Sir,
A safe and effective implementation of ultrasound-guided nerve block application depends on the accurate visualization of the needle tip. The development of psychomotor skills for holding the ultrasound transducer with one hand in a balanced way, simultaneously with the other hand steering of the needle to the destination requires a certain learning period.[1] In order to shorten the duration of the training process and not to harm the patient, simulation models were developed.[2,3] The efficacy of the simulation models is proportional to the ability to mimic the real clinical applications and the similarity of the human anatomy. However, the use of the high-reality simulation models is difficulty to access or, because of their expensiveness, they are limited.
We have developed a simple and economical simulation model created with easily obtained materials that provides real-time feedback for learners to help distinguish whether the needle tip or the shaft is contacting the target.
Materials required for the preparation of the model are beef from a butcher containing the least animal fat, tendon and nerve tissue content region with the dimensions about 15 cm × 10 cm × 10 cm (length × width × height), 3 mm diameter metal rod, a battery-powered bicycle buzzer with LED light, an insulated electrical cable tape and an insulated standard nerve block needle [Figure 1]. In order to eliminate the meat smell, the meat was stored in alcohol for 30 min. All meat was covered with a transparent stretch film. All materials other than the medical supplies could be bought from local retail stores for about 15 Euros.
Figure 1.
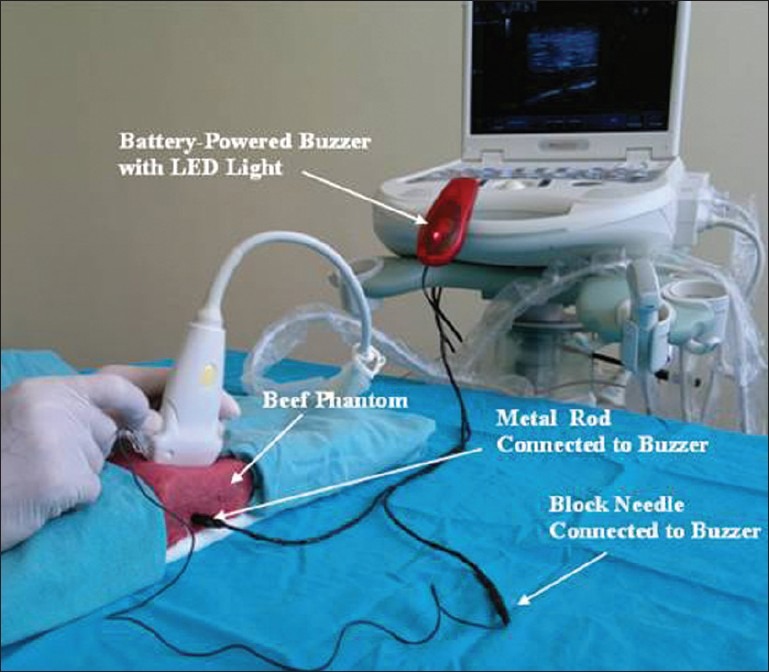
Materials used for constructing the model
The metal rod, selected for imitation of the target, was placed about 2.5 cm in depth of the meat longitudinally recumbent. One of the cables of the buzzer was connected and wrapped with an electrical tape to the metal rod from the extended part. The other cable was inserted to the tip of entry attachment point of the block needle to the electrostimulator and was taped.
In this model, the metal bar was identified as a target for learners and they were asked to forward the needle to the hyperechoic metal rod with the in-plane approach [Figure 2]. When the needle tip and not the needle shaft contacts with the metal rod, the electrical circuit is completed. The circuit makes a buzzer sound and illuminates the LED light thus providing objective feedback to both the instructor and the practitioner.
Figure 2.
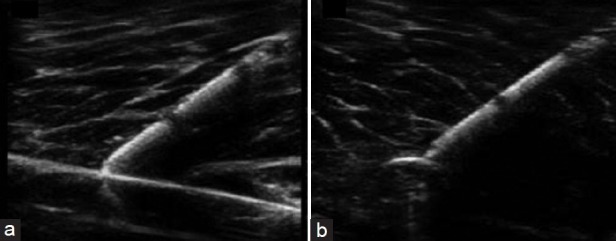
Long axis (a) and short axis (b) ultrasound images of hyperechoic target with in-plane approach of a 22-gauge needle in the beef phantom
This model can be modified according to the difficulty level of training; in the later stage of the training, the depth of the target can be increased and the target size can be reduced. Learners can make short and long-axis target scans, in-plane and out-of-plane needle insertions transactions in this model.
We used the beef phantom in order to increase the realism of the simulation model. The factors that limit low-fidelity models are their weak similarities to the clinical applications. Practitioners may be disappointed when faced with real patient tissue because the needle is very easily viewable in agar/gelatin phantoms. They are useful in the early stages of learning needle guidance before progressing to harder targets or meat phantoms.[4] The most important factor restricting our model is the short life-time of the meat.
REFERENCES
- 1.Sites BD, Gallagher JD, Cravero J, Lundberg J, Blike G. The learning curve associated with a simulated ultrasound guided interventional task by inexperienced anesthesia residents. Reg Anesth Pain Med. 2004;29:544–8. doi: 10.1016/j.rapm.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Surry KJ, Smith WL, Campbell LJ, Mills GR, Downey DB, Fenster A. The development and evaluation of a threedimensional ultrasound-guided breast biopsy apparatus. Med Image Anal. 2002;6:301–23. doi: 10.1016/s1361-8415(02)00087-7. [DOI] [PubMed] [Google Scholar]
- 3.Tsui BC, Dillane D, Walji AH. Cadaveric ultrasound imaging for training in ultrasound-guided peripheral nerve blocks: Upper extremity. Can J Anaesth. 2007;54:392–6. doi: 10.1007/BF03022663. [DOI] [PubMed] [Google Scholar]
- 4.Hocking G, Hebard S, Mitchell CH. A review of the benefits and pitfalls of phantoms in ultrasound-guided regional anesthesia. Reg Anesth Pain Med. 2011;36:162–70. doi: 10.1097/aap.0b013e31820d4207. [DOI] [PubMed] [Google Scholar]


