Abstract
Background:
Fungi may play a key part in periradicular diseases. The aim of this study was to evaluate and compare the antifungal properties of two root-end filling materials, ProRoot Mineral trioxide aggregate (MTA) and MTA-Angelus, against Candida albicans using tube-dilution test.
Materials and Methods:
The antifungal properties of ProRoot MTA and MTA-Angelus against C. albicans was assessed at 1, 24, and 48 hours following administration of two concentrations of the antifungal agents (50 and 100 mg/ml). A total of 50 culture wells were divided into four experimental groups (Freshly mixed MTA, Freshly mixed MTA-Angelus, 24-h set MTA, and 24-h set MTA-Angelus) and two control groups. Each well was prepared for one specific agent with a specific concentration. For the set groups, the mixture was prepared and left for 24 hours. One milliliter of suspension of fungal colonies with concentration of 104 CFU/ml was then added to the mixtures in each well. All wells were incubated at 37°C and assessed at 1, 24, and 48 hours. This observation was based on the turbidity of the suspension in the tubes. At each time point, 0.02 ml of each suspension was cultured on a Sabouraud dextrose agar plate to confirm C. albicans growth. The results were analyzed using Kruskal-Wallis test.
Results:
Although all fresh and set samples were incapable of killing C. albicans at 1 hour, they demonstrated fungicidal ability on agar plates at 24 and 48-hour time points.
Conclusion:
MTA-angelus proved to be an effective antifungal agent compared to ProRoot MTA at concentrations of 50 mg/ml and 100 mg/ml.
Keywords: Antifungal agents, Candida, endodontic
INTRODUCTION
Microorganisms are the main cause of endodontic infections. The residual and resistant microorganisms have been recognized as the basic reason for failures in root canal treatments.[1] Fungi, chemoorganotrophic eukaryotic microorganisms, may play a key part in periradicular diseases.[2,3] While they have been found sporadically in initial root canal infections, fungi tend to be found more often in canals where treatment has failed.[2] Failure of some endodontic treatments may therefore be explained by the presence of Candida albicans in the oral flora.[3] It is reported that in 20% of endodontic treatment failures, C. albicans is present.[4] Candida species, which have a tendency to invade dentin, are regarded as dentinophilic microorganisms.[2] The presence of C. albicans in endodontic treatment failures may be the result of coronal leakage after, or contamination during, the endodontic treatment. Several factors, such as an ability to survive despite a lack of nutrients or resistance to intracanalicular treatment materials, may result in C. albicans remaining in the root canal system.[4] C. albicans has been found in some failed endodontic treatments; a phenomenon that might be explained by the invasive nature of this fungus or its resistance to some intracanalicular medications, e.g., calcium hydroxide.[2]
If repeated treatment has either failed or is unfeasible, the only alternative is a root-end resection. Apical sealing, avoiding contamination, and reducing the number of microorganisms, including bacteria and fungi, influence the success rate of such treatment. Therefore, the antibacterial and antifungal properties of root-end filling materials are important to the outcome of these procedures.
Mineral trioxide aggregate (MTA) was introduced in 1993 and, after different examinations, approved, in 1998, by the US Food and Drug Administration as an endodontic biomaterial, used in root-end filling, vital pulp capping, apexification, and root or furcal perforation repair.[5–8] MTA is marketed as gray and white. However, because of the tooth-discoloring properties of gray MTA, white MTA has been pushed to replace it. MTA has a number of advantages, including excellent sealing ability, biocompatibility, high alkalinity, radiopacity, antimicrobial effects, and resistance to fluid and blood contamination.[9–11] In spite of having disadvantages, such as delayed setting time, poor handling properties, and high price, MTA, because of its physical and chemical properties, has become the gold standard of root-end filling materials.[12]
MTA-Angelus is made from Portland cement. Bismuth oxide is added in order to raise its radiopacity. Its characteristics include releasing calcium ions and increasing the pH.[11] MTA-Angelus particles are not as homogenous as ProRoot MTA.[13] In comparison to ProRoot MTA, MTA-Angelus releases slightly more calcium ions.[14] MTA-Angelus shows several advantages, such as good marginal adaptation, good sealing, sealing ability in mineralized tissues with complete closure, and has been reported to be inflammation-free in most cases.[15–17] MTA-Angelus has an excellent antibacterial effect and a strong fungicidal effect against C. albicans.[11,18,19] While both the white and gray MTA-Angelus have arsenic in their structures, white MTA-Angelus has the benefit of containing arsenic levels below the limit set by the ISO 9917-1 standard.[20] Like ProRoot MTA, MTA-Angelus has low cytotoxicity.[21]
A limited number of researches have compared the antifungal effects of ProRoot MTA and MTA-Angelus.[11,18] However, such studies have been conducted using agar diffusion test (ADT), a method that does not seem appropriate because of low solubility and diffusibility of MTA.[22]
The aim of this in vitro study was to evaluate and compare the antifungal properties of fresh and set ProRoot MTA and MTA-Angelus, in concentrations of 50 mg/ml and 100 mg/ml, against C. albicans at 1-, 24-, and 48-hour time points. The null hypothesis of this study was that there is no difference in the in vitro antifungal properties of these two materials.
MATERIALS AND METHODS
The antifungal activity of ProRoot MTA (Dentsply Tulsa Dental, Tulsa, USA) as well as MTA-Angelus (Angelus, Londrina, Brazil) was evaluated against C. albicans. The culture of Sabouraud dextrose agar (Merck, Darmstadt, Germany) was prepared according to the manufacturer's instructions with a definite ratio of powder to liquid. After autoclave sterilization, the agar was poured into culture plates. Samples of live C. albicans, (ATCC 10231) provided by Scientific Research Organization, (Tehran, Iran) were subcultured on the Sabouraud dextrose agar plates. The agar plates, containing the fungus, were then maintained at 37°C. Times and conditions for the culture of C. albicans in this study were determined following the NCCLS standards (National Committee on Clinical Laboratory Standards).
A total of 50 culture wells were divided into four experimental groups (Freshly mixed MTA, Freshly mixed MTA-Angelus, 24-h set MTA, 24-h set MTA-Angelus) and two control groups (positive control, negative control). Each culture well was prepared for one specific agent with a specific concentration. The root canal filling materials were prepared according to their instructions and then mixed with the appropriate volume of sterile water to reach the concentrations of 50°mg/ml or 100°mg/ml. For the set groups, the mixture was prepared and left for 24 hours. Each group consisted of 10 wells, and the control groups consisted of five wells each.
Suspensions were then made by the addition of several fungal colonies from the surface of the Sabouraud dextrose agar plates to Sabouraud dextrose broth media. A final concentration of 104 CFU/ml (colony forming unit/milliliter) was achieved, as recommended by the NCCLS, via microscopic cell counting. One milliliter of this suspension was then added to the mixtures in each well.
Wells with 1 ml of C. albicans suspension mixed and 1 ml of Sabouraud dextrose broth media without root end-filling materials served as positive control and wells with 1 ml of Sabouraud dextrose broth media without C. albicans served as negative control.
All wells were incubated at 37°C and evaluated for 1, 24, and 48 hours by an independent observer by assessing the colonies of C. albicans in each well. This assessment was based on the turbidity of the suspension in the tubes. At each time point, 0.02 ml of each suspension was cultured on Sabouraud dextrose agar plate to confirm C. albicans growth. The results were evaluated and analyzed using Kruskal-Wallis test. Statistical significance was established at P<0.05.
RESULTS
After the culture of 0.02°ml of the treated suspension on the agar plates, the fungal growth was assessed at 1-, 24-, and 48-hour time points. While fungal growth was not observed in any of the negative control groups, it was observed in each of the positive control groups.
After 1 hour, both the MTA and MTA-Angelus were incapable of killing C. albicans. The results were the same for both freshly mixed and set samples at both concentrations (50 and 100 mg/ml).
Increasing the incubation time to 24 hours and then 48 hours demonstrated a lack of fungal growth on agar plates. Both materials were fungicidal for C. albicans at both concentrations of 50 and 100 mg/ml, and in both states of fresh and set [Table 1].
Table 1.
Comparison of ProRoot MTA and MTA-Angelus in concentration of 50 mg/ml and 100 mg/ml at 1, 24, and 48-h time intervals
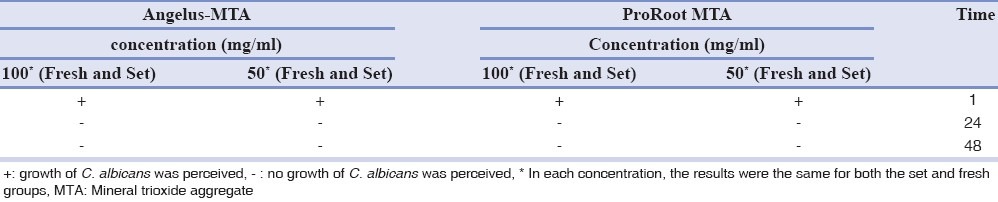
There was no significant difference between using the two materials at either of the concentrations or either of the 1-hour, 24-hour, or 48-hour time points (P<0.05).
DISCUSSION
In this study, the antifungal properties of ProRoot MTA and MTA-Angelus against C. albicans in two concentrations and in fresh and set situations were compared by using tube-dilution test. Because the two materials elicited the same reaction against C. albicans in different conditions, the null hypothesis that there is no difference in the in vitro properties of these two materials has to be accepted.
The most common method for assessing the antifungal or antibacterial activity of root-end filling materials is the ADT.[11] However, several parameters, such as lack of standardization of inoculum density, adequate culture medium, agar viscosity, plate storage condition, size and number of specimens per plate, time and temperature of incubation, and reading point of the inhibition zones, can affect the results of the ADT.[23] The method used in this in vitro study was the tube-dilution susceptibility test; an efficient method for evaluating antifungal characteristics of materials.[24] In this technique, direct contact between C. albicans and the experimental materials was allowed, allowing a more realistic interaction.
Because of possible changes in the chemical structure of the products, root-end filling materials should be tested in two situations; one where the material is used immediately after mixing, and another, where it is used after having been allowed to reach its final chemical composition, or set state. In this study, ProRoot MTA and MTA-Angelus were tested in freshly mixed and set states, to mimic clinical use of the materials. After setting, materials are still able to release active ingredients. Consequently, the perceived difference in antifungal patterns of the materials may be a result of the differences in the degree of setting.[25] However, in our study, the results were similar in the two different states for all tested materials. Based on NCCLS standards, 1-, 24-, and 48-hour time points were used.
The results of this study showed that C. albicans was not affected by the freshly mixed and set, ProRoot MTA and MTA-Angelus, at 1 hour. However, these materials were effective in eliminating C. albicans by the 24-h time point.
Some studies have reported the inhibitory effect of ProRoot MTA and MTA-Angelus on C. albicans by determining the diameter of the inhibition zones in millimeters, and have resulted conclusions similar to this study.[11,18]
The presence of calcium hydroxide, produced by a hydration reaction from the mixing of MTA with water, and an increase in pH, as a result of the release of hydroxyl ions, is probably the mechanism of the antimicrobial activity of MTA-Angelus. Alkalinity can inactivate cell membrane enzymes in microorganisms. This in turn inhibits their biological activity.[26] Some studies have assessed the susceptibility of C. albicans to calcium hydroxide. They suggested that the presence of calcium hydroxide is capable of, initially, reducing and, ultimately, eliminating the fungus.[27,28]
It is important to mention that the results presented in this study were obtained under in vitro conditions, and may not accurately describe in vivo activity. Further studies are necessary to investigate the effect of these materials on bacteria and fungi in clinical application.
CONCLUSION
This study shows that MTA-Angelus has an effective antifungal property comparable to ProRoot MTA at concentrations of 50 and 100 mg/ml.
ACKNOWLEDGEMENT
This study was supported by the Iranian Center for Endodontic Research, Shahid Beheshti Medical University, Tehran, Iran.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sundqvist G, Figdor D, Persson S, Sjögren U. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:86–93. doi: 10.1016/s1079-2104(98)90404-8. [DOI] [PubMed] [Google Scholar]
- 2.Siqueira JF, Jr, Sen BH. Fungi in endodontic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:632–41. doi: 10.1016/S1079210404000046. [DOI] [PubMed] [Google Scholar]
- 3.Zbidi ND, Zaki A, Zouiten S, Boughzala A, Baccouche C. Prevalence of endodontic yeasts in periapical infections. Odontostomatol Trop. 2005;28:5–12. [PubMed] [Google Scholar]
- 4.Waltimo TM, Sen BH, Meurman JH, Ørstavik D, Haapasalo MP. Yeasts in apical periodontitis. Crit Rev Oral Biol Med. 2003;14:128–37. doi: 10.1177/154411130301400206. [DOI] [PubMed] [Google Scholar]
- 5.Torabinejad M, Watson TF, Pitt Ford TR. Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J Endod. 1993;19:591–5. doi: 10.1016/S0099-2399(06)80271-2. [DOI] [PubMed] [Google Scholar]
- 6.Ford TR, Torabinejad M, Abedi HR, Bakland LK, Kariyawasam SP. Using mineral trioxide aggregate as a pulp-capping material. J Am Dent Assoc. 1996;127:1491–4. doi: 10.14219/jada.archive.1996.0058. [DOI] [PubMed] [Google Scholar]
- 7.Hayashi M, Shimizu A, Ebisu S. MTA for obturation of mandibular central incisors with open apices: Case report. J Endod. 2004;30:120–2. doi: 10.1097/00004770-200402000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Ford TR, Torabinejad M, McKendry D, Hong CU, Kariyawasam SP. Use of mineral trioxide for repair of furcal perforations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:756–62. doi: 10.1016/s1079-2104(05)80313-0. [DOI] [PubMed] [Google Scholar]
- 9.Torabinejad M, Pitt Ford TR, McKendry DJ, Abedi HR, Miller DA, Kariyawasam SP. Histologic assessment of mineral trioxide aggregate as a root-end filling in monkeys. Int Endod J. 2009;42:408–11. doi: 10.1111/j.1365-2591.2009.01556.x. [DOI] [PubMed] [Google Scholar]
- 10.Sarkar NK, Caicedo R, Ritwik P, Moiseyeva R, Kawashima I. Physicochemical basis of the biologic properties of mineral trioxide aggregate. J Endod. 2005;31:97–100. doi: 10.1097/01.don.0000133155.04468.41. [DOI] [PubMed] [Google Scholar]
- 11.Tanomaru-Filho M, Tanomaru JM, Barros DB, Watanabe E, Ito IY. In vitro antimicrobial activity of endodontic sealers, MTA-based cements and Portland cement. J Oral Sci. 2007;49:41–5. doi: 10.2334/josnusd.49.41. [DOI] [PubMed] [Google Scholar]
- 12.Chng HK, Islam I, Yap AU, Tong YW, Koh ET. Properties of a new root-end filling material. J Endod. 2005;31:665–8. doi: 10.1097/01.don.0000157993.89164.be. [DOI] [PubMed] [Google Scholar]
- 13.Komabayashi T, Spångberg LS. Comparative analysis of the particle size and shape of commercially available mineral trioxide aggregates and Portland cement: A study with a flow particle image analyzer. J Endod. 2008;34:94–8. doi: 10.1016/j.joen.2007.10.013. [DOI] [PubMed] [Google Scholar]
- 14.Duarte MA, Demarchi AC, Yamashita JC, Kuga MC, Fraga Sde C. PH and calcium ion release of 2 root-end filling materials. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:345–7. doi: 10.1067/moe.2003.12. [DOI] [PubMed] [Google Scholar]
- 15.Xavier CB, Weismann R, de Oliveira MG, Demarco FF, Pozza DH. Root-end filling materials: Apical microleakage and marginal adaptation. J Endod. 2005;31:539–42. doi: 10.1097/01.don.0000152297.10249.5a. [DOI] [PubMed] [Google Scholar]
- 16.Lolayekar N, Bhat SS, Hegde S. Sealing ability of ProRoot MTA and MTA-Angelus simulating a one-step apical barrier technique-an in vitro study. J Clin Pediatr Dent. 2009;33:305–10. doi: 10.17796/jcpd.33.4.gp472416163h7818. [DOI] [PubMed] [Google Scholar]
- 17.Juarez Broon N, Bramante CM, Assis GF, Bortoluzzi EA, Bernardineli N, Moraes IG, et al. Healing of root perforations treated with Mineral Trioxide Aggregate (MTA) and Portland cement. J Appl Oral Sci. 2006;14:305–11. doi: 10.1590/S1678-77572006000500002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tanomaru JM, Tanomaru-Filho M, Hotta J, Watanabe E, Ito IY. Antimicrobial activity of endodontic sealers based on calcium hydroxide and MTA. Acta Odontol Latinoam. 2008;21:147–51. [PubMed] [Google Scholar]
- 19.Ribeiro CS, Kuteken FA, Hirata Júnior R, Scelza MF. Comparative evaluation of antimicrobial action of MTA, calcium hydroxide and Portland cement. J Appl Oral Sci. 2006;14:330–3. doi: 10.1590/S1678-77572006000500006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Monteiro Bramante C, Demarchi AC, de Moraes IG, Bernadineli N, Garcia RB, Spångberg LS, et al. Presence of arsenic in different types of MTA and white and gray Portland cement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:909–13. doi: 10.1016/j.tripleo.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 21.Koulaouzidou EA, Economides N, Beltes P, Geromichalos G, Papazisis K. In vitro evaluation of the cytotoxicity of ProRoot MTA and MTA Angelus. J Oral Sci. 2008;50:397–402. doi: 10.2334/josnusd.50.397. [DOI] [PubMed] [Google Scholar]
- 22.Al-Nazhan S, Al-Judai A. Evaluation of antifungal activity of mineral trioxide aggregate. J Endod. 2003;29:826–7. doi: 10.1097/00004770-200312000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Sipert CR, Hussne RP, Nishiyama CK, Torres SA. In vitro antimicrobial activity of Fill Canal, Sealapex, Mineral Trioxide Aggregate, Portland cement and EndoRez. Int Endod J. 2005;38:539–43. doi: 10.1111/j.1365-2591.2005.00984.x. [DOI] [PubMed] [Google Scholar]
- 24.Mohammadi Z, Modaresi J, Yazdizadeh M. Evaluation of the antifungal effects of mineral trioxide aggregate materials. Aust Endod J. 2006;32:120–2. doi: 10.1111/j.1747-4477.2006.00032.x. [DOI] [PubMed] [Google Scholar]
- 25.Torabinejad M, Hong CU, Pitt Ford TR, Kettering JD. Antibacterial effects of some root end filling materials. J Endod. 1995;21:403–6. doi: 10.1016/s0099-2399(06)80824-1. [DOI] [PubMed] [Google Scholar]
- 26.Estrela C, Sydney GB, Bammann LL, Felippe Júnior O. Mechanism of action of calcium and hydroxyl ions of calcium hydroxide on tissue and bacteria. Braz Dent J. 1995;6:85–90. [PubMed] [Google Scholar]
- 27.Barbosa SV, Spangberg LS, Almeida D. Low surface tension calcium hydroxide solution is an effective antiseptic. Int Endod J. 1994;27:6–10. doi: 10.1111/j.1365-2591.1994.tb00221.x. [DOI] [PubMed] [Google Scholar]
- 28.Siqueira JF, Jr, Rôças IN, Lopes HP, Magalhães FA, de Uzeda M. Elimination of Candida albicans infection of the radicular dentin by intracanal medications. J Endod. 2003;29:501–4. doi: 10.1097/00004770-200308000-00003. [DOI] [PubMed] [Google Scholar]


