Abstract
Hemangiomatous ameloblastoma (HA), which is a rare ameloblastic variant, is presented in a 15-year-old boy in the maxillary right molar region associated with unerupted canine and premolars. Radiologic and computed tomographic analysis was suggestive of cystic lesion. An histology picture confirmed the diagnosis of HA. There are less than eight cases documented in the literature and mostly are in the middle age with mandibular location. This is first ever reported case of HA in a 15-year-old boy with maxillary location. Due to less number of documented cases and no long-term follow-ups, clinical behavior and prognosis of this lesion are uncertain. In this case report, the clinical, histological, and radiographic features of HA are presented.
Keywords: Ameloblastoma variants, hemangiomas, unilocular radiolucency, vascular ameloblastoma
INTRODUCTION
Ameloblastomas in young people (i.e., 19 years old and younger) are thought to be rare. They account for approximately 10–15% of all reported cases of ameloblastoma.[1] However, there is less accurate information available regarding its prevalence. It is a true neoplasm known for its destructive and recurrent behavior. On the basis of clinical and biological behavior, it is principally categorized into three types: solid or multicystic, unicystic, and peripheral. There are various numbers of histopathological patterns of ameloblastoma. The follicular and plexiform patterns are the main histologic types. Commonly encountered histologic variants are acanthomatous and granular cell types. Other less commonly encountered histologic patterns include desmoplastic ameloblastoma, basal cell ameloblastoma, clear cell ameloblastoma, and unicystic ameloblastoma[2] Although with the exception of desmoplastic and unicystic type, histopathological variation does not carry significance in terms of prognosis and biological behavior.[3] The hemangiomatous ameloblastoma (HA) was originally described as an ameloblastoma in which part of the tumor contained spaces filled with blood or large endothelial-lined capillaries.[4] Lesions with similar histologic features that probably represented the same entity were documented in the early literature as ameloblastic hemangiomas,[5] adamantinohemangiomas,[6,7] and hemangio ameloblastomas.[8]
To the best of our knowledge, there are less than eight cases documented earlier in the literature.[7–12] Other reported cases are mostly in the mandible and in the middle age. This is the first case of HA in a child with maxillary location. This article presents a rare form of ameloblastoma with clinical, radiological, and histological features consistent with those of an HA which will contribute to the literature in studying biological behavior and prognosis of the lesion.
CASE REPORT
A 15-year-old boy presented with a right maxillary swelling 3.5 cm in the width and 3 cm in length with a duration of 5 months with a history of gradual enlargement of the right jaw and the swelling had displaced the lateral wall of the nose on the right side up to the nasal septum. The patient noticed the swelling of face 5 months ago and pain on palpation. The swelling also encroached onto the upper alveolar process on the right side and adjoining hard palate up to the midline. The medical history was insignificant. Routine blood investigations such as hemogram, bleeding, and clotting time were normal. An intraoral examination revealed a firm, smooth, and nonfluctuating swelling that was bony hard in consistency and fixed to the right maxilla. The upper permanent canine, first and second premolar teeth were missing on the right side while deciduous canine, first and second molar were present and they were mobile [Figure 1].
Figure 1.

Facial aspect showing retained deciduous teeth and swelling
RADIOGRAPHIC FINDINGS
Radiographic examinations revealed well-defined radiolucency with sclerotic border in the maxillary canine region extending up to second molar surrounding the second premolar tooth bud. Permanent canine and premolars were unerupted and deciduous canine, first molars and second molar were retained [Figures 2 and 3]. Radiograph of the paranasal sinuses [Figure 4] showed a hazy right maxillary antrum with expansion and thinning of all its bony walls with the right upper canine tooth, pushed up to the floor of the orbit. Contrast enhanced computed tomography (CECT) of face suggestive of a well-defined expansile cystic lesion with 3.7 cm in width, 3 cm in length, and 3 cm in depth with a CT value in the range of 15– 25 HU with corticated margin arising from alveolar arch, maxilla, and hard palate on the right side with tooth lying within it. The lesion is extending from the hard palate inferiorly and up to the floor of orbit superiorly leading to displacement of septum toward its side with bilateral maxillary sinusitis giving the impression of dentigerous cyst [Figure 5].
Figure 2.

OPG showing well-defined radiolucency with sclerotic border in the maxillary canine region extending up to second molar surrounding the second premolar tooth bud
Figure 3.
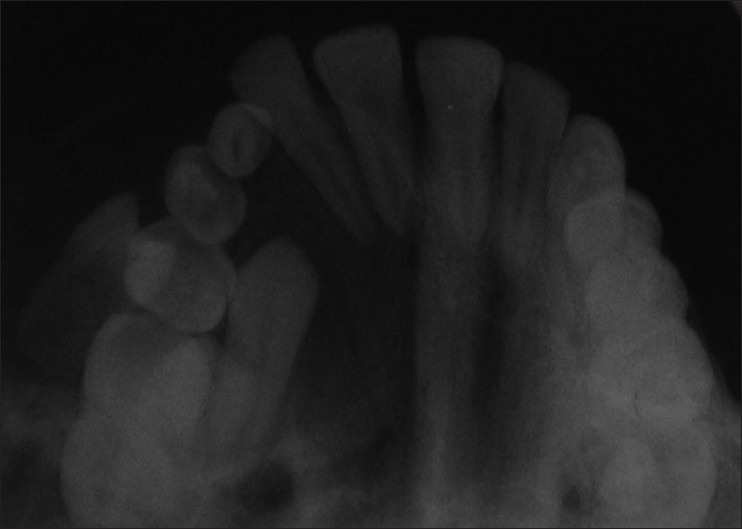
Occlusal radiograph showing permanent unerupted canine and retained deciduous teeth
Figure 4.

Hazy right maxillary antrum with expansion and thinning of all its bony walls
Figure 5.

Well-defined expansile cystic lesions with size with corticated margin arising from alveolar arch, maxilla, and hard palate on the right side with tooth lying within it
The lesion was operated on under general anesthesia by the Caldwell-Luc approach and enucleated along with removal of the displaced canine tooth and one premolar. The cystic lesion was subjected to the histopathological examination which revealed cystic lumen with odontogenic epithelial lining proliferating as in follicular ameloblastoma with a prominent vascular component. The ameloblastoma consisted of anastomosing cords and sheets of odontogenic epithelium in a loosely arranged stroma. The peripheral cells of the anastomosing cords exhibit columnar or cuboidal ameloblast-like cells. The vascular component consisted of numerous endothelial-lined channels and large blood-filled spaces in the stromal component [Figures 6 and 7]. On the basis of these histopathological findings, the lesion was diagnosed as Hemangiomatous ameloblastoma. The patient is under follow-up since enucleation for the past 6 months [Figures 8 and 9].
Figure 6.
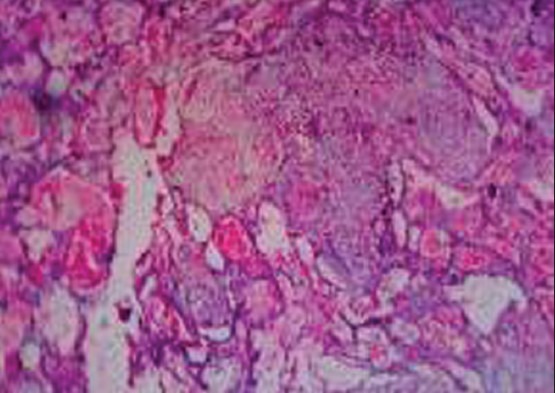
The ameloblastoma consisted of anastomosing cords and sheets of odontogenic epithelium in a loosely arranged stroma
Figure 7.
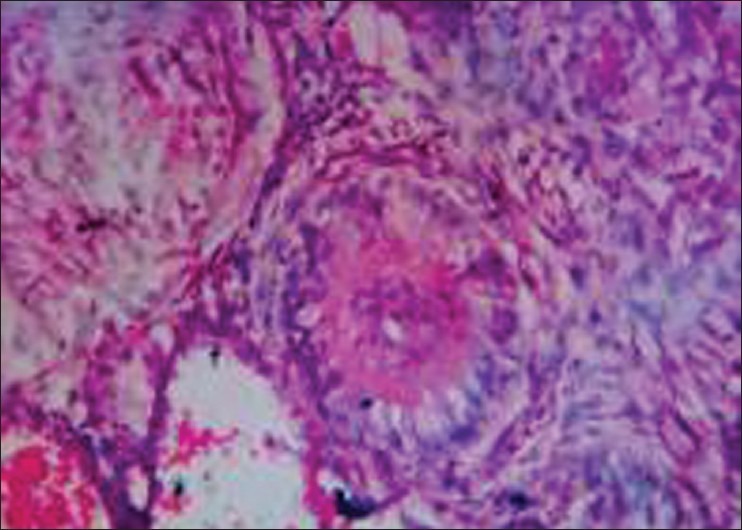
Cystic lumen with odontogenic epithelial lining proliferating as in follicular ameloblastoma with a prominent vascular component
Figure 8.

Postop facial aspect
Figure 9.

Post-op OPG
DISCUSSION
The term “hemangio ameloblastoma” is used to describe the variant of ameloblastoma in which stromal connective tissue is largely replaced by vascular tissue. There are numerous schools of thoughts regarding the pathogenesis of the vascular component of HA but whether the vascular component of the HA is part of the neoplastic process, represents a separate neoplasm, or is a hamartomatous malformation has not been satisfactorily resolved.
The stroma part of ameloblastoma consists of loose myxoid tissue which can undergo degeneration so blood vessels are left without any support. They become enlarged, and rupture leading to escape blood into empty stromal space.[5]
A traumatic incident such as a tooth extraction may provide a stimulus required for proliferation of epithelial cell rests in the periodontal ligament and subsequent tumor development.[6] Tissue damage is usually followed by repair, and this involves the formation of the granulation tissue in which proliferating endothelial cells and new capillaries are prominent. A disturbance in the repair of neoplastic odontogenic tissue may result in excessive granulation tissue formation or the development of an abnormal vascular component.
At the time of tooth development, numerous blood vessels furnish supply to outer enamel epithelium. It is probable that blood vessels are abnormally induced to become part of tumor or abnormal angiogenesis due to excess inductive influence can lead to overgrowth of vascular elements. It has been suggested that the HA represents a collision tumor. In this type, two separate tumors grow in the same area and collide with each other and the tumor elements intermingle.[8]
The HA observed here differs histologically and radiologically from a conventional ameloblastoma. Histologically, it consists of an ameloblastoma with a prominent vascular component while its conventional radiologic features are nonspecific.
A CT scan clearly demonstrates cystic features in this tumor, such as its expansile nature and soft tissue contents. According to Smith,[10] this HA is similar histopathologically to conventional ameloblastoma and not a distinct entity. Vascular supply to this tumor is variable. Whether it is hamaratomatous malformation or a separate neoplasm is not clear. Its vascular features are, however, well documented, and vascular variants of such neoplasm are accepted as separate histologic entities. Examples are the angiomatoid malignant fibrous histiocytoma[13] and the telangiectatic osteosarcoma.[14] The angiomatoid malignant fibrous histiocytoma combines the features of both a fibrohistiocytic tumor and a vascular tumor, while the telangiectatic osteosarcoma contains large blood-filled spaces, thrombus formation, organization, and massive areas of necrosis.
CONCLUSION
Vascular lesions of the jaws are of much concern as fatality is documented following minor procedures. Cases have been reported in the literature as early in 1933 in which improper management led to rapid, fatal exsanguinations.[15] The biologic behavior of HA is thought to be similar to that of the conventional ameloblastoma, but because a few cases have been reported with no long-term follow-up so the pathogenesis and clinical features are not yet fully understood and biologic behavior cannot be predicted. Whether it should be given the status of distinct entity or just a variant of ameloblastoma, further research is needed.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kessler A, Dominguez FV. Ameloblastoma in childhood. J Oral Maxillofac Surg. 1986;44:609–13. doi: 10.1016/s0278-2391(86)80071-4. [DOI] [PubMed] [Google Scholar]
- 2.Krammer IR, Pindborg JJ, Shear M. Histological typing of odontogenic Tumors. Berlin: Springer-Verlag; 1992. pp. 11–4. [Google Scholar]
- 3.Waldron CA, Small IA, Silverman H. Clear cell ameloblastoma: An odontogenic carcinoma. J Oral Maxillofac Surg. 1985;43:707–17. doi: 10.1016/0278-2391(85)90198-3. [DOI] [PubMed] [Google Scholar]
- 4.Stones HH. Oral and dental diseases. 3rd ed. Edinburg and London: E & S Livingstone; 1957. p. 836. [Google Scholar]
- 5.Shafer WY, Hine MK, Levy BM. A text book of oral pathology. 4th ed. Philadelphia: WB Saunders; 1983. [Google Scholar]
- 6.Thoma KH. Oral pathology. Louis: CV Mosby; 1994. p. 294. [Google Scholar]
- 7.Aisenberg MS. Adamantinohemangioma. Oral Surg Oral Med Oral Pathol. 1950;3:798–801. doi: 10.1016/0030-4220(50)90277-5. [DOI] [PubMed] [Google Scholar]
- 8.Oliver RT, McKenna WF, Shafer WY. Hemangioameloblastoma; report of a case. J Oral Surg Anesth Hosp Dent Serv. 1961;19:245–8. [PubMed] [Google Scholar]
- 9.Villa VG. Hemangioma of the cavernous type associated with ameloblastoma (ameloblastic hemangioma) J Oral Surg Anesth Hosp Dent Serv. 1960;18:429–31. [PubMed] [Google Scholar]
- 10.Smith JF. The controversial Ameloblastoma. Oral Surg Oral Med Oral Pathol. 1968;26:45–75. doi: 10.1016/0030-4220(68)90223-5. [DOI] [PubMed] [Google Scholar]
- 11.Van Rensburg LJ, Thompson IO, Kruger HE, Norval EJ. Hemangiomatous ameloblastoma: Clinical, radiologic, and pathologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:374–80. doi: 10.1067/moe.2001.111761. [DOI] [PubMed] [Google Scholar]
- 12.Tamgadge AP, Sirur DG, Bhalerao SS, Pariera T, Tamgadge SA. Hemangiomatous Ameloblastoma: A case report of a rare variant of ameloblastoma. Int J Contemp Dent. 2010;2:16–9. [Google Scholar]
- 13.Enzinger FM. Angiomatoid malignant fibrous histiocytoma: A distinct fibrohistiocytic tumour of children and young adults simulating a vascular neoplasm. Cancer. 1979;44:2147–57. doi: 10.1002/1097-0142(197912)44:6<2147::aid-cncr2820440627>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 14.Matsuno T, Unni KK, Mcleod R, Dahlin D. Telangiectatic osteosarcoma. Cancer. 1976;38:2538–47. doi: 10.1002/1097-0142(197612)38:6<2538::aid-cncr2820380643>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 15.Van Rensburg LJ, Nortje CJ, Wood RE. Advanced imaging in evaluation of a central mandibular haemangioma. Dentomaxillofac Radiol. 1994;23:111–6. doi: 10.1259/dmfr.23.2.7835502. [DOI] [PubMed] [Google Scholar]


