Abstract
Malignant phylloides tumor is a relatively rare and rapidly growing tumor of the breast. Presentation during pregnancy is uncommon. Reports regarding malignancy in these tumors differ greatly in incidence, and most of them are stromal malignancies. We report this case in which 24-year old primigravid patient in the 36th week of her pregnancy had a malignant phylloides tumor of breast with sudden growth and fine needle aspiration cytology of the breast was positive for malignancy. Ultimately after her caesarean delivery, excision biopsy was in favor of a malignant process. Pregnancy with nulliparous prolapse is also a rare condition. Those conditions are not associated with each other, but presence of two rare conditions in the same time in the same person is unique.
Key Words: Malignant phyllodes tumor, prolapse, pregnancy, malignancy
Introduction
Malignant phylloides tumor is a relatively rare tumor of the breast.1 Expressing this tumor as “sarcoma” is somewhat misleading, because it connotes malignancy, however, it is now well known that both benign and malignant forms of the disease can occur.2 Presentation during pregnancy is even less common, and may be associated with rapid increase in size.3,4 Reports regarding malignancy in these tumors differ greatly in incidence and mostly being stromal malignancies. We report the present case in which the patient had a malignant phylloides tumor of breast. Sudden rapid growth had occurred in the second half of pregnancy and fine needle aspiration cytology (FNAC) suggested malignancy. Eventually excision biopsy revealed malignant phylloides tumor of breast. Pregnancy with nulliparous prolapse is also a rare condition. They are not associated with each other but presence of two rare conditions at same time in a same person is unique.
Case Description
A 24-year-old primipara in the 36th week of her pregnancy presented with a huge lump in her right breast (figure 1). She had a history of an earlier operation in the same breast for a lump, which its nature was not known 1.5 years earlier. She did not undergo any treatment for the mass, and the recurrence of the mass before the onset of pregnancy. The mass remained relatively small with a size of around two inches in diameter as per her description till the 28th week of her pregnancy. It began to grow rapidly in size, practically in days, and at the time of presentation was as large as a football (figure 1), and was causing pain for the patient. Examination revealed a characteristically ill-shaped swelling with variegated consistency. It was so large and heavy that required the support by her hands during moving around (figure 1). The axillae and opposite breast revealed no significant findings. The patient had also a uterine prolapse since few days after marriage (figure 2). Fine needle aspiration cytology was positive for malignancy, chest X-ray with shield was normal, and ultrasonography of abdomen for metastases was normal.
Figure 1.
Huge lump in breast of the patients with malignant phylloides tumor during pregnancy
Figure 2.

Co-incidental nulliparous prolapse in pregnancy
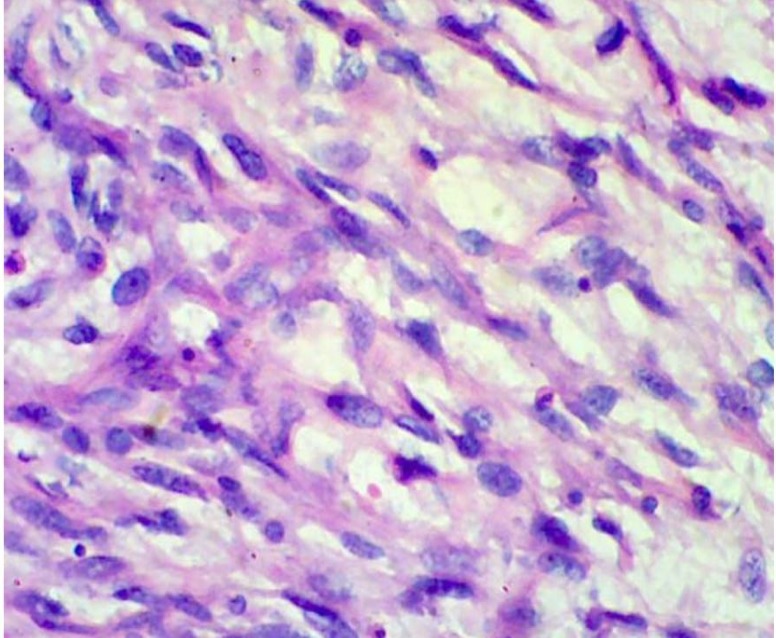
A decision was taken to defer removal of the lesion till completion of pregnancy. Delivery was achieved by caesarean section in the 37th week of pregnancy, since there was uneffaced cervix due to nulliparous prolapse of uterus. Liver and abdomen examination during the caesarean section revealed no metastases. Recovery from caesarean section was uneventful. As had been advised, the patient returned for surgical treatment in a private setting approximately two months after delivery. Since there was no palpable axillary lymph node, simple mastectomy was done without any axillary clearance. Gross picture was not taken due to ignorance of the surgeon. However, we somehow managed to obtain the biopsy report, which confirmed that the mass was malignant phylloides tumor of breast. The photomicrographic view (×400) of H/E stained section shows spindle-shaped, highly pleomorphic and hyper chromatic stromal cells, and atypical tripolar mitotic figure, which had grown independent from epithelial components (figure 3). These two signs were indicative of malignancy.
Figure 3.
Microphotograph of malignant phylloides tumor of the breast (H&E stained ×400).
Subsequent to a discussion with the surgeon of the case we came to know that the patient was recovered uneventfully after surgery, and stitches were removed on the 7th post operative day. Following discharge, the patient was asked to take advice from the Oncology Department in a higher center as no facility of radiotherapy or chemotherapy was available here in our set up. Owing to very low education and socioeconomic condition the patient never turned up.
Discussion
Malignant phylloides tumor is a relatively rare tumor of the breast, constituting 0.5% of breast tumors.1 Only six previous cases of phylloides tumor in pregnancy were found, and majority was in the last trimester.3 It characteristically grows very rapidly and attains large sizes by the time of presentation.4 Rapid enlargement of the tumor in pregnancies, as seen in our case, has been previously reported.4-6 Though rare cases of bilateral malignancy have been reported,3,7 the proportion of malignant tumors amongst such lesions, as reported in literature, seems to vary considerably. Vorherr et al.8 reported that 10-30% of cases were malignant, whilst others 1 stated that as many as 33% were malignant and a further 27% were borderline. Karim et al.9 reported that 12% and 33% of cases were malignant or borderline, respectively. They commented on the pathogenesis of malignant change in cystosarcoma, and stressed the importance of loss of the stromal-epithelial interdependency, increased stromal proliferation, angiogenesis, and matrix alterations in the progression to malignancy. They also commented on the greater percentage of tumors with higher grades and higher recurrence rate in Asian women. The malignant changes arise from the stromal tissues, and hence form sarcomas. Fine needle aspiration cytology has been used to detect malignancy in these tumors,10 but the definite proof requires obtain biopsy.
Management of malignant phylloides tumor of breast has always been controversial, and cannot be standardized for all patients. Wide local excision for small tumors and simple mastectomy for larger ones are usually satisfactory. Excision of the pectoralis major muscle may be necessary, if the fascia or muscle is infiltrated. Because of very low incidence of lymph node involvement, most of the studies believe that axillary node clearance is not required.2,11,12
Conclusion
The signs and symptoms as well as laboratory and radiographic findings of the present case indicate that it was a case of malignant phylloides tumor of breast. Such a tumor can occur in pregnancy and is fast growing.
Conflict of Interest: None declared
References
- 1.Lenhard MS, Kahlert S, Himsl I, et al. Phyllodes tumour of the breast: clinical follow-up of 33 cases of this rare disease. Eur J Obstet Gynecol Reprod Biol. 2008;138:217–21. doi: 10.1016/j.ejogrb.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Agrawal PP, Mohanta PK, Singh K, Bahadur AK. Cystosarcoma phyllodes with lymph node metastasis. Commun Oncol. 2006;3:44–8. [Google Scholar]
- 3.Blaker KM, Sahoo S, Schweichler MR, Chagpar AB. Malignant phylloides tumor in pregnancy. Am Surg. 2010;76:302–5. [PubMed] [Google Scholar]
- 4.Way JC, Culham BA. Phyllodes tumour in pregnancy: a case report. Can J Surg. 1998;41:407–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma JB, Wadhwa L, Malhotra M, et al. A case of huge enlargement of cystosarcoma phylloides of breast in pregnancy. Eur J Obstet Gynecol Reprod Biol. 2004;115:237–9. doi: 10.1016/j.ejogrb.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Nejc D, Pasz-walczak G, Piekarski J, et al. Astonishingly rapid growth of malignant cystosarcoma phyllodes tumor in a pregnant woman-a case report. Int J of Gynecol Cancer. 2008;18:856–9. doi: 10.1111/j.1525-1438.2007.01077.x. [DOI] [PubMed] [Google Scholar]
- 7.Mrad K, Driss M, Maalej M, Romdhane KB. Bilateral cystosarcoma phyllodes of the breast: A case report of malignant form with contralateral benign form. Ann Diagn Pathol. 2000;4:370–2. doi: 10.1053/adpa.2000.19375. [DOI] [PubMed] [Google Scholar]
- 8.Vorherr H, Vorherr UF, Kutvirt DM, Key CR. Cystosarcoma phyllodes: Epidemiology, pathohistology, pathobiology, diagnosis, therapy, and survival. Arch Gynecol. 1985;236:173–81. doi: 10.1007/BF02133961. [DOI] [PubMed] [Google Scholar]
- 9.Karim RZ, Gerega SK, Yang YH, et al. Phyllodes tumours of the breast: a clinicopathological analysis of 65 cases from a single institution. Breast. 2009;18:165–70. doi: 10.1016/j.breast.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Sugie T, Takeuchi E, Kunishima F, et al. A case of ductal carcinoma with squamous differentiation in malignant phyllodes tumor. Breast Cancer. 2007;14:327–32. doi: 10.2325/jbcs.14.327. [DOI] [PubMed] [Google Scholar]
- 11.Soumarová R, Seneklová Z, Horová H, et al. Retrospective analysis of 25 women with malignant cystosarcoma phyllodes-treatment results. Arch Gynecol Obstet. 2004;269:278–81. doi: 10.1007/s00404-003-0593-7. [DOI] [PubMed] [Google Scholar]
- 12.Staren ED, Lynch G, Boyle C, et al. Malignant cystosarcoma phyllodes. Am Surg. 1994;60:583–5. [PubMed] [Google Scholar]