Abstract
Purpose:
The objective of the study was to compare the performance of i-gel supraglottic airway with cLMA in difficult airway management in post burn neck contracture patients and assess the feasibility of i-gel use for emergency airway management in difficult airway situation with reduced neck movement and limited mouth opening.
Methods:
Prospective, crossover, randomized controlled trial was performed amongst forty eight post burn neck contracture patients with limited mouth opening and neck movement. i-gel and cLMA were placed in random order in each patient. Primary outcome was overall success rate. Other measurements were time to successful ventilation, airway leak pressure, fiberoptic glottic view, visualization of square wave pattern.
Results:
Success rate for the i-gel was 91.7% versus 79.2% for the cLMA. i-gel required shorter insertion time (19.3 seconds vs. 23.5 seconds, P=0.000). Airway leak pressure difference was statistically significant (i-gel 21.2 cm H20; cLMA 16.9 cm H20; P=0.00). Fiberoptic view through the i-gel showed there were less epiglottic downfolding and better fiberoptic view of the glottis than cLMA. Overall agreement in insertion outcome for i-gel was 22/24 (91.7%) successes and 2/24(8.3%) failure and for cLMA, 19/24 (79.16%) successes and 5/24 (16.7%) failure in the first attempt.
Conclusion:
The i-gel is cheap, effective airway device which is easier to insert and has better clinical performance in the difficult airway management of the airway in the post burn contracture of the neck. Our study shows that i-gel is feasible for emergency airway management in difficult airway situation with reduced neck movement and limited mouth opening in post burn neck.
Keywords: cLMA, difficult airway management, i-gel, post burn neck contracture
INTRODUCTION
i-gel airway is a novel and innovative supraglottic airway management device made up of a medical grade thermoplastic elastomer which is soft, gel like and transparent [Figure 1]. It creates a non-inflatable anatomical seal of the pharyngeal, laryngeal and perilaryngeal structures whilst avoiding the compression trauma that can occur with inflatable supraglottic airway devices. A supraglottic airway without an inflatable cuff has several potential advantages including easier insertion, minimal risk of tissue compression and stability after insertion. The buccal cavity stabilizer has a widened, elliptical, symmetrical and laterally flattened cross sectional shape (but still round airway channel), providing good vertical stability and axial strength upon insertion. This houses a standard airway and separate gastric channel.[1] An integrated gastric channel can provide early indication of regurgitation, facilitating venting of gas from the stomach and allows for passage of nasogastric tube to empty the stomach contents. The cLMA has been widely used as a routine airway for elective surgery and during cardiopulmonary resuscitation [Figure 2].[2] Growing concern over the ability to clean reusable devices effectively led to the increase in the use of single-use devices.[3]
Figure 1.
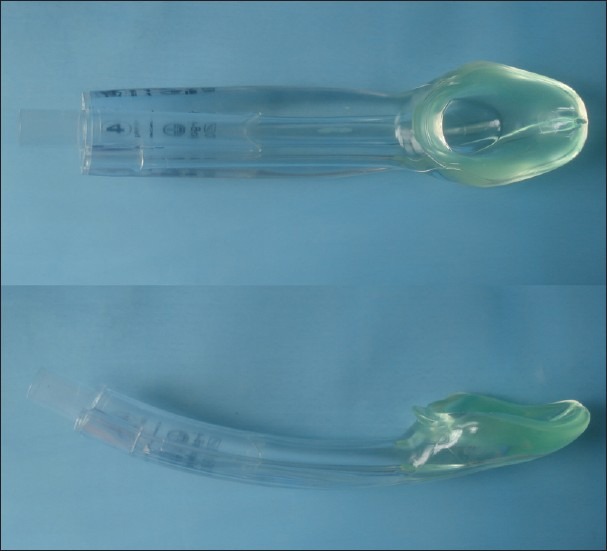
i-gel
Figure 2.
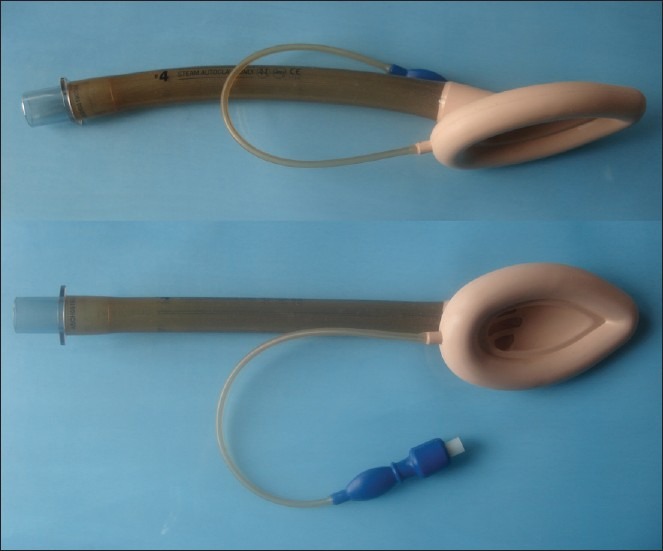
cLMA
Depending upon the material from which the cuff is made, they can absorb anaesthetic gases, which can lead to increased mucosal pressure.[4] The i-gel has been compared with other supraglottic airway devices for ease of insertion in airway training manikins and was found to be the best performing device tested.[5]
In an observational study by Richez et al., i-gel had a success rate of 97%.[6] In a recent study, i-gel had a first time success rate of 86% which improved to 97% following two attempts.[7] In this randomized cross-over study, we compared the i-gel supraglottic airway and cLMA with respect to first time and overall success rate of insertion, ease of insertion, leak pressure and fiberoptically determined laryngeal view of glottis in adult patients with post burn neck contracture undergoing general anaesthesia.
METHODS
After obtaining the Institutional Ethical committee's approval, 48 adults attending hospital during March 2009 till December 2010 were enrolled constituting both sexes, ASA-I and ASA-II, aged 16-50 years, weighing 35-75 kgs undergoing various surgical procedures like release of post burn contracture, debridement, split skin graft (SSG) and change of dressing for post burn neck contracture in whom laryngeal mask airway was considered appropriate.
With a type I error 0.05 and power of 80% we calculated that the sample size required was at least 21 in each group, based on a parallel group design.[8] Data were entered and statistical analysis was performed using SPSS software (version 16, SPSS Inc.., Chicago, IL, USA). The significance level was set at 0.05.
All the patients underwent pre-operative fasting according to the hospital guideline. The size of device used was decided by the anaesthetists based on the patient's bodyweight and manufactures’ recommendation. For the cLMA size 3 was used when the patients’ weight was <50 kg, size 4 for the patients weighing between 50-90 kg and size 5 for patients weighing more than 90 kgs. The i-gel size 3 was used for patients weighing between 30-60 kgs, size 4 between 50-90 kgs and size 5 for patients weighing >90 kgs. Both the devices were soaked with normal saline before use. In this crossover trial, both airways were inserted in each patient in random order. Patients were allocated randomly into one of the two groups using sequentially numbered sealed opaque envelop naming the airway device to be evaluated first, group I i-gel group and group II cLMA group. Randomization was performed by an envelop method. The insertions were performed by a single user who had experience of more than 1000 insertions of cLMA and at least 20 insertions for the i-gel.
A thorough pre anesthetic evaluation was done a day before the procedure. All patients with co-exiting disease were excluded from the study. All elective patients as per the study protocol were enrolled. The induction procedures were explained to them and informed consent was taken. All the patients in both the groups were pre-medicated with oral Midazolam 7.5 mg one hour prior to induction of anesthesia. Both the groups received intra-venous injection midazolam 0.02 mg/kg, glycopyrrolate 0.2 mg and fentanyl 2 mcg/kg as premedication. Induction of anesthesia was done by propofol titrated to loss of verbal contact with the patient, loss of eyelash reflex and relaxation of jaw. If coughing, gagging, or body movement occurred during insertion of device, propofol 1 mg/kg was added to achieve an adequate level of anesthesia. For the safety reason of the patients before the insertion of any of the devices after loss of verbal contact, the anesthetist checked that hand-ventilation with a facemask was possible.
Adequate placement of the airway device was assessed by gentle squeezing the reservoir bag and observing the end-tidal CO2 waveform and movement of the chest wall. If ventilation was deemed inadequate, the following manipulations were allowed: gentle pushing or pulling the device, chin lift, jaw thrust, head extension, or neck flexion. The number of attempts required for insertion was recorded. A “failed attempt” was defined as removal of the device from the mouth before re-insertion. Two attempts were allowed for placement of each device with mask ventilation with oxygen between attempts. If second attempt also failed then the device was changed into other study device. The airway was manipulated after each attempt if a secure airway was not achieved. Intervention required on the airway was graded as either minor [changing neck position/adjusting head (changing depth of inspiration)] or major (requiring jaw thrust, re-insertion/change of device).
Effective ventilation was defined as proper chest expansion or square wave capnograph trace, absence of audible leak and lack of gastric insufflations. The total time of placement from grasping of the device to observing a square wave capnograph trace (the insertion time) and the numbers of attempts were recorded. Airway leak pressure tests were then performed. The oropharyngeal leak pressure was measured by closing the expiratory valve of the circle system at a fixed gas flow of 3 litters per minute and noting the airway pressure (maximum allowed 40 cm H2O). The position of the device was assessed and graded by the investigators using a fiberoptic bronchoscope (2.8 mm: Olympus, Tokyo, Japan) for the view of glottis.
Pre insertion complications were defined as minor (coughing or gagging on insertion, hiccough, gastric insufflations); or major (bronchospasm or airway obstruction). If both the devices failed then fiberoptic bronchoscope was kept as backup plan for intubation and the patients were excluded from the study.
RESULTS
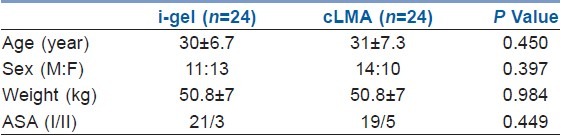
Forty Eight patients were enrolled into the study. All patients enrolled in the study group were included in the analysis. In i-gel group there were 11 male and 13 female patients where as in cLMA group there were 14 male and 10 female patients, both the groups were comparable with respect to sex.
The mean age in i-gel group was 30±6.7 years (Mean±SD) with the range of 18 to 48 years, the mean age in cLMA group was 31±7.3 (Mean±SD) with a range of 16 to 47 years as shown in Table 1 (P=0.450). The mean weight in i-gel group was 50.8±7 kgs (Mean±SD) was similar to the weight of patients in cLMA group with Mean±SD of 50.8±7kgs (P=0.984).
Table 1.
Demographic profile
There were no episodes of hypoxia, pulmonary aspiration, regurgitation, laryngospasm or gastric insufflations in both the groups. There were differences in the incidence of blood staining. With i-gel none of the patients had blood staining whereas in the cLMA blood staining was found in 20% (5/24) on the removal of the device. There were no incidence of major airway obstruction or bronchospasm intra-operatively in i-gel group but there were 2 incidences of major airway obstruction in cLMA group.
The i-gel and cLMA were successfully inserted at the first attempt in 91.7% and 79.2% of the patients respectively. In the second attempt, the percentage of successful insertion for the i-gel remained same at 91.7% whereas in cLMA the success rate improved to 83.33%.
The mean leak pressure was greater with i-gel (21.2 cm of H2O) compared to the cLMA (16.9 cm of H2O) which was clinically and statistically significant as shown in Table 2 (P=0.00). Fiberoptically, a view of cords was obtained in all patients (24/24 or 100%) in i-gel group whereas in cLMA group, a view was obtained only in 22/24 patients (91.66%)
Table 2.
Pre-insertion and pre-operative parameters of i-gel compared to cLMA
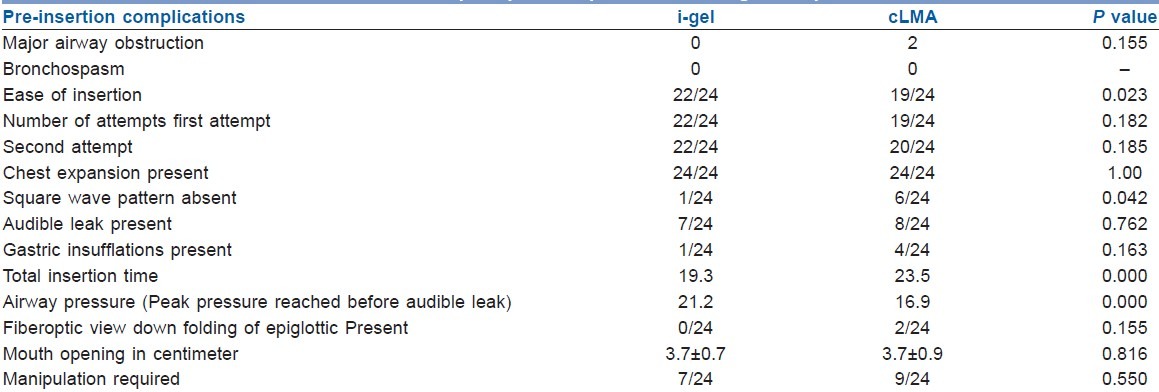
The mean insertion time was 19.3 seconds in the i-gel group and 23.5 seconds in the cLMA group (P=0.000). Significant differences were found in regards to square wave pattern in end-expiratory CO2. Square wave pattern in the capnography was absent in 1/24 patient in i-gel group whereas in cLMA group it was absent in 6/24 patients (P=0.042).
The mean mouth opening in the i-gel group was 3.7 cm ± 0.7 (SD) and for the cLMA it was 3.7±0.9 cm (SD) (P=0.816) which was statistically not significant.
This study was a cross-over control trial and hence the postoperative pharyngeal morbidity was not assessed.
DISCUSSION
The results of this study were very encouraging. The i-gel was successfully inserted in all patients and allowed effective controlled ventilation in 91.7% in the first attempt whereas it was possible only in 79.16% with cLMA. Overall insertion success rate with few minor manipulation of the device was 91.7% (with two attempts) with i-gel. With second attempt the success rate raise to 83.3% with cLMA. The results were comparable with the study done by Gatward JJ et al. who had evaluated size 4 i-gel in one hundred non-paralysed patients. Their study showed the first time success rate in insertion was 86% with i-gel but raised to 100% within three attempts or less.[7]
Rates of failure, manipulations required and complications with i-gel were very low compared to cLMA, which we have studied with similar methodology. The i-gel was well tolerated throughout anaesthesia and emergence, with few sequelae reported by patients. The i-gel, therefore appears to be a suitable device for anaesthesia using controlled ventilation and spontaneously breathing post burn neck contracture patients with limited neck movements compared to cLMA. For the busy clinician and even more for the preclinical working emergency physicians, it is of importance to know which airway device will perform with high success rate because supraglottic devices are recommended in the difficult airway algorithms during life-saving procedures.[9,10] Therefore, we intended to add another piece of evidence to guide clinical decisions.
Airway seal was better with the i-gel than cLMA which was statistically significant. The efficacy of seal depends on the fit between the oval-shaped groove surrounding the glottis and the oval shaped cuff of the laryngeal mask airway device.[11] The i-gel is made of a thermoplastic elastomer with a soft durometer material which is designed anatomically to fit the perilaryngeal and hypolaryngeal structures without the use of an inflatable cuff. This may explain the reason for the improved seal. The mean airway leak pressure was 5 cmH2O higher for the i-gel than the cLMA. This result is consistent with the results of earlier studies, reporting that the i-gel provides an airway leak pressure of 24-33 cmH2O.[6,7,12] Airway leak pressure with i-gel was greater than cLMA in the present study. Our results were consistent with the study by Shin WJ et al. where they reported that the airway sealing pressure achieved with the i-gel was greater than that with cLMA.[13]
The number of patients in whom the vocal cords were visible fiberoptically was significantly different between the groups, with i-gel better than the cLMA. This correlates with a recent crossover trial done by Janakiraman C et al. comparing the i-gel supraglottic airway and classic laryngeal mask airway.[8] Their study showed that a view of cords was obtained in all the patients in the i-gel group who had successful insertion in 100% patients whereas in the cLMA group, a view of cords was obtained only in 85% patients who had successful insertion. The ease of insertion was more with i-gel than with cLMA which was statistically significant. Levitan RM and Kinkle WC presumed that on insertion of cLMA with inflatable mask the deflated edge of the mask can catch the epiglottis and cause it to downfold or impede proper placement beneath the tongue.[14] It was shown that the i-gel is easier and quicker to insert at the first attempt than the cLMA which correlates with the study done using various manikins for the beginners compared with LMA insertion.[14] In our study, there was a significant difference in success rate between the two groups, success rate at first attempt in the i-gel group was higher than cLMA.
A study done by Levitan RM and Kinkle WC has shown that the sore throat after i-gel was reported by 18% of patients and complications of blood adhesion were reported to be 1%, whereas there were no case of blood adhesion to the i-gel but there was significantly higher incidences of blood adhesion in the cLMA.[14] Incidence of major airway obstruction during induction was more with cLMA than with i-gel which was statistically significant. Both i-gel and cLMA had no incidence of bronchospasm/laryngospasm which correlates with the study done by Gatward JJ et al. where they found only one case of partial airway obstruction with i-gel during evaluation of the size 4 i-gel airway in one hundred non-paralysed patients.[7] A recent study by Shin WJ et al. reported no such episodes in their study.[13]
From the results of this study, we conclude that i-gel has merit against c-LMA in terms of success rate of insertion, efficacy of air-way seal, greater airway leak pressure. Meanwhile major airway obstruction during induction was less with i-gel thus it allowed controlled ventilation with reduced risk of regurgitation and aspiration. Future clinical studies comparing i-gel and cLMA including large sample size is recommended to support the evidence of our present study and better understanding the phenomenon associated with the outcome of insertion of i-gel against cLMA.
CONCLUSION
The i-gel is cheap, effective airway device which is easier to insert and has better clinical performance in the difficult airway management in the post burn contracture of the neck. It has other potential advantages like effective airway sealing pressure which was within the normal limit, less blood staining of the device and less tongue, lip and dental trauma. Our study showed that i-gel is feasible for emergency airway management in difficult airway situation with reduced neck movement and limited mouth opening in post burn neck contracture.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.i-gel user guide. 7th ed. Workingham, UK: Intersurgical Ltd; 2009. [Google Scholar]
- 2.Stone B, Leach AB, Alexander CA. The use of the laryngeal mask airway by nurses during cardiopulmonary resuscitation. Results of a multicentre trial. Anaesthesia. 1994;49:3–7. doi: 10.1111/j.1365-2044.1994.tb03302.x. [DOI] [PubMed] [Google Scholar]
- 3.Blunt MC, Burchett KR. Varient Creutzfeldt-Jakob disease and disposable anaesthetic equipment-balancing the risks. Br J Anaesth. 2003;90:1–3. doi: 10.1093/bja/90.1.1. [DOI] [PubMed] [Google Scholar]
- 4.Esler MD, Baines LC, Wilkinson DJ, Langford RM. Decontamination of laryngoscopes: A survey of national practice. Anaesthesia. 1999;54:587–92. doi: 10.1046/j.1365-2044.1999.00755.x. [DOI] [PubMed] [Google Scholar]
- 5.Jackson KM, Cook TM. Evaluation of four airway manikins as patient simulators for the insertion of eight types of supraglottic airway devices. Anaesthesia. 2007;62:388–93. doi: 10.1111/j.1365-2044.2007.04983.x. [DOI] [PubMed] [Google Scholar]
- 6.Richez B, Saltel L, Banchereau F, Torrielli R, Cros AM. A new single use supraglottic airway device with a non inflatable cuff and esophageal vent: An observational study of the i-gel. Anesth Analg. 2008;106:1137–9. doi: 10.1213/ane.0b013e318164f062. [DOI] [PubMed] [Google Scholar]
- 7.Gatward JJ, Cook TM, Seller C, Handel J, Simpson T, Vanek V, et al. Evaluation of the size 4 i-gel airway in one hundred non paralysed patients. Anaesthesia. 2008;63:1124–30. doi: 10.1111/j.1365-2044.2008.05561.x. [DOI] [PubMed] [Google Scholar]
- 8.Janakiraman C, Chethan DB, Wilkes AR, Stacey MR, Goodwin N. A randomized crossover trial comparing the i-gel supraglottic airway and classic laryngeal mask airway. Anaesthesia. 2009;64:674–8. doi: 10.1111/j.1365-2044.2009.05898.x. [DOI] [PubMed] [Google Scholar]
- 9.Caplan RA, Benumof JL, Berry FA, Blitt CD, Bode RH, Cheney FW, et al. Practice guidelines for management of the difficult airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269–77. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 10.Nolan JP, Deakin CD, Soar J, Bottiger BW, Smith G. European Resuscitation Council guidelines for resuscitation 2005. Section 4. Adult advanced life support. Resuscitation. 2005;67(Suppl 1):39–86. doi: 10.1016/j.resuscitation.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 11.Brimacombe J, Holyoake L, Keller C, Brimacombe N, Scully M, Barry J, et al. Pharyngolaryngeal, neck, and jaw discomfort after anesthesia with the face mask and laryngeal mask airway at high and low cuff volumes in males and females. Anesthesiology. 2000;93:26–31. doi: 10.1097/00000542-200007000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Bamgbade OA, Macnab WR, Khalaf WM. Evaluation of the i-gel airway in 300 patients. Eur J Anaesthesiol. 2008;25:865–6. doi: 10.1017/S0265021508004511. [DOI] [PubMed] [Google Scholar]
- 13.Shin WJ, Cheong YS, Yang HS, Nishiyama T. The supraglottic airway i-gel in comparison with ProSeal Laryngeal mask airway and classic laryngeal mask airway in anaesthetized patients. Eur J Anaesthesiol. 2010;27:588–601. doi: 10.1097/EJA.0b013e3283340a81. [DOI] [PubMed] [Google Scholar]
- 14.Livitan R M, Kinkle W C. Initial anatomic investigations of the airway: A novel supraglotic airway without inflatable cuff. Anaesthesia. 2005;60:1022–6. doi: 10.1111/j.1365-2044.2005.04258.x. [DOI] [PubMed] [Google Scholar]


