Abstract
The National Library of Medicine’s MedlinePlus Connect service extends the reach of the consumer health website MedlinePlus.gov to deliver relevant information to patients and providers via health IT systems, electronic health records, and patient portals.
Automation has been a part of the healthcare landscape for 50 years.1–3 Healthcare organizations have shifted from paper to computers for everything from billing and reporting to maintaining patient records, and recent IT advances now offer opportunities for institutions and individuals to access interoperable systems. This will have a profound impact on medical records in the form of electronic health records (EHRs) and patient health records (see the “Electronic Health Records” sidebar).
Furthermore, new incentives have emerged for patient engagement in the health IT community. The Health Information Technology for Economic and Clinical Health (HITECH) Act, part of the American Recovery and Reinvestment Act of 2009, contains incentives for demonstrating the “meaningful use” of certified EHRs.4 The regulations resulting from the HITECH Act define mandatory and optional “menu” objectives that eligible providers must achieve to show that they’re using EHRs in a meaningful way. One criterion for such meaningful use is providing patients educational information. More specifically, an EHR system should allow providers “to identify patient-specific education resources and provide those resources to the patient,” based on their individual diagnoses, medications, and laboratory tests.”5
To support the increasing use of IT in healthcare, and to address the new meaningful use requirements, the US National Library of Medicine (NLM), part of the National Institutes of Health (NIH), US Department of Health and Human Services (HHS), optimized its health information website, MedlinePlus.gov, for use in patient portals and EHRs.6 Since 1998, MedlinePlus.gov has provided reliable, up-to-date health information for patients and families. It contains authoritative, consumer-level health information in a variety of formats. NLM expanded MedlinePlus.gov to create MedlinePlus Connect, a service that brings high-quality, context-relevant health information to patients and healthcare providers as needed in a health IT system.
Electronic Health Records.
An electronic health record (EHR) is an electronic version of a patient’s medical history maintained by a healthcare provider. It can include key administrative clinical data relevant to a patient’s care under a particular provider, including progress notes, problems, medications, vital signs, past medical history, immunizations, laboratory data, and radiology reports. EHRs automate access to information and have the potential to streamline the healthcare provider’s workflow. EHRs can also support other care-related activities directly or indirectly through various interfaces, including evidence-based decision support, quality management, and outcomes reporting (see www.cms.gov/ehealthrecords).
EHRs go a step beyond the digital version of the paper charts in the healthcare provider’s office. They’re designed to reach out beyond the health organization that originally collects and compiles the information. Fully functional EHRs are built to share information with other healthcare providers, such as laboratories and specialists, so they contain information from different groups and healthcare providers involved in the patient’s care.1
EHRs are another step forward in healthcare’s continued progress, as they can strengthen the relationship between patients and healthcare providers. Timely and easily accessible data can enable providers to make better decisions and provide better care.1 EHRs are designed to be accessed by different people involved in a patient’s care—including patients themselves via patient portals. These portals can contain reports of laboratory tests, information on diagnoses, and a list of current medications.
With fully functional EHRs, members of the healthcare team have ready access to the latest information, allowing for more coordinated, patient-centered care.
- 1.Garrett P, Seidman J. EMR vs. EHR: What Is the Difference? HealthITBuzz. 2011 Jan 4; www.healthit.gov/buzz-blog/electronic-health-and-medical-records/emr-vs-ehr-difference.
MedlinePlus Connect
NLM developed MedlinePlus Connect with input and encouragement from the Institute for Family Health (IFH), a group of community health centers in New York. IFH sought to bring the consumer-friendly content from MedlinePlus to patients as needed in their patient portal. NLM and IFH partnered to develop the MedlinePlus Connect pilot. Throughout this process, NLM also worked with Epic, the EHR vendor of IFH’s patient portal—Epic MyChart.
MedlinePlus.gov contains information on hundreds of diseases, conditions, and wellness issues, and offers a medical encyclopedia, over-the-counter and prescription drug information, and herbs and supplements information. It also includes a medical dictionary, interactive tutorials, anatomy and surgery videos, health news, directories of healthcare providers, and links to thousands of pages written and maintained by government agencies and other trusted and authoritative US health organizations. The site is available in English and Spanish, with select information in over 40 other languages. A version of MedlinePlus optimized for mobile devices is also available at m.medlineplus.gov (see the related article in this issue, “MedlinePlus Mobile: Consumer Health Information On-the-Go”).
Through patient portals, EHRs, and other health IT systems, MedlinePlus Connect delivers this information tailored to patients’ specific diagnoses, prescriptions and over-the counter medications, and laboratory tests. To achieve this context-sensitive information delivery, MedlinePlus Connect relies on coding standards already in use by health IT systems and healthcare organizations (see the “Healthcare Standards: Related URLs” sidebar).
Healthcare Standards: Related URLs.
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM):
www.cdc.gov/nchs/icd/icd9cm.htm
Systemized Nomenclature of Medicine—Clinical Terms (SNOMED CT)
www.nlm.nih.gov/research/umls/Snomed/snomed_main.html
Clinical Observations Recording and Encoding (CORE) Problem List Subset of SNOMED CT:
www.nlm.nih.gov/research/umls/Snomed/core_subset.html
RxNorm and RxNorm Concept Unique Identifiers (RXCUI):
www.nlm.nih.gov/research/umls/rxnorm/overview.html
National Drug Codes (NDC):
www.fda.gov/Drugs/InformationOnDrugs/ucm142438.htm
Logical Observation Identifiers Names and Codes (LOINC):
Coding Standards
MedlinePlus Connect supports the following coding standards.
The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) is a system based on the World Health Organization’s International Classification of Diseases. The Centers for Disease Control and Prevention and the Center for Medicare and Medicaid Services oversee the changes and modifications to ICD-9-CM, which is used to assign codes to inpatient, outpatient, and office-visit diagnoses and to inpatient procedures in the US. There are over 14,000 diagnosis codes in ICD-9-CM.
The Systemized Nomenclature of Medicine—Clinical Terms (SNOMED CT), including the Clinical Observations Recording and Encoding (CORE) Problem List Subset codes and their descendants, is a comprehensive clinical terminology. Originally created by the College of American Pathologists, the International Health Terminology Standards Development Organization now maintains SNOMED CT, which contains over 311,000 unique concepts. The CORE Problem List Subset contains the most frequently used 14,800 terms that cover 95 percent of usage volume in seven major medical institutions.
RxNorm Concept Unique Identifiers (RXCUI) are identifiers in RxNorm, a standardized nomenclature produced by the NLM for clinical drugs for humans.
National Drug Codes (NDC) are three-segment numbers that serve as universal identifiers for human drugs. Drug manufacturers provide these codes to the US Food and Drug Administration.
Logical Observation Identifiers Names and Codes (LOINC), produced by the Regenstrief Institute at Indiana University, provides formal names and standardized codes for laboratory and other clinical observations. LOINC contains more than 65,000 terms.
Operation and Communication
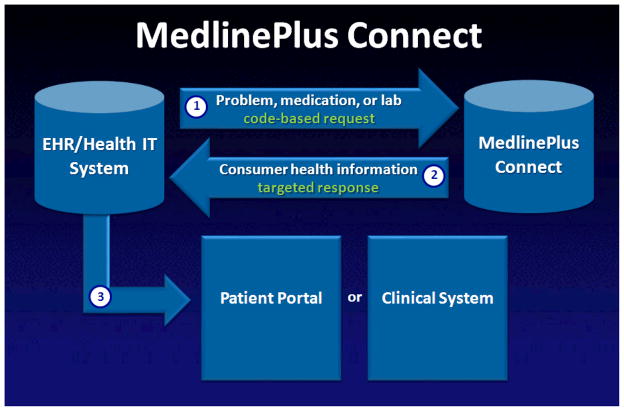
MedlinePlus Connect operates through a simple request-and response-based process. An EHR interface, patient portal, or health IT system sends a code-based request to MedlinePlus Connect, which responds with relevant information on diagnoses, medications, and laboratory tests. The requesting system then delivers the content to patients and providers through a patient portal or clinical interface (see Figure 1).
Figure 1.
The basic structure for MedlinePlus Connect communications. MedlinePlus Connect receives code-based requests and responds with relevant information. The requesting system then delivers the content to patients and providers through a patient portal or clinical interface.
Any health IT system, EHR, or patient portal that uses one or more of the coding standards just described can implement MedlinePlus Connect. Health IT system vendors can offer MedlinePlus Connect as a feature or option to their clients. Alternatively, health IT system purchasers can implement MedlinePlus Connect directly if they have appropriate administrative rights within the system.
To maximize implementation flexibility, NLM offers MedlinePlus Connect as a Web application and Web service. The Web application responds to requests with an on-demand formatted webpage that contains relevant information for patients. The Web service responds to requests with XML, which can be incorporated into any health IT interface in a fully customizable fashion. Because NLM maintains the code-based mappings, topic links, and retrieval technologies, MedlinePlus Connect only needs to be implemented once and requires little maintenance on the part of health IT vendors or purchasers.
Technical Approach
In the first phase of development, IFH’s needs guided the MedlinePlus Connect team. IFH wanted to link its patient portal to MedlinePlus using the ICD-9-CM code system. The developers built a simple three-tier system, with NLM’s ColdFusion application servers handling presentation and business logic, and the Enterprise Oracle Database Cluster handling mappings between the code-based requests and appropriate MedlinePlus content. The developers designed the application to abstract the business logic using a ColdFusion component, and a ColdFusion template handled all presentation logic. This allowed for modular development, so the system could support requests for different code systems as it (and its users’ needs) grew, without requiring developers to alter or rewrite the core program. NLM designed this initial implementation as a Web application that provides an HTML page in response to requests.
The Mapping Process
The process for mapping the individual codes to appropriate consumer-friendly content from MedlinePlus.gov was iterative. NLM initially investigated two automated approaches, using a de-identified file of the top 2,500 ICD-9-CM codes provided by IFH. IFH removed personally identifying information from the file. The Lister Hill National Center for Biomedical Communications explored automated approaches using programs from NLM’s Unified Medical Language System, and those preliminary mappings helped with—but couldn’t replace—the manual mapping process. The MedlinePlus Connect team found that manual mapping ensured the best possible matches.
Also, the MedlinePlus Connect team reviewed the National Hospital Discharge Survey (www.cdc.gov/nchs/nhds.htm) to determine the most frequently used inpatient diagnosis codes and identified clinical topics on MedlinePlus that had not yet been mapped to a diagnosis codes. During this process, the team would match one ICD-9-CM diagnosis code with up to three MedlinePlus topics, and they expanded MedlinePlus to include more topics to better address the needs of EHR users. For example, a popular problem code is for a medical checkup. The MedlinePlus team researched and created a topic called Health Checkup to meet this need. Since the initial release of MedlinePlus Connect, the team has regularly reviewed the incoming code-based requests, looking for codes that have not yet been mapped.
The initial MedlinePlus Connect system was a home-grown, proof-of-concept implementation and followed no published standard. Subsequently, NLM engaged in conversations with two of the authors of the Health Level Seven (HL7) Context-Award Knowledge Retrieval (Infobutton) standard, which allows health IT systems to submit knowledge requests to knowledge resources.7 NLM adopted the HL7 Context-Aware Knowledge Retrieval (Infobutton) specification.
The team later released support for SNOMED CT CORE Problem List Subset code requests and the ability to provide answers to diagnosis code requests in Spanish. Recently, NLM expanded this coverage to include the descendants of the SNOMED CT CORE Problem List subset.
For laboratory test information, NLM took a similar approach and manually mapped LOINC codes to appropriate content on MedlinePlus.gov. NLM mapped the Common Lab Orders Value Set to specific pages on MedlinePlus that correspond to each lab test (see http://loinc.org/usage/orders/common-lab-orders-value-set.pdf). In most cases, a single page of content directly matched the test represented by the code. In some (infrequent) cases, the MedlinePlus Connect team mapped lab test codes to more than one page of content. LOINC experts from the Lister Hill National Center for Biomedical Communications reviewed and validated the mappings.
Providing responses for prescription and over-the-counter medications proved to be the most challenging feature to implement for MedlinePlus Connect. MedlinePlus.gov contains detailed medication information, but this content does not include mappings to the NDCs commonly used in EHRs, and the sheer number of medication codes prohibited a manual mapping approach.
To provide medication information through MedlinePlus Connect, NLM uses the RxNorm API (http://rxnav.nlm.nih.gov/RxNormAPI.html), which is a Representational State Transfer (REST) Web service for accessing the current RxNorm data set, in combination with using the Vivisimo search engine to identify appropriate content in the MedlinePlus.gov medication information collection. RxNorm is a standardized nomenclature for clinical drugs. MedlinePlus Connect can receive an RXCUI, NDC, or text string as a request for information related to a specific medication.
After receiving an NDC or a text string, MedlinePlus Connect sends the request to the RxNorm API, which responds with the corresponding RXCUI. Once the RXCUI is identified, or if the RXCUI is sent directly from the outside system, MedlinePlus Connect sends a second request to the RxNorm API to identify the medication brand names corresponding to that RXCUI. NLM executes a search for the brand names on MedlinePlus.gov using the Vivisimo search engine. (The MedlinePlus Connect team explored searching on ingredients, as opposed to the brand names, but found the results were not as robust or precise.) This multistep process yields positive results for MedlinePlus Connect users.
Table 1 shows the code types and systems MedlinePlus Connect supports and the processes that NLM uses to match codes to patient content on MedlinePlus.gov.
Table 1.
The US National Library of Medicine’s process for matching clinical codes to MedlinePlus.gov content.
| Request | |||
|---|---|---|---|
| Code type | Code system* | Matching process | MedlinePlus content |
| Problems | ICD-9-CM or SNOMED CT | Mapping file | Health topic pages |
| Lab tests | LOINC | Mapping file | Lab-related articles |
| Drugs | RXCUI or NDC | RxNorm API and search of MedlinePlus drug information | Drug-related articles |
See the “Coding Standards” section in the main text for more information
Following the Web application’s release, the programmers developed the MedlinePlus Connect API Web service. The service was written in parallel with the evolving HL7 specification for Web services, the HL7 Infobutton Service Oriented Architecture Implementation Guide.8 The service is implemented following the REST pattern of a GET request to the service with an XML packet conforming to the HL7 Specification.
A Typical Use Case
For both the MedlinePlus Connect Web application and Web service, a typical HTTP request from a user includes both the coding system and code. The base URL indicates whether the request is to the MedlinePlus Connect Web application or the service (http://apps.nlm.nih.gov/medlineplus/services/mpconnect.cfm [mpconnect_service.cfm], respectively). The naming convention for the URL parameters follows the HL7 Infobutton standard.
Table 2 shows the meaning of each parameter and Figure 2 shows complete requests for information on osteoporosis in English using the ICD-9-CM code 733.00.
Table 2.
Parameter definitions for a request to MedlinePlus Connect.
| URL parameter | Name | Example |
|---|---|---|
| mainSearchCriteria.v.cs | Coding system | mainSearchCriteria.v.cs=2.16.840.1.113883.6.103 |
| mainSearchCriteria.v.c | Code | mainSearchCriteria.v.c=733.00 |
| mainSearchCriteria.v.dn | Search test | mainSearchCriteria.v.dn=Osteoporosis |
| informationRecipient.languageCode.c | Language | informationRecipient.languageCode.c=en (for English) informationRecipient.languageCode.c=sp (for Spanish) |
Figure 2.
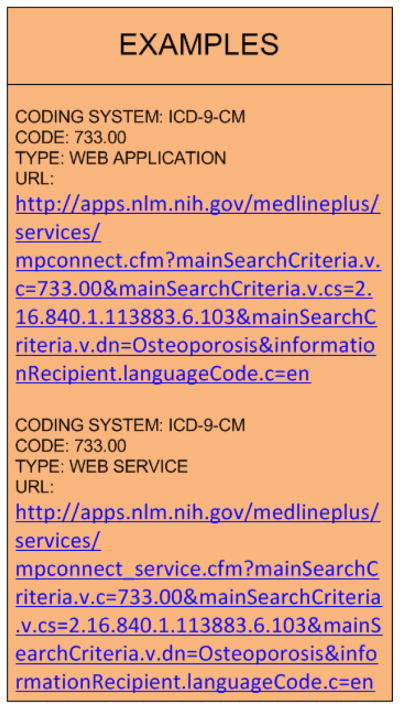
Examples of the complete URLs for MedlinePlus Connect (a) Web application and (b) Web service requests.
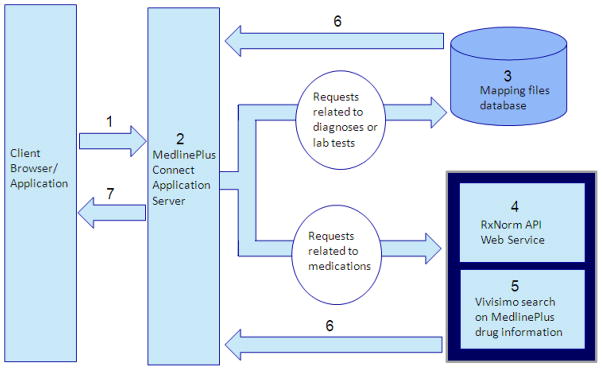
Figure 3 shows the steps for a typical MedlinePlus Connect use case. First, the user makes a request using the standard base URL and URL parameters. Second, the MedlinePlus Connect server decodes the URL requests and routes the request to the appropriate process. Third, for diagnosis codes and lab test codes, the MedlinePlus Connect server interacts with the mapping database to retrieve appropriate MedlinePlus information.
Figure 3.
Typical use case for MedlinePlus Connect. The steps taken depend in part on the type of request.
However, for medication information, MedlinePlus Connect interacts with the RxNorm API for any text string and NDC code requests to retrieve the appropriate RXCUI and corresponding brand names (fourth step). Then, using the brand names retrieved from the RxNorm API, MedlinePlus Connect conducts a Vivisimo search of MedlinePlus medication information (fifth step).
For the sixth step, Vivisimo returns a response containing links to relevant medication information to the MedlinePlus Connect server. Finally, for diagnosis, lab test, and medication codes, the MedlinePlus Connect server generates the HL7-compliant response and returns it to the user.
MedlinePlus Connect exemplifies an interdisciplinary, collaborative project that relied on expertise and input from both public and private sector partners. Its team overcame seemingly insurmountable challenges by building on existing NLM APIs and Web services to create linkages between clinical codes and relevant content. In addition, the team deliberately supported common clinical code systems and industry standards to make MedlinePlus Connect scalable and easy to implement and maintain.
In the future, the NLM will release support for Spanish medication responses and other clinical coding systems and vocabularies, including ICD-10-CM when it becomes the US standard. The team will also explore how to enhance responses to medication-related requests, other methods of delivering responses, and how to better tailor the responses.
Since it was first announced in November 2010, MedlinePlus Connect’s use has steadily increased, and it has been well received by the industry. In March 2011, MedlinePlus Connect received the coveted “HHSinnovates” award from US Department of Health and Human Services Secretary Kathleen Sebelius, recognizing NLM’s achievement and investment in harnessing technology to improve the public health. NLM anticipates that use and recognition of MedlinePlus Connect will continue to grow as adoption of health IT becomes more widespread and prevalent. For more information about MedlinePlus Connect, visit http://medlineplus.gov/connect.
Biographies
Sarena Burgess serves as programmatic technical lead for MedlinePlus Connect and as a librarian in the Health Information Products Unit at the National Library of Medicine. Her professional interests include consumer health information services and technologies. Burgess received her MS in information science from the University of Tennessee. Contact her at sarena.burgess@nih.gov.
Stephanie Dennis is the project manager for MedlinePlus Connect and a technical information specialist in the Health Information Products Unit at the National Library of Medicine. Her professional interests include consumer health information and health IT. Dennis received her MLS in library science from the University of Maryland College Park. Contact her at stephanie.dennis@nih.gov.
Soma Lanka works as a software consultant on the MedlinePlus Connect team in the Office of Computing and Communications Services at the National Library of Medicine. His professional interests include mobile technologies and health information systems. Lanka received his MS in electrical and computer engineering from the Ohio University. Contact him at soma.lanka@nih.hhs.gov.
Naomi Miller is manager of consumer health information at the National Library of Medicine. Her professional interests include consumer health information and vocabulary. Miller received her MLS from the University of Wisconsin-Madison. Contact her at millern@mail.nlm.nih.gov.
Joseph Potvin built the MedlinePlus Connect technical infrastructure and works as an IT team lead in the Office of Computer and Communications Systems at the National Library of Medicine. He specializes in Web applications, mobile, and section 508 Web accessibility. Contact him at joseph.potvin@nih.gov.
References
- 1.Haux R. Health Information Systems—Past, Present, Future. Int’l J Medical Informatics. 2006;75(3–4):268–81. doi: 10.1016/j.ijmedinf.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Collen MF. The Origins of Informatics. J Am Medical Informatics Assoc. 1994;1(2):91–107. doi: 10.1136/jamia.1994.95236152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morris DC, Brandon JS. Future Integrated and Interfaced HIS Systems. Computers in Healthcare. 1998;9(10):50–53. [PubMed] [Google Scholar]
- 4.HITECH Act Enforcement Interim Final Rule. US Department of Health and Human Services; Apr, 2012. www.hhs.gov/ocr/privacy/hipaa/administrative/enforcementrule/hitechenforcementifr.html. [Google Scholar]
- 5.Eligible Professional Meaningful Use Table of Contents Core and Menu Set Objectives. Centers for Medicare and Medicaid Services; Apr, 2012. www.cms.gov/EHRIncentivePrograms/Downloads/EP-MU-TOC.pdf. [Google Scholar]
- 6.Miller N, Lacroix E-M, Backus JEB. MedlinePlus: Building and Maintaining the National Library of Medicine’s Consumer Health Web Site. Bull Medical Library Assoc. 2000;88(1):11–17. www.ncbi.nlm.nih.gov/pmc/articles/PMC35193. [PMC free article] [PubMed] [Google Scholar]
- 7.HL7 Context-Aware Knowledge Retrieval (Infobutton) Knowledge Request URL-Based Implementation. Health Level Seven Int’l specification. 2010 Jan; http://wiki.hl7.org/index.php?title=Product_Infobutton#Product_Name_-_HL7_V3_IG:_URL-Based_Implementations_of_the_Context-Aware_Information_Retrieval_.28Infobutton.29.
- 8.HL7 Context-Aware Knowledge Retrieval (Infobutton) Service-Oriented Architecture Implementation Guide. Health Level Seven Int’l. 2011 Jan; http://wiki.hl7.org/index.php?title=Product_Infobutton#Product_Name_-_HL7_V3_Implementation_Guide:_Context-Aware_Knowledge_Retrieval_.28Infobutton.29_-_Service-Oriented_Architecture_Implementation_Guide.