Abstract
Background
Since 2001, Massachusetts state law dictates that emergency department (ED) patients with limited English proficiency have the right to a professional interpreter.
Methods
one year later, for two 24-h periods, we interviewed adult patients presenting to four Boston EDs. We assessed language barriers and compared this need with the observed use and type of interpreter during the ED visit.
Results
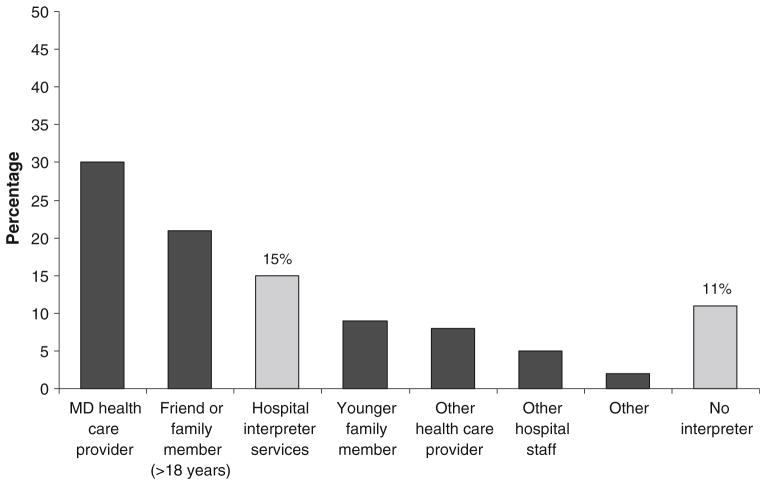
We interviewed 530 patients (70% of eligible) and estimated that an interpreter was needed for 60 (11%; 95% confidence interval, 7–12%) patients. The primary interpreter for these clinical encounters was a physician (30%), friend or family member age ≥18 years (22%), hospital interpreter services (15%), younger family member (11%), or other hospital staff (17%).
Conclusions
We found that 11% of ED patients had significant language barriers, but use of professional medical interpreters remained low. One year after passage of legislation mandating access, use of professional medical interpreters remained inadequate.
Keywords: Interpreters, Language barriers, Emergency department, Immigrants
Introduction
Since 2001, Massachusetts state law dictates that emergency department (ED) patients with no or limited English proficiency have the right to a professional medical interpreter [1]. Medical interpretation for limited-English-speaking patients significantly increases the quality of health care delivery, patient compliance, and overall patient satisfaction with the medical encounter [2, 3]. Interpreter type has an impact on the medical experience; a professionally trained interpreter is medically, linguistically, and culturally competent, providing the best interpretation for a medical encounter with a language barrier [4, 5]. The use of professional interpreters during an ED visit may lead to decreased ED re-visit rate and increased access to outpatient services, without simultaneous increase in length of stay or cost of the index ED visit [6, 7].
We conducted a prospective multicenter study in which we assessed language barriers during an interview in English (to assess interpreter demand), and compared this demand with the observed use and type of interpreter during the ED visit.
Methods
This multicenter, cross-sectional study was performed at four EDs in the Boston area: two university-affiliated hospitals and one community hospital in an urban setting, and one community hospital in a suburban setting. All sites are members of the Emergency Medicine Network (http://www.emnet-usa.org), which coordinated the study. The study was approved by the Institutional Review Board at all sites with a waiver of written informed consent.
Consecutive patients age 18 or older were enrolled over two 24-hour periods (one Wednesday and one Saturday) at each hospital in 2002. We attempted to interview all adult ED patients during the study period who were able to provide informed consent. Exclusion criteria were patients who were already interviewed for this study (i.e., repeat visits), and per treating clinicians, patients with critical illness or acute distress, potential victims of sexual assault, and emotionally disturbed patients.
Trained interviewers assessed patients’ need for an interpreter, based on patient preference and ability to respond to initial demographic questions in English. Specifically, the interviewer assessed whether the patient had difficulty answering questions due to language barrier and whether an interpreter was used during the study interview. For study interviews conducted in English, the interviewer assessed for significant language barrier, by responding to the following question: “Did you perceive a significant communication barrier as a result of conducting interview in English? (e.g., excessive confusion compared to other interviews).” Additionally, the interviewer determined whether an interpreter was used during the ED clinical care, and if so, what type of interpreter was used. Possible interpreter categories were: friend of family member (stratified by age), MD or other health care provider, hospital interpreter services, or other hospital staff.
Statistical Analysis
All analyses were performed using STATA 9.0 (StataCorp, College Station, TX). Data are presented as proportions [with 95% confidence intervals (CI)], means [with standard deviation (SD)], and medians [with interquartile range (IQR)]. We used chi-square tests, Fishers exact tests, Student’s t-tests, and Wilcoxon rank sum tests, when appropriate, to evaluate differences between participants who experienced language barriers and those who did not. Two-tailed P <0.05 was considered statistically significant.
Results
Of 754 eligible patients, 530 (70%) agreed to participate. Demographic characteristics of the sample were: median age 45 years; 52% female; 64% white, 19% Hispanic, 15% black, 2% other; and 27% born outside of the US. The primary language was 78% English, 15% Spanish, and 7% other.
Among the 530 enrolled patients, the interview was conducted largely or entirely in English for most patients. Only 45 (9%; 95% CI, 6–11%) patients had their interview conducted in a language other than English. Additionally, among the 485 patients whose interview was conducted in English, a significant communication barrier was detected for 15 (3%) patients. Thus, during the ED stay, we estimated that 60 (11%; 95% CI, 9–14%) patients needed an interpreter.
Patients who needed an interpreter did not differ from those who did not need an interpreter with respect to age (48 vs. 42 years; P = 0.19) or sex (female, 52% vs. 52%; P = 0.92). Patients needing an interpreter were more likely to be Hispanic (85% vs. 12%; P <0.001) and to be born outside of the US (82% vs. 3%; P <0.001).
Most interviews (72%) requiring an interpreter were performed by bilingual study staff. Only 4% of study interviews, in which language barriers were detected, were interpreted by hospital interpreter services. Figure 1 shows what type of interpreter was used for clinical care of patients with language barriers during the ED stay. Interpretation was most often provided by a physician or other healthcare provider. Only 15% of patients with identified language barriers received interpretation by hospital interpreter services and 11% had no interpreter at all.
Fig. 1.
Interpreter for patients who needed language interpretation during the emergency department stay
Considerable site variation was observed. Across the four sites 1%, 7%, 12%, and 35% of patients needed an interpreter. The proportion of patients receiving an interpreter from hospital interpreter services also varied (100%, 14%, 35%, and 92%, respectively).
Discussion
As discussed in a recent editorial by former US Surgeon General, Dr. Richard Carmona, communication barriers faced by non-English speaking patients leads to disparities in access to preventive services and an increased reliance on emergency services [8]. Even one year after the enactment of state legislation that mandates the right to a medical interpreter, we found that utilization among ED patients with limited English remained low.
In our sample of Boston EDs, 11% of patients had significant identifiable language barriers, but only 15% of these patients received services of a professional medical interpreter. The assessment for use of interpreter and significant language barriers appeared more extensive by interviewers than by the judgment of treating clinicians. The utilization of interpreter services in ED-based studies prior to passage of the medical interpreter law was 12–15%, which suggests that access did not improve with enactment of this legislation [6, 7]. However, we did find clear variation by site in need and use of professional interpreters, which indicates that some hospitals may have adapted differently to the legal requirement.
The ability of providers to accurately ascertain information and patients to fully understand diagnosis, risks and benefits, and instructions is especially important in the ED environment, where patients are faced with complex medical decisions in the face of illness or injury. Indeed, Bernstein, et al. found that compared to non-English speaking patients who did not receive interpreter services, those who received interpreter services had higher rates of primary care follow-up, lower rates of return ED visits, and lower charges in the 30 days following the index ED visit [7]. These data suggest that the ability communicate instructions and transition to outpatient care is enhanced by use of professional interpreters.
Health care professionals, most often physicians, accounted for nearly half of personnel, who interpreted for the clinical visit. Although the ability to communicate with these patients was likely better than those who did not have any interpreter, Moreno et al. [9] found that one-quarter of designated dual-role staff interpreters had insufficient language skills. Since much of observed staff-performed interpretation was provided on an informal basis without any formal designation, we would expect that access to adequate language skills was even lower.
Additionally, for one-third of our patients with language barriers, friends or family members provided interpretation for the ED clinical care. Rosenberg et al. [10] found that professional interpreters performed better than family members at ensuring accurate information transfer and maintaining interview efficiency. These qualities are specifically important in the ED, where accurate and efficient communication is necessary to ensure timely diagnosis and appropriate treatment. Of particular concern is that one-third of friend/family interpreters were <18 years old. We would expect that communication via these children and adolescents would be further limited and lead, on average, to compromised quality and patient safety.
This study has several potential limitations. The sites were geographically limited, and our sample had lower racial/ethnic diversity compared to many urban EDs. However, we would anticipate even higher interpreter need in more diverse ED populations. The sampling strategy and the presence of non-respondents may bias observed estimates and associations. However, the potential for this bias is minimized by consecutive sampling during data collection days and the overall high response rate. Research personnel determined need for interpreter, but they were not formally trained in this assessment and other factors, such as patient mistrust, may have influenced the ability to assess true language barrier. Although presence of the study may have influenced use of interpreters for clinical care, most research interviews were performed by bilingual study staff, which limits potential for such bias. Finally, lack of professional interpreter use does not necessarily mean that it was not offered. Patients may have preferred to use friends or family members as interpreters.
Conclusions
In four Boston EDs, we found that 11% of patients had language barriers that required interpreters, but only 15% of these patients were assisted by professional medical interpreters. One year after passage of legislation mandating access, use of professional medical interpreters remained inadequate. The impact of these language barriers on ED care merits further investigation and greater emphasis in professional education, interpreter access, and quality improvement programs.
Acknowledgments
Dr. Camargo is supported by Grant U01 AI-67693 from the National Institutes of Health (Bethesda, MD).
Contributor Information
Adit A. Ginde, Department of Emergency Medicine, University of Colorado Denver School of Medicine, Aurora, CO, USA
Sunday Clark, Division of General Internal Medicine, University of Pittsburgh, Pittsburgh, PA, USA.
Carlos A. Camargo, Jr., Email: ccamargo@partners.org, Department of Emergency Medicine, EMNet Coordinating Center, Massachusetts General Hospital, Harvard Medical School, 326 Cambridge Street, Suite 410, Boston, MA 02114, USA.
References
- 1.Massachusetts General Laws Chapter 111, Sect. 25 J and Chapter 123, Sect. 23 A. [Accessed February 26, 2008];An act requiring competent interpreter services in the delivery of certain acute health care services. Available at: http://www.mass.gov/legis/laws/seslaw00/sl000066.htm.
- 2.Sarver J, Baker DW. Effect of language barriers on follow-up appointments after an emergency department visit. J Gen Intern Med. 2000;15:256–64. doi: 10.1111/j.1525-1497.2000.06469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jacobs EA, Lauderdale DS, Meltzer D, Shorey JM, Levinson W, Thisted RA. Impact of interpreter services on delivery of health care to limited-English-proficient patients. J Gen Intern Med. 2001;16:493–5. doi: 10.1046/j.1525-1497.2001.016007468.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rivadeneyra R, Elderkin-Thompson V, Silver RC, Waitzkin H. Patient centeredness in medical encounters requiring an interpreter. Am J Med. 2000;108:470–4. doi: 10.1016/S0002-9343(99) 00445-3. [DOI] [PubMed] [Google Scholar]
- 5.Ngo-Metzger Q, Sorkin DH, Phillips RS. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med. 2007;22(Suppl 2):324–30. doi: 10.1007/s11606-007-0340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baker DW, Parker RM, Williams MV, Coates WC, Pitkin K. Use and effectiveness of interpreters in an emergency department. J Am Med Assoc. 1996;275:783–8. doi: 10.1001/jama.275.10.783. [DOI] [PubMed] [Google Scholar]
- 7.Bernstein J, Bernstein E, Dave A, Hardt E, James T, Linden J, et al. Trained medical interpreters in the emergency department: effects on services, subsequent charges, and follow-up. J Immigr Health. 2002;4:171–6. doi: 10.1023/A:1020125425820. [DOI] [PubMed] [Google Scholar]
- 8.Carmona RH. Improving language access: a personal and national agenda. J Gen Intern Med. 2007;22(Suppl 2):277–8. doi: 10.1007/s11606-007-0376-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moreno MR, Otero-Sabogal R, Newman J. Assessing dual-role staff-interpreter linguistic competency in an integrated healthcare system. J Gen Intern Med. 2007;22(Suppl 2):277–8. doi: 10.1007/ s11606-007-0344-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenberg E, Seller R, Leanza Y. Through interpreters’ eyes: comparing roles of professional and family interpreters. Patient Educ Couns. 2008;80:87–93. doi: 10.1016/j.pec.2007.09.015. [DOI] [PubMed] [Google Scholar]