Abstract
Clopidogrel is an oral antiplatelet agent used in the treatment of coronary artery disease, peripheral vascular disease and cerebrovascular disease. Gastrointestinal symptomsincluding nausea, diarrhea and constipation are the common side effects ofthis drug. Serious side effects like intracranial hemorrhage and severe neutropenia were also reported but spontaneous pectoral hematoma due to the clopidogrel has not been reported previously. We present a case of large spontaneous pectoral hematoma during clopidogrel therapy in an elderly woman.
KEY WORDS: Clopidogrel, pectoral hematoma, adverse effect
Introduction
Clopidogrel is an oral antiplatelet agent used in the treatment of coronary artery disease, peripheral vascular disease and cerebrovascular disease. Clopidogrel is a thienopyridine derivative, selectively inhibits the binding to adenosine diphosphate (ADP) and inhibits platelet aggregation.[1] Gastrointestinal problems including nausea, diarrhea and constipation are the common side effects of clopidogrel. Serious side effects like intracranial hemorrhage and severe neutropenia have been reported but spontaneous pectoral hematoma due to the clopidogrel has not been reported previously.[2,3] We present a case of large spontaneous pectoral hematoma during clopidogrel therapy in an elderly woman.
Case Report
A 81 year old woman was admitted to emergency department complaining of a purple discoloration and tenderness on her skin of chest wall and back, which developed rapidly over a few hours. The patient denied trauma or any other medication except clopidogrel that may cause skin hemorrhage. The patient suffered from hypertension since 10 years and had undergone coronary artery bypass grafting ten years ago. She was discharged on aspirin, ramipril, carvedilol and pantoprazole. However ouicy to be gastric irritation, clopidogrel 75 mg/day had been added instead of aspirin. The physical examination revealed a normal heart rate and regular rhythm, normal oxygenation and normal blood pressure (110/70 mmHg). The lungs were clear to auscultation bilaterally. The abdomen was soft and nontender. Examination revealed a large hematoma originating from the skin of her left chest wall and back [Figures 1a, b]. Laboratory tests showed mildly decreased hemoglobin and hematocrit levels (10,3 g/dl and 31,6%, respectively). Platelet count (349.000 K/uL), creatinine level (1.3 mg/dl) and albumin (5.3 mg/dl) were normal. Prothrombin time, activated partial thromboblastin time, bleeding time and clotting time were within normal range. Enhanced computed tomography (CT) of thorax showed subpectoral hematoma on the left side [Figure 2]. Clopidogrel therapy was withheld. The patient was treated with intravenous fluids. Repeated hemogram tests showed no significant decrease in the values and the patient did not require hemo-transfusion. The patient was discharged 12 hours after admission. The hematoma completely disappeared within two weeks.
Figure 1.

Hematoma with extensive ecchymosis extending from left thoracic region to lower back (a) anterior view, (b) lateral view
Figure 2.
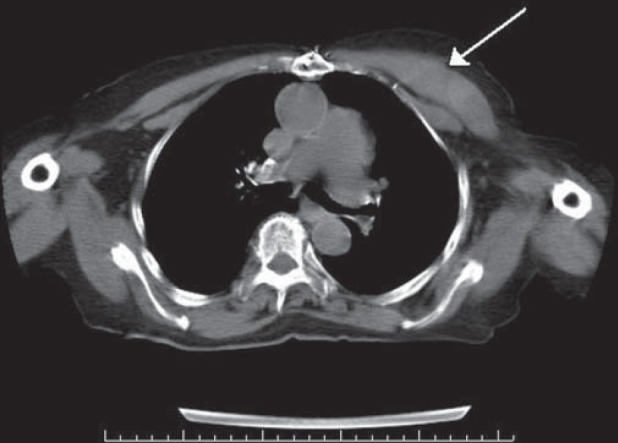
Enhanced computed tomography (CT) of thorax showing a left pectoralis major hematoma (arrow)
Discussion
ADP is a platelet activator that is released from red blood cells, activated platelets, and damaged endothelial cells and that induces platelet adhesion and aggregation. Clopidogrel inhibits platelet aggregation induced by ADP, resulting in prolongation of bleeding time and delay of clot retraction. Clopidogrel is at least as effective as aspirin in preventing serious cardiovascular events in patients with stable vascular disease.[4] Anti-platelet therapy, while efficacious in reducing the incidence of ischemic complications, can cause serious adverse reactions. The most common adverse effects of clopidogrel include gastrointestinal hemorrhage, diarrhea, rash, and pruritis. Some serious adverse effects, such as intracranial hemorrhage, neutropenia, and thrombotic thrombocytopenic purpura, urticarial rash have been reported.[5,6] Gastrointestinal and intracranial bleeding due to clopidogrel therapy have been reported, but pectoral hematoma has not been reported. This is the first case report of a patient developing spontaneous hematoma while receiving clopidogrel therapy.
Several factors are reported which increase the risk of patients developing hemorrhage while receiving clopidogrel, these include advanced age, female gender, hypertension, coagulopathy and usage of other antiplatelet agents. Pathogenesis of hematoma formation may be multifactorial. We cannot completely rule out the possibility of a coincidence of pectoral hematoma and clopidogrel therapy; however, the probability of a causal association would seem to be much higher because of the anti platelet action of clopidogrel.
Sung et al. reported a 60 year old woman that used clopidogrel for transient ischemic attack and after 6 months the drug caused spontenaus spinal epidural hematoma (SSEH).[7] Laboratory findings were normal . In this case no other possible cause of hamatoma was detected. Paraplegia developed due to compression of the hematoma and thereafter she underwent emergent laminectomy from T6 to T9 and a thick epidural hematoma was removed completely. There was no evidence of vascular malformation at histomorphologic examination. In our case, hematoma did not compress any adjacent structures. After clopidogrel was withdrawn, clinical findings recovered within two weeks.
Drug induced adverse effects and drug-drug interactions are commonly seen in the elderly. Total plasma volume decreases and plasma drug concentration increases with aging. The rising plasma concentration of drugs leads to increased efficacy up to a certain level, after which the efficacy of the drug diminishes and there is a concomitant rise in adverse reactions. Most elderly patients are also on multiple medications, increasing the chance for drug-drug interactions. In our patient, dramatic improvement of hematoma was observed after withdrawal of clopidogrel. There was no other medication except clopidogrel that could cause the hemorrhage. Based on the Naranjo's Scale, a score of 8 suggested that the clopidogrel was the probable cause of the pectoral hematoma.
In conclusion, spontaneous hematoma can occur during clopidogrel therapy. And a vigilance to this possible adverse effect of this drug is recommended.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Makkar K, Wilensky RL, Julien MB, Herrmann HC, Spinler SA. Rash with both clopidogrel and ticlopidine in two patients following percutaneous coronary intervention with drug-eluting stents. Ann Pharmacother. 2006;40:1204–7. doi: 10.1345/aph.1G587. [DOI] [PubMed] [Google Scholar]
- 2.Cay S, Yilmaz MB, Korkmaz S. Intracranial bleeding associated with clopidogrel. Cardiovasc Drugs Ther. 2005;19:157–8. doi: 10.1007/s10557-005-0896-y. [DOI] [PubMed] [Google Scholar]
- 3.Montalto M, Porto I, Gallo A, Camaioni C, Della Bona R, Grieco A, et al. Clopidogrel-induced neutropenia after coronary stenting: Is cilostazol a good alternative? Int J Vasc Med. 2011;2011:867964. doi: 10.1155/2011/867964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events. Lancet. 1996;348:1329–39. doi: 10.1016/s0140-6736(96)09457-3. [DOI] [PubMed] [Google Scholar]
- 5.Balamuthusamy S, Arora R. Hematologic adverse effects of clopidogrel. Am J Ther. 2007;14:106–12. doi: 10.1097/01.mjt.0000212708.81034.22. [DOI] [PubMed] [Google Scholar]
- 6.Khambekar SK, Kovac J, Gershlick AH. Clopidogrel induced urticarial rash in a patient with left main stem percutaneous coronary intervention: Management issues. Heart. 2004;90:e14. doi: 10.1136/hrt.2003.027367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sung JH, Hong JT, Son BC, Lee SW. Clopidogrel-induced spontaneous spinal epidural hematoma. J Korean Med Sci. 2007;22:577–9. doi: 10.3346/jkms.2007.22.3.577. [DOI] [PMC free article] [PubMed] [Google Scholar]


