Abstract
The number of day-care surgeries is increasing every day. The boundaries of day-care surgeries are being redefined on a continual basis. Multi-dimensional benefits to the patient, hospital and national economy are the driving forces behind the changing scenario on the horizon of day surgery. The literature search included Google, medlinx, pubmed and medline. We have attempted to look at the controversies in patient selection with comorbidities, pre-operative assessment and an acceptable ASA grade of patients. An attempt is also made to look at suitable surgical procedures, a pathway of introducing procedures, which are still complex and specialist procedures in challenging environment. The techniques of general anaesthesia, central neuraxial blocks, regional nerve blocks with indwelling catheters and monitoring techniques are deliberated upon. Finally the most important post-operative issues of discharge criteria, including recovery after spinal anaesthetic, oral fluid intake, voiding and travel after day surgery, are considered.
Keywords: Ambulatory surgery, anaesthetic techniques, controversies, day surgery, discharge, patient selection, surgical procedures
INTRODUCTION
International Association of Ambulatory Surgery defines day-care surgery as ‘An operation or procedure, an office or outpatient operation/procedure, where the patient is discharged on the same working day’.
The boundaries of day-care surgery are redefined exponentially with time. The rapidly changing financial situation in the world has led to the increase in the incidence of ambulatory surgery. The advances in surgery, anaesthesia and pain management have allowed huge expansion of this modality of care with a consequent reduction in the need for hospitalization. The target for day surgeries in the USA and UK are 80% and >75% of the total surgeries, respectively. Even though data are not available for India, there is huge potential in view of a massive population of 1.2 billion and recent huge expansion in the private sector has created an opportunity for expansion in day surgery in India.[1–3]
The advantages of day case surgeries are to patient, hospital and insurance companies. They include minimal psychological disturbances for the patient, especially children, economical with reduced requirement of nursing and medical supervision and hospital services allowing more number of patients to be treated and finally consequent reduction in the risk of hospital-acquired infection and venous thromboembolism (VTE).
Few controversies related to day case surgery are under the following: patient selection, surgical procedures, preparation, anaesthetic management, recovery and organizational issues.
PATIENT SELECTION
Most of the patients are suitable for day surgery. With the current in-patient procedures, we should question ourselves if there are any ways with which they can be managed as day cases.
Age
It is now a routine to accept full-term infants of more than 1 month age and 60 weeks post-conception age in premature born for day case procedures. Post-operative apnoea is a serious complication in infants with recent episodes of apnoea, cardiac or respiratory disease, family history of sudden infant death syndrome and adverse social circumstances who should be admitted for overnight observation with close monitoring. Children are ideal for day surgery as there is minimal separation from parents and risk of hospital-acquired infection.[1,2,4] Federation of ambulatory surgery association has observed that there is no significant relationship with pre-existing diseases and incidence of post-operative complications; elderly with multiple co-morbidities are also acceptable for day surgery.[2]
Hypertension
The benefits of deferring surgery solely for the purpose of control of a possibly isolated high BP of up to 160/100 mmHg are not clear. Uncontrolled hypertension in itself is a minor risk factor for peri-operative outcomes. There is neither level 1 evidence to support the hypothesis that pre-operative control of arterial blood pressure is beneficial in reducing adverse events nor that moderate hypertension is a predictor of adverse outcomes. Even though cardiovascular complications are common in hypertensive patients, they are of limited consequence. Pre-operative blood pressure of more than 160/100 mmHg would require further investigation and treatment.
Intra-operative hypotension is more frequent in patients taking angiotensin-converting enzyme (ACI) inhibitors and angiotensin II receptor antagonists. It is common for all antihypertensive agents to be continued except ACE inhibitors. As intra-operative hypotension is more frequent, whether ACE inhibitors and angiotensin blocking drugs should be continued as before or stopped is still controversial. The benefits of continuing medications include cardio protection, improved renal function and reduced sympathetic response and the fact that hypotensive consequences are generally mild and respond to usual corrective measures.[5,6]
Obesity
It is defined as the body mass index (BMI) of more than 30 kg/m2. Department of health in UK suggests that patients with BMI up to 40 kg/m2 are also suitable for day surgery. There is little evidence to support the view that obese patients suffer clinically relevant increased morbidity after day surgery. The incidence of complications during the peri-operative period increases with increasing BMI. These problems occur in the first 3- to 4-hour post-operative period, can be easily resolved and later patient can be discharged. The day surgery with its short duration anaesthetics and early mobilization are especially suitable for obese patients.[7]
Obstructive sleep apnoea
The main problems with obstructive sleep apnoea (OSA) patients are as follows: airway management – increased risk of difficult mask ventilation and intubation, there is increased risk of post-operative obstruction and hypoxia in airway surgery and residual sedation with increased risk of post-operative apnoea. Any anaesthetic techniques including local or regional anaesthesia, total intravenous anaesthesia or general anaesthesia with sevoflurane, using paracetamol, NSAIDS, remifentanil, are appropriate if used judiciously.
The type of surgery whether for correction of OSA or coincidental surgery, severity of OSA, presence of comorbidity, availability of nasal continuous positive airway pressure device, adequacy of post-operative observation, ability to manage complications and patient's support system at home determine suitability for day-care anaesthesia. An anaesthetist should individually assess patients with severe symptoms and comorbidities regarding suitability for day surgery depending on the surgery and the anaesthetic planned.[6,8,9]
Patients on anti-platelet and anti-coagulant drugs
Patients with VTE in last 3 months, recurrent VTE and mechanical mitral valves are not suitable for day-care surgery. A discussion with cardiologist and haematologist is essential in patients with mechanical aortic valve, with atrial fibrillation and arterial thrombus within a month for their peri-operative care planning. Pre-operative assessment allows us to identify patients with anticoagulant drugs and advise them regarding drug management.[6]
Patients with upper respiratory infection
What should be done with day case patients with colds?
The history of reactive airways, copious secretions, nasal congestion, smoking or productive cough favours post-ponement. The available evidence suggests that increased upper airway reactivity may lead to increase in intra-operative complications.
Anaesthetic and surgical factors and probability of complications
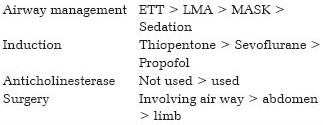
(Reproduced from booklet ‘Ten dilemmas in pre-operative assessment for day surgery’ (page 34), published by British Association of Day Surgery (available from www.bads.co.uk), 2009 with permission)
Consider postponing the procedure for 3 weeks in patients with upper respiratory infection (URI) based on the anaesthetic necessities and surgical factors shown in Table 1. It is suggested to assess carefully for the presence of lower respiratory infections before going ahead with surgery for patients with URI.[6]
Table 1.
Investigations depending on patient's disease type and severity
Diabetes
Many patients with diabetes need surgical procedures that are suitable for day surgery. A recent consensus statement concludes ‘the usefulness of strict control of blood glucose concentration (i.e. a blood glucose level of <8 mmol/l) during the peri-operative period is uncertain in patients with diabetes or acute hyperglycaemia who are undergoing surgery’.[10] Tight glycaemia control is not necessary in stable diabetics and in those requiring up to 8 hours of peri-operative fasting.
The combination of less invasive surgical techniques, modern anaesthetic agents with less post-operative nausea and vomiting and improved patient understanding of their diabetic control mean many patients can be safely managed as day case. Minor and intermediate procedures are suitable for day case surgery. Major procedures with increased risk of post-operative nausea and vomiting and delay in oral intake will increase the risk of unplanned admission. Choose anaesthetic techniques that reduce post-operative nausea and vomiting. Local or regional anaesthesia has the advantage of minimizing metabolic disturbance and enabling early return to oral intake. Type 1 diabetic patients have more variable blood sugar than type 2 patients peri-operatively. Diabetic patients should be the first on the list allowing sufficient time for glycaemic stability. Type 1 and 2 diabetic patients with glycosylated haemoglobin (HbA1C) less than 8.5% are acceptable. Diabetic patients with comorbidity should be assessed similar to any non-diabetic patient.[2,6,10]
Haematological disorders
A coordinated planning and liaison with haematologist is required for better outcome. The recommendations for safe platelet counts in adults include
dentistry procedures ≥30×109/L
minor surgery ≥50×109/L
major surgery/neuraxial blocks ≥80×109/L.
Neuromuscular disorders
There is an increased risk of peri-operative respiratory complications during day surgery in patients with neuromuscular disorders. The patients with motor neuron disorders are at increased risk of aspiration and developing respiratory failure. In patients with peripheral neuropathies, the pre-anaesthetic assessment allows for documentation of neurological impairment and enables comparison in the post-operative period when regional anaesthetic is planned. An overnight stay is necessary in the event of peri-operative severe respiratory problems for careful observation. Patients with Myasthenia gravis requiring general anaesthesia are not suitable candidates for day surgery as recurrent aspirations can occur. Similarly patients with muscular dystrophy requiring general anaesthesia have to stay overnight for observation of respiratory function.
But if day-care surgery is suggested, regional or local anaesthesia is a safer option in patients with respiratory or bulbar involvement. General anaesthesia with neuromuscular blockade may have prolonged or unpredictable effects.[6]
Alcohol abuse
The post-operative alcohol consumption can increase the opioid-induced respiratory depression. Few patients who abuse alcohol may pose problems to the day surgery unit including higher risk of peri-operative complication.[11] Following alcohol abstinence, platelet function/bleeding time can recover in 1-2 weeks and improved wound healing after 8 weeks.
American society of anaesthesiologists classification
American Society of Anaesthesiologists (ASA) class 1 and 2 patients are to be considered for ambulatory care including uncomplicated obese and elderly patients. Few ASA 3 and 4 patients are also suitable for day surgery. Serious health problems, psychiatric disorders and mental/cognitive deficits are not necessarily contraindications.[2,12]
Surgical factors
The procedure with risk of serious complications like haemorrhage and cardiovascular instability are unsuitable for day-care surgeries. Post-operative pain and nausea and vomiting must be easily controllable by the use of combination of oral medications and local anaesthetic techniques. The procedure should allow the patient to resume oral intake within few hours and be able to mobilize before discharge although full mobilization is not always necessary.[2,12] The examples of advanced procedures successfully carried out in ambulatory setting are
laparoscopic major gastrointestinal surgery such as cholecystectomy, fundoplication, gastric banding (obese)
laparoscopic major gynaecology including hysterectomy
breast cancer surgery
cruciate ligament repair
major plastic surgeries like breast reduction, liposuction.
Day surgery for urgent procedures
Patients presenting with acute conditions requiring urgent surgery also can be efficiently treated as day cases via a semi-elective pathway. This reduces the likelihood of repeated postponement in the main hospital (prioritization). Robust day surgery process is essential.[2,13] These urgent procedures include manipulation of fractures, tendon repairs, laparoscopic ectopic pregnancy, evacuation of retained products of conception, laparoscopic appendicectomy or incision and drainage and similar procedures.
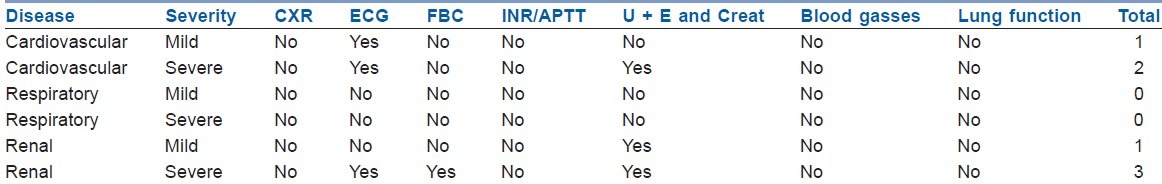
Pre-op investigations
The National Institute of Clinical Excellence (NICE) guidelines can be used to conduct pre-operative investigations. However, one study has showed no difference in the outcomes of day surgery even when all investigations were omitted.[14]
(Reproduced from Organisational issues in pre-operative assessment for day surgery, British Association of day surgery (available from www.bads.co.uk), 2010, with permission)
One-stop clinic
An early pre-operative assessment is necessary with shorter time between ‘decision to treat’ and surgery. At one-stop clinic, patients will have access for all consultations, investigations and other preparations. It eliminates the second hospital visit and gives more time for pre-op investigation or optimization. It also provides a pool of patients should a cancellation arise, early appointment to another patient is generally popular. The disadvantages include planning of resources (staff/facilities) to deal with unpredictable demand from outpatient clinics. Careful planning allows us to predict which slots should be available for one-stop patients and which can be reserved for scheduled appointments.[15]
Pre-operative sedation, amnesic and anxiolytic drugs can be administered safely without clinically significant delays in recovery times even after short procedures. Ketamine can be safely used in mentally disabled patients without increase in side effects.[1]
Anaesthetic techniques
The anaesthetic techniques chosen should have minimum stress and provide maximum comfort to patient in addition to minimal residual effects. A multimodal peri-operative analgesia with paracetamol, NSAIDS, opiates and local anaesthetics should be a part of anaesthesia.
Total intravenous anaesthesia or inhalational anaesthesia
Total intravenous anaesthesia (TIVA) in day surgery is advantageous because of rapid recovery without agitation and behavioural disorders. It is simple to use without the need for sophisticated gas delivery systems and scavenger equipment. It avoids the risks of failure of regional blocks, residual paralysis and less chance of side effects like post-operative nausea and vomiting. It also avoids environmental pollution and also avoids the possibility of malignant hyperthermia. The disadvantages include pump failure, disconnection and awareness.[2,12] The use of N2O is associated with increased risk of post-operative nausea and vomiting.
The inhalational agents sevoflurane, desflurane and isoflurane have advantages of amnesia and safety in multi-allergy patients. Monitoring their end-tidal concentration provides indication of depth of anaesthesia which has no equivalent in TIVA. Sevoflurane and desflurane are associated with rapid emergence than propofol. Desflurane emergence is faster than sevoflurane even in prolonged procedures especially in obese patients.[2,12]
Use of laryngeal mask airway
The face mask is an alternative only if the patient is fasted, as it does not provide protection against aspiration. The laryngeal mask airway (LMA) is the most commonly used airway devices in day surgery. According to the UK National audit project 4 first generation LMAs carry higher incidence of aspiration. Second-generation LMAs like I-gel-, Proseal providing additional port for gastric emptying are more safer. The use of LMA may not need muscle relaxants and are less invasive to airway than intubation. Post-operative airway problems like coughing or laryngospasm are minimal. The main disadvantage is that the protection against aspiration is less compared to endotracheal tube. However, there is still some role for endotracheal intubation in patients with obesity, pregnancy, gastro-oesophageal reflux disease and surgery in prone position.
Central neuraxial blocks
Spinal or caudal anaesthesia are suitable in lower extremity, abdominal and gynaecological procedures. The use of sub-clinical doses of local anaesthetics and opioid adjuncts has a superior recovery profile. Isobaric prilocaine may be well suited for day surgery. The advantages are rapid onset, offset and ease of administration. It is cheaper, have less side effects including fivefold reduction in post-operative nausea/vomiting compared with GA. The technique of selective spinal anaesthesia using low dose lidocaine 10 mg and sufentanil 10 mcg for gynaecological laparoscopic procedures has better results compared with desflurane and nitrous oxide.[1] The disadvantage of post-dural puncture headache (0-2%) can be reduced with 25 or 27 G pencil point needles. Transient neurological symptoms are more common in lithotomy or knee arthroscopy position. These symptoms are more with lignocaine than procaine and mepivacaine. Post-operative pain is the most significant complaint among ASA-1, young adults, larger BMI, prolonged surgeries including orthopaedic, urologic and plastic surgeries and hence multimodal analgesia recommended.[1,2,12]
Regional anaesthetic techniques
The advantages include excellent anaesthesia and post-operative pain relief. It requires less sedation with minimal cognitive dysfunction, hence especially useful in elderly patients and less post-operative nausea and vomiting. Full recovery of the block is not necessary and may even be beneficial because of good pain relief. Patients must be clearly explained with written instructions about the duration of the block, protection of limb and ensure adequate support is available.[2,12]
Post-operative discharge is based on the following three phases of recovery:
Phase 1. Ready to go toward from recovery - patient is awake, pain is controlled. Alderete score is useful here.
Phase 2. Home readiness - post-anaesthesia discharge scoring system (PADSS) is used.
Phase 3. Late recovery – full physiological and psychological recoveries may take weeks or months.
Following spinal anaesthetic, the patient should have normal perianal sensation, ability to plantar flex foot to pre-operative level and proprioception of big toe before discharge to home.
Travel after day surgery
Current evidence does not support specific limitation on the journey period. Patients willing to accept long journeys should be permitted. Patients should have access to emergency care nearer to their home. It is common for patients to travel several hundred miles after day surgery in North America and Europe.[16]
CONTROVERSIES
Oral fluid intake and voiding before discharge is no longer enforced. Mandatory drinking may in fact provoke nausea and vomiting. With regard to voiding, blockade of sympathetic nerve supply to bladder and urethra may cause retention of urine. Micturition reflex returns on regression of sub-arachanoid block below the S-3 level. Hence, in patients with low risk of retention, voiding before discharge is unnecessary.[1,12]
CONCLUSION
There is an explosion in the number of day surgery procedures conducted in both developed and developing countries. The advances in anaesthesia, surgery and monitoring technology have allowed increasingly complex surgeries being performed on patients with multiple co-morbidities. There are several controversial issues in selection of patients, surgical procedures and organization for day surgery. In future, the ambulatory care will reach people in geographically distant areas as well.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Harsoor SS. Changing concepts in anaesthesia for day case surgery. Indian J Anaesth. 2010;54:485–8. doi: 10.4103/0019-5049.72635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verma R, Alladi R, Jackson I, Johnston I, Kumar, Page R, et al. Guide lines – day case and short stay surgery: 2. Anaesthesia. 2011;66:417–34. doi: 10.1111/j.1365-2044.2011.06651.x. [DOI] [PubMed] [Google Scholar]
- 3.Naresh T. Row: Progress of day surgery in India. Ambul Surg. 2010;16:15–6. [Google Scholar]
- 4.Collins CE, Everett CL. Challenges in paediatric ambulatory anaesthesia: Kids are different. Anesthesiol Clin. 2010;28:315–28. doi: 10.1016/j.anclin.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 5.Smith I, Jackson I. Beta- blockers, calcium channel blockers, angiotensin converting enzyme inhibitors and angiotensin receptors; should they be stopped or not before ambulatory anaesthesia? Curr Opinion Anaesthesiol. 2010;23:687–90. doi: 10.1097/ACO.0b013e32833eeb19. [DOI] [PubMed] [Google Scholar]
- 6.Montgomery J, Stocker M, Armstrong I, Lipp A, Carr C, Khaira H, et al. Ten dilemmas in pre-operative assessment for day surgery: British association of day surgery handbook. Norwich, UK: Coleman print; 2009. pp. 1–34. [Google Scholar]
- 7.Watson B, Healy J, Dhumale R, Houghton K, Turner B, Cahill H, et al. Ten dilemmas in day surgery: British association for day surgery handbook. 2006:1–18. [Google Scholar]
- 8.Jahan A. Annual meeting report 5: OSA: Thank god for guide lines? The news letters of society of Ambulatory Anaesthesia. 2007;22:11–3. [Google Scholar]
- 9.Stierer TL, Wright C, George A, Thompson RE, Wu CL, Collop N. Risk assessment of obstructive sleep apnea in a population of patients undergoing ambulatory surgery. J Clin Sleep Med. 2010;6:467–72. [PMC free article] [PubMed] [Google Scholar]
- 10.Joshi GP, Chung F, Ann Vann M, Ahmed S, Gan TJ, Goulson DT, et al. Society of ambulatory anaesthesia consensus statement on peri operative blood glucose management in diabetic patients undergoing ambulatory surgery. Anesth Analg. 2010;111:1378–87. doi: 10.1213/ANE.0b013e3181f9c288. [DOI] [PubMed] [Google Scholar]
- 11.Armstorng I, Dhumale R, Hammond C, Lipp A, Nash R, Smiths I, et al. Ten more dilemmas in day surgery: British association of day surgery hand book. Norwich, UK: Coleman print; 2008. pp. 1–24. [Google Scholar]
- 12.Reader J. Clinical ambulatory anaesthesia book. Cambridge, UK: Cambridge University Press; 2010. pp. 1–185. [Google Scholar]
- 13.Mayell AC, Barnes SJ, Stocker M. Introducing emergency surgery to the day care setting. The Journal of one Day Surgery. 2009;19:10–13. [Google Scholar]
- 14.Stocker M, Montgomery J, Lipp A, Olaye B, Lewis S, Armstrong I, et al. British association of day surgery. Norwich, UK: Coleman print; 2010. Organisational issues in pre-operative assessment for day surgery Hand book; pp. 1–33. [Google Scholar]
- 15.Stocker ME, Montgomery JE. Pre-operative assessment for day and short stay surgery. RCOA Bulletin. 2011;69:19–21. [Google Scholar]
- 16.Smith I. Selection criteria for day surgery. RCOA bulletin. 2011;9:22–3. [Google Scholar]


