Abstract
Successful social functioning requires adaptive forms of emotion awareness and regulation. However, despite well-documented deficits in social functioning in individuals with schizophrenia, little is known about emotion awareness and regulation in this population. Therefore, we compared emotion awareness and regulation in individuals with schizophrenia and healthy controls, and then, within the schizophrenia group, we examined their impact on social functioning. Forty-four individuals with schizophrenia and 20 healthy controls completed measures of emotion awareness, emotion regulation, and social functioning, in addition to control measures, including neurocognitive functioning. Compared to controls, individuals with schizophrenia displayed significant deficits describing and identifying their emotions and used significantly less reappraisal and more suppression to regulate their emotions. Among the schizophrenia group, better social functioning was associated with the ability to identify, and in particular to describe emotions, better emotion management, as well as greater use of reappraisal and less use of suppression. A hierarchical multiple regression analysis indicated that, after controlling for age and neurocognition, difficulties describing feelings accounted for 35% of the social functioning variance. The present study highlights the importance of emotion awareness and regulation in schizophrenia, pointing to their substantial influence on social functioning above and beyond the impact of neurocognitive functioning.
Keywords: Social Cognition, Emotion Processing, Alexithymia, Neurocognition, Negative Symptoms, Suppression, Reappraisal
1. Introduction
Schizophrenia is commonly associated with decreased levels of daily functioning and increased levels of disability (Brekke et al., 2009a). Although the population incidence of schizophrenia is about 1%, it is the 9th leading cause of disability worldwide (Lopez et al., 2006), thus representing a serious public health concern (Green, 2007). Previous attempts to identify the determinants of daily dysfunction and disability in schizophrenia have focused primarily on neurocognitive deficits (Green, 2007; Nuechterlein et al., 2011). Overall, these studies have shown that neurocognition typically explains 20–40% of the functional outcome variance, leaving a substantial proportion of the variance unaccounted (Couture et al., 2006).
In recent years, social cognition has emerged as an important area of research in schizophrenia (Green and Leitman, 2008), in part due to a growing recognition of its critical impact on functional outcomes (Couture et al., 2006). A recent meta-analysis of 52 studies found that social cognition was more strongly associated with community functioning than neurocognition (Fett et al., 2011). Consistent with this emerging appreciation, the National Institute of Mental Health designated social cognition as a priority research area in schizophrenia, specifying five primary domains of research including theory of mind, social perception, social knowledge, attribution bias, and emotion processing (Green et al., 2005; Green and Leitman, 2008). While a number of domains, such as theory of mind, and perceiving other people's emotions have attracted much interest, other components received less attention. In particular, the way in which individuals with schizophrenia process and regulate their own emotions and their impact on social functioning has received relatively little consideration. This scant attention stands in sharp contrast to an extensive basic affective science literature that indicates that successful social functioning is contingent on effective emotion awareness and regulation. This discrepancy between the clinical and basic affective science literatures has been identified as the single most problematic obstacle to progress in social cognition research in schizophrenia (Green and Leitman, 2008). To address this discrepancy, in the next sections we review the basic affective science literature on emotion processing, in particular studies of emotion awareness and regulation, along with the schizophrenia clinical research literature.
1.1. Emotion Awareness and Regulation: Insights from Basic Affective Science
Emotion is generally viewed as a relatively brief form of affect (Ekman, 1992) that arises when external or internal stimuli signal to the individual that something important may be at stake. Emotions are important for social functioning as they provide information about the significance of current social situations, as well as guide potential actions to be taken to address such situations (Barrett et al., 2001). In particular, negative emotional experiences have great informational value in signaling the need to change or adjust one's current state or activity, with failure to respond resulting in potential harm. Because different emotions may call for the use of distinct response strategies, lack of awareness or reduced clarity of experienced feelings may make it difficult for individuals to select appropriate response strategies for dealing effectively with the social situation at hand (Barrett et al., 2001), potentially resulting in social dysfunction. Thus, successful adaptation to ever-changing social environments is contingent upon knowledge of one's own emotions, which has been termed “emotion awareness” (Taylor et al., 1997). Such awareness encompasses the capacity to be attentive to one's own emotions, the ability to distinguish between distinct emotions, and the use of discrete verbal labels to describe them, all of which are important for adaptive social functioning.
To describe individuals with low levels of emotion awareness, Sifneos (1996) introduced the term alexithymia. The term now refers to a multi-dimensional subclinical phenomenon that encompasses difficulties identifying and describing feelings, difficulties in distinguishing feelings from the sensations of emotional arousal, impaired symbolization, and a tendency to focus on external events (Taylor et al., 1991). Approximately 10% of the general population is characterized by poor awareness of emotional states (Linden et al., 1994; Salminen et al., 1999). Limited emotion awareness, in particular difficulties in identifying and describing feelings, has been linked to poor social functioning and quality of life (Salminen et al., 1999; Kokkonen et al., 2001). Specifically, difficulties identifying and describing feelings were associated with reduced positive affect, increased negative affect, depression, anxiety, and poor quality of life (Henry et al., 2006). Similarly, individuals with difficulties identifying and describing feelings had significantly lower levels of social contacts, fewer acquaintances, and were more often unmarried (Kauhanen et al., 1993).
Although emotions often seem to play out entirely beyond one's control, individuals in fact can exert considerable influence over the course of their emotions. Emotion regulation has been defined as the processes that are engaged in order to influence which emotions people have, when they have them, and how these emotions are experienced or expressed (Gross, 2007). A number of emotion regulation strategies have been identified - Gross (1998) has described a process model of emotion regulation that distinguishes between antecedent- and response-focused strategies, with the former preceding the full emotional response, and the latter being initiated once the response is already under way.
Previous reports indicate that effective emotion regulation has been linked with enhanced psychosocial functioning (Gross and Muñoz, 1995). In particular, the use of antecedent-focused strategies, such as reappraisal, has been associated with lower negative emotional experience, enhanced social functioning and quality of life, greater expression of positive emotion, increased well-being, as well as better academic performance (John and Gross, 2004; Brackett and Salovey, 2006). In contrast, response-focused strategies such as suppression have been linked to greater expression of negative emotion, poorer social functioning, lower social support, satisfaction and sense of closeness to others, as well as decreased well-being (Gross, 1998; Gross and John, 2003; van't Wout et al., 2010). Consistent with these findings, clinical populations have been found to use significantly less reappraisal and more suppression (Campbell-Sills et al., 2006; Joormann and Gotlib, 2010). The positive influence of reappraisal on social functioning may be attributed to antecedent-focused strategies manipulating information prior to the elicitation of full emotional reaction, thus reducing negative emotions. In contrast, suppression typically influences an already initiated emotional reaction (Gross, 1998).
1.2. Emotion Awareness and Regulation: Empirical Findings in Individuals with Schizophrenia
Difficulties in emotion processing are considered a core component of schizophrenia and have been linked to functional disability (Kee et al., 2003; Baslet et al., 2009; Kring and Caponigro, 2010). The bulk of emotion processing studies in schizophrenia to date have focused on perception and identification of affective facial expressions of others (Laroi et al., 2010). In contrast, few studies concentrated on emotion awareness. van't Wout and colleagues (2007) found that individuals with schizophrenia reported significantly more difficulties identifying and describing feelings compared to their not-ill siblings, as well as healthy controls. Similarly, Yu et al. (2011) reported significant differences between individuals with paranoid schizophrenia and healthy controls. These findings are consistent with previous reports of substantial emotion awareness deficits in individuals with schizophrenia (Stanghellini and Ricca, 1995; Cedro et al., 2001), although they are not universal (Henry et al., 2010). Such difficulties appear to predate the onset of psychosis, as they have been identified in individuals at clinical high risk for psychosis (Kimhy and Corcoran, 2008; van Rijn et al., 2011). Conflicting with these findings is a substantial literature indicating that individuals with schizophrenia display no in-the-moment emotion awareness deficits. Kring and Moran (2008) reviewed 44 studies in which a plurality reported no in-the-moment emotion experience differences from healthy controls. However, the conclusions of this review are limited on two points: 1) in virtually all of the studies, the participants were required to respond to the stimuli using semi-structured questions in which a limited predetermined range of emotional responses were listed (i.e., happy, sad, anxious). Such semi-structured questions represent an easier task than open-ended questions which require the participant to come up independently with an appropriate label to describe their current emotional state; and 2) such tasks may also have poor ecological validity as individuals typically do not have access to such predetermined list of responses during the course of daily social interactions.
Studies of emotion regulation in schizophrenia have utilized measures assessing both global and strategy-specific emotion regulation indices. For global measures, the Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT) has been one of the most commonly used instruments. Previous studies using the MSCEIT have reported significant deficits in emotion regulation in individuals with schizophrenia compared to healthy controls (Nuechterlein and Green, 2006), although association with changes in social functioning following cognitive enhancement therapy were modest (Eack et al., 2010). For specific emotion regulation strategies, van der Meer and colleagues (2009) found that individuals with schizophrenia were significantly more likely than healthy controls to suppress their emotions, even after accounting for level of depression. Other studies provide additional indirect support - for example, Jansen et al. (2000) found individuals with schizophrenia scored significantly higher on use of escape, avoidance, and passive coping strategies compared to healthy controls. However, these findings are not universal – a number of studies reported no differences in use of reappraisal and suppression between individuals with schizophrenia and healthy participants (Henry et al., 2008; Badcock et al., 2011; Perry et al., 2011). Regarding relationship with social functioning, Henry et al. (2008) reported modest correlations with use of reappraisal, but not suppression among individuals with schizophrenia. In contrast, Perry et al. (2011) found greater use of suppression was associated with poorer social functioning, while reappraisal was not significantly related to social functioning.
While a growing clinical literature suggests significant deficits in emotion awareness and regulation in individuals with schizophrenia, a number of important gaps in the literature remain unaddressed. First, there remain inconsistencies in the clinical literature regarding the extent to which individuals with schizophrenia display deficits in emotion awareness and in particular emotion regulation compared to healthy participants. Second, the putative associations of emotion awareness, emotion regulation, and social functioning in individuals with schizophrenia have not been investigated, and it is not known whether difficulties with emotion awareness and regulation would predict social functioning in individuals with schizophrenia above and beyond previously identified neurocognitive difficulties.
1.3. The Present Study
Given the evidence of substantial social dysfunction in individuals with schizophrenia, the centrality of emotion awareness and emotion regulation to social functioning, and the dearth of studies exploring their relationship, our aims are: 1) to extend findings from previous studies indicating group differences between individuals with schizophrenia and healthy controls in emotion awareness, emotion regulation, and social functioning; 2) to examine the links between emotion awareness, emotion regulation, and social functioning in individuals with schizophrenia; and 3) to assess whether emotion awareness and emotion regulation would predict social functioning in individuals with schizophrenia, controlling for covariates and previously identified predictors.
2. Method
2.1. Participants
Forty-four individuals with schizophrenia and 20 healthy controls were recruited as part of studies of emotion and autonomic regulation during recovery from psychosis conducted at the New York State Psychiatric Institute (NYSPI). The studies were approved by the NYSPI's Institutional Review Board and all subjects provided written informed consent. Individuals with schizophrenia were recruited from inpatients and outpatients treated at the Columbia University Medical Center, referrals from clinicians in the community, and online advertisements. Twenty healthy participants were recruited via advertisements posted at the Columbia University Medical Center campus. Inclusion and exclusion criteria for all participants included: males or females between the ages of 18–50, English speaking, have not used street drugs within the past 4 weeks (confirmed using urine toxicology test), no history of neurological problems or loss of consciousness (>1 hour), no history of serious cardiopulmonary problems or very high blood pressure, no diagnosis of mental retardation, and no recent history of serious suicidal/aggressive behavior. For the patient group, the inclusion criteria also included a DSM-IV diagnosis of schizophrenia spectrum disorder, presence of active psychosis (ratings of ≥3 for any psychosis item on the SAPS), and capacity to give informed consent. For the healthy controls group, exclusion criteria included a history of psychosis, a diagnosis of any DSM-IV Axis II Cluster A personality disorder, a first degree family member with history of psychosis, and being adopted. In the schizophrenia group, 35 participants had a DSM-IV diagnosis of Schizophrenia, 3 had Schizoaffective Disorder, 3 Schizophreniform Disorder, and 3 Psychosis NOS. The average dosage of antipsychotic medication prescribed (as indexed by chlorpromazine equivalence) was 239.97 (SD=242.79).
2.2. Procedure
Participants were referred to the study from clinics associated with NYSPI, as well as clinicians in the community. After an initial phone screen, participants signed the informed consent forms and completed the assessment of inclusion/exclusion criteria. Four participants' data were excluded – 3 due to positive toxicology results, and one due to disorganization). Participants typically completed all emotion processing, social functioning, and clinical ratings within 1–2 weeks of study entry. Establishment of research diagnoses and assessment of neurocognition was completed within 1–2 months from study entry. Diagnoses were determined using the Diagnostic Interview for Genetic Studies (DIGS), a semi-structured diagnostic interview and medical records review that is used to gather diagnostic and course of illness information for mood, psychotic, and substance use DSM-IV disorders. The DIGS was administered by clinical research interviewers at the Masters' level or above. A team of research clinical psychologists and psychiatrists made consensus diagnoses based on information collected via the DIGS. Positive and negative symptom were characterized using the SAPS and SANS.
2.3. Measures
Measures were obtained to assess our three primary domains of interest, including: (1) emotion awareness, (2) emotion regulation, and (3) social functioning. In addition, we assessed important control measures including neurocognitive functioning, medication and demographic factors. We also assessed self-reflectiveness to ascertain whether the results may reflect difficulties in emotional awareness, or a more general deficit in self-reflection.
Emotion Awareness
Identification and Description of Feelings - was assessed using the Toronto Alexithymia Scale (TAS-20; Bagby et al., 1994), a 20-item self-report questionnaire, with higher score indicating poorer functioning. The TAS-20 has three subscales: Difficulty Identifying Feelings (DIF; 7 items), Difficulty Describing Feelings (DDF; 5 items), and Externally-Oriented Thinking (EOT; 8 items). Participants are asked to indicate on a 5-point scale (from 1=“Strongly Disagree” to 5=“Strongly Agree”) to what extent they agreed with each statement. The TAS-20 has a solid internal consistency (≥0.80) with the DIF and DDF subscales demonstrating good reliability (r=0.79–0.83). However, we elected to exclude the EOT subscale due to questionable reliability (Kooiman et al., 2002).
Emotion Regulation
Emotion regulation was evaluated using both global and strategy-specific measures:
Emotion Management
We assessed global emotion management using the Emotion Management Task (EMT) of the Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT; Section D; Nuechterlein and Green, 2006). The task is an ability measure in which the respondent rates the effectiveness of potential actions in managing emotions in various situations depicted in vignettes. Respondents are asked to indicate the effectiveness of each action (from 1=“very ineffective” to 5=“very effective”). The MSCEIT has been shown to be a reliable and valid measure of emotion management among individuals with schizophrenia (r=0.73; ICC=0.73; n=167; Nuechterlein and Green, 2006). The MSCEIT has been selected as it has been used in previous studies of individuals with schizophrenia, thus, allowing comparison across studies.
Suppression and Reappraisal
Use of specific emotion regulation strategies was assessed using the Emotion Regulation Questionnaire (ERQ; Gross and John, 2003). The 10-item self-report questionnaire contains six items assessing reappraisal and four assessing suppression. Participants are asked to indicate on a 7-point scale (from 1=“strongly disagree” to 7=“strongly agree”) to what extent they agree with each statement, with higher scores reflecting stronger endorsement of using the strategy. The ERQ has been shown to be a reliable and valid measure of emotion regulation, with an average alpha reliability of 0.79 for reappraisal and 0.73 for suppression. Test–retest correlations across three months were .69 for both scales (Gross and John, 2003).
Social Functioning
Social Functioning was assessed using the Provision of Social Relations Scale (PSRS; Turner et al., 1983), a 15-item scale measuring social relationships with family and friends. Items are scored on a 5-point scale (from 1=“Very much like me” to 5=“Not at all like me”) with higher scores indicating lower support and relationship quality. The PSRS was found to have alpha coefficients of 0.85, 0.80, and 0.78 among individuals with schizophrenia, bipolar disorder and healthy controls, respectively (Horan et al., 2007), as well as solid test-retest reliability of 0.75–0.87 (Huprich et al., 2002).
Control Measures
Demographic and Clinical Information
was collected including age, sex, primary language, reading ability, and use of antipsychotic medication (as indexed by chlorpromazine equivalence).
Neurocognitive Functioning
was assessed using the MATRICS Consensus Cognitive Battery (MCCB) which includes the following domains: speed of processing, attention/vigilance, working memory, verbal learning, visual learning, as well as reasoning and problem solving (Nuechterlein and Green, 2006)
Self-Reflection
was assessed using the Self-Reflection index of the Beck Cognitive Insight Scale (BCIS-SR). The BCIS is a 15-item self-report questionnaire comprised of two subscales: Self-Reflectiveness (SR) and Self-Certainty. The BCIS has demonstrated solid internal consistency with Cronbach's alpha of 0.7 for the SR index (Riggs et al., 2010).
2.4. Data Analyses
For each analysis, we first evaluated the emotion variables of interest alone, followed by analyses controlling for covariates. Group differences in emotion awareness, emotion regulation and social functioning were assessed using 2-tailed t-tests with significance levels set at p<0.05, followed by ANCOVAs controlling for age. Associations among emotion awareness, emotion regulation, and social functioning were examined first using Pearson correlations, followed by partial correlations controlling for age. Finally, assessment of whether emotion awareness and regulation would predict social functioning was tested using hierarchical regression analysis, with social functioning entered as a dependent variable, the control variables and previously identified predictors entered in block 1, the emotion awareness variables entered in block 2, and emotion regulation variables entered in block 3.
3. Results
The sample's demographic and clinical characteristics are presented in Table 1. There were no significant differences between individuals with schizophrenia and healthy controls with regard to sex, ethnicity, reading ability, and the proportion of speakers of English as a second language. However, the healthy controls were significantly younger.
Table 1.
Demographic and Clinical Information
| Schizophrenia | Healthy Controls | t / X2 | p | |
|---|---|---|---|---|
|
| ||||
| Age | 30.33 (8.08) | 24.20 (4.62) | 3.16 | <.01 |
|
| ||||
| Sex (% female) | 36% | 50% | 1.06 | .30 |
|
| ||||
| Ethnicity (% Hispanic) | 32% | 20% | .95 | .33 |
|
| ||||
| Race: | ||||
| Asian | 7 (16%) | 3 (15%) | ||
| Black/African-American | 3 (7%) | 2 (10%) | ||
| White | 24 (54%) | 14 (70%) | ||
| More than one race | 10 (23%) | 1 (5%) | ||
|
| ||||
| English is Second Language (% yes) | 34% | 35% | 2.86 | .24 |
|
| ||||
| Reading Ability (WTAR Total Score) | 40.05 (8.43) | 43.85 (6.78) | 1.77 | .08 |
|
| ||||
| Self-Reflectiveness (BCIS-SR) | 15.21 (4.90) | 14.19 (4.42) | .82 | .41 |
| Schizophrenia | Mean | SD |
|---|---|---|
|
| ||
| Positive Symptoms (SAPS Global Ratings) | ||
| Hallucinations | 3.36 | 1.83 |
| Delusions | 3.26 | 1.37 |
| Bizarre Behavior | .69 | 1.08 |
| Positive Formal Thought Disorder | 1.28 | 1.36 |
| Total SAPS | 8.59 | 3.69 |
|
| ||
| Negative Symptoms (SANS Global Ratings) | ||
| Affective Flattening | 2.21 | 1.34 |
| Alogia | 1.21 | 1.48 |
| Avolition-Apathy | 2.29 | 1.50 |
| Anhedonia-Asociality | 2.74 | 1.48 |
| Attention | 1.68 | 1.63 |
| Total SANS | 10.10 | 5.02 |
|
| ||
| Neurocognition (Standardized MCCB Domain Scores) | ||
| Speed of Processing | 33.41 | 12.92 |
| Attention/Vigilance | 43.74 | 9.79 |
| Working Memory | 41.06 | 10.94 |
| Verbal Learning | 38.03 | 10.21 |
| Visual Learning | 38.75 | 9.28 |
| Reasoning & Problem Solving | 37.61 | 11.10 |
| Social Cognition | 37.27 | 13.89 |
Note: n=64 (Schizophrenia=44, Healthy Controls=20); WTAR – Wechsler Test of Adult Reading; BCIS – Beck Cognitive Insight Scale; SAPS – Scale for Assessment of Positive Symptoms; SANS - Scale for Assessment of Negative Symptoms; MCCB - MATRICS Consensus Cognitive Battery.
3.1. Emotion Awareness and Regulation in Individuals with Schizophrenia Versus Healthy Controls
Our first aim was to evaluate whether individuals with schizophrenia differ from healthy individuals in their ability to identify and describe emotions, as well as their use of emotion regulation strategies. These data are presented in Table 2. Individuals with schizophrenia reported significantly more difficulties identifying and describing emotions than healthy controls. They also reported using higher levels of suppression and lower levels of reappraisal, compared to healthy controls, as well as demonstrated lower ability to effectively manage emotions, suggesting a less adaptive emotion regulation profile. Consistent with previous reports, individuals with schizophrenia also displayed significantly lower social functioning. These differences remain significant after controlling for the impact of age. Cohen's d calculations indicated large effect sizes for the differences between the groups. In contrast, there were no significant group differences in self-reflectiveness (BCIS-SR; t=0.82, p=0.41), which is also consistent with our previous report (Kimhy et al., in press). Likewise, in the schizophrenia group, there was no significant association between self-reflectiveness and emotion awareness and regulation (r=0.09, p=0.55 and r=−0.03, p=0.84, respectively).
Table 2.
Emotion Awareness, Emotion Regulation, and Social Functioning in Individuals with Schizophrenia and Healthy Controls
| Schizo. | Healthy Controls | t-test | ANCOVA* | Cohen's | ||||
|---|---|---|---|---|---|---|---|---|
| t | P | F(1, 62) | P | d | ||||
| Social Functioning | Provision of Social Relations Scale (PSRS) | 37.31 (12.10) | 20.94 (3.54) | 7.96 | <.001 | 23.42 | <.001 | 1.83 |
| Emotion Regulation | Reappraisal (ERQ) | 26.77 (8.23) | 31.35 (6.87) | 2.16 | .03 | 5.27 | .02 | .60 |
| Suppression (ERQ) | 16.36 (5.67) | 12.55 (5.53) | 2.51 | .01 | 5.42 | .02 | .68 | |
| Emotion Management Task (MSCEIT) | 88.34 (12.59) | 101.80 (12.70) | 3.22 | <.001 | 8.29 | <.01 | 1.06 | |
| Emotion Awareness | Difficulty Identifying Feelings (TAS-20) | 19.67 (7.12) | 11.29 (4.48) | 4.49 | <.001 | 17.64 | <.001 | 1.41 |
| Difficulty Describing Feelings (TAS-20) | 14.67 (4.17) | 9.47 (3.10) | 4.63 | <.001 | 19.88 | <.001 | 1.41 | |
Note: PSRS - Provision of Social Relations Scale; Higher scores on the TAS-20 and PSRS indicate lower functioning; TAS-20 - Toronto Alexithymia Scale; ERQ – Emotion Regulation Questionnaire; MSCEIT - Mayer-Salovey-Caruso Emotional Intelligence Test;
- controlling for age.
3.2. Emotion Awareness, Emotion Regulation, and Social Functioning in Individuals with Schizophrenia
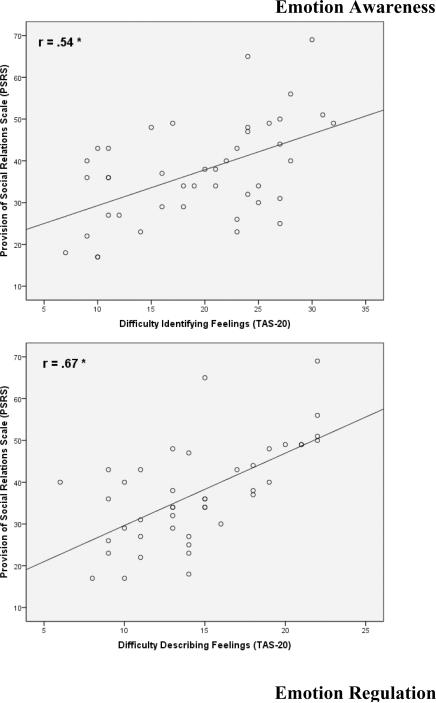
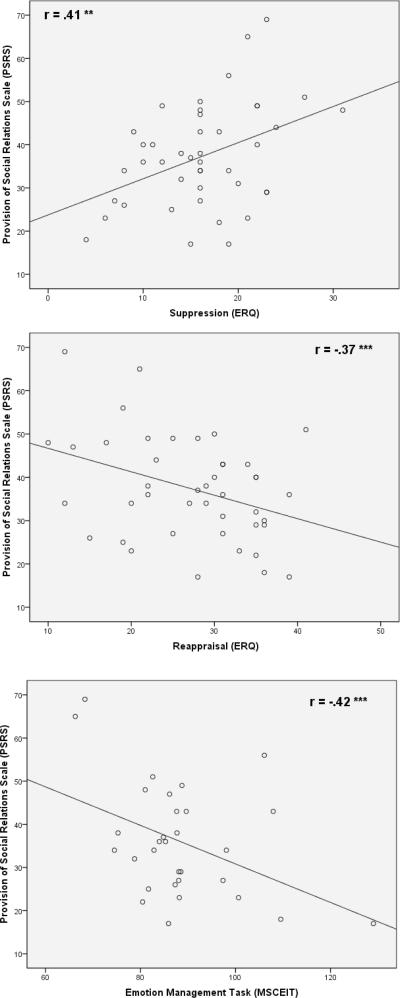
Our second aim was to evaluate the associations between the abilities to identify and describe feelings, use of emotion regulation strategies, and social functioning in individuals with schizophrenia. These data are presented in Table 3. Enhanced social functioning was associated with the ability to identify, and in particular to describe emotions (Figure 1). Enhanced social functioning was also associated with greater reappraisal use and lesser suppression use, as well as overall better emotion management. These associations remain largely comparable after controlling for the impact of age and neurocognitive functioning. Interestingly, difficulties identifying and describing feelings were associated with use of suppression, but not reappraisal or the EMT. In contrast, the association between the EMT and social functioning became non-significant after controlling for age and neurocognitive functioning.
Table 3.
Zero-Order and Partial Correlations of Social Functioning with Emotion Awareness and Emotion Regulation in Individuals with Schizophrenia
| Provision of Social Relations Scale (PSRS) | Reappraisal (ERQ) | Suppression (ERQ) | Difficulty Identifying Feelings (TAS-20) | Difficulty Describing Feelings (TAS-20) | Emotion Manag. Task (MSCEIT) | |
|---|---|---|---|---|---|---|
| Provision of Social Relations Scale (PSRS) | --- | *−.37 | **.41 | **.54 | **.67 | *−.42 |
| Reappraisal (ERQ) | .44*- | --- | −.14 | −.29 | −.23 | .19 |
| Suppression (ERQ) | *.38 | −.13 | --- | *.37 | **.48 | −.28 |
| Difficulty Identifying Feelings (TAS-20) | .43* | −.29 | *.37 | --- | **.61 | −.34 |
| Difficulty Describing Feelings (TAS-20) | .50** | −.26 | **.47 | **.53 | --- | −.25 |
| Emotion Manag. Task (MSCEIT) | .20- | .18 | −.26 | −.34 | −.08 | --- |
Note:
< .05,
< .01;
Zero-order correlations are presented above the diagonal. Partial correlations are presented below the diagonal (controlling for age, depression and MATRICS neurocognitive domain indices including speed of processing, attention/ vigilance, working memory, verbal learning, visual learning, and reasoning & problem solving); PSRS - Provision of Social Relations Scale; TAS-20 - Toronto Alexithymia Scale; ERQ – Emotion Regulation Questionnaire; MSCEIT - Mayer-Salovey-Caruso Emotional Intelligence Test.
Figure 1.
The Association of Emotion Awareness and Regulation with Social Functioning in Individuals with Schizophrenia
* <.001; ** <.01; *** <.05;
Note: PSRS - Provision of Social Relations Scale; TAS-20 - Toronto Alexithymia Scale; ERQ - Emotion Regulation Questionnaire; MSCEIT - Mayer-Salovey-Caruso Emotional Intelligence Test.
3.3. Emotion Awareness and Emotion Regulation as Predictors of Social Functioning
Our third aim was to assess whether emotion awareness and emotion regulation would predict social functioning in individuals with schizophrenia. As a first step, we evaluated the roles of demographic and other factors including sex, age, race, ethnicity, reading ability, language (English as second language), self-reflectiveness and use of antipsychotic medication (chlorpromazine equivalence). Only age was associated with social functioning (r=0.27, p=0.04 and r=0.38, p=0.02, respectively). Next, a hierarchical multiple regression analysis was conducted with social functioning entered as a dependent variable; age, and neurocognitive MCCB domain scores entered in block 1; the emotion awareness variables (TAS) entered in block 2; and the emotion regulation variables (ERQ, EMT) entered in block 3. We elected not to include negative symptoms as independent predictors in our analysis given such symptoms represent to large degree measures of emotion and social (dys) function, just with different labels. This decision was informed by previous reports indicating high correlations between negative symptoms and social functioning among individuals with schizophrenia (r=0.60–0.89; n=295; Hunter and Barry, 2011), along with post-hoc findings from our sample (i.e., correlation between SANS Anhedonia-Asociality and social functioning; r=0.59, p<.001).
The regression analysis indicates that age and neurocognitive functioning entered in block 1 as control variables accounted for 14% of the variance in social functioning, but failed to reach significance. The block of emotion awareness variables (TAS) accounted for 35% of the explained variance (F9,30=3.12, p=0.009). Within the emotion awareness predictors, difficulties describing feelings contributed uniquely to the model's validity (β=0.46, t=2.15, p=0.04). The addition of emotion regulation measures in block 3 (ERQ, EMT) to the equation yielded a validity increment of 10%, but was not significant. Overall, the model (F12,27=3.12, p=0.007) accounted for 66% of the social functioning variance.
4. Discussion
The present study is the first to examine emotion awareness, emotion regulation, and social functioning in schizophrenia. Our findings indicate that compared to healthy individuals, people with schizophrenia display significantly lower emotion awareness as indexed by having more difficulties identifying and describing their own feelings. Likewise, individuals with schizophrenia display deficits in emotion regulation as characterized by a significantly higher use of suppression and lower use of reappraisal. Most importantly, our findings indicate that among individuals with schizophrenia, difficulties with emotion awareness are strongly predictive of poorer social functioning after controlling for age and neurocognitive functioning.
4.1. Emotion Awareness and Regulation in Individuals with Schizophrenia
Our findings regarding decreased emotion awareness in individuals with schizophrenia are consistent with previous reports (Stanghellini and Ricca, 1995; Cedro et al., 2001; van't Wout et al., 2010; Yu et al., 2011). An exception to this trend is the finding by Henry and colleagues who reported no differences between patients and healthy controls (Henry et al., 2010). Similarly, our findings regarding emotion regulation are consistent with some (van der Meer et al., 2009), but not all previous reports (Henry et al., 2008; Badcock et al., 2011; Perry et al., 2011).
The incongruities among the various findings invite speculation regarding potential explanations for these discrepancies. One potential explanation may be related to different proportions of individuals with a diagnosis of schizoaffective disorder in the various studies. Emotion awareness studies with relatively higher proportions (28%) did not report differences in emotion awareness (Henry et al., 2010). In contrast, studies that reported significant differences had far lower schizoaffective disorder rates (7% in our sample; 2% in van't Wout et al., 2010; and 0% in Yu et al., 2011). Likewise, in the emotion regulation studies, samples with higher proportion of schizoaffective disorder (22% in Henry et al., 2008; 39% in Perry et al., 2011; and 16% in Badcock et al., 2011 - personal communication from Drs. Johanna Badcock and Georgie Paulik) found no differences from healthy controls. Whereas, significant differences were reported in studies with lower rates - 7% in our sample and none in van der Meer's sample (van der Meer et al., 2009). These differences are consistent with previous reports of schizoaffective disorder being associated with enhanced social cognition and functioning compared to schizophrenia (Fiszdon et al., 2007). Taken together, these findings suggest that emotion awareness and regulation may pose particular difficulties for individuals with schizophrenia, but perhaps not for those with schizoaffective disorder.
4.2. Emotion Awareness, Emotion Regulation, and Social Functioning in Individuals with Schizophrenia
The most important finding of the present study is that emotion awareness, and in particular difficulties describing feelings, predicted 35% of the variance in social functioning in individuals with schizophrenia, after controlling for age and neurocognition. The overall model, including emotion regulation, neurocognition and age predicted 58% of the variance, a substantially larger variance than results reported in studies that focused solely on neurocognitive predictors (Bell et al., 2010; Mancuso et al., 2011; Shamsi et al., 2011). Thus, our results build on previous findings (Fett et al., 2011) by providing a novel contribution to the understanding of social cognition, highlighting the central role emotion awareness deficits play in determining social functioning in individuals with schizophrenia.
Our use of a self-report measure to index social functioning may potentially introduce response biases. However, while social functioning measures that involve behavioral observations are often considered to be the most phenomenologically robust, there is a growing recognition that such measures fail to address some crucial aspects of functional outcome (Bromley and Brekke, 2010). In particular, behavioral measures have been criticized for being discordant with schizophrenia patients' priorities regarding recovery (Bromley and Brekke, 2010). Specifically, Brekke and colleagues reported that individuals with schizophrenia selected improvement in subjective experiences, including quality of relationships, as far more important to them than enhancement in functional skills or reduction in clinical symptoms (Brekke and Long, 2000). These findings are consistent with the values espoused by the “recovery movement”, as well as reports that subjective experiences constitute a unique domain of recovery among individuals with schizophrenia that is distinct from clinical or functional improvements (Brekke et al., 2009b; Bromley and Brekke, 2010).
Our findings are in agreement with the extensive basic affective science literature that points to strong links between emotion awareness and regulation deficits and social dysfunction. The results invite speculation about the potential mechanisms linking emotion awareness, emotion regulation and social dysfunction in schizophrenia. The findings of significant associations between poor emotion awareness and use of suppression, but not reappraisal, are consistent with previous reports among individuals with schizophrenia (van der Meer et al., 2009) and other clinical populations (Taylor et al., 1997). Gross and John (2003) defined antecedent-focused emotion regulation strategies, such as reappraisal, as “things we do before the emotion response tendencies have become fully activated and have changed our behavior and peripheral physiological responding” (p. 348; Gross and John, 2003). Accordingly, the limited use of reappraisal among individuals with schizophrenia may potentially be related to difficulties identifying and describing feelings. Such difficulties may prevent the development of timely emotion awareness, or at least slow them down, resulting in full activation of behavioral and physiological responses, making the use of antecedent-focused emotion regulation strategies (such as reappraisal) less likely. Consequently, individuals with schizophrenia may increasingly have to rely on response-focused strategies (suppression) to regulate already-generated emotions, leading to less effective social functioning.
4.3. Clinical Implications
As deficits in both emotion awareness and emotion regulation have been linked to poor social functioning, our results invite speculation about the potential to improve social dysfunction by ameliorating such deficits. Increasing patients' abilities to identify and describe emotions is an important component of many contemporary psychotherapy approaches including ACT, Mindfulness-Based CBT, DBT, as well as Emotion-Focused Therapy. For example, Greenberg and colleagues considered improvement of emotion awareness and regulation as central to recovery, pointing out that the first goal of treatment “is for clients to become aware of their primary emotions … primary emotions need to be accessed in awareness for their adaptive information and capacity to organize action” (p. 621; Greenberg and Pascual-Leone, 2006). Similarly, Linehan indicated, “the first step in regulating emotions is learning to identify and label current emotions” (p. 84; Linehan, 1993). A number of studies reported significant reductions in alexithymia following treatments in individuals with panic disorder and social phobia (Fukunishi et al., 1997), as well as depression (Honkalampi et al., 2000), suggesting potential feasibility and efficacy of improving poor emotion awareness.
The longitudinal stability of emotion awareness and emotion regulation in individuals with schizophrenia has not been evaluated to date, yet reports suggest that improvements may be feasible. In a study of paranoid individuals (Hepworth et al., 2011), a brief three-session intervention encouraging patients to explicitly express negative feelings associated with paranoid delusions, significantly reduced worry and depression one month later, with trends for reduction in rumination and anxiety, all of which have been linked with social dysfunction. Similarly, a number of schizophrenia treatment studies demonstrated improved facial affect perception, an index of emotion processing (Roberts and Penn, 2009; Horan et al., 2011).
4.4. Limitations and Future Directions
The potential limitations of our study should be acknowledged. One is the relatively modest sample of individuals with schizophrenia. While a greater sample size would have been preferable, the highly significant results, along with negative indices of multicollinearity, provide support for our conclusions. However, the small sample size prevented drawing conclusions about possible differences in emotion awareness and regulation between individuals with schizophrenia and schizoaffective disorders. A second limitation is the lack of a clinical control group, leaving the possibility that the findings may apply to other clinical populations rather than just schizophrenia. Thirdly, it is possible that our findings of poor emotional awareness and regulation, along with poor social functioning in the schizophrenia group reflect a general tendency for negative attitudes about the self. As we did not evaluate this construct, this potential confounder needs to be addressed in future studies. Finally, additional limitations also include the use of a self-report measure to assess social functioning, as well as the focus on only two specific emotion regulation strategies.
Table 4.
Predictors of Social Functioning in Individuals with Schizophrenia
| Dependent Variable: Social Functioning (PSRS) | B | Std. Error | Beta (β) | P | R2 | Adj. R2 | ΔR2 | Sig.F Change |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Block 1 | .14 | −.05 | .14 | .65 | ||||
| Age | .23 | .42 | .10 | .59 | ||||
| Speed of Processing (MCCB) | .23 | .36 | .17 | .52 | ||||
| Attention/Vigilance (MCCB) | −.04 | .41 | −.02 | .93 | ||||
| Working Memory (MCCB) | .05 | .34 | .03 | .89 | ||||
| Verbal Learning (MCCB) | −.60 | .38 | −.36 | .12 | ||||
| Visual Learning (MCCB) | .08 | .34 | .05 | .81 | ||||
| Reasoning & Problem Solving (MCCB) | −.17 | .37 | −.11 | .65 | ||||
|
| ||||||||
| Block 2 | .48 | .33 | .35 | .00 | ||||
| Age | .32 | .34 | .14 | .35 | ||||
| Speed of Processing (MCCB) | −.09 | .29 | −.07 | .75 | ||||
| Attention/Vigilance (MCCB) | −.13 | .34 | −.07 | .70 | ||||
| Working Memory (MCCB) | .37 | .29 | .25 | .22 | ||||
| Verbal Learning (MCCB) | −.36 | .30 | −.21 | .25 | ||||
| Visual Learning (MCCB) | .09 | .27 | .05 | .74 | ||||
| Reasoning & Problem Solving (MCCB) | .22 | .31 | .14 | .47 | ||||
| Difficulty Identifying Feeling (TAS-20) | .57 | .47 | .24 | .23 | ||||
| Difficulty Describing Feeling (TAS-20) | 1.78 | .82 | .46 | .04 | ||||
|
| ||||||||
| Block 3 | .58 | .39 | .10 | .12 | ||||
| Age | .40 | .32 | .17 | .22 | ||||
| Speed of Processing (MCCB) | −.28 | .29 | −.21 | .34 | ||||
| Attention/Vigilance (MCCB) | −.14 | .33 | −.07 | .66 | ||||
| Working Memory (MCCB) | .55 | .29 | .37 | .07 | ||||
| Verbal Learning (MCCB) | −.35 | .31 | −.20 | .27 | ||||
| Visual Learning (MCCB) | −.10 | .27 | −.06 | .70 | ||||
| Reasoning & Problem Solving (MCCB) | .53 | .32 | .32 | .12 | ||||
| Difficulty Identifying Feeling (TAS-20) | .12 | .48 | .05 | .80 | ||||
| Difficulty Describing Feeling (TAS-20) | 1.77 | .81 | .46 | .04 | ||||
| Reappraisal (ERQ) | −.55 | .33 | −.25 | .11 | ||||
| Suppression (ERQ) | .43 | .51 | .14 | .40 | ||||
| Emotion Management Task (MSCEIT) | −.23 | .25 | −.18 | .37 | ||||
Note: N=40; PSRS - Provision of Social Relations Scale; MCCB - MATRICS Consensus Cognitive Battery; TAS-20 - Toronto Alexithymia Scale; ERQ – Emotion Regulation Questionnaire; MSCEIT - Mayer-Salovey-Caruso Emotional Intelligence Test. Higher scores on the PSRS and TAS-20 indicate lower functioning.
Acknowledgment
This work was supported by grants 1K23MH077653 (DK) from the National Institute of Mental Health, Bethesda, MD, USA and a Young Investigator Award (DK) from the National Alliance for Research on Schizophrenia and Depression (NARSAD), Great Neck, NY, USA. We would like to thank Samira Khan for her help in the preparation of this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Badcock JC, Paulik G, Maybery MT. The role of emotion regulation in auditory hallucinations. Psychiatry Res. 2011;185:303–308. doi: 10.1016/j.psychres.2010.07.011. [DOI] [PubMed] [Google Scholar]
- Bagby RM, Parker JDA, Taylor GJ. The twenty-item Toronto Alexithymia scale--I. Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research. 1994;38:23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]
- Barrett LF, Gross J, Christensen TC, Benvenuto M. Knowing what you're feeling and knowing what to do about it: Mapping the relation between emotion differentiation and emotion regulation. Cognition & Emotion. 2001;15:713–724. [Google Scholar]
- Baslet G, Termini L, Herbener E. Deficits in Emotional Awareness in Schizophrenia and Their Relationship With Other Measures of Functioning. Journal of Nervous and Mental Disease. 2009;197:655–660. doi: 10.1097/NMD.0b013e3181b3b20f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell MD, Fiszdon JM, Greig TC, Wexler BE. Social attribution test--multiple choice (SAT-MC) in schizophrenia: comparison with community sample and relationship to neurocognitive, social cognitive and symptom measures. Schizophr Res. 2010;122:164–171. doi: 10.1016/j.schres.2010.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brackett MA, Salovey P. Measuring emotional intelligence with the Mayer-Salovery-Caruso Emotional Intelligence Test (MSCEIT) Psicothema. 2006;18(Suppl):34–41. [PubMed] [Google Scholar]
- Brekke JS, Hoe M, Green MF. Neurocognitive change, functional change and service intensity during community-based psychosocial rehabilitation for schizophrenia. Psychol Med. 2009a;39:1637–1647. doi: 10.1017/S003329170900539X. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Long JD. Community-based psychosocial rehabilitation and prospective change in functional, clinical, and subjective experience variables in schizophrenia. Schizophrenia bulletin. 2000;26:667–680. doi: 10.1093/oxfordjournals.schbul.a033485. [DOI] [PubMed] [Google Scholar]
- Brekke JS, Phillips E, Pancake L, Lewis J, Duke J. Implementation Practice and Implementation Research: A Report From the Field. Res Soc Work Prac. 2009b;19:592–601. [Google Scholar]
- Bromley E, Brekke JS. Assessing function and functional outcome in schizophrenia. Curr Top Behav Neurosci. 2010;4:3–21. doi: 10.1007/7854_2010_40. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Barlow DH, Brown TA, Hofmann SG. Acceptability and suppression of negative emotion in anxiety and mood disorders. Emotion. 2006;6:587–595. doi: 10.1037/1528-3542.6.4.587. [DOI] [PubMed] [Google Scholar]
- Cedro A, Kokoszka A, Popiel A, Narkiewicz-Jodko W. Alexithymia in schizophrenia: an exploratory study. Psychol Rep. 2001;89:95–98. doi: 10.2466/pr0.2001.89.1.95. [DOI] [PubMed] [Google Scholar]
- Couture SM, Penn DL, Roberts DL. The functional significance of social cognition in schizophrenia: a review. Schizophr Bull. 2006;32(Suppl 1):S44–63. doi: 10.1093/schbul/sbl029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eack SM, Greeno CG, Pogue-Geile MF, Newhill CE, Hogarty GE, Keshavan MS. Assessing social-cognitive deficits in schizophrenia with the Mayer-Salovey-Caruso Emotional Intelligence Test. Schizophrenia bulletin. 2010;36:370–380. doi: 10.1093/schbul/sbn091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekman P. An Argument for Basic Emotions. Cognition & Emotion. 1992;6:169–200. [Google Scholar]
- Fett AK, Viechtbauer W, Dominguez MD, Penn DL, van Os J, Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci Biobehav Rev. 2011;35:573–588. doi: 10.1016/j.neubiorev.2010.07.001. [DOI] [PubMed] [Google Scholar]
- Fiszdon JM, Richardson R, Greig T, Bell MD. A comparison of basic and social cognition between schizophrenia and schizoaffective disorder. Schizophrenia Research. 2007;91:117–121. doi: 10.1016/j.schres.2006.12.012. [DOI] [PubMed] [Google Scholar]
- Fukunishi I, Kikuchi M, Wogan J, Takubo M. Secondary alexithymia as a state reaction in panic disorder and social phobia. Compr Psychiatry. 1997;38:166–170. doi: 10.1016/s0010-440x(97)90070-5. [DOI] [PubMed] [Google Scholar]
- Green MF. Stimulating the development of drug treatments to improve cognition in schizophrenia. Annu Rev Clin Psychol. 2007;3:159–180. doi: 10.1146/annurev.clinpsy.3.022806.091529. [DOI] [PubMed] [Google Scholar]
- Green MF, Leitman DI. Social cognition in schizophrenia. Schizophr Bull. 2008;34:670–672. doi: 10.1093/schbul/sbn045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green MF, Olivier B, Crawley JN, Penn DL, Silverstein S. Social cognition in schizophrenia: Recommendations from the Measurement and Treatment Research to Improve Cognition in Schizophrenia New Approaches Conference. Schizophrenia Bulletin. 2005;31:882–887. doi: 10.1093/schbul/sbi049. [DOI] [PubMed] [Google Scholar]
- Greenberg LS, Pascual-Leone A. Emotion in psychotherapy: a practice-friendly research review. J Clin Psychol. 2006;62:611–630. doi: 10.1002/jclp.20252. [DOI] [PubMed] [Google Scholar]
- Gross JJ. Antecedent- and response-focused emotion regulation: divergent consequences for experience, expression, and physiology. J Pers Soc Psychol. 1998;74:224–237. doi: 10.1037//0022-3514.74.1.224. [DOI] [PubMed] [Google Scholar]
- Gross JJ. Emotion regulation: Conceptual foundations. Guilford Press; 2007. [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Muñoz RF. Emotion Regulation and Mental Health. Clinical Psychology: Science and Practice. 1995;2:151–164. [Google Scholar]
- Henry JD, Bailey PE, von Hippel C, Rendell PG, Lane A. Alexithymia in schizophrenia. J Clin Exp Neuropsychol. 2010;32:890–897. doi: 10.1080/13803391003596462. [DOI] [PubMed] [Google Scholar]
- Henry JD, Phillips LH, Maylor EA, Hosie J, Milne AB, Meyer C. A new conceptualization of alexithymia in the general adult population: implications for research involving older adults. Journal of Psychosomatic Research. 2006;60:535–543. doi: 10.1016/j.jpsychores.2005.09.008. [DOI] [PubMed] [Google Scholar]
- Henry JD, Rendell PG, Green MJ, McDonald S, O'Donnell M. Emotion regulation in schizophrenia: affective, social, and clinical correlates of suppression and reappraisal. J Abnorm Psychol. 2008;117:473–478. doi: 10.1037/0021-843X.117.2.473. [DOI] [PubMed] [Google Scholar]
- Hepworth C, Startup H, Freeman D. Developing treatments of persistent persecutory delusions: the impact of an emotional processing and metacognitive awareness intervention. J Nerv Ment Dis. 2011;199:653–658. doi: 10.1097/NMD.0b013e318229cfa8. [DOI] [PubMed] [Google Scholar]
- Honkalampi K, Hintikka J, Tanskanen A, Lehtonen J, Viinamaki H. Depression is strongly associated with alexithymia in the general population. Journal of Psychosomatic Research. 2000;48:99–104. doi: 10.1016/s0022-3999(99)00083-5. [DOI] [PubMed] [Google Scholar]
- Horan WP, Green MF, Degroot M, Fiske A, Hellemann G, Kee K, Kern RS, Lee J, Sergi MJ, Subotnik KL, Sugar CA, Ventura J, Nuechterlein KH. Social Cognition in Schizophrenia, Part 2: 12-Month Stability and Prediction of Functional Outcome in First-Episode Patients. Schizophr Bull; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horan WP, Ventura J, Mintz J, Kopelowicz A, Wirshing D, Christian-Herman J, Foy D, Liberman RP. Stress and coping responses to a natural disaster in people with schizophrenia. Psychiatry Res. 2007;151:77–86. doi: 10.1016/j.psychres.2006.10.009. [DOI] [PubMed] [Google Scholar]
- Hunter R, Barry S. Negative symptoms and psychosocial functioning in schizophrenia: Neglected but important targets for treatment. Eur Psychiatry; 2011. [DOI] [PubMed] [Google Scholar]
- Huprich SK, Sanford K, Smith M. Psychometric evaluation of the depressive personality disorder inventory. J Pers Disord. 2002;16:255–269. doi: 10.1521/pedi.16.3.255.22539. [DOI] [PubMed] [Google Scholar]
- Jansen LM, Gispen-de Wied CC, Kahn RS. Selective impairments in the stress response in schizophrenic patients. Psychopharmacology (Berl) 2000;149:319–325. doi: 10.1007/s002130000381. [DOI] [PubMed] [Google Scholar]
- John OP, Gross JJ. Healthy and unhealthy emotion regulation: personality processes, individual differences, and life span development. J Pers. 2004;72:1301–1333. doi: 10.1111/j.1467-6494.2004.00298.x. [DOI] [PubMed] [Google Scholar]
- Joormann J, Gotlib IH. Emotion Regulation in Depression: Relation to Cognitive Inhibition. Cogn Emot. 2010;24:281–298. doi: 10.1080/02699930903407948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauhanen J, Kaplan GA, Julkunen J, Wilson TW, Salonen JT. Social factors in alexithymia. Compr Psychiatry. 1993;34:330–335. doi: 10.1016/0010-440x(93)90019-z. [DOI] [PubMed] [Google Scholar]
- Kee KS, Green MF, Mintz J, Brekke JS. Is emotion processing a predictor of functional outcome in schizophrenia? Schizophrenia Bulletin. 2003;29:487–497. doi: 10.1093/oxfordjournals.schbul.a007021. [DOI] [PubMed] [Google Scholar]
- Kimhy D, Corcoran C. Use of Palm computer as an adjunct to cognitive-behavioural therapy with an ultra-high-risk patient: a case report. Early Intervention in Psychiatry. 2008;2:234–241. doi: 10.1111/j.1751-7893.2008.00083.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokkonen P, Karvonen JT, Veijola J, Laksy K, Jokelainen J, Jarvelin MR, Joukamaa M. Prevalence and sociodemographic correlates of alexithymia in a population sample of young adults. Compr Psychiatry. 2001;42:471–476. doi: 10.1053/comp.2001.27892. [DOI] [PubMed] [Google Scholar]
- Kooiman CG, Spinhoven P, Trijsburg RW. The assessment of alexithymia: A critical review of the literature and a psychometric study of the Toronto Alexithymia Scale-20. Journal of Psychosomatic Research. 2002;53:1083–1090. doi: 10.1016/s0022-3999(02)00348-3. [DOI] [PubMed] [Google Scholar]
- Kring AM, Caponigro JM. Emotion in Schizophrenia. Current Directions in Psychological Science. 2010;19:255–259. doi: 10.1177/0963721410377599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kring AM, Moran EK. Emotional response deficits in schizophrenia: insights from affective science. Schizophrenia bulletin. 2008;34:819–834. doi: 10.1093/schbul/sbn071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laroi F, Fonteneau B, Mourad H, Raballo A. Basic emotion recognition and psychopathology in schizophrenia. J Nerv Ment Dis. 2010;198:79–81. doi: 10.1097/NMD.0b013e3181c84cb0. [DOI] [PubMed] [Google Scholar]
- Linden W, Wen F, Paulhaus DL. Measuring alexithymia: reliability, validity, and prevalence. In: Butcher J, Spielberger C, editors. Advances in Personality Assessment. Lawrence Erlbaum Associates; Hillsdale, NJ: 1994. [Google Scholar]
- Linehan M. Skills-Training Manual for Treatment of Borderline Personality Disorder. Guilford; New York: 1993. [Google Scholar]
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- Mancuso F, Horan WP, Kern RS, Green MF. Social cognition in psychosis: multidimensional structure, clinical correlates, and relationship with functional outcome. Schizophr Res. 2011;125:143–151. doi: 10.1016/j.schres.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuechterlein KH, Green MF. MATRICS Consensus Battery Manual. MATRICS Assessment Inc.; Los Angeles: 2006. [Google Scholar]
- Nuechterlein KH, Subotnik KL, Green MF, Ventura J, Asarnow RF, Gitlin MJ, Yee CM, Gretchen-Doorly D, Mintz J. Neurocognitive predictors of work outcome in recent-onset schizophrenia. Schizophr Bull. 2011;37(Suppl 2):S33–40. doi: 10.1093/schbul/sbr084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry Y, Henry JD, Grisham JR. The habitual use of emotion regulation strategies in schizophrenia. British Journal of Clinical Psychology. 2011;50:217–222. doi: 10.1111/j.2044-8260.2010.02001.x. [DOI] [PubMed] [Google Scholar]
- Riggs SE, Grant PM, Perivoliotis D, Beck AT. Assessment of Cognitive Insight: A Qualitative Review. Schizophrenia bulletin; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts DL, Penn DL. Social cognition and interaction training (SCIT) for outpatients with schizophrenia: a preliminary study. Psychiatry Res. 2009;166:141–147. doi: 10.1016/j.psychres.2008.02.007. [DOI] [PubMed] [Google Scholar]
- Salminen JK, Saarijarvi S, Aarela E, Toikka T, Kauhanen J. Prevalence of alexithymia and its association with sociodemographic variables in the general population of Finland. J Psychosom Res. 1999;46:75–82. doi: 10.1016/s0022-3999(98)00053-1. [DOI] [PubMed] [Google Scholar]
- Shamsi S, Lau A, Lencz T, Burdick KE, DeRosse P, Brenner R, Lindenmayer J-P, Malhotra AK. Cognitive and symptomatic predictors of functional disability in schizophrenia. Schizophrenia Research. 2011;126:257–264. doi: 10.1016/j.schres.2010.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sifneos PE. Alexithymia: past and present. Am J Psychiatry. 1996;153:137–142. doi: 10.1176/ajp.153.7.137. [DOI] [PubMed] [Google Scholar]
- Stanghellini G, Ricca V. Alexithymia and schizophrenias. Psychopathology. 1995;28:263–272. doi: 10.1159/000284937. [DOI] [PubMed] [Google Scholar]
- Taylor GJ, Bagby RM, Parker JD. The alexithymia construct. A potential paradigm for psychosomatic medicine. Psychosomatics. 1991;32:153–164. doi: 10.1016/s0033-3182(91)72086-0. [DOI] [PubMed] [Google Scholar]
- Taylor GJ, Bagby RM, Parker JDA. Disorders of affect regulation: Alexithymia in medical and psychiatric illness. Cambridge University Press; Cambridge: 1997. [Google Scholar]
- Turner RJ, Frankel BG, Levin D. Social support: Conceptualization, measurement, and implications for mental health. In: Greenley JR, editor. Research in community mental health. JAI Press; Greenwich, CT: 1983. [Google Scholar]
- van 't Wout M, Aleman A, Bermond B, Kahn RS. No words for feelings: alexithymia in schizophrenia patients and first-degree relatives. Compr Psychiatry. 2007;48:27–33. doi: 10.1016/j.comppsych.2006.07.003. [DOI] [PubMed] [Google Scholar]
- van der Meer L, van't Wout M, Aleman A. Emotion regulation strategies in patients with schizophrenia. Psychiatry Res. 2009;170:108–113. doi: 10.1016/j.psychres.2009.07.010. [DOI] [PubMed] [Google Scholar]
- van Rijn S, Schothorst P, van 't Wout M, Sprong M, Ziermans T, van Engeland H, Aleman A, Swaab H. Affective dysfunctions in adolescents at risk for psychosis: Emotion awareness and social functioning. Psychiatry Res. 2011;187:100–105. doi: 10.1016/j.psychres.2010.10.007. [DOI] [PubMed] [Google Scholar]
- van't Wout M, Chang LJ, Sanfey AG. The influence of emotion regulation on social interactive decision-making. Emotion. 2010;10:815–821. doi: 10.1037/a0020069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu S, Li H, Liu W, Zheng L, Ma Y, Chen Q, Chen Y, Yu H, Lu Y, Pan B, Wang W. Alexithymia and Personality Disorder Functioning Styles in Paranoid Schizophrenia. Psychopathology. 2011;44:371–378. doi: 10.1159/000325168. [DOI] [PubMed] [Google Scholar]