Abstract
Purpose
The PCR was compared with routine microbial studies for the detection of fungal pathogens in clinically suspected fungal keratitis.
Methods
A prospective nonrandomized study was undertaken at a tertiary eye care centre to evaluate 30 eyes of 30 patients with presumed fungal keratitis, both fresh and treated. Corneal scrapings were performed on each patient. The specimens were analysed by a semi-nested PCR assay using fungal-specific primers. PCR products were cloned and sequenced for identification, and compared with a conventional microbial work-up (smear and culture).
Results
Of the 30 samples, the PCR showed positivity in 93.3%, culture in 40%, and potassium hydroxide in 20%. Of the 28 PCR-positive cases, 12 were culture-positive and 16 were culture-negative. Two samples were both PCR and culture test negative. Culture-negative samples were PCR-positive in 16 of 18 (88.9%) cases. The PCR did not yield any false-negative findings in a culture-positive specimen. Both common and uncommon aetiologic fungi have been identified by DNA sequencing analysis.
Conclusion
The PCR was able to detect fungal DNA in a high proportion of culture-negative cases. Technical considerations of the PCR process include extraction of artifacts and amplification of non-pathogenic DNA. Nonetheless, our findings suggest that the PCR can be a useful adjunct to smear and culture in the rapid diagnosis of fungal keratitis, particularly in cases of failed detection from routine procedures.
Keywords: PCR, fungal keratitis, corneal ulcer
Introduction
Microbial keratitis is a common cause of monocular blindness around the world. With proper management most community acquired corneal ulcers can be resolved. However, severe infections such as those caused by fungi, which are predominately in tropical areas,1 have been difficult to treat resulting in corneal perforation, or even the loss of an eye.2 Often the onset follows a minor injury to the cornea, secondary to vegetative matter, and progresses slowly.3, 4 The therapy for fungal keratitis is hampered by the limited availability of an effective antifungal for topical use.
Until recently, 5% Natamycin has been the only commercially available topical antifungal medication. Natamycin has also been the preferred first-line drug of choice for filamentous fungi. However, its corneal penetration is poor and has not been effective for deeper keratitis.5 In addition, some fungal pathogens such as Fusarium, which has been reported as a common pathogen, can penetrate an intact Descemet membrane, resulting in endophthalmitis.6 Therefore, early diagnosis and treatment are important in the proper management of fungal keratitis.7 However, fungal isolation via a conventional culture may take ∼5–15 days to become positive.
A PCR is a highly sensitive and rapid technique to identify pathogens by extraction and amplification from small quantities of DNA. In ophthalmology, the use of PCR in the diagnosis of causative pathogens in uveitis,8, 9, 10, 11 and viral keratitis, has increased in the past few years.12 However, its application in microbial keratitis has been limited. This study aimed to compare the result of the conventional microbial work-up to those of the PCR in the detection of fungal pathogens in patients with suspected fungal keratitis.
Materials and methods
Study design
This study was a prospective nonrandomized study undertaken at a tertiary eye centre in Northern Thailand and was approved by the Research and Ethic Committee of Faculty of Medicine, Chiang Mai University. The research method adhered to the tenets of the Declaration of Helsinki.
Patient selection
All participants were recruited from the Chiang Mai University Hospital, a tertiary hospital in Northern Thailand. The clinical presumption of fungal keratitis was made from the history and the morphology of the ulcers. Patients who were eligible to contribute corneal specimens for the study included those with a history of corneal trauma with organic matter, use of topical steroids, or a compromised immune system, and clinical findings of presumed fungal infection such as ulcers with dry surface, feathery edge, unleveled hypopyon, pigmented lesion, or endothelial plaque.13 Exclusion criteria included as follows: patients who were uncooperative, or the inability to give informed consent, and inadequate or contaminated specimens.
Sample collection and processing
Corneal samples were collected consecutively from 30 patients with suspected fungal keratitis from July 2007 to May 2009. After complete history taking and ocular examination, corneal scrapings were performed by using a Kimura spatula under a slit-lamp biomicroscope after the instillation of topical 0.5% tetracaine hydrochloride.
The specimens were obtained at the edge and base of lesions, then smeared directly onto two separate glass slides for Gram staining and potassium hydroxide (KOH) wet mount. Subsequent scrapings were inoculated in culture media including blood agar, chocolate agar, Sabouraud's dextrose agar, and Thioglycolate broth for both a bacterial and fungal culture. The spatula was flame-sterilized between each sample. The samples for PCR were obtained by scraping and stirring the spatula in 1.5-ml microtubes containing 200 μl of sterile normal saline solution.
The specimens were sent separately for PCR analysis at the Department of Microbiology, Faculty of medicine, Chiang Mai University. The routine work-ups were carried out at the central laboratory unit of Chiang Mai University hospital.
DNA extraction, PCR, and sequencing
Genomic DNA was extracted from corneal scrapings with known fungal and bacterial strains as controls by using the QIAamp DNA mini kit (QIAGEN GmbH, Hilden, Germany). Briefly, the samples were treated with 20 μl of proteinase K solution and 180 μl of ATL buffer (both solutions were supplied in the kit) for 20 min at 56 °C. Then 200 μl of AL buffer was added, and the samples were incubated for 10 min at 70 °C. The purification of the DNA was done by precipitating with 200 μl absolute ethanol, column binding, and washing of the bound DNA with the supplied wash buffer solutions. The DNA was then eluted with 50 μl of AE elution buffer.
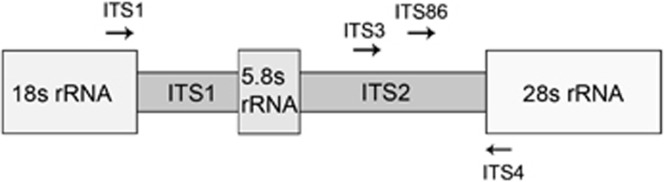
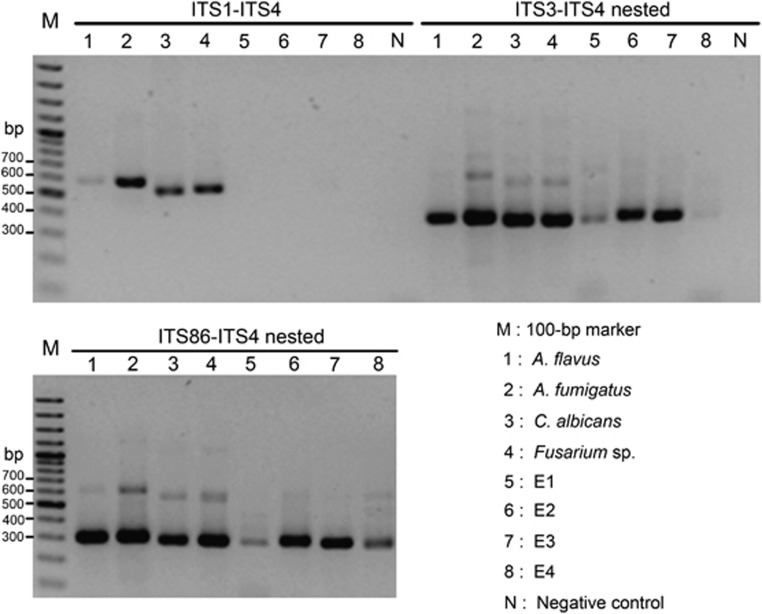
All DNA samples were subjected to semi-nested PCR analysis for the amplification of internal transcribed spacer (ITS) regions. The primers used for the first PCR were ITS1 (5′-TCCGTAGGTGAACCTGCGG-3′), ITS4 (5′-TCCTCCGCTTATTGATATGC-3′),14 and for the second semi-nested PCR were ITS3 (5′-GCATCGATGAAGAACGCAGC-3′)15 or ITS86 (5′-GTGAATCATCGAATCTTTGAAC-3′)14 and ITS4. The primer-binding sites are illustrated in Figure 1. The PCR reactions contained the final concentration of 1.5 mM MgCl2, 0.2 mM each dNTP, 0.4 M each primer, and 0.6 U Taq DNA polymerase (Qiagen GmbH) in the final volume of 25 μl. Five microliters of the DNA extracted from corneal scraping was used as a template in the first PCR reaction, and 1 μl of the first PCR products was used in the second, semi-nested PCR reaction. PCR parameters started with an initial denaturation of the template DNA for 5 min at 95 °C. The amplification cycles were 35 rounds of denaturation for 30 s at 95 °C, annealing for 30 s at either 50 °C for the first PCR or 56 °C for the semi-nested PCR, and extension for one minute at 72 °C. The final extension was made for 7 min at 72 °C. The PCR products were analysed by 1% agarose gel electrophoresis and the ethidium bromide staining procedure. The size of PCR products, which were estimated by comparing to a marker, 100-bp plus (Fermentas International Inc., Vilnius, Lithuania) were 550–820 bp for ITS1–ITS4 primers, 320–500 bp for ITS3–ITS4 primers, and 250–360 bp for ITS86–ITS4 primers. The positive control was 10ng/μl of DNA of Aspergillus fumigatus, Aspergillus flavus, Candida albicans, and Fusarium species from our Medical Mycology laboratory and the negative control was sterile distilled water. The agarose gel electrophoresis is shown in Figure 2. The amplified PCR products were purified, cloned, and sequenced. The DNA sequences were analysed using the BLAST programme of the GenBank database (National Institute of Health; http://www.ncbi.nlm.nih.gov).
Figure 1.
Site of primers binding on the ITS region.
Figure 2.
PCR amplification of DNA with primers ITS1, ITS4 (first primer pair) and with primers ITS3, ITS4, or primers ITS86, ITS4 (second primer pair). Lanes: 1, A. flavus; 2, A. fumigatus; 3, C. albicans; 4, Fusarium species; and 5–8, clinical specimens from four patients. N, negative control; M, size marker of 100-bp ladder standard DNA.
Results
Patients' details and treatment outcomes
The mean age of the patients was 54 (SD±12.4, range 33–80) years old. There were 19 males and 11 females. The most common predisposing factor was corneal trauma (20 cases), followed by undetermined risk factor (3 cases), topical steroid use (2 cases), splashed water (2 cases), diabetes mellitus (2 cases), and insecticide vapour (1 case). The majority of the patients (90%, 27/30) received prior treatment and was referred after unsuccessful treatment before presentation (25 by ophthalmologists and 2 by general practitioners).
Almost all of the patients received a treatment of combined topical antifungal–antibacterial (23 cases), followed by a topical antifungal (4 cases), and a topical antibacterial (3 cases). In total, 17 cases were successfully treated with medications. Surgical interventions were performed in 13 cases including: enucleation (four), evisceration (four), tissue adhesive (three), sclera patch graft (one), and amniotic membrane patch graft (one). One patient was referred to another institute because of treatment failure. At last visit given treatment, VA improved more than one line in 3 cases, improved more than two lines in 13 cases, had no changes in 3 cases, worse than the initial VA in 2 cases, and lost an eye in 9 cases. The average follow-up time was 7 (range 1–28) months.
Conventional work-up results: smear and culture
The KOH wet mount was positive for fungus in 6 of 30 (20%) cases, and the Gram stains failed to identify any fungal elements. The culture was positive for fungus in 12 of 30 (40%). Of these, 5 were positive for both the smear and culture (patients 2, 7, 18, 29, and 30), and one sample was culture-negative but smear-positive (patient 27; Table 1).
Table 1. Patients' demographic data, results of direct examination, culture, and PCR (N=30).
| No. | Age/sex | Risk factors | Pre treated | Smear | Culture | PCR | DNA sequencing | Response to treatment |
|---|---|---|---|---|---|---|---|---|
| 1 | 43 M | Non-veg FB | Yes | − | Fusarium sp. | + | Fusarium sp. | No (evisceration) |
| 2 | 42 F | Steroid drops | Yes | Pseudo hyphae | Candida albicans | + | C. albicans | No (glue) |
| 3 | 44 M | Veg FB | Yes | − | − | + | Candida parapsilosis | Yes |
| 4 | 53 M | Tree trauma | Yes | − | Unidentified dematiaceous fungus | + | Hyphodontia sp.a | Yes |
| 5 | 61 F | DM | Yes | − | − | + | Candida etchellsii | Yes |
| 6 | 62 M | Non-veg FB | Yes | − | − | + | Cryptococcus pseudolongus | No (enucleation) |
| 7 | 69 M | Non-veg FB | No | Filamentous fungus | Unidentified dematiaceous fungus | + | Botryosphaeria sp.a | Yes |
| 8 | 38 M | Steroid drops | No | − | Fusarium sp. | + | Fusarium solani | Yes |
| 9 | 52 M | Undetermined | Yes | − | − | + | Fusarium proliferatum | Yes |
| 10 | 80 F | DM | Yes | − | − | + | Erysiphe guercicola | No (enucleation) |
| 11 | 48 M | Trauma | Yes | − | − | + | Cladosporium colocasiaea | No (glue) |
| 12 | 40 M | Veg FB | Yes | − | − | + | Exidiopsis calcea | No |
| 13 | 58 F | Tree trauma | Yes | − | − | + | Cladosporium oxysporuma | Yes |
| 14 | 79 M | Tree trauma | Yes | − | − | + | Curvularia affinisa | No (sclera patch) |
| 15 | 47 F | Non-veg FB | Yes | − | − | + | Cladosporium sp.a | No (enucleation) |
| 16 | 64 M | Veg FB | Yes | − | − | + | C. parapsilosis | No (enucleation) |
| 17 | 77 M | Undetermined | No | − | − | + | Phanerochaete sordida | No (glue) |
| 18 | 57 F | Non-veg FB | Yes | Hyaline septate hyphae | Aspergillus fumigatus | + | A. fumigatus | Yes |
| 19 | 45 F | Veg FB | Yes | − | Unidentified dematiaceous fungus | + | Cladosporium sp.a | No (evisceration) |
| 20 | 59 F | Veg FB | Yes | − | Fusarium sp. | + | Alternaria alternata | No (evisceration) |
| 21 | 52 F | Veg FB | Yes | − | − | + | Fusarium sp. | No (evisceration) |
| 22 | 71 M | Non-veg FB | Yes (GP) | − | Unidentified dematiaceous fungus | + | Botryosphaeria rhodinaa | Yes |
| 23 | 49 M | Veg FB | Yes (GP) | − | − | + | Botryosphaeria rhodinaa | Yes |
| 24 | 38 F | Chemical vapour | Yes | − | − | + | F. solani | Yes |
| 25 | 33 M | Veg FB | Yes | − | Fusarium sp. | + | F. solani | Yes |
| 26 | 56 M | Tree trauma | Yes | − | − | − | − | Yes |
| 27 | 48 M | Non-veg FB | Yes | Hyaline septate hyphae | − | + | Acremonium sp. | Yes |
| 28 | 39 F | Splashed water | Yes | − | − | − | − | Yes |
| 29 | 55 M | Splashed water | Yes | Hyaline septate hyphae | Fusarium sp. | + | Fusarium oxysporum | Yes |
| 30 | 53 M | Undetermined | Yes | Septate hyphae | Curvularia sp. | + | Curvularia sp.a | Yes |
Abbreviations: DM, diabetes mellitus; FB, foreign body; GP, general practitioner; veg, vegetative matters.
These fungi are dematiaceous fungi.
PCR results
Of the 30 samples, 28 were PCR-positive. Two negative PCR samples were culture-negative as well (patients 26 and 28). Of those with a positive PCR, 12 were culture positive. The results of the culture and PCR were matched in 11 cases and unmatched in 1 case. The most common fungal pathogens that were recovered from both the culture and PCR (seven cases) were in Genus Fusarium (n=4), followed by Candida (n=1), Aspergillus (n=1), and Curvularia (n=1). In four samples with unidentified dematiceous fungi observed from the culture, the following dematiceous fungi were identified by the PCR analysis: Hyphodontia (n=1), Cladosporium (n=1), and Botryosphaeria (n=2). For one unmatched case (patient 20), the culture was positive for Fusarium species, but Alternaria alternata was identified by PCR analysis. In one case with negative culture but positive PCR results (patient 27), the sequence analysis revealed the fungus as the Acremonium species, which correlated with the KOH-positive result for hyaline septate hyphae. Of the 18 culture-negative samples, 16 (88.9%) were PCR-positive. The results of PCR products in culture-negative samples are demonstrated in Table 1. As depicted in Table 2, the positive and negative predictive value (95% CI) of the PCR was 42.9% (25.0–62.6), and 100% (19.8–100), respectively.
Table 2. Comparison between microbial cultures vs PCR results.
| Culture positive | Culture negative | Total | |
|---|---|---|---|
| PCR positive | 12 Fusarium=5 Dematiaceous fungi =4 Aspergillus =1 Curvularia =1 Candida=1 | 16 Clinical impressiona: Fungal keratitis=10 Uncertain=6 | 28 |
| PCR negative | 0 | 2 Clinical impressiona: Bacterial Keratitis=1 Fungal keratitis=1 | 2 |
| Total | 12 | 18 | 30 |
Clinical impression was made according to clinical features and a response to treatment.
Discussion
Until recently, smear and culture remained the gold standard methodologies for the identification of causative organisms in microbial keratitis. However, most bacterial corneal ulcers can be treated successfully with broad spectrum antibiotics without a microbial work-up. This is in contrast with cases of fungal keratitis, even after treatment with antifungal agents, the visual outcome in some cases remains poor, especially in cases that present late. This may be due to the limited available topical antifungal agents compared with antibacterial agents. Moreover, most of topical antifungal drugs poorly penetrate the cornea.
In ophthalmic practice, particularly in the developing countries where corneal ulcers are a common eye problem, before consulting a specialist, patients with suspected fungal keratitis have already received a variety of treatments including an antifungal, together with antibiotics in various combinations.16 Prior treatment with antimicrobial agents can modify the clinical features as well as influence the culture results. Therefore, diagnosis in such cases is difficult and may require an advanced technique such as PCR. In this study, semi-nested PCR was applied because it is relatively easy with minimal cost, making this method popular in the detection of various infectious diseases.17, 18, 19 Primers can be designed specifically and serve numerous purposes. They provide high sensitivity and possibilities to detect the fungal DNA in a minute sample amount thus enhance the sensitivity of the diagnosis. In this study, panfungal primers were used to amplify the rRNA gene of all fungi, to enhance the identification of fungal pathogens.
In this case series, a routine microbial work-up including smear and culture yielded positive results in only 20% and 40% of the cases, respectively, compared with 93.3% by PCR methods. The seemingly low-positive smear and culture rate may be partly due to a small amount of corneal specimens, particularly in patients that presented with a thinned cornea and most of the cases were referred after being unsuccessfully treated. Of those culture-positive samples, 91.7% (11/12) matched with sequenced PCR products. The PCR could identify uncommon dematiaceous (dark pigmented) organisms including: Hyphodontia, Cladosporium, and Botryosphaeria by the nucleotide sequence analysis. PCR also yielded high-positive results of 16 from 18 cases (88.9%) in culture-negative samples. Of these, some unusual fungi were identified including Eryshiphe, Exidiopsis, Botryosphaeria, Hyphodontia, and Phanerochate sordica.
Exidiopsis and Phanerochaete can be found in woods. Plant pathogens such as Hyphodontia, Botryosphaeria, Erysiphe, and Phanerochaete were also reported as pathogens in humans. Botryosphaeria was reported as a new emerging pathogen causing ocular disease.20 Phanerochaete, which was teleomorph or the sexual state of Sporotrichum, was considered as a rare and emerging agent causing hyalohyphomycosis in humans.21 These unusual fungi identified by PCR might be uncultured by routine media, as has been reported from previous studies.20, 22, 23
A. alternata has been reported as a corneal pathogen by PCR.24 In this series, A. alternata was identified in one case by PCR analysis whereas Fusarium species was grown on a routine culture. The result was considered as a mismatch in this study. It may have been a mixed infection in this case and one organism was missed by each method, or could be due to contamination of the PCR sample during specimen collection or PCR processing.
The high-positive rate in the isolation of pathogens by the PCR method may not be unexpected, as PCR can amplify even minute amounts of pathogen DNA. In addition, PCR can detect DNA from either dead or living organisms, whereas only living organisms can grow in cultures. Even though routine fungal media are capable of detecting and growing common fungal pathogens, some unusual fungi may not be cultured in the routine media. While the use of pan-fungal primers in the PCR or nested PCR may alleviate this problem.
In this study, the relatively low-positive predictive value (43%) of the PCR method may be related to the low positivity rate (40%) of microbial culture, which was the proportion of culture-proved cases rather than the true prevalence of fungal keratitis in our series. However, the low-positive predictive value suggests that it is unclear whether the samples that were PCR-positive but culture-negative represent true positives or false positives. There are several reasons that PCR may be more sensitive than culture at detecting fungal keratitis, including its ability to amplify even minute amounts of pathogen DNA, and to identify either dead or living organisms. However, PCR may also be more likely to produce false positives, as the technique is at risk for contamination with incidental fungal organisms present in the examination room or the laboratory. Future studies of PCR for fungal keratitis could assess this by clinical cases known not to be caused by fungus (ie, cases caused by bacteria), and by including negative control swabs of the air in the processing laboratory and the clinical examination room.
In practice, the conventional work-up via smear and culture is still an essential tool to identify causative organisms even though it may be less sensitive than the PCR. Moreover, culture allows for testing of antifungal susceptibility and will allow growth of fungal organisms not detectable with the primers used in the PCR assay. PCR may be considered as an alternative, or adjunctive in cases that the causative pathogen cannot be identified by a routine work-up. Nonetheless, the PCR is not available in all institutes, and its turnaround time may take more time than a smear and culture. In addition, the cost of the PCR is more expensive than a routine work-up; therefore, a larger number of patients with adequate controls are required for developing primers that are specific to the more common fungal DNA. This can reduce the cost of the PCR and enhance its widespread use as a screening technique in areas where fungal keratitis is endemic.
Acknowledgments
This study was supported by the Faculty of Medicine Endowment Fund, Faculty of Medicine, Chiang Mai University. The authors did not have a proprietary or any financial interest in products mentioned in this study.
This study was supported by the Faculty of Medicine Endowment Fund for Medical Research, Chiang Mai University, Chiang Mai, Thailand.
The authors declare no conflict of interest.
Footnotes
This study was presented in part at the 2nd Asia Cornea Society Biennial Scientific Meeting, Kyoto, Japan, December 2010.
References
- Bharathi MJ, Ramakrishnan R, Meenakshi R, Shivakumar C, Raj DL. Analysis of the risk factors predisposing to fungal, bacterial and Acanthamoeba keratitis in south India. Indian J Med Res. 2009;130 (6:749–757. [PubMed] [Google Scholar]
- Upadhyay MP, Srinivasan M, Whitcher JP. Microbial keratitis in the developing world: does prevention work. Int Ophthalmol Clin. 2007;47 (3:17–25. doi: 10.1097/IIO.0b013e318074e0b3. [DOI] [PubMed] [Google Scholar]
- Xie L, Zhong W, Shi W, Sun S. Spectrum of fungal keratitis in north China. Ophthalmology. 2006;113 (11:1943–1948. doi: 10.1016/j.ophtha.2006.05.035. [DOI] [PubMed] [Google Scholar]
- Bharathi MJ, Ramakrishnan R, Meenakshi R, Padmavathy S, Shivakumar C, Srinivasan M. Microbial keratitis in South India: influence of risk factors, climate, and geographical variation. Ophthalmic Epidemiol. 2007;14 (2:61–69. doi: 10.1080/09286580601001347. [DOI] [PubMed] [Google Scholar]
- Tu EY, McCartney DL, Beatty RF, Springer KL, Levy J, Edward D. Successful treatment of resistant ocular fusariosis with posaconazole (SCH-56592) Am J Ophthalmol. 2007;143 (2:222–227. doi: 10.1016/j.ajo.2006.10.048. [DOI] [PubMed] [Google Scholar]
- Dursun D, Fernandez V, Miller D, Alfonso EC. Advanced fusarium keratitis progressing to endophthalmitis. Cornea. 2003;22 (4:300–303. doi: 10.1097/00003226-200305000-00004. [DOI] [PubMed] [Google Scholar]
- Lalitha P, Prajna NV, Kabra A, Mahadevan K, Srinivasan M. Risk factors for treatment outcome in fungal keratitis. Ophthalmology. 2006;113 (4:526–530. doi: 10.1016/j.ophtha.2005.10.063. [DOI] [PubMed] [Google Scholar]
- Chee SP, Jap A.Presumed fuchs heterochromic iridocyclitis and Posner-Schlossman syndrome: comparison of cytomegalovirus-positive and negative eyes Am J Ophthalmol 2008146(6883–889.e881. [DOI] [PubMed] [Google Scholar]
- Dworkin LL, Gibler TM, Van Gelder RN. Real-time quantitative polymerase chain reaction diagnosis of infectious posterior uveitis. Arch Ophthalmol. 2002;120 (11:1534–1539. doi: 10.1001/archopht.120.11.1534. [DOI] [PubMed] [Google Scholar]
- Dabil H, Boley ML, Schmitz TM, Van Gelder RN. Validation of a diagnostic multiplex polymerase chain reaction assay for infectious posterior uveitis. Arch Ophthalmol. 2001;119 (9:1315–1322. doi: 10.1001/archopht.119.9.1315. [DOI] [PubMed] [Google Scholar]
- De Groot-Mijnes JD, Rothova A, Van Loon AM, Schuller M, Ten Dam-Van Loon NH, De Boer JH, et al. Polymerase chain reaction and Goldmann-Witmer coefficient analysis are complimentary for the diagnosis of infectious uveitis. Am J Ophthalmol. 2006;141 (2:313–318. doi: 10.1016/j.ajo.2005.09.017. [DOI] [PubMed] [Google Scholar]
- Van Gelder RN. Applications of the polymerase chain reaction to diagnosis of ophthalmic disease. Surv Ophthalmol. 2001;46 (3:248–258. doi: 10.1016/s0039-6257(01)00274-0. [DOI] [PubMed] [Google Scholar]
- Thomas PA, Leck AK, Myatt M. Characteristic clinical features as an aid to the diagnosis of suppurative keratitis caused by filamentous fungi. Br J Ophthalmol. 2005;89 (12:1554–1558. doi: 10.1136/bjo.2005.076315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer C, Colom F, Frases S, Mulet E, Abad JL, Alio JL. Detection and identification of fungal pathogens by PCR and by ITS2 and 5.8S ribosomal DNA typing in ocular infections. J Clin Microbiol. 2001;39 (8:2873–2879. doi: 10.1128/JCM.39.8.2873-2879.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar M, Shukla PK. Single-stranded conformation polymorphism of large subunit of ribosomal RNA is best suited to diagnosing fungal infections and differentiating fungi at species level. Diagn Microbiol Infect Dis. 2006;56 (1:45–51. doi: 10.1016/j.diagmicrobio.2006.03.003. [DOI] [PubMed] [Google Scholar]
- Tananuvat N, Suwanniponth M. Microbial keratitis in Thailand: a survey of common practice patterns. J Med Assoc Thai. 2008;91 (3:316–322. [PubMed] [Google Scholar]
- Nix WA, Oberste MS, Pallansch MA. Sensitive, seminested PCR amplification of VP1 sequences for direct identification of all enterovirus serotypes from original clinical specimens. J Clin Microbiol. 2006;44 (8:2698–2704. doi: 10.1128/JCM.00542-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagyalakshmi R, Therese KL, Madhavan HN. Application of semi-nested polymerase chain reaction targeting internal transcribed spacer region for rapid detection of panfungal genome directly from ocular specimens. Indian J Ophthalmol. 2007;55 (4:261–265. doi: 10.4103/0301-4738.33037. [DOI] [PubMed] [Google Scholar]
- Pugliese N, Circella E, Pazzani C, Pupillo A, Camarda A. Validation of a seminested PCR approach for rapid detection of Salmonella enterica subsp. enterica serovar Gallinarum. J Microbiol Methods. 85 (1:22–27. doi: 10.1016/j.mimet.2011.01.003. [DOI] [PubMed] [Google Scholar]
- Kim E, Chidambaram JD, Srinivasan M, Lalitha P, Wee D, Lietman TM, et al. Prospective comparison of microbial culture and polymerase chain reaction in the diagnosis of corneal ulcer Am J Ophthalmol 20081465714–723.e711. [DOI] [PubMed] [Google Scholar]
- Sutton D. Rare and emerging agents of hyalohyphomycosis. Curr Fungal Infect Rep. 2008;2:134–142. [Google Scholar]
- Kumar M, Mishra NK, Shukla PK. Sensitive and rapid polymerase chain reaction based diagnosis of mycotic keratitis through single stranded conformation polymorphism. Am J Ophthalmol. 2005;140 (5:851–857. doi: 10.1016/j.ajo.2005.05.019. [DOI] [PubMed] [Google Scholar]
- Ghosh A, Basu S, Datta H, Chattopadhyay D. Evaluation of polymerase chain reaction-based ribosomal DNA sequencing technique for the diagnosis of mycotic keratitis. Am J Ophthalmol. 2007;144 (3:396–403. doi: 10.1016/j.ajo.2007.05.017. [DOI] [PubMed] [Google Scholar]
- Ferrer C, Munoz G, Alio JL, Abad JL, Colomm F. Polymerase chain reaction diagnosis in fungal keratitis caused by Alternaria alternata. Am J Ophthalmol. 2002;133 (3:398–399. doi: 10.1016/s0002-9394(01)01329-0. [DOI] [PubMed] [Google Scholar]