Abstract
Qualitative data was collected from Mexican-American (MA) and Puerto Rican (PR) breast cancer survivors to gain their perspectives on the relevant issues surrounding breast cancer survivorship and exercise. Six focus groups, a total of 31 participants were convened (three in Puerto Rico and three in Texas). Responses were analyzed and compared between the Mexican-American and Puerto Rican groups. Follow-up sessions were conducted at the sites to review the initial results and to validate a culturally adapted exercise intervention trial. A total of 900 responses were catalogued into 27 codes. Both groups had similar descriptions of exercise and barriers to exercise. Both groups expressed lack of information regarding their exercise capabilities. The groups differed in their responses to perceived safety in their community and how to deliver a culturally adapted exercise intervention in their community. We found important cultural differences and similarities in relevant factors of exercise and breast cancer survivorship.
Keywords: Hispanic, breast cancer, cultural adaptation, exercise, survivorship
INTRODUCTION
The evidence for the broad and far reaching benefits of exercise continues to accumulate. After the experience of cancer, many breast cancer survivors who were not previously active will stay inactive; and, those who were active do not return to their previous level of activity. Documented benefits of exercise include, improved physical and emotional well-being 1–4, reduced risk for cardiovascular disease 5, diabetes mellitus 6, weight management 7, osteoporosis8, and, second primary cancers 9, 10. Though these benefits have been well documented, less than half of adults meet the recommendations for physical activity and a fourth report no leisure time activity at all 11, 12; cancer survivors report similar or lower levels of inactivity 7, 13, 14.
There are now over 11.4 million cancer survivors in the U.S., with 1.5 million new cases reported annually 15. Approximately 1.8 million of those 11.4 million are Hispanic 15. Hispanics are the most rapidly growing ethnicity in the United States 16. For Hispanic women, breast cancer is the leading cause of cancer death 17 and in Puerto Rico it accounts for approximately 34% of all female cancers 18. The reasons why breast cancer survivors do not exercise are not well understood. Thus research in the knowledge, attitudes and barriers towards exercise in breast cancer survivors is fundamental to aid in the development of culturally adapted exercise interventions.
While the benefits of exercise for cancer survivors are understood, research is needed to identify interventions that encourage survivors to begin and maintain exercise. Intervention strategies for healthy younger populations, may not apply to specific ethno-cultural populations who have had the experience of cancer and/or additional cultural factors that affect exercise behaviors. Furthermore, diversity within Hispanics may also affect the likelihood of exercise. There are differences in race, country of origin, levels of acculturation, English language proficiency, foods, etc., that affect behaviors, including exercise. Thus, investigating the key variables that affect exercise adoption and maintenance within specific cultural contexts of Hispanic cancer survivors is a high priority for research.
To provide formative data for culturally adapting an exercise intervention based on Social Cognitive Theory (SCT), six focus groups of Mexican-American (MA) and Puerto Rican (PR) breast cancer survivors were formed to gain their perspectives on relevant factors surrounding cancer survivorship and exercise. Here we present the methodological approach and qualitative analyses of our results.
METHODS
With participating institutions’ IRB approval, six focus groups were conducted with breast cancer survivors in Texas and in Puerto Rico. PR focus group participants were recruited from the Oncology Hospital of Dr. Isaac Gonzalez Martinez Clinic. MA participants were recruited from local community support groups. The MA groups were conducted in three cities; Harlingen (located in lower Rio Grande valley along the south Texas-Mexico border), Houston, and San Antonio. The PR focus groups were conducted in the San Juan metropolitan area. There was a range of 3–7 participants in each focus group for a total of 31 women.
Breast cancer survivors of self-reported MA or PR Hispanic ethnicity were invited to participate. Focus groups were conducted in the language of choice. All PR focus groups and the MA Houston, Texas focus groups were conducted in Spanish. The groups were facilitated by competent bilingual research staff and bilingual Principal Investigators. Group sessions were audio recorded, transcribed, and Spanish sessions translated into English. After transcription, recordings were destroyed. No participant identifying information was included in the transcription.
Participants were asked six questions: 1.) “What comes to your mind when I say the word exercise?”; 2.) “What kind of exercise experiences have you had prior to cancer?”; 3.) “How do you think exercise might affect you in dealing with cancer?”; 4.) “Do you have any issues of safety or neighborhood safety?” 5.) “How do friends and family feel about exercise for themselves?” “about you exercising?” 6.) “Do you have any ideas about how to best deliver an exercise intervention within the Hispanic community?”
Approximately four months after the initial session, the groups were reconvened. Participants were given a summary of the initial group session results and asked an open ended question: “Did we miss anything?” Responses were recorded and included in the subsequent qualitative analysis reported below.
Analysis
The research team reviewed transcriptions from the group sessions and reached consensus for the emerging themes. Atlas.ti (Berlin, Germany) version 6.0 Qualitative Data Analysis (QDA) software was used. Transcriptions were coded by two research team members. Major themes were aggregated and coded further. The research team reached consensus on the final results presented here.
RESULTS
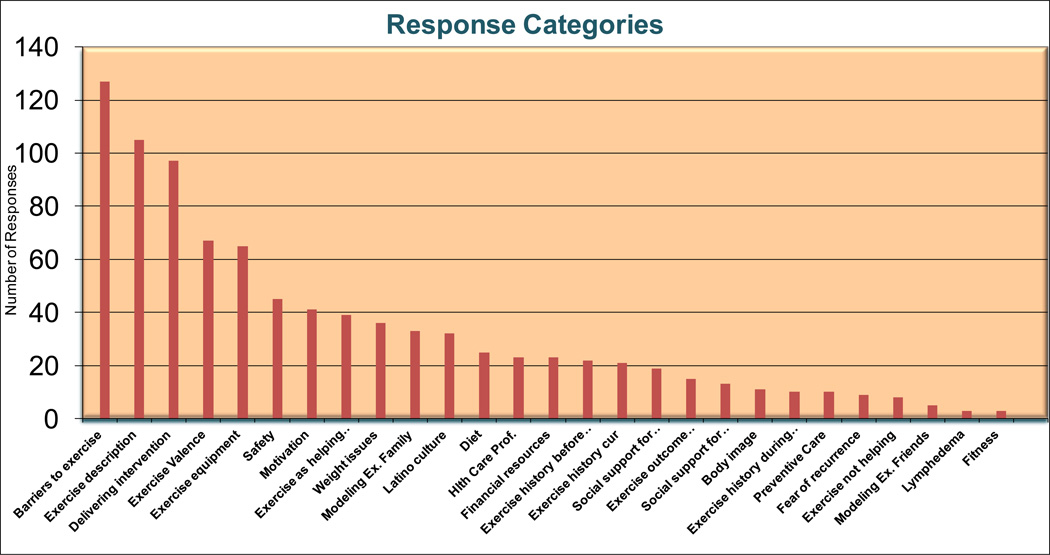
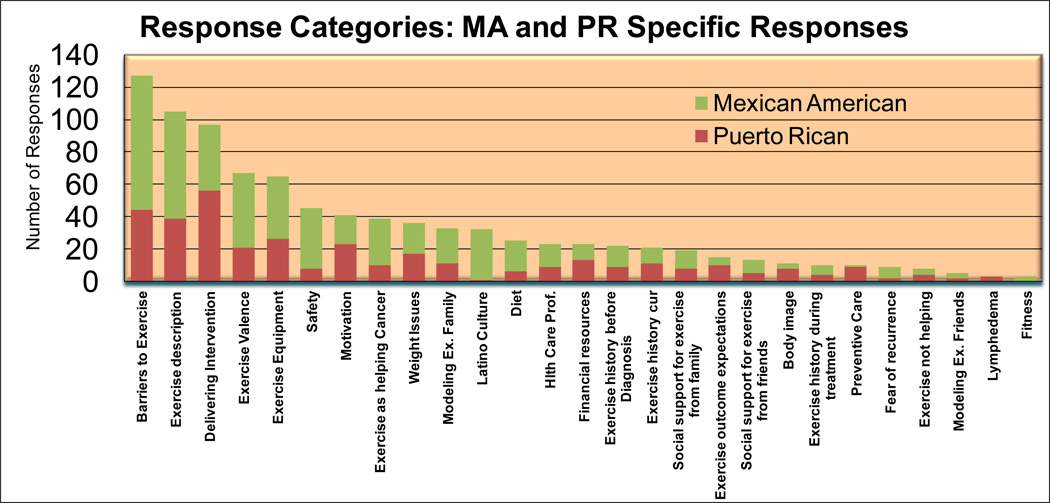
For session one of focus groups, a total of 27 themes were identified and used to catalogue 900 individual responses. Some responses were catalogued into more than one code. Participants had similar responses on what they considered “exercise” to be. They described exercise as walking, dancing, swimming and associated “gym” with exercise. Among the more popular forms of exercise mentioned was walking on trails and on the beach (PR participants). Dancing for fun was mentioned consistently as well. Consistent responses were associating “exercise” with doing chores at home. Chores included: gardening, mopping, cleaning, cutting the grass and taking care of children and grandchildren.
Participants described themselves as being active in their youth. Typical comments were: “I was very active when I was younger and then there was about a period of 25 years when I didn’t exercise.” Prior to cancer diagnosis, participants described themselves as being “very active”: “I’ve always been active, not so much doing exercise but just being active”; and, “Before my cancer I was a very active person. I did not do exercise…. I did whatever needed to be done at home.” During active treatment, participants mentioned being less active: “then I got the cancer and I got even less active.”
Many of the participants reported not doing much current exercise. Typical comments included: “I do not exercise… I still work full time. I work standing all day and walk all day long… I do not have time to exercise”; and, “After my cancer, I do not exercise but I do not know why.” Several participants however reported doing some form of exercise. For example: “Now, I do aerobics 3 times a week, dance and abdominals.” Another consistent message was reporting difficulty with exercise: “I try but I cannot use the [treadmill] machine more than 15 minutes. I get really tired.”
Another common theme among the groups was the lack of information from health care providers regarding exercise during and after active treatments. Participants consistently reported confusion regarding their post treatment care and how much ambulation or physical activity they should or could do. Participants indicated a desire for more direction. Typical comments included: “I did not have any orientation about exercise after my mastectomy operation. Now that I think back I would [have] liked to have received information.” Participants who had completed active treatment reported having sought help from other cancer survivors, personal supporters, or from the internet in lieu of receiving information from health care professionals.
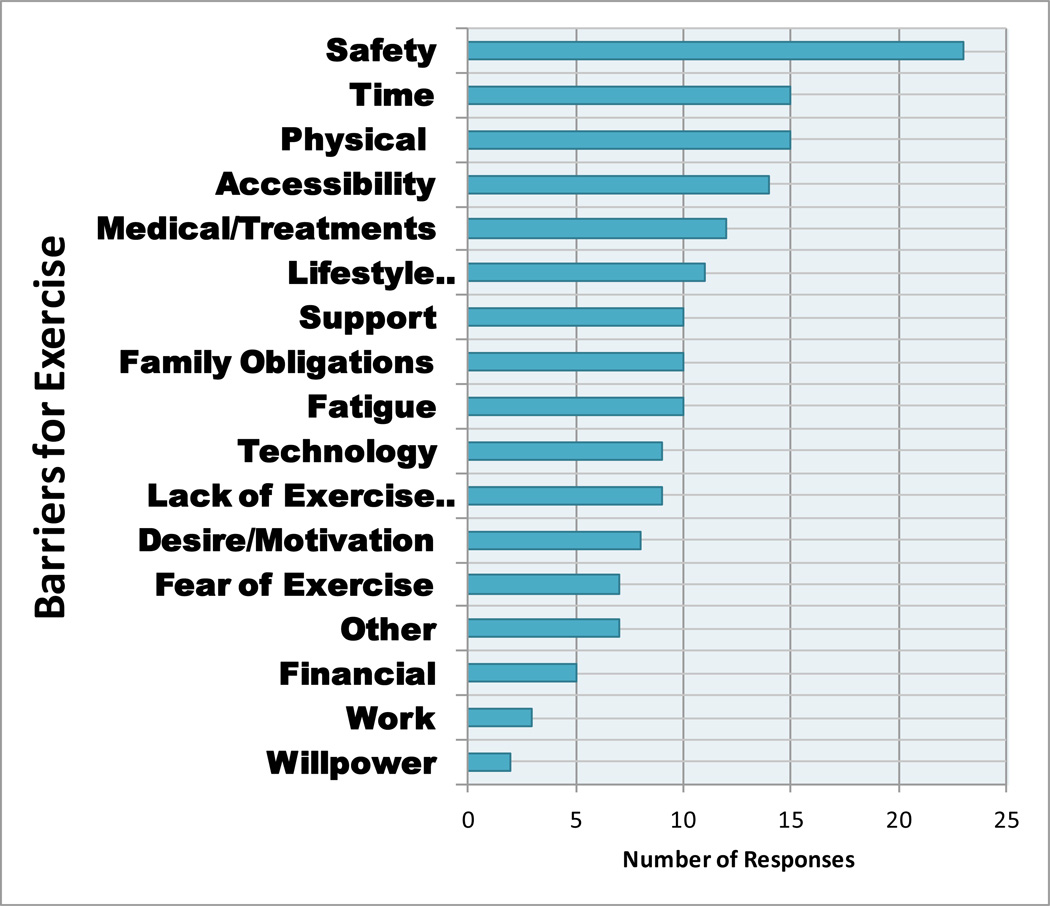
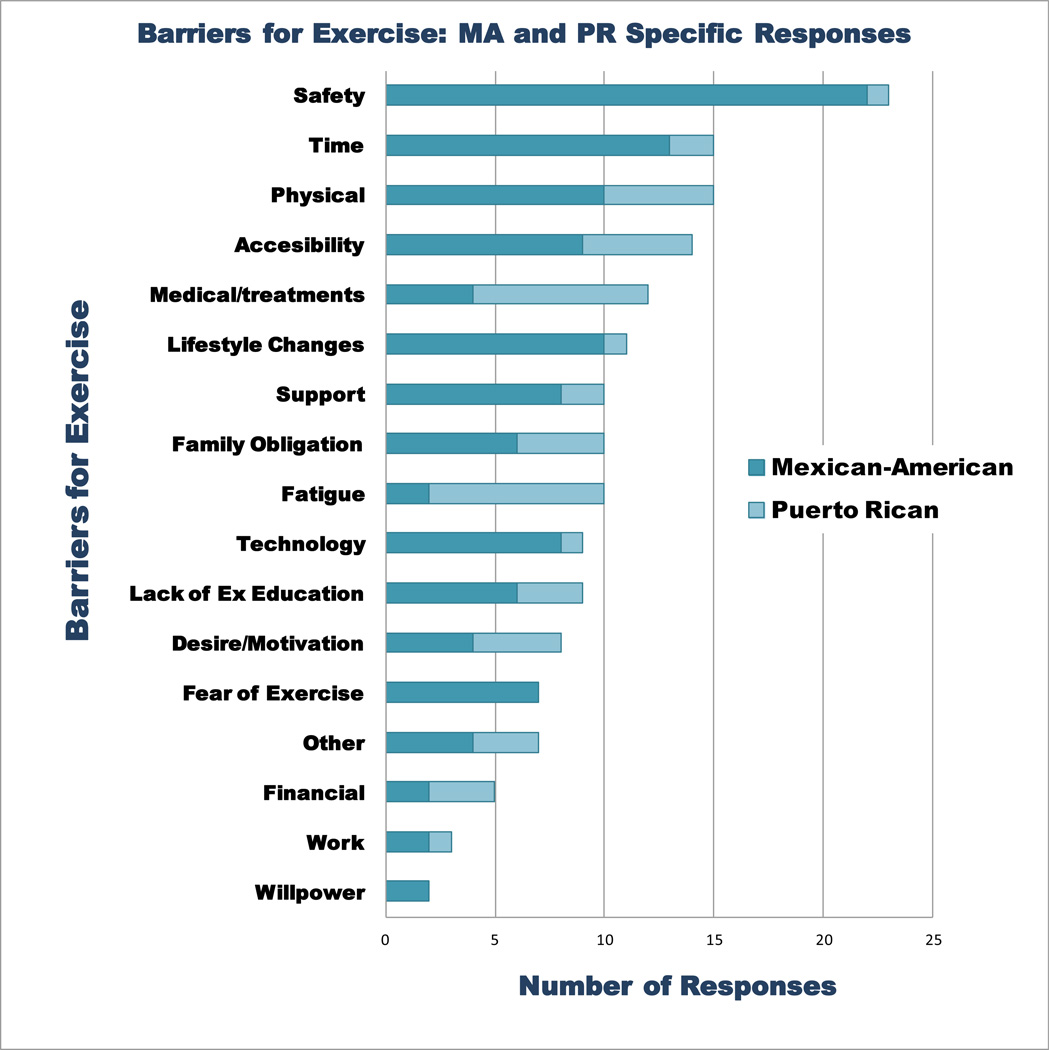
Survivors identified several key barriers to exercise. Aside from their own medical and treatment history, safety, time and accessibility to exercise facilities were common across groups. The lack of time for exercise included issues of attending to family needs. Typical comments included: “Different things got in the way like my husband coming from work to eat or that I had to help the kids with school”; “The older I get the harder it gets in finding the time; my kids are grown, I have 5 grandkids now”; and, “I was not very active, I was too focused on my career… I would work 60 hours a week plus the family.” Accessibility was also a barrier for both groups. The MA group reported not having any parks close by and the lack of sidewalks to walk on in their neighborhoods whereas the PR group mentioned the lack of access to gym facilities.
Consistent with SCT, lack of support was a common response as a barrier to exercise. Participants responded that they would like to have more support to exercise from family and friends. Typical comments were: “In my case, I will get more motivated if a member of my family or a friend goes and exercises with me”; and, “Sometimes we need a stimulus to exercise, a person that will go with me and will share with me. Nobody in my family exercises.”
Participants reported “fatigue” as a common barrier for exercise. Typical comments included: “This tiredness may be the reason why we are not motivated to exercise.” Participants felt that their bodies were not the same: “I feel that now after receiving all the cancer treatments my resistance is lower. I get tired and fatigued more often”. The PR group cited “fatigue” as the main barrier to exercise; whereas, the MA cited “time” as a main barrier. It is worth mentioning that PR “fatigue” may have been linked to their treatment since these participants were directly recruited from the oncology clinic.
Although, there were similarities in responses to the six questions between both groups, there were key differences as well. Though both groups cited safety as an issue, there were differences in perceived safety in their surroundings. The PR groups stated their neighborhoods, parks and beaches were safe to exercise in; whereas, MA groups had concerns with safety in their neighborhoods and parks. They reported loose dogs, suspicious people or “gang” members, and lack of security or vigilance. Typical examples included: “In my neighborhood I have some dogs that tend to jump the fence and bark at you and they seem kind of menacing”; and, “In my neighborhood there is a park that I walk at, but a group of gang members have been gathering there and I get scared now…”.
In session one focus groups, a major difference was on the responses to the question of: “Do you have any ideas about how to best deliver an exercise intervention within the Hispanic community?” The MA group preferred to exercise in a group setting, mentioning that “mixed” groups that included people that were part of the intervention and those that were not (i.e. friends and family members, active or inactive) would be a good way to motivate those that were in the program. Another MA participant mentioned that various group settings would work for their Hispanic community: “I am not only saying to make one. It could be various groups for example one in the North side and another group in the South side”. Another participant suggested “having more community events, like right now Brownsville (Texas) is having the biggest loser there were like 500 people out there”. Conversely, the PR group preferred individual exercise: “I would prefer receiving the orientation after surgery at the hospital room. That’s including developing an exercise plan individualized for me, what I can do and what I can’t in summary after surgery. Since I had no orientation after surgery I felt lost.” The PR group preferred individualized exercise integrated with their health care: “It could be good that patients receive treatments and after they finished they can go to an area to exercise at the same hospital. I would like to see exercise as part of my treatment”. The groups differed in their preferences for the intervention setting. The MA group preferred to have interventions in places like community parks, walking trails, churches, activity centers, and clinics: “In schools, clinics, and definitely in the churches, they are the center of information most frequently given that we have.” In contrast, the PR group chose hospital settings for exercise and wanted some sort of gym facility or space available where they could exercise while waiting for their follow up appointments.
While exercise education was important to both groups, there were differences in the way they wanted to receive the information. The MA group preferred exercise through support groups, testimonies, and community events. They indicated personal testimonies would encourage exercise: “I think just giving them our testimonies of what we’ve been through and exercise we’ve done …would encourage them to do it.” The PR group preferred demonstrations: “I think people like contact with other people. Conference and demonstrations can be given by the social workers, the priest, or they could hire a personal trainer”; and, “Visuals are very important, that’s why Power Point presentations are a success”.
The PR group preferred not to use the internet for an intervention in contrast to the MA participants. PR participants mentioned that the internet was not a good tool for them to use: “I do like a demonstration in front of me, no video, and no internet.” The MA group liked the internet: “Now there is also the internet and there’s also chat where you can talk to other people and ask them a question.”
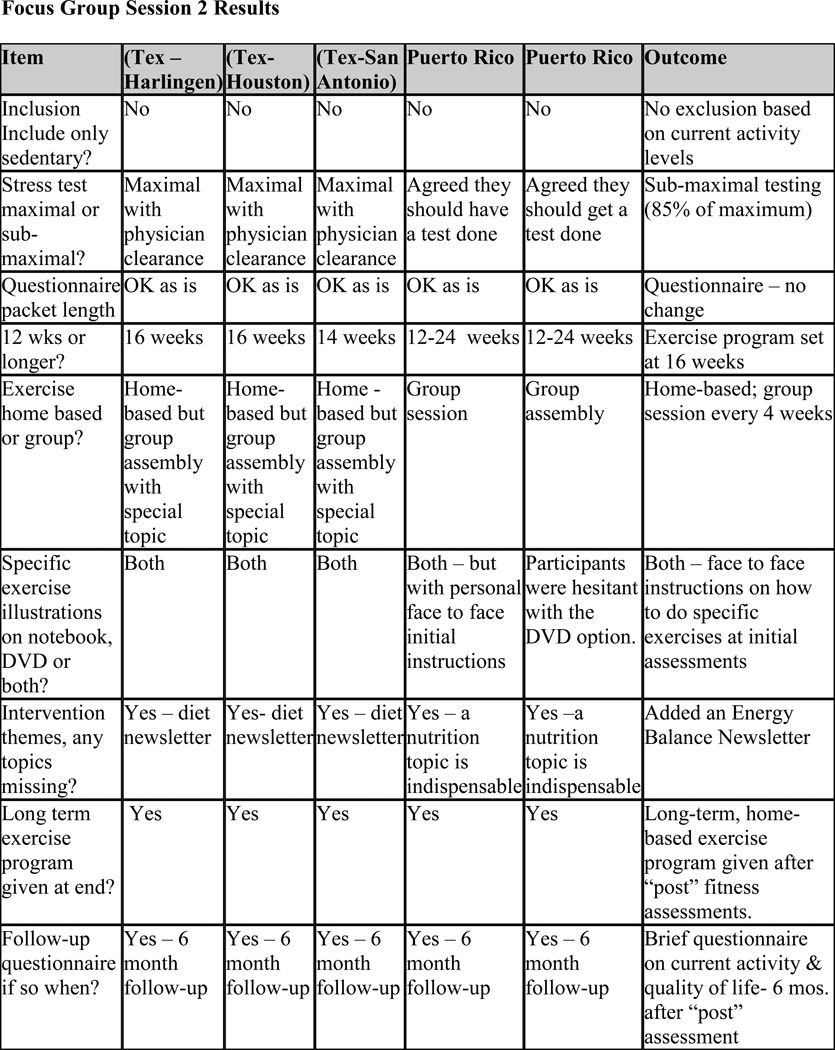
We incorporated the information from these initial sessions to formulate a culturally adapted prototype pilot intervention. We invited the same participants for a second round of sessions to review the results. The focus for this session was to garner survivors’ input on key decision points to inform both assessment and exercise intervention methodologies. We presented a flow diagram of the methodology, and asked for input on 9 key issues.
Consistent with the initial sessions, there was agreement and differences between the two groups. Both groups agreed with: maximal exercise testing, questionnaire length, intervention length, adding a dieting newsletter, providing a long term exercise program, and the addition of a follow-up questionnaire six months after the study. The groups differed in the mode of the exercise reference materials and whether the intervention should have a home-based or group based focus. In contrast to the first session where the PR group preferred individual exercise; on the second session the PR group preferred group sessions and direct contact with research staff. In comparison to the first session where MA mentioned group exercise intervention, in session two, the MA group favored a home-based intervention with occasional group exercise so that they could still do the exercise program based on their own schedule and time reservations. Key modifications were made to the methodology based on these results.
DISCUSSION
Published literature regarding strategies and variables for successful recruitment and initiation of physical activity among Hispanics is limited 19. More studies are needed that sample females and other racial and ethnic groups since concepts of time, adherence to schedules, and other cultural dimensions are different between ethnic groups. If not examined, similar programs might be used in divergent populations resulting in lowered levels of engagement of physical activity in populations that may benefit the most 20. Here we sought informative data on issues of breast cancer survivorship and exercise from MA and PR breast cancer survivors to develop a specific culturally adapted exercise intervention. Information on participants’ views of exercise and the cancer experience, and specific barriers to exercise were collected in an initial set of focus group meetings. The same participants were invited for a second session to provide direct feedback on the methodology of a culturally adapted intervention pilot based on their input. The ultimate objective of our research efforts is to develop specific culturally competent exercise interventions for Hispanic cancer survivors.
We found important cultural similarities and differences surrounding the issues of their specific experiences in regards to exercise and breast cancer survivorship for both groups. Both groups defined exercise similarly and cited “barriers to exercise” as a major issue; “time” and “fatigue” being the most cited barrier. Similar barriers to the ones we found have been published in a study with non-Hispanic breast cancer survivors. However, in this study one of the most cited barriers was “age” 21. Another consistent theme was a lack of information and education from health care professionals on what exercise could or should be done at critical times in the cancer treatment continuum, such as after diagnosis, during active treatment, and post treatment. This lack of knowledge may contribute to what they reported as a perceived fear of exercising. Findings from another study suggest that oncologists’ recommendation for exercise may increase exercise behavior in breast cancer survivors as soon as they are diagnosed 22.
The groups differed on the methodology for delivery of an exercise intervention in their communities. MA survivors preferred interventions to be more home-based and with technology (e.g. Internet access); whereas, the PR group preferred more in-person intervention done in a clinic or hospital setting. However, both groups had an interest in at least some group participation. This differs from studies that have showed that breast cancer survivors stated not wanting any structured or formalized exercise but rather wanted things such as gardening and everyday activities in their exercise program 21.
The generalizations of our results need to be viewed within the context of a few limitations. First, we only conducted 2 rounds of focus groups sessions; results may have been different if we had continued with more interactive sessions with the same participants. Secondly, we used qualitative analyses; care must be taken not to interpret the results “quantitatively”. Even though our focus groups provided insight to our queries, data from focus groups is better served as a source of suggestions and direction for a new program 23. Finally, although we had consensus on coding themes, and we followed a SCT based model in the methodology of our analytic approach, we may have unintentionally biased the results by our selection of themes. Despite these limitations, our results indicate the need to account for key cultural issues to succeed in design of a culturally competent intervention. Moreover, we infused formative data from the focus groups to create and then revise the methodology of a pilot intervention based on this data. We forward that an intervention informed by data from the potential participants will ultimately be more effective in engendering exercise behaviors than an intervention developed without such information.
Our results of working with these focus groups illustrate clearly that even though both Mexican-Americans and Puerto Ricans are often grouped together as “Hispanic” breast cancer survivors; there is important cultural variability between the two groups in issues related to exercise and cancer survivorship. We have taken the steps to understand these similarities and variabilities and to incorporate them in a specific culturally adapted intervention. Further research to understand cultural specific variables of exercise behaviors for specific ethnic breast cancer survivors are urgently needed.
Figure 1.
Codes for responses for first round of focus groups sessions.
Figure 2.
Category “barriers for exercise” coded into further themes, for focus group one.
Figure 3.
Group Specific response categories for the first round of focus groups.
Figure 4.
Focus group one, specific responses for “barriers for exercise” themes between MA and PR.
Figure 5.
Changes to pilot intervention based on second round of focus groups.
Table 1.
Mexican- American Participant Characteristics
| Participant characteristics* | (n) |
|---|---|
| Age, years (M=55.8; SD =7.9; range = 44–72) | |
| Nativity | |
| United States – Texas | (10) |
| United States – Other State | (1) |
| Latin – Mexico | (3) |
| Latin – other country | (1) |
| Education | |
| Greater than bachelor degree | (1) |
| 4-year college degree | (4) |
| Some college | (5) |
| Technical/vocational degree | (3) |
| High school degree | (1) |
| Did not complete high school | (1) |
| Employment | |
| Part time | (7) |
| Full time | (1) |
| Homemaker | (3) |
| Retired | (4) |
| Marital Status | |
| Single | (3) |
| Married/Co-Habitating | (9) |
| Divorced | (3) |
| Language Spoken at Home | |
| Spanish | (3) |
| Both Spanish & English | (7) |
| English | (5) |
Demographic information was collected on the MA focus group participants as shown in Table 1 (There was no demographic information collected on the PR participants due to IRB approval as an exempt protocol). The average of the MA focus group participants was 55.8 (± 7.9) years of age with the youngest participant 44 years old and the oldest 72. Most participants were born in the U.S. (75%) with only 4 participants from either Mexico or Colombia. For those born outside the U.S. time in the U.S. averaged 25 years.
The group was well educated with only one participant not completing high school and 75% of the participants having at least some college. About half (53%) of the participants were employed outside the home. Language preference at home was either Spanish or both Spanish and English (77%) with only 5 participants reporting English as the primary language spoken at home.
Acknowledgments
The project described was supported by the National Cancer Institute Award Number K22CA154626 and National Cancer Institute Award Number U54 CA 96300. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health. The authors gratefully acknowledge the support of the Cancer Therapy and Research Center at the University of Texas Health Science Center San Antonio, an NCI-designated Cancer Center, (P30CA054174). The authors gratefully acknowledge those breast cancer survivors who participated in the focus groups in Texas and Puerto Rico and who so openly shared their views.
Contributor Information
Liliana Vallejo, Email: LNVallejo@mdanderson.org.
Daniel C. Hughes, Email: HughesDC@uthscsa.edu.
Velda Gonzalez, Email: velda.gonzalez@upr.edu.
Maribel Tirado-Gomez, Email: maribel.tirado1@upr.edu.
Karen Basen-Engquist, Email: kbasenen@mdanderson.org.
REFERENCES
- 1.Courneya KS. Exercise in cancer survivors: an overview of research. Med Sci Sports Exerc. 2003 Nov;35(11):1846–1852. doi: 10.1249/01.MSS.0000093622.41587.B6. [DOI] [PubMed] [Google Scholar]
- 2.Courneya KS, Mackey JR, Bell GJ, Jones LW, Field CJ, Fairey AS. Randomized controlled trial of exercise training in postmenopausal breast cancer survivors: cardiopulmonary and quality of life outcomes. J Clin Oncol. 2003 May 1;21(9):1660–1668. doi: 10.1200/JCO.2003.04.093. [DOI] [PubMed] [Google Scholar]
- 3.Segal R, Evans W, Johnson D, et al. Structured exercise improves physical functioning in women with stages I and II breast cancer: results of a randomized controlled trial. J Clin Oncol. 2001 Feb 1;19(3):657–665. doi: 10.1200/JCO.2001.19.3.657. [DOI] [PubMed] [Google Scholar]
- 4.Pinto BM, Frierson GM, Trunzo JJ, Marcus BH. Home-based physical activity intervention for breast cancer patients. J Clin Oncol. 2005 May 20;23(15):3577–3587. doi: 10.1200/JCO.2005.03.080. 2005; [DOI] [PubMed] [Google Scholar]
- 5.LaCroix AZ, Leveille SG, Hecht JA, Grothaus LC, Wagner EH. Does walking decrease the risk of cardiovascular disease hospitalizations and death in older adults? J Am Geriatr Soc. 1996 Feb;44(2):113–120. doi: 10.1111/j.1532-5415.1996.tb02425.x. [DOI] [PubMed] [Google Scholar]
- 6.Helmrich SP, Ragland DR, Leung RW, Paffenbarger RS., Jr. Physical activity and reduced occurrence of non-insulin-dependent diabetes mellitus. N Engl J Med. 1991 Jul 18;325(3):147–152. doi: 10.1056/NEJM199107183250302. [DOI] [PubMed] [Google Scholar]
- 7.Doyle C, Kushi LH, Byers T, et al. Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA: A Cancer Journal for Clinicians. 2006 Nov-Dec;56(6):323–353. doi: 10.3322/canjclin.56.6.323. [DOI] [PubMed] [Google Scholar]
- 8.Devogelaer J, de Deuxchaisnes C. Therapy and the 1990s: Osteoporosis. Br J Rheumato. 1993;32:48–55. doi: 10.1093/rheumatology/32.suppl_4.48. [DOI] [PubMed] [Google Scholar]
- 9.Giovannucci E, Ascherio A, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Physical activity, obesity, and risk for colon cancer and adenoma in men. Ann Intern Med. 1995 Mar 1;122(5):327–334. doi: 10.7326/0003-4819-122-5-199503010-00002. [DOI] [PubMed] [Google Scholar]
- 10.Holmes MD, Chen WY, Feskanich D, Kroenke CH, Colditz GA. Physical activity and survival after breast cancer diagnosis. JAMA. 2005 May 25;293(20):2479–2486. doi: 10.1001/jama.293.20.2479. [DOI] [PubMed] [Google Scholar]
- 11.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health: a recommendation from the centers for disease control and prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 12.Blair SN, Cheng Y, Holder JS. Is physical activity or physical fitness more important in defining health benefits? Med Sci Sports Exerc. 2001 Jun;33(6 Suppl):S379–S399. doi: 10.1097/00005768-200106001-00007. discussion S419-320. [DOI] [PubMed] [Google Scholar]
- 13.Courneya KS, Friedenreich CM. Relationship between exercise pattern across the cancer experience and current quality of life in colorectal cancer survivors. J Altern Complement Med. 1997 Fall;3(3):215–226. doi: 10.1089/acm.1997.3.215. [DOI] [PubMed] [Google Scholar]
- 14.Irwin ML, Crumley D, McTiernan A, et al. Physical activity levels before and after a diagnosis of breast carcinoma: the Health, Eating, Activity, and Lifestyle (HEAL) study. Cancer. 2003 Apr 1;97(7):1746–1757. doi: 10.1002/cncr.11227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Cancer Society. Cancer Facts & Figures 2010. Atlanta, GA: American Cancer Society; 2010. [Google Scholar]
- 16.United States Census Bureau. Statistical Abstract of the United States: 2000. 120th ed. Washington, DC: United States Government Printing Office; 2000. [Google Scholar]
- 17.American Cancer Society. Cancer facts and figures for Hispanics/Latinos. 2009–2011. Atlanta, GA: American Cancer Society; 2009. [Google Scholar]
- 18.Puerto Rico Central Cancer Registry. Puerto Rico Cancer Incidence File (May 2007) 2007 [Google Scholar]
- 19.Whitehorse LE, Manzano R, Baezconde-Garbanati LA, Ginger H. Culturally tailoring a physical activity program for Hispanic women: recruitment successes of La Vida Buena's salsa aerobics. Journal of Health Education. 1999;30(2):S18–S24. [Google Scholar]
- 20.Ransdell LB, Wells CL. Physical activity in urban white, African-American, and Mexican-American women. Med Sci Sports Exerc. 1998;30(11):1608–1615. doi: 10.1097/00005768-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Milne HM, Gordon S, Guilfoyle A, Wallman KE, Courneya KS. Association between physical activity and quality of life among Western Australian breast cancer survivors. Psychooncology. 2007 Dec;16(12):1059–1068. doi: 10.1002/pon.1211. [DOI] [PubMed] [Google Scholar]
- 22.Jones LW, Courneya KS, Fairey AS, Mackey JR. Effects of an oncologist's recommendation to exercise on self-reported exercise behavior in newly diagnosed breast cancer survivors: a single-blind, randomized controlled trial. Ann Behav Med. 2004 Oct;28(2):105–113. doi: 10.1207/s15324796abm2802_5. [DOI] [PubMed] [Google Scholar]
- 23.Ramirez AG, Shepperd J. The use of focus groups in health research. Scand J Prim Health Care Suppl. 1988;1:81–90. [PubMed] [Google Scholar]