food refusal. Behavior Modification. 2001;25:385–405. doi: 10.1177/0145445501253002. [DOI] [PubMed] [Google Scholar]
- Bachmeyer M. H. Treatment of selective and inadequate food intake in children: A review and practical guide. Behavior Analysis in Practice. 2009;2:43–50. doi: 10.1007/BF03391736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budd K. S, McGraw T. E, Farbisz R, Murphy T. B, Hawkins D, Heilman N, et al. Psychosocial concomitants of children's feeding disorders. Journal of Pediatric Psychology. 1992;17:81–94. doi: 10.1093/jpepsy/17.1.81. [DOI] [PubMed] [Google Scholar]
- Dawson J. E, Piazza C. C, Sevin B. M, Gulotta C. S, Lerman D, Kelley M. L. Use of the high-probability instructional sequence and escape extinction in a child with food refusal. Journal of Applied Behavior Analysis. 2003;36:105–108. doi: 10.1901/jaba.2003.36-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher W, Piazza C. C, Bowman L. G, Hagopian L. P, Owens J. C, Slevin I. A comparison of two approaches for identifying reinforcers for persons with severe and profound disabilities. Journal of Applied Behavior Analysis. 1992;25:491–498. doi: 10.1901/jaba.1992.25-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman K. A, Piazza C. C. Combining stimulus fading, reinforcement, and extinction to treat food refusal. Journal of Applied Behavior Analysis. 1998;31:691–694. doi: 10.1901/jaba.1998.31-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kern L, Marder T. J. A comparison of simultaneous and delayed reinforcement as treatments for food selectivity. Journal of Applied Behavior Analysis. 1996;29:243–246. doi: 10.1901/jaba.1996.29-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mace C. F, Hock M. L, Lalli J. S, West B. J, Belfiore P, Pinter E, et al. Behavioral momentum in the treatment of noncompliance. Journal of Applied Behavior Analysis. 1988;21:123–141. doi: 10.1901/jaba.1988.21-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najdowski A. C, Wallace M. D, Doney J. K, Ghezzi P. M. Parental assessment and treatment of food selectivity in natural settings. Journal of Applied Behavior Analysis. 2003;36:383–386. doi: 10.1901/jaba.2003.36-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace G. M, Ivancic M. T, Edwards G. L, Iwata B. A, Page T. J. Assessment of stimulus preference and reinforcer value with profoundly retarded individuals. Journal of Applied Behavior Analysis. 1985;18:249–255. doi: 10.1901/jaba.1985.18-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel M, Reed G. K, Piazza C. C, Mueller M, Bachmeyer M. H, Layer S. A. Use of a high-probability instructional sequence to increase compliance to feeding demands in the absence of escape extinction. Behavioral Interventions. 2007;22:305–310. [Google Scholar]
- Penrod B, Wallace M. D, Reagon K, Betz A, Higbee T. S. A component analysis of a parent-conducted multi-component treatment for food selectivity. Behavioral Interventions. 2010;25:207–228. [Google Scholar]