Abstract
Background:
The flexible fibreoptic bronchoscope and bonfils rigid intubation endoscope are being widely used for difficult intubations.
Methods:
The haemodynamic response to intubation under general anaesthesia was studied in 60 adult female patients who were intubated using either flexible fibreoptic bronchoscope or bonfils rigid intubation endoscope (30 in each group). Non-invasive blood pressure and heart rate (HR) was recorded before induction of anaesthesia, immediately after induction, at the time of intubation and, thereafter, every minute for the next 5 min. The product of HR and systolic blood pressure (rate pressure product) at every point of time was also calculated.
Statistical Analyses:
Graph pad prism, 5.0 statistical software, independent t test and repeated measure ANOVA test were used.
Results:
Both bonfils rigid intubation endoscope and flexible fibreoptic bronchoscope required a similar time (less than 1 min) for orotracheal intubation. After intubation, there was a significant increase in HR, blood pressure and rate pressure product (P<0.001) in both the groups compared with the baseline and post-induction values. There was no significant difference in HR, blood pressure and rate pressure product at any of the measuring points or in their maximum values during observation between the two groups. The time required for recovery of systolic blood pressure and HR to post-induction value (±10%) was not significantly different between the two groups (more than 2 min).
Conclusion:
In female adults under general anaesthesia, bonfils rigid intubation endoscope and flexible fibreoptic bronchoscope require a similar time for successful orotracheal intubation and cause a similar magnitude of haemodynamic response.
Keywords: Airway management, blood pressure, intubation, bronchoscopy, endoscopes, endotracheal, heart rate, haemodynamics
INTRODUCTION
Bonfils intubation endoscope is a semi-rigid optical stylet, 40 cm in length, with a fixed anterior curvature of its tip of 40 degrees.[1–5] The fibreoptic bundle is encased in a stainless steel tube that provides a resolution of 15,000 pixel. The Bonfils intubation endoscope is available in three different sizes (2/3.5/5 mm external diameter). This device can navigate through the soft tissues and physically lift the epiglottis. It is portable, convenient to handle, easy to clean and more affordable. Difficult oro-tracheal intubations can be safely performed with its use. One major limitation is that it has an immobile tip and cannot be used for nasotracheal intubation.
Flexible fibreoptic bronchoscope has been the gold standard for difficult intubations.[6–8] A flexible bronchoscope is longer and thinner than a rigid bonfils endoscope. It contains a fibreoptic system, which transmits the image from the tip of the instrument to an eyepiece or video camera at the opposite end. It is available in three different sizes (2.5 mm, 3.5 mm, 5.5 mm external diameter). There is a flexible distal tip, which can be moved by the operator in different directions to help visualize the airway structures.
Many studies have compared the haemodynamic responses to laryngoscopy and fibreoptic intubation.[9–14] The primary objective of this randomized clinical study was to investigate whether there is a clinically significant difference between the haemodynamic response to orotracheal intubation, guided by either of the two devices (flexible fibreoptic bronchoscope and bonfils rigid intubation endoscope). The secondary objective was to compare the time taken for intubation with the use of either of the two devices.
It was hypothesized that the haemodynamic response to intubation would be significantly greater using the bonfils rigid intubation endoscope than the flexible fibreoptic bronchoscopic intubation; and the flexible fibreoptic bronchoscopic intubation would be significantly faster than the bonfils rigid endoscope-guided intubation.
METHODS
After obtaining the ethics committee approval and written informed consent from the patients, 60 adult females of ASA physical status I–II, who were scheduled for elective surgery under general anaesthesia and required endotracheal intubation, were included in this study. All patients were female, as gender can significantly affect the haemodynamic response to endotracheal intubation.[15]
Exclusion criteria included a history of reactive airway disease, gastro-oesophageal reflux, morbid obesity, hypertension and the use of medications that affect blood pressure and heart rate (HR). Patients were randomly allocated to be intubated using either of the two devices – Bonfils rigid intubation endoscope (Bonfils, Karl Storz, Tuttlingen, Germany) - Rigid group (n=30) or Flexible fibreoptic bronchoscope (Portal View LF-GP, Olympus Optical Co. Ltd., Tokyo, Japan) - Flexible group (n=30), according to a computerized randomized table.
Pre-operatively, all the patients were fasted adequately (solids – 6 h; clear fluids – 2 h). In the operation theatre, an 18 G I.V. cannula was secured. Monitoring of SpO2, ECG and non-invasive blood pressure was started. After a stabilization period of 10 min, baseline values of systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP) and HR were recorded.
The head of the patient was stabilized on a ring of height 7 cm. A portex cuffed endotracheal tube with an internal diameter of 7 mm was used in this study. Before intubation, the endotracheal tube was lubricated with 2% lignocaine gel and threaded over the intubating device.
The patient was pre-oxygenated for 5 min and anaesthesia was induced with fentanyl citrate 2 μg/kg and propofol 2 mg/kg injected I.V. After checking for adequate ventilation, neuromuscular blockade was produced with vecuronium bromide 0.1 mg/kg injected I.V. The patient was ventilated using the mask with 1% isoflurane in oxygen. If any difficulty was encountered in performing the mask ventilation, the patient was withdrawn from this study.
Tracheal intubation was attempted after 3 min of vecuronium injection. During intubation, the patient's head was placed in sniffing position and a clear airway maneuver was maintained by two trained assistants, who extended the atlanto-occipital joint and displaced the mandible anteriorly by application of a firm pressure behind the ascending rami. Macintosh laryngoscope was not used to aid the intubation.
All the intubations were performed by a single anaesthesiologist (who had an experience of more than 10 years and had completed orotracheal intubation in 100 patients with both the devices – flexible fibreoptic bronchoscope and bonfils rigid intubation endoscope; before the study). The operator stood behind the patient to introduce the fibreoptic bronchoscope or bonfils rigid intubation endoscope into the oropharynx, using the midline approach. The endotracheal tube was mounted over the scope and inserted under vision into the oropharynx. After visualizing the glottis, the endotracheal tube was slided into the middle of the trachea by railroading over the bonfils rigid intubation endoscope, while the flexible fibreoptic bronchoscope was inserted between the vocal cords into the middle of the trachea. The tip of the bronchoscope was not advanced too deep into the trachea (less than 6 cm below glottis) to avoid stimulation of the carina. The endotracheal tube was then advanced over the fibreoptic bronchoscope. After confirming the position of the endotracheal tube, the fibreoptic bronchoscope was removed.
After successful intubation, the endotracheal tube was connected to the circle breathing system of the anaesthesia machine for intermittent positive-pressure ventilation. Anaesthesia was maintained with isoflurane/O2:N2O (33%:66%). A fresh gas flow of 1.5 L/min was used. The ventilator settings and the isoflurane concentration were adjusted to maintain end-expired carbon dioxide and isoflurane concentration of 35–40 mmHg and 1%, respectively.
The BP and HR were recorded before induction of anaesthesia, immediately after induction, at the time of intubation and, thereafter, every minute for the next 5 min. The product of HR and SBP (rate pressure product – RPP), at every point of time, was calculated. The maximum values of BP and HR during the observation were also recorded.
The intubation time (T1 – time in sec, from termination of manual ventilation using a facemask to restarting of the ventilation through the endotracheal tube), the time required to reach the maximum values of SBP and HR (T2 and T3 – time in sec, from initiation of the intubation to the occurrence of the maximum values of SBP and HR, respectively) and the time required for recovery of SBP and HR to post-induction values (T4 and T5 – time in sec, from the completion of intubation to the occurrence of recovery of SBP and HR to the post-induction values±10%) were observed using a stopwatch. If SBP and HR did not recover to the post-induction values (±10%) within 5 min after the intubation, they were observed continuously until the target values were achieved.
During the observation, no manipulations (including any movement of the head and neck and preparation of the operative field) were performed on the patient. Any patient who required more than one attempt to achieve successful intubation was excluded from statistical analyses of the data. Post-operatively, the patients were monitored for 24 h for any complications from the intubations, like sore throat, coughing, stridor, dysphagia and dysphonia.
Statistical analyses
The sample size calculation was based on a previous study,[16] which indicated that at least 30 patients would be required in each group to demonstrate a clinically significant difference in MAP of 15 mmHg or HR of 15 beats/min between the two groups (α=0.05, ß=0.2).
Statistical analysis was performed using the Graph pad prism 5.0 statistical software. The demographic profile, T1, T2, T3, T4 and T5, were compared between the two groups using the independent t test. HR, SBP, DBP, MBP and RPP were compared between the two groups over time using the two-way ANOVA test. The intragroup differences of HR, SBP, DBP, MBP and RPP over the time period were analyzed using the repeated measure ANOVA test. The quantitative data were expressed as mean (M) and standard deviation (SD). P<0.05 was considered as statistically significant.
RESULTS
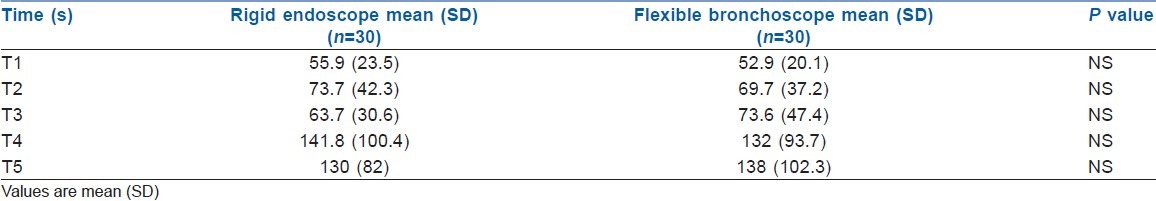
There was no statistically significant difference in the demographic profile and the baseline values of the haemodynamic variables between the two groups. The endotracheal intubation was successfully performed in a single attempt in all the patients. The mean (SD) intubation time was not significantly different in the two groups (Flexible group=52.9 (20.1) s, Rigid group=55.9 (23.5) s) [Table 1]. Mean (SD) time required to reach the maximum values of SBP (T2) and HR (T3) were not significantly different in the two groups (T2 – Flexible group=69.7 (37.2) s, Rigid group=73.7 (42.3) s; T3 – Flexible group=73.6 (47.4) s, Rigid group=63.7 (30.6) s; Table 1). Mean (SD) time required for the recovery of SBP (T4) and HR (T5) to the post-induction values (±10%) were also statistically similar in the two groups (T4 – Flexible group=132 (93.7) s, Rigid group=141.8 (100.4) s; T5 – Flexible group=138 (102.3) s, Rigid group=130 (82) s; Table 1).
Table 1.
Time in seconds required for intubation (T1), time in seconds required for occurrence of the maximum values of systolic blood pressure and heart rate (T2 and T3) from initiation of intubation and time in seconds required for the recovery of systolic blood pressure and heart rate to post-induction values (±10%) in the two groups (T4 and T5)
After the induction of anaesthesia, HR, SBP, DBP, MBP and RPP decreased significantly compared with the baseline values in both the groups (P<0.001) [Table 2, Figures 1 and 2]. After endotracheal intubation, there was a significant increase in HR, SBP, DBP, MBP and RPP in both the groups (P<0.001) compared with the baseline and the post-induction values [Table 2, Figures 1 and 2]. There was no significant difference in HR, SBP, DBP, MBP and RPP at any of the measuring points or in their maximum values during the observation between the two groups [Table 2, Figures 1 and 2]. No patient developed bradycardia/hypotension and SpO2 was maintained at 100% in all the patients, throughout the observation. There were no complications observed with the use of both the devices.
Table 2.
Blood pressure, heart rate and rate pressure product before and after anaesthesia induction, at intubation, 1 min post-intubation and the maximum values in two groups
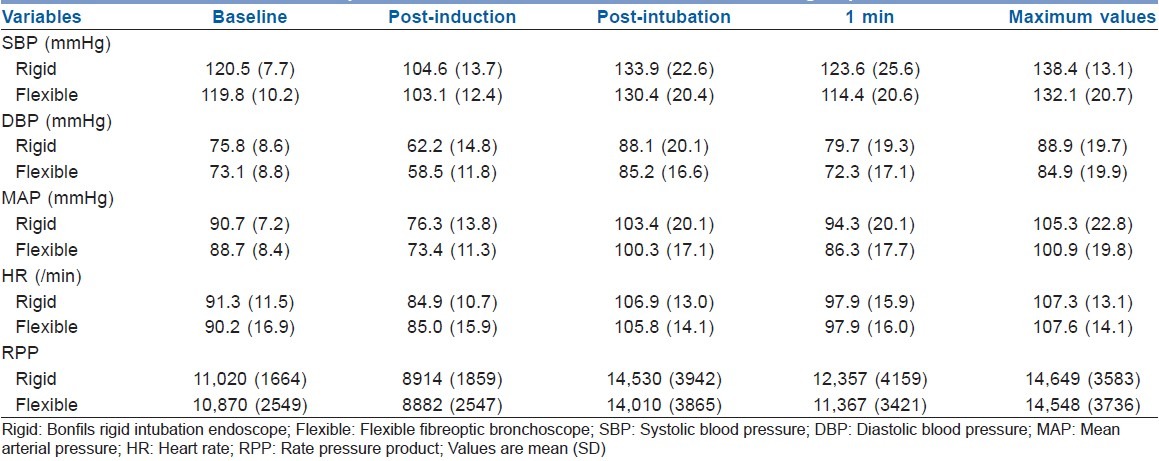
Figure 1.
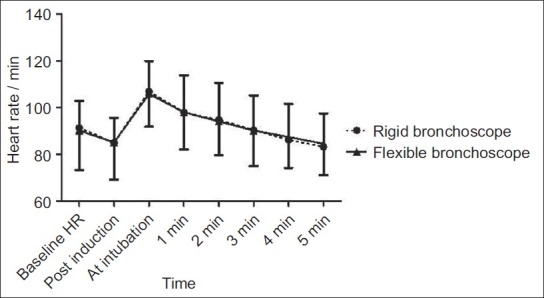
Heart rate changes associated with rigid endoscope guided and flexible fibreoptic intubations over time. Points represent mean±SD
Figure 2.
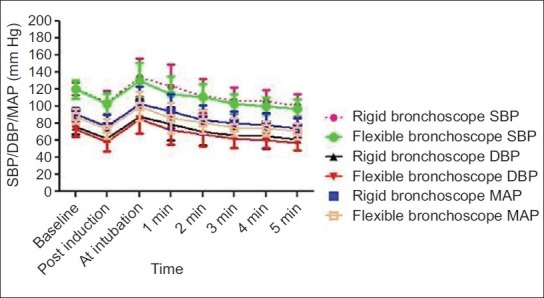
Systolic, mean and diastolic blood pressure changes associated with rigid endoscope guided and flexible fibreoptic intubations over time. Points represent mean±SD
DISCUSSION
Laryngoscopy and intubation causes sympathetic stimulation, leading to an increase in HR (15–20%) and BP (20–40%). These haemodynamic changes peak 1 min after initiation of the intubation and persist for 5–10 min. This haemodynamic response has two components,[13,14] initially to laryngoscopy and then to the tracheal intubation. Flexible fibreoptic intubation causes a significant increase in HR and BP[9,10,13,14] under general anaesthesia. Tracheal tube insertion is the most invasive stimulus causing this haemodynamic response.[9–14,17] The site of the airway stimulation and the total time of the airway stimulation[18,19] are the main determinants of this haemodynamic response.
The flexible fibreoptic bronchoscope has a mobile distal tip, which should make it a faster device for intubation compared with the bonfils rigid intubation endoscope. The flexible fibreoptic intubation seems to cause a lesser haemodynamic response because we can better centralize its mobile distal tip thus minimizing the stimulation of the laryngeal surface. Bonfils rigid intubation endoscope has an immobile tip[1,20] thus having a higher probability of stimulating the laryngeal surface. The intubation time with bonfils rigid intubation endoscope might be longer, as we have to manipulate its immobile tip with our wrist, to visualize the vocal cords. These two factors might accentuate the haemodynamic response to intubation using the bonfils rigid intubation endoscope.
In our study, contrary to the hypothesis, the intubation (airway stimuli) time (T1) was similar in both the rigid and the flexible groups (less than 60 s). Both the devices provided a good view of the vocal cords and had a low complication rate. Hence, both the devices can be safely used to secure an unanticipated difficult airway. Contrary to our study, the bonfils rigid endoscope-guided intubation was found to be easier and faster (mean time 38±10 s) than the flexible fibreoptic intubation (mean time 86±18 s) in patients with grade 3 difficult airways.[21] The use of bonfils rigid endoscope was recommended for all the difficult intubations, with the assistance of a direct laryngoscope.[21] Rudolf et al. also reported that the intubation using bonfils endoscope was faster than the flexible fibreoptic intubation.[22] Both these studies used direct laryngoscopy to aid the fibreoptic visualization, which was different from our method of jaw traction by displacing the mandible anteriorly. This might have been the reason for the difference in the times to intubation, in comparison with our study.
Najafi et al. found a mean intubation time of 40 s with the use of bonfils rigid endoscope in patients without neuromuscular paralysis.[23] Halligan et al.[24] found that the median (range) time to intubation using bonfils intubation endoscope was 33 (24–50) s with the aid of the Macintosh blade in patients with neuromuscular paralysis. Bein et al. found a median (range) intubation time of 40 (23–77) s, with the bonfils endoscope in patients with predicted difficult airways.[25] Barak et al.[13] and Cole et al.[26] found the flexible fibreoptic intubation times (mean±SD) to be 55±22.5 s and 56±24 s, respectively; which were similar to our study.
In our study, in both the groups, the endotracheal intubation caused a similar and a significant increase (P<0.001) in HR (15–20%) and BP (10–20%) over the baseline and the post-induction values [Table 2, Figures 1 and 2]. A similar haemodynamic response in both the groups might have been due to the expertise of the anaesthesiologist, who was proficient with the use of both the devices. He centralised both the scopes in the larynx and caused minimal airway stimulation in both the groups. He also took a similar time for intubation in both the groups. Similar to our study, Soo et al. found a significantly similar haemodynamic response to intubation using the flexible fibreoptic bronchoscope and the bonfils rigid intubating endoscope.[21]
In our study, in both the groups, there was a haemodynamic response in spite of administering fentanyl citrate 2 μg/kg I.V. 5 min before intubation. This is in contrast to the study by Ko et al., which concluded that fentanyl 2 μg/kg administered I.V., 5 min before intubation, effectively blunts the haemodynamic response to orotracheal intubation.[27] In our study, in both the groups, the maximum increase in BP and HR occurred 1 min after the initiation of the intubation process, and this response lasted only for 2 min after the successful intubation [Table 2, Figures 1 and 2]. Similar to our study, Adachi et al.[10] and Barak et al.[13] found that there was a significant increase in HR and BP for the first 3 min after the initiation of flexible fibreoptic intubation, but this did not correlate with the blood catecholamine levels. In our study, the induction of anaesthesia caused a significant decrease in HR (5–10%) and BP (10–15%) in both the groups compared with the baseline values.
Rate pressure product is an index of myocardial oxygen consumption;[28] a value exceeding 22,000 may be associated with myocardial ischemia.[29] In our study, in both the groups, the rate pressure product did not reach 22,000 at any point of time. Hence, both the flexible fibreoptic bronchoscope and the bonfils rigid intubation endoscope are safe to use in patients with ischemic heart disease. Bonfils rigid intubation endoscope ($8000 or INR 3.5 lakh) is less expensive compared with the flexible fibreoptic bronchoscope ($ 12,000 or INR 5.5 lakh).
CONCLUSION
This study demonstrates that both the flexible fibreoptic intubation and the bonfils rigid endoscope-guided intubation require a similar time for successful orotracheal intubation and cause a similar magnitude of haemodynamic response in female adults under general anaesthesia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Abramson SI, Holmes AA, Hagberg CA. Awake insertion of the bonfils retromolar intubation fiberscope in five patients with anticipated difficult airways. Anesth Analg. 2008;106:1215–7. doi: 10.1213/ane.0b013e318167cc7c. [DOI] [PubMed] [Google Scholar]
- 2.Bein B, Yan M, Tonner PH, Scholz J, Steinfath M, Dorges V. Tracheal intubation using the bonfils intubation fiberscope, after failed direct laryngoscopy. Anaesthesia. 2004;59:1207–9. doi: 10.1111/j.1365-2044.2004.03967.x. [DOI] [PubMed] [Google Scholar]
- 3.Medhat M, Aljuhani T. Awake intubation with bonfil's retromolar fiberscope in a patient with hard and fixed swelling of the right side of the neck and the tonsillar tumor. Saudi J Anaesth. 2011;5:423–5. doi: 10.4103/1658-354X.87275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corbanese U, Possamai C. Awake intubation with the bonfils fiberscope in patients with difficult airway. Eur J Anaesthesiol. 2009;26:837–41. doi: 10.1097/EJA.0b013e32832c6076. [DOI] [PubMed] [Google Scholar]
- 5.Mazeres JE, Lefranc A, Cropet C, Steghens A, Bachmann P, Petrol O, et al. Evaluation of the bonfils intubating fiberscope for predicted difficult intubation in awake patients with ear, nose and throat cancer. Eur J Anaesthesiol. 2011;28:646–50. doi: 10.1097/EJA.0b013e3283495b85. [DOI] [PubMed] [Google Scholar]
- 6.Ovassapian A. The flexible bronchoscope: A tool for anesthesiologists. Clin Chest Med. 2001;22:281–99. doi: 10.1016/s0272-5231(05)70043-5. [DOI] [PubMed] [Google Scholar]
- 7.Bokhari A, Benhams SW, Popat MT. Management of unanticipated difficult intubation: A survey of current practice in the oxford region. Eur J Anaesthesiol. 2004;21:123–7. doi: 10.1017/s0265021504002078. [DOI] [PubMed] [Google Scholar]
- 8.Liem EB, Bjoraker DG, Gravenstein D. New options for airway management: Intubating fibreoptic stylets. Br J Anaesth. 2003;91:408–18. doi: 10.1093/bja/aeg011. [DOI] [PubMed] [Google Scholar]
- 9.Adachi YU, Takamatsu I, Watanabe K, Uchihashi Y, Higuchi H, Satosh T. Evaluation of the cardiovascular responses to fiberoptic orotracheal intubation with television monitoring: Comparison with conventional direct laryngoscope. J Clin Anesth. 2000;12:503–8. doi: 10.1016/s0952-8180(00)00196-3. [DOI] [PubMed] [Google Scholar]
- 10.Adachi YU, Satomoto M, Higuchi H, Watanabe K. Fentanyl attenuates the hemodynamic response to endotracheal intubation more than response to laryngoscopy. Anesth Analg. 2002;95:233–7. doi: 10.1097/00000539-200207000-00043. [DOI] [PubMed] [Google Scholar]
- 11.Machata AM, Gonano C, Holzer A. Awake nasotracheal fiberoptic intubation: Patient comfort, itubating conditions, and hemodynamic stability during conscious sedation with remifentanil. Anesth Analg. 2003;97:904–8. doi: 10.1213/01.ANE.0000074089.39416.F1. [DOI] [PubMed] [Google Scholar]
- 12.Smith JE, King MJ, Yanny HF, Pottinger KA, Pomirska MB. Effect of fentanyl on circulatory responses to orotracheal fiberoptic intubation. Anaesthesia. 1992;47:20–3. doi: 10.1111/j.1365-2044.1992.tb01946.x. [DOI] [PubMed] [Google Scholar]
- 13.Barak M, Ziser A, Greenberg A, Lischinsky S, Rosenberg B. Haemodynamic and catecholamine response to tracheal intubation: Direct laryngoscopy compared with fiberoptic intubation. J Clin Anesth. 2003;15:132–6. doi: 10.1016/s0952-8180(02)00514-7. [DOI] [PubMed] [Google Scholar]
- 14.Shibata Y, Okamoto K, Matsumoto M, Suzuki K, Sadanaga M, Morioka T. Cardiovascular responses to fiberoptic intubation: A comparison of orotracheal and nasotracheal intubation. J Anesth. 1992;6:262–8. doi: 10.1007/s0054020060262. [DOI] [PubMed] [Google Scholar]
- 15.Jee D, Moon HL. Gender may affect the hemodynamic response to induction and intubation in young adults. J Clin Anesth. 2004;16:563–7. doi: 10.1016/j.jclinane.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 16.Sun HY, Xue FS, Li CW, Sun HT, Liu KP. Comparison of haemodynamic responses to nasotracheal intubation with fiberoptic bronchoscope and direct laryngoscope. Chin J Anesth. 2005;5:394–5. [Google Scholar]
- 17.Takahashi S, Mizutani T, Miyabe M, Toyooka H. Hemodynamic responses to tracheal intubation with laryngoscope versus lightwand Intubating device (Trachlight) in adults with normal airway. Anesth Analg. 2002;95:480–4. doi: 10.1097/00000539-200208000-00046. [DOI] [PubMed] [Google Scholar]
- 18.Ng WS. Pathophysiological effects of tracheal intubation. In: Latto IP, Vaughan RS, editors. Difficulties in tracheal intubation. 2nd ed. London: W.B.Saunders; 1997. pp. 13–27. [Google Scholar]
- 19.Yoshihiro H, Shuji D. Differences in cardiovascular response to airway stimulation at different sites and blockade of the responses by lidocaine. Anesthesiology. 2000;93:95–103. doi: 10.1097/00000542-200007000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Boedeker BH, Barak-Bernhagen MA, Miller DJ, Nicholas TA, 4th, Linnaus A, Murray WB. Improving rigid fiberoptic intubation: A comparison of the Bonfils Intubating Fiberscope with a novel modification. BMC Emerg Med. 2010;10:11. doi: 10.1186/1471-227X-10-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Soo HK, Su JW, Jong HM. A comparison of bonfils intubation fiberscopy and fiberoptic bronchoscopy in difficult airways, assisted with direct laryngoscopy. Korean J Anesthesiol. 2010;58:249–55. doi: 10.4097/kjae.2010.58.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rudolph C, Henn- Beilharz A, Gottschall R, Wallenborn J, Schaffranietz L. The unanticipated difficult intubation: Rigid or flexible endoscope? Minerva Anestesiol. 2007;73:567–74. [PubMed] [Google Scholar]
- 23.Najafi A, Rahimi E, Shariat MR, Hussain KZ. Bonfils fiberscope: Intubating conditions and hemodynamic changes without neuromuscular blockade. Acta Med Iran. 2011;49:201–7. [PubMed] [Google Scholar]
- 24.Halligan M, Charters P. A clinical evaluation of the bonfils intubation fibrescope. Anaesthesia. 2003;58:1087–91. doi: 10.1046/j.1365-2044.2003.03407.x. [DOI] [PubMed] [Google Scholar]
- 25.Bein B, Worthmann F, Scholz J, Brinkmann F, Tonner PH, Steinfath M, et al. A comparison of the intubating LMA and the bonfils intubation endoscope in patients with predicted difficult airways. Anaesthesia. 2004;59:668–74. doi: 10.1111/j.1365-2044.2004.03778.x. [DOI] [PubMed] [Google Scholar]
- 26.Cole AFD, Mallon JS, Rolbin SH, Ananthanarayan C. Fiberoptic intubation using anesthetized, paralyzed, apneic patients: Results of a resident training program. Anesthesiology. 1996;5:1101–6. doi: 10.1097/00000542-199605000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Ko SH, Kim DC, Han YJ, Song HS. Small- dose fentanyl: optimal time of injection for blunting the circulatory responses to tracheal intubation. Anesth Analg. 1998;86:658–61. doi: 10.1097/00000539-199803000-00041. [DOI] [PubMed] [Google Scholar]
- 28.Gobel FL, Nordstrom LA, Nelson RR, Jorgensen CR, Wang Y. The rate- pressure product as an index of myocardial oxygen consumption during excercise in patients with angina pectoris. Circulation. 1978;57:549–56. doi: 10.1161/01.cir.57.3.549. [DOI] [PubMed] [Google Scholar]
- 29.Robinson BF. Relation of heart rate and systolic blood pressure to the onset of pain in angina pectoris. Circulation. 1967;35:1073–83. doi: 10.1161/01.cir.35.6.1073. [DOI] [PubMed] [Google Scholar]


