Abstract
Background: Edinburgh Postnatal Depression Scale (EPDS) has been used as a reliable screening tool for postpartum depression in many countries. This study aimed to assess the psychometric properties and diagnostic accuracy of the EPDS in a sample of Iranian women.
Methods: Using stratified sampling 262 postpartum women (2 weeks-3 months after delivery) were selected from urban and rural health center in the city of Isfahan. They were interviewed using EPDS and Hamilton depression rating scale (HDRS). Data were assessed using factor analysis, diagnosis analysis of receiver operating characteristic (ROC) curve, Cronbach's alpha and Pearson correlation coefficient.
Results: The age of then participants ranged 18-45 years (26.6±5.1). Based on a cut-off point of >13 for HDRS, 18.3% of the participants.
The overall reliability (Cronbach's alpha) of EPDS was 0.79. There was a significant correlation (r2=0.60, P value<0.01) between EPDS and HDRS. Two factor analysis showed that anhedonia and depression were two explanatory factors. At a cut-off point12 the sensitivity of the questionnaire was 78% (95% CI: 73%-83%) and its specificity was 75% (95% CI: 72%-78%).
Conclusion: The Persian version of the EPDS showed appropriate psychometric properties diagnostic accuracy index. It can be used by health system professionals for detection, assessment and treatment for mothers with post partum depression.
Key Words: Depression, psychometrics, postpartum depression, postnatal depression
Introduction
Postpartum depression (PPD) is a non-psychotic depressive episode of mild to moderate severity, beginning in or extending into the first postnatal year.1 It is one of the most common risks for mothers after the stressful period of pregnancy and delivery.2
Postpartum depression not only has a negative effect on mother-infant and marital relationship, but also causes depression in the husbands,3 causes or aggravates marital problems, and even leads to separation or divorce.4 A depressed mother cannot have a suitable emotional connection with her child, and this leads to negative impact on mother-infant relationship, and child’s cognitive development.5 In special cases of PPD there is a risk of suicide and injury to neonates, which is always a very sad event.6
In two prospective studies the prevalence of PPD in the 6th week post partum in England,7 and the US,8 was estimated to be 9.1% and 15.4%, respectively. In a study using Beck depression scale for screening of PPD among 6628 women during 2-12 months after delivery in rural parts of Isfahan province in Iran, the prevalence of moderately and severely depressed women was 19.3% and 19.8%, respectively.9 A meta-analysis of 59 studies with a total sample of 12 810 women found that the average prevalence rate of non-psychotic PPD was 13% (95% CI: 12.3–13.4).10
Evidence demonstrates that all countries face the challenge of PPD, but low-to middle-income countries face the greatest burden. The evidence also shows that not all women are assessed for PPD, nor do all women receive treatment.11 Moreover, it has recently been shown that in Iran the prevalence of mental disorders in women (25.9%) was higher than men (15.9%).12
Given the high prevalence and high morbidity of undiagnosed PPD, the screening of mothers during postpartum period for early detection of those with probable PPD has always been a matter of interest for the researchers and clinicians.
One of the prominent tools for the diagnosis of PPD is the Edinburgh Postnatal Depression Scale (EPDS) that was designed by Cox et al. in 1987 as a self-report questionnaire.13 The EPDS consists of 10 items with acceptable sensitivity, specificity and positive predictive value. It has been used in many studies, and has been introduced as a valuable and powerful PPD screening tool in different cultures.10
Although evidence surrounding clinical and cost-effectiveness of various methods of identifying PPD is lacking,14 it has been suggested that EPDS is not only an acceptable and desirable screening tool of PPD from women's views, but also a suitable tool for universal perinatal depression screening from policy-maker’s views.15
Berle et al. reported that the Norwegian translation of EPDS served equally well as other translations as a screening tool for postnatal depression.16
Vega-Dienstmaiar et al. in a study on 321 women in the first year after delivery reported that EPDS had a maximum cut-off point of 13.5, a sensitivity of 84%, and a specificity of 79% in diagnosis of major depressive disorder (MDD). They reported a correlation coefficient of 0.44 between EPDS and some of the symptoms of MDD and a Cronbach's alpha=0.70, and concluded that Spanish version of EDPS had appropriate psychometric properties.17
Montazeri et al. in a study on 100 women in Iran showed that 22% in 6-8 weeks and 18% in 12-14 weeks after delivery developed PPD.18 Cronbach's alpha for the questionnaire used in the first period (test) was 0.77, and that for the second period (retest) was 0.86.
The SF36 questionnaire was used for determination of the validity of EPDS and coefficients were -0.41 in first period (test) and -0.57 in second period (retest).18 Howeverm, they did not assessed other important characteristics of EPDS such cut-off point, sensitivity and specificity.18
In another study by Mazhari et al. a Cronbach's alpha of 0.83 for the whole scale, and the best cut-off scores for major depression were 12/13 with a sensitivity and specificity of 95.3% and 87.9%, respectively.19
Considering the importance of EPDS, this study was designed to evaluate the full range of psychometric properties of EPDS including cut-off point, sensitivity, specificity, and diagnostic accuracy Index in a sample of Iranian women.
Materials and Methods
Participants
This is a cross-sectional descriptive study conducted in Isfanhan, Iran using 262 postpartum women selected using stratified random sampling method to examine psychometric properties of EPDS including cut-off point, sensitivity, specificity, and diagnostic accuracy index. The samples were selected from rural and urban centers of Isfahan, Iran among postpartum (2 weeks-3 months after delivery) women who had family records in governmental health centers.
Inclusion criteria for the participants were women in postpartum period (2 weeks-3 months after delivery), age of 18-49 years, and ability to read and write in Persian. Exclusion criteria included the presence of any psychiatric disorders according to a semi-structured clinical interview based on Diagnostic and Statistical Manual of Mental Disorders IV- Third Revision (DSM-IV-TR) by an expert and well-trained clinical psychologist, organic diseases causing depression, and being under treatment with psychiatric medications or any medications which affect the mood.
Materials
The EPDS and Hamilton Depression Rating Scale (HDRS) were used in this study.
Edinburgh Postnatal Depression Scale was designed by Cox et al. in 1987 in England. It is a 10-item scale, which focuses on the cognitive and affective features of depression rather than somatic symptoms. Edinburgh Postnatal Depression Scale is the only self-report scale that has been validated for use in pregnancy and postnatal period. It cannot confirm a diagnosis of depression, but a score of above 12 is widely used to indicate probable depressive disorder.13 The scale was understood and completed in similar ways by women in different English speaking and non-English speaking population groups in Australia. With the proviso that careful translation processes and extensive piloting of translations are always needed, these findings lend further support to the use of the EPDS in cross-cultural research on depression following child birth.20
In this study we used Persian version of EPDS prepared by Montazeri et al.18
Hamilton Depression Rating Scale (HDRS) is a clinical assessment scale, which was designed by Max Hamilton in 1960. It is one of the most reliable scales in depression assessment. The scale is an instrument for a semi-structured interview based on DSM-VI criteria, which is performed by a trained person.21
We used the HDRS as a gold standard of depression diagnosis in this study, because of its acceptability for this application.22 The scale characterizes the symptoms of depressed mood, cognitive and physical signs of depression, and signs and symptoms of anxiety. It has 17-items with five (0-4) or three (0-2) Likert spectrum scale and a cut-off point of 13.23
Data Collection Methods
Twenty urban and seven rural health centers were selected among 61 urban and 16 rural health centers using stratified random sampling method. According to the family records, 10 women with inclusion criteria were selected in each selected health center using simple random sampling method. All of the selected participants were invited to the health centers and the purpose and method of the study were explained to them. A written consent, approved by the Research Ethic Committee of Isfahan University of Medical Sciences, was obtained from all of the participants. Afterwards, a semi-structured interview was done with participants by a clinical psychologist using HDRS in a relaxed and private situation in health centers in the absence of any other person including their husbands and other family members. Then after a break of 15 minute, they filled EPDS as a self-report scale.
Data were analyzed using Statistical Package for Social Sciences (SPSS, version 15). Cronbach's alpha was used to assess the reliability of the EPDS and Pearson coefficient was used to determine the face and content validity of HDRS. Calculation of Z and T was used to determine of standard scores. For classifying the factors related to the items of the questionnaires, explanatory factor analysis was used with Eigen value greater than 1. Receiver operating characteristic (ROC) curves was used to find an optimum sensitivity, specificity and cut-off point based on a semi-structured clinical interview using HDRS as gold standard.
Results
Two hundred seventy postpartum mothers aged 18-45 years possessing the inclusion criteria were enrolled in this study. Eight of the participants were excluded from the study for different reasons including suspected psychosis or mental retardation, lack of reliability, or mood affecting medications. The age of the participants was 26.6±5.1 years (CI 95%: 25.9, 27.2). The time after delivery in non-depressed and depressed women were 52.5±27.2 months (CI 95%: 48.9, 56.1) and 56.4±27.3 months (CI 95%: 50.5, 62.3), respectively. Table 1 summarizes the frequency (%) of distribution some of the characteristics of postpartum women based on HDRS. Based on a cut-off point of 13, HDRS showed that 18.3% of the participants were depressed.
Table 1.
The number and percentage (%) of distribution of some of the characteristics of postpartum women in the study based on Hamilton Depression Rating Scale
| Characteristics | No-depress Depress | P value | ||
|---|---|---|---|---|
| Education | Primary | 44 (20.6) | 14 (29.2) | 0.154 |
| Secondary | 44 (20.6) | 14 (29.2) | ||
| College | 88 (41.1) | 16 (33.3) | ||
| University | 38 (17.8) | 4 (8.3) | ||
| Child sex | Boy | 100 (46.7) | 24 (50.0) | 0.682 |
| Girl | 114 (53.3) | 24 (50.0) | ||
| Number of child | One | 125 (58.4) | 22 (45.8) | 0.037 |
| Two | 68 (31.8) | 15 (31.3) | ||
| Three or more | 21 (9.8) | 11 (22.9) | ||
| Type of delivery | Vaginal | 92 (43.0) | 22 (83.3) | 0.720 |
| Cesarean | 122 (57.0) | 26 (54.2) | ||
| Feeding | Brest feeding | 196 (91.6) | 40 (83.3) | 0.188 |
| Ancillary | 5 (2.3) | 3 (6.3) | ||
| Both | 13 (6.1) | 5 (10.4) | ||
| Drug use | Yes | 25 (11.7) | 10 (20.8) | 0.092 |
| No | 189 (88.3) | 38 (79.2) | ||
| Job | Employee | 9 (4.2) | 1 (2.1) | 0.488 |
| Housekeeper | 205 (95.8) | 47 (97.9) | ||
The mean score of EPDS in this study was 10.2±5.3, and scale reliability calculated using Cronbach's alpha was 0.791. Cronbach's alpha range calculated by omitting each question ranged between 0.76-0.79. There was a significant correlation between EPDS and HDRS (r=0.62, P<0.001).
Kaiser-Meyer-Olkin index for adequacy of sample size was 0.84 with Bartlell's test of sphericity (X2=530, df=45, P<0.001). Explanatory factor analysis was done with Varimax rotation and two factors were extracted using principal component analysis method. On the whole, these two factors determined 62% of variance in all the questions (46.4 for depression item and 15.6 for anhedonia item). Table 2 shows these factors and their loads.
Table 2.
Explanatory factor loads for depression and anhedonia (the first and second factor) of the Edinburgh Postnatal Depression Scale.
| Questions | Anhedonia | Depression | Cornbache’s Alpha if item Deleted |
|---|---|---|---|
| 1-I have been able to laugh and see the funny side of things | 0.77 | - | 0.777 |
| 2-I have looked forward with enjoyment to things | 0.86 | - | 0.790 |
| 3-I have blamed myself unnecessarily when things went wrong | - | 0.57 | 0.778 |
| 4-I have been anxious or worried for no good reason | - | 0.69 | 0.762 |
| 5-I have felt scared or panicky for not very good reason | - | 0.58 | 0.775 |
| 6-Things have been getting on top of me | - | 0.60 | 0.769 |
| 7-I have been so unhappy that I have had difficulty sleeping | - | 0.58 | 0.767 |
| 8-I have felt sad or miserable | - | 0.69 | 0.759 |
| 9-I have been so unhappy that I have been crying | - | 0.67 | 0.769 |
| 10-The thought of harming myself has occurred to me | - | 0.46 | 0.782 |
| Eigen value | 1.6 | 3.1 | - |
| %Variance | 15.6 | 46.4 | - |
The T scores varied from 30.66 to 81.70, and Z scores were between -1.09 and 3.17.
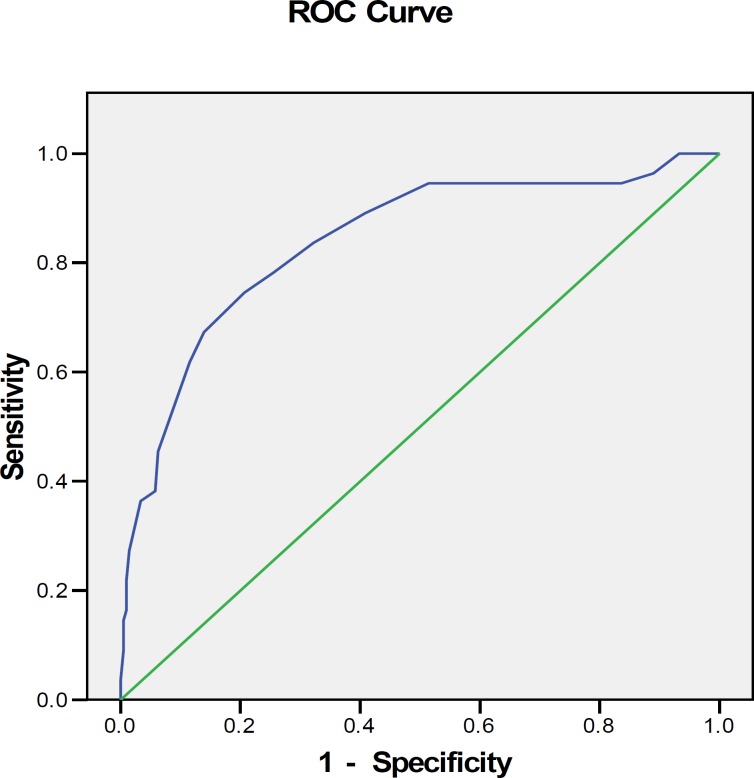
Receiver operating characteristic curves show that using a cut-off point of >12 to differentiate depressed people, the sensitivity and specificity were 78% and 75%, respectively (table 3), and the area under the curve was 0.84 (CI 95%: 0.77-0.90) (figure 1).
Table 3.
The sensitivity and specificity of Edinburgh Postnatal Depression Scale (EPDS) using different cut-off points
| Cut point | Sensitivity | Specificity |
|---|---|---|
| 11 | 0.836 | 0.322 |
| 12 | 0.782 | 0.255 |
| 13 | 0.745 | 0.207 |
| 14 | 0.673 | 0.139 |
| 15 | 0.618 | 0.115 |
Figure 1.
Receiver operating characteristic (ROC) curve according to Hamilton Depression Rating Scale using cut-off point of 13.
Discussion
Edinburgh postnatal depression scale is the most-used scale for screening the depression in postnatal period worldwide. It has already been validated in many countries.10
This study aimed to determine the psychometric properties of Persian version of the EPDS.
Isfahan as an industrial province in central zone of Iran, and is a destination of immigration from other areas of the country. The population composition of Isfahan is so varied that practically every Iran's ethnicity is represented in the province.24 Therefore, the participants in this study can be considered a representative of the Iranian urban and rural population. The sample size of the study (n=262) is considered proper for explanatory and confirmatory factor analysis.
Our results showed that EPDS had a Cronbach's alpha of 0.79. Montazeri et al. in a previous study in an Iranian sample determined Cronbach's alpha of EPDS in two stages to be 0.77 and 0.86.18 In other studies it was reported to be 0.72,16 0.70,17 and 0.83,25 respectively.
For validity evaluation, correlation coefficients of the EPDS and HDRS scores was 0.60 and 0.73 which were significant (P value=0.01
These results are in agreement with the results of a study in Malaysia which reported a correlation coefficient of 0.88.26 Montazeri et al. study in Tehran used correlation coefficient with SF36 for validity determination of EPDS and reported this coefficient as -0.41 in first stage and -0.57 in second stage.18
To determine the validity of EPDS, Montazeri et al.18 examined its correlation coefficient with SF36. They reported a coefficient as -0.41 in first stage and -0.57 in second stage.18 In another study in Iran by Mazhari et al. the coefficient for the whole scale was 0.83.19
In Norway Beck Depressive Inventory (BDI) and HDRS scales were used for the determination of correlation coefficients, which were reported to be 0.68 and 0.55, respectively.16 In the lithuania, a correlation coefficient of 0.83 was reported between Composite International Diagnostics Interview Short Form (CIDI-SF) and EPDS.25
Explanatory factor analysis was conducted, and two factors were determined with the common variance of 46.4%. These factors included anhedonia (first factor, questions 1 and 2) and depression (second factor, questions 3-9). Our findings confirm the multidimensionality of EPDS, demonstrating a two factor structure with similar loadings. Since Cox et al. suggested that EPDS had a one dimensional aspect,13 a number of studies that have examined its structure, have found the EPDS to be multidimensional and that it can distinguish two,27-30 or three,18,30-33 factors with near range of loadings. These findings may be explained by the different periods of application of EPDS or the different culture backgrounds.32
The load of presentation of a major depressive symptom is a culture-bound phenomenon with somatic presentation is prominent in the eastern and mental presentation in western societies,34 and this may be explained by the differences in the findings from explanatory factor analysis of this scale in different studies.
Although the first validation study,13 suggested the 9/10 as the cut-off score for use of the scale in the community surveys and screening, the 12/13 threshold was more useful in the clinic assessment of the postnatal depression.35
Berle et al.16 reported a cut-off point of 11, a sensitivity of 96%, a specificity of 78%, and positive predictive value of 59%, and negative predictive value of 62%, which are somehow different from our results. In Spain the EPDS cut-off point was reported as 13.5 with a sensitivity of 84% and a specificity of 79%.17 A cut-off of 11/12 was reported as more suitable for screening a French population,36 and a cut-off score of 8/9 with a sensitivity of 94.4% and a specificity of 87.4% was more appropriate in an Italian population.37
In the present study, the optimal sensitivity of 78%, specificity of 75%, and the area under the curve of 0.84 (CI 95%: 0.77-0.90), which was obtained by ROC curve with cut-off point of 13 in HDRS, allows the use of this score in the community screenings. Given the false positivity of EPDS and the importance of differentiating various forms of major depression by clinical interviews for different managements, our choice of cut-off point score was mandated by the need to screen mothers rather than to definite diagnosis of depression. Therefore, we propose a clinical interview for definite diagnosis of MDD in those with a score of above 12 in EPDS.
The present study suffers from the fact that the prevalence rate of 18.3% for postnatal depression that we achieved is more than the average prevalence rate of 13% reported by O'hara in a meta-analysis of 59 studies.10 This may be a limitation for the positive and negative predictive values of this version. However, the similarity of our prevalence rate with other studies in Iran,38 might support our findings that the rate of depression might be higher in Iran.
Conclusion
The findings of the present study indicate that the Persian version of the EPDS has a satisfactory reliability and factor analysis indicated by two components. Receiver operating characteristic curve analysis versus HDRS provides the score of 12 as the best cut-off point for PPD screening in Iranian society.
Acknowledgment
We are grateful to all participants and staff of local health centers, who helped us to conduct this study. This study was supported by a research grant from the Vice-Chancellor for Research, Isfahan University of Medical Sciences.
Conflict of Interest: None declared
References
- 1.Scottish Intercollegiate Guidelines Network. Management of postnatal depression and puerperal psychosis. A national clinical guideline, guideline number 6. Edinburgh: SIGN Executive; 2002. [Google Scholar]
- 2.Vesga-López O, Blanco C, Keyes K, et al. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65:805–15. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roberts SL, Bushnell JA, Collings SC, Purdie GL. Psychological health of men with partners who have post-partum depression. Aust N Z J Psychiatry. 2006;40:704–11. doi: 10.1080/j.1440-1614.2006.01871.x. [DOI] [PubMed] [Google Scholar]
- 4.Seto M, Cornelius MD, Goldschmidt L, et al. Long-term effects of chronic depressive symptoms among low-income childrearing mothers. Matern Child Health J. 2005;9:263–71. doi: 10.1007/s10995-005-0002-x. [DOI] [PubMed] [Google Scholar]
- 5.Tronick E, Reck C. Infants of depressed mothers. Harv Rev Psychiatry. 2009;17:147–56. doi: 10.1080/10673220902899714. [DOI] [PubMed] [Google Scholar]
- 6.Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health. 2005;8:77–87. doi: 10.1007/s00737-005-0080-1. [DOI] [PubMed] [Google Scholar]
- 7.Evans J, Heron J, Francomb H. cohort study of depression mood during pregnancy and after childbirth. BMJ. 2001;323:257–60. doi: 10.1136/bmj.323.7307.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Segre LS, O’Hara MW, Arndt S, Stuart S. The prevalence of postpartum depression: the relative significance of three social status indices. Soc Psychiatry Psychiatr Epidemiol. 2007;42:316–21. doi: 10.1007/s00127-007-0168-1. [DOI] [PubMed] [Google Scholar]
- 9.Maracy MR, Barekatain M, et al. Risk Factors of Postpartum Depression in Rural Areas of Isfahan Province, Iran. Arch Iranian Med. 2009;12:461–7. [PubMed] [Google Scholar]
- 10.Gibson J, McKenzie-Mcharg K, Shakespeare J, et al. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119:350–64. doi: 10.1111/j.1600-0447.2009.01363.x. [DOI] [PubMed] [Google Scholar]
- 11.Almond P. Postnatal depression: a global public health persprcive. Perspect Public Health. 2009;129:221–7. doi: 10.1177/1757913909343882. [DOI] [PubMed] [Google Scholar]
- 12.Noorbala AA, Yasamy MT, Mohammad K. Mental health survey of the adult population in Iran. Br J Psychiatry. 2004;184:70–3. doi: 10.1192/bjp.184.1.70. [DOI] [PubMed] [Google Scholar]
- 13.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–6. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 14.Hewitt C, Gilbody S, Brealey S, et al. Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis. Health Technol Assess. 2009;13:1–145. doi: 10.3310/hta13360. [DOI] [PubMed] [Google Scholar]
- 15.Gemmill AW, Leigh B, Ericksen J, Milgrom J. A survey of the clinical acceptability of screening for postnatal depression in depressed and non-depressed women. BMC Public Health. 2006;6:211. doi: 10.1186/1471-2458-6-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berle JØ, Aarre TF, Mykletun A, et al. Screening for Postnatal depression validation of the Norwegian version of the Edinburgh Postnatal depression scale and assessment of risk factors for postnatal depression. J Affect Disord. 2003;76:151–6. doi: 10.1016/s0165-0327(02)00082-4. [DOI] [PubMed] [Google Scholar]
- 17.Vega-Dienstmaiar JM. Validation of a Spanish version of the Edinburgh postnatal depression scale. Actas Esp Psiquiatr. 2002;30:106–11. [PubMed] [Google Scholar]
- 18.Montazeri A, Torkan B, Omidvari S. The Edinburgh postnatal depression scale: translation and validation study of the Iranian version. BMC Psychiatry. 2007:7–11. doi: 10.1186/1471-244X-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mazaheri S, Nakhaee N. Validation of the Edinburgh postnatal depression scale in an Iranian sample. Arch Women Ment Health. 2007;10:293–7. doi: 10.1007/s00737-007-0204-x. [DOI] [PubMed] [Google Scholar]
- 20.Small R, Lumley J, Yelland J, Brown S. The performance of the Edinburgh Postnatal Depression Scale in English speaking and non-English speaking populations in Australia. Soc Psychiatry Psychiatr Epidemiol. 2007;42:70–8. doi: 10.1007/s00127-006-0134-3. [DOI] [PubMed] [Google Scholar]
- 21.Williams JB, Kobak KA, Bech P, et al. The GRID-HAMD: standardization of the Hamilton Depression Rating Scale. Int Clin Psychopharmacol. 2008;23:120–9. doi: 10.1097/YIC.0b013e3282f948f5. [DOI] [PubMed] [Google Scholar]
- 22.Shuang J, Long Q, Newport DJ, et al. Validity of depression rating scales during pregnancy and the postpartum period: Impact of trimester and parity. J Psychiatr Res. 2011;45:213–9. doi: 10.1016/j.jpsychires.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bagby RM, Ryder AG, Schuller DR, Marshall MB. The Hamilton Depression Rating Scale: has the Gold Standard Become a Lead Weight? Am J Psychiatry. 2004;161:2163–77. doi: 10.1176/appi.ajp.161.12.2163. [DOI] [PubMed] [Google Scholar]
- 24.Golbabaei F, Islami F. Evaluation of workers' exposure to dust, ammonia and endotoxin in poultry industries at the province of Isfahan, Iran. Ind Health. 2000;38:41–6. doi: 10.2486/indhealth.38.41. [DOI] [PubMed] [Google Scholar]
- 25.Bunevicius A, Kusminskas L, BuneviciusR P02-206 Validity of the Edinburgh postnatal depression scale. European Psychiatry. 2009;24:896–902. [Google Scholar]
- 26.Rashidi WM, Amir A, Mahmood NM. Revalidation of the Malay Version of the Edinburgh Postnatal Depression Scale (EPDS) Among Malay Postpartum Women Attending the Bakar Bata Health Center in Alor Setar, Kedah, Northwest of Peninsular Malaysia. Malaysian Journal of Medical Sciences. 2003;10:71–5. [PMC free article] [PubMed] [Google Scholar]
- 27.Jomeen J, Martin CR. Replicability and stability of the multidimensional model of the Edinburgh Postnatal Depression Scale in late pregnancy. J Psychiatr Ment Health Nurs. 2007;14:319–24. doi: 10.1111/j.1365-2850.2007.01084.x. [DOI] [PubMed] [Google Scholar]
- 28.Jomeen J, Martin CR. Self-esteem and mental health during early pregnancy. Clinical Effectiveness in Nursing. 2005;9:92–5. [Google Scholar]
- 29.Chabrol H, Teissedre F. Relation between Edinburgh Postnatal Depression Scale scores at 2-3 days and 4-6 weeks post-partum. J Reprod Infant Psychol. 2004;22:33. [Google Scholar]
- 30.Ross LE, Sellers EM, Romach MK. Mood changes during pregnancy and the postpartum period: development of a biopsychosocial model. Acta Psychiatr Scand. 2004;109:457–66. doi: 10.1111/j.1600-0047.2004.00296.x. [DOI] [PubMed] [Google Scholar]
- 31.Brouwers EP, Pop VJ. Does the Edinburgh Postnatal Depression Scale measure anxiety? J Psychosom Res. 2001;51:659–63. doi: 10.1016/s0022-3999(01)00245-8. [DOI] [PubMed] [Google Scholar]
- 32.Chabrol H, Teissedre F. Relation between Edinburgh Postnatal Depression Scale scores at 2-3 days and 4-6 weeks post-partum. J Reprod Infant Psychol. 2004;22:33. [Google Scholar]
- 33.Jomeen J, Martin CR. Confirmation of an occluded anxiety component within the Edinburgh Postnatal Depression Scale (EPDS) during early pregnancy. Journal of Reproductive and Infant Psychology. 2005;23:143–54. [Google Scholar]
- 34.Benjamin JS, Virginia AS. Comprehensive text book of psychiatry. Philadephia: Lippinncot Williams and Wilkins; 2009. [Google Scholar]
- 35.Vivilaki VG, Dafermos V, Kogevinas M, et al. The Edinburgh Postnatal Depression Scale: translation and validation for a Greek sample. BMC Public Health. 2009;9:329. doi: 10.1186/1471-2458-9-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guedeney N, Fermanian J. Validation study of French version of the Edinburgh Postnatal Depression Scale (EPDS) Eur Psychiatry. 1998;13:83–9. doi: 10.1016/S0924-9338(98)80023-0. [DOI] [PubMed] [Google Scholar]
- 37.Benvenuti P, Ferrara M, Niccolai C, et al. The Edinburgh Postnatal Depression Scale: validation on an Italian sample. J Affect Disord. 1999;53:137–41. doi: 10.1016/s0165-0327(98)00102-5. [DOI] [PubMed] [Google Scholar]
- 38.Bahadoran P, Ehsanpour S, Abedi A. A meta-analysis on studies about obstetric risk factors of postpartum depression in Iran within 1995-2005. IJNMR. 2008;13:129–33. [Google Scholar]