Abstract
Illicit drug use continues to be a common problem among pediatric patients. Daily marijuana use among high school seniors is currently at a 30-year high. Marijuana use in adults has rarely been associated with cardiovascular adverse effects, including hypertension, tachycardia, arrhythmia, and myocardial infarction. Recently, abuse of synthetic cannabinoids, such as the incense “K2” or “Spice,” has been increasingly reported in the lay press and medical literature. Overdose and chronic use of these substances may cause adverse effects including altered mental status, tachycardia, and loss of consciousness. Overdoses in adult patients have been described; however, limited reports in the pediatric population have been documented. A recent case series describes myocardial infarctions in pediatric patients, associated with synthetic cannabinoid use. In this report, we describe two adolescent patients admitted after they inhaled “K2,” resulting in loss of consciousness, tachycardia, and diffuse pain.
INDEX TERMS: K2, Spice, synthetic cannabinoids
INTRODUCTION
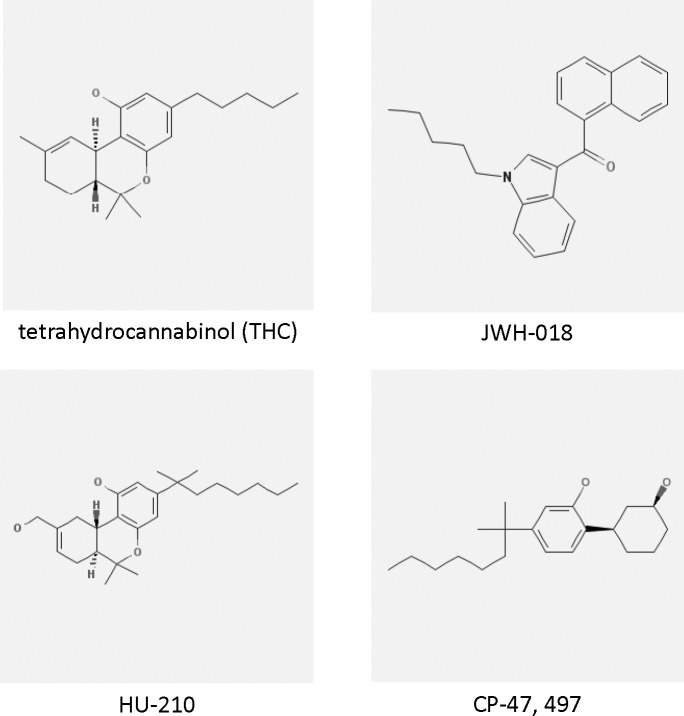
Drug use and abuse continue to remain major health problems among adolescents and young adults.1 More than half of high school students have been reported to have used illicit drugs such as marijuana.2 Marijuana use and abuse have important health, social, and legal consequences, and proper education for caregivers and patients is imperative to address these issues.2,3 In the recent past, compounds similar to tetrahydrocannabinol (THC), the active ingredient in marijuana, have been synthetically produced and previously offered commercially as legal substances. Use and abuse of these cannabinoids has been reported in the lay press.4 A national survey in 2011 indicated 11.4% of high school seniors had used these products within the last 12 months.1 These substances include either THC or THC-like compounds such as JWH-018, HU-210, or CP-47, 497 (Figure) and can produce euphoria, relaxation, and loss of inhibitions.4–8 Often referred to as “Spice” or “K2,” these products are commonly sold as incense and may contain combinations of synthetic cannabinoids and other chemicals. A variety of formulations of these products are available for purchase on the Internet or in stores specializing in tobacco or drug paraphernalia (Table). They are often inhaled via a pipe or rolled into a cigarette.9
Figure.
Chemical structures of THC, JWH-018, HU-210, and CP-47,49726
Table.
Brand Names of Common Synthetic Cannabinoids Available on the Internet25
A few case reports have been published linking the abuse of “K2” with signs or symptoms of addiction or withdrawal.8,10 In those cases, cardiovascular and neurological symptoms, including tachycardia, myocardial infarction, and loss of consciousness, were reported.8,10,11 As of December 2010, 8264 exposures to these substances in adults and children were reported to United States Poison Centers, including involvement in 4 deaths.12 Over the same time frame, approximately two-thirds of the cases were reported to be exposure to marijuana, cocaine, and bath salts.12 These reports of overdose and adverse effects have led to the emergency scheduling of several of these substances, including JWH-018, JWH-073, JWH-200, CP-47,497, and cannabicyclohexanol, as Schedule I by the United States Drug Enforcement Agency (DEA) in November 2010.13 Despite the growing body of literature, there is limited information describing the effects of these substances in pediatric patients.11,14
CASE 1
A 17-year-old Caucasian male was found by his mother slumped over on the couch with increased generalized muscular tone in the extremities, cyanosis, and apnea. Upon stimulation, he began to breathe spontaneously and progressively regained responsiveness in a stuporous and confused state for the 10 minutes prior to arrival of emergency medical services. He was noted to have ocular redness and swelling. His initial heart rate in the prehospital setting was 180 BPM, with questionable supraventricular tachycardia. He was given adenosine, 6 mg intravenously, which decreased the heart rate to 140 BPM, consistent with sinus tachycardia. Upon presentation to the emergency department (ED), his muscular tone had improved, and his sinus rhythm had returned to normal. He continued to have altered mental status, with confused speech and somnolence, but he was able to complain of chest and back pain. In the ED, the patient admitted inhaling “K2” via a pipe approximately 2 hours prior to admission. He stated that he purchased it from a local store and reported using it previously on multiple occasions with no adverse reactions. It was unclear the exact brand and amount of product used by the patient. He was admitted to the pediatric intensive care unit (PICU) for close observation of his mental status and chest pain and for monitoring of recurrence of arrhythmias.
His medical history included heroin abuse for which he was in an outpatient treatment program. His most recent use of heroin had been 10 days prior to admission. He was not taking any prescription or over-the-counter medications. He denied any other recent illicit drug abuse and was witnessed to be in his usual state of health 2 hours prior to being discovered in an unresponsive state.
Upon admission to the PICU, the patient's heart rate was 89 BPM, blood pressure was 117/76 mm Hg, respiratory rate was 19 breaths per minute, and arterial O2 saturation was 100% on room air. Generally, he was alert, oriented, and appropriate and complained of diffuse muscular pain and weakness, especially upon inspiration. His mental status had returned to baseline, roughly 8 to 12 hours after inhalation of “K2.” His pupils were 4 to 5 mm and reactive. His initial serum chemistry analysis, complete blood count, and liver function test results were within normal limits. His initial creatine kinase was 208 IU/L (normal range, 25 to 260 IU/L). Urine and blood drug screen results were negative except for cannabinoids.
Overnight, the patient's pain slowly subsided, requiring only treatment with acetaminophen. His mental status remained appropriate throughout the remainder of his hospital stay. His repeated laboratory test values remained normal except for an increase in creatine kinase to 1157 IU/L. His CK-MB, troponin, and telemetry findings remained normal throughout his hospital stay. The patient was discharged home on the day after admission, with follow-up with his substance abuse treatment program.
CASE 2
A 15-year-old Caucasian male was found unconscious and was transported to the ED, where he was unresponsive and had a heart rate of 172 BPM and a blood pressure of 162/57 mm Hg. His respiratory rate and oxygen saturation were 16 breaths per minute and 99% on room air, respectively. An EKG performed at the time showed sinus tachycardia. The patient regained consciousness but was unable to recall the event and complained of a mild headache and fatigue. In the ED, he reported smoking “K2” via cigarette approximately an hour prior to admission. The quantity and brand of product ingested were unknown. Thirty minutes after regaining consciousness, his heart rate and blood pressure decreased to 92 BPM and blood pressure to 129/65 mm Hg, respectively. The patient was admitted to the PICU to monitor his mental status, blood pressure, and telemetry for arrhythmias.
The patient had a medical history significant for substance abuse, including marijuana and alcohol. He denied ingesting any other substance prior to admission and was taking no prescription or over-the-counter medications.
Upon admission to the PICU, urine drug screen and serum drug concentration tests for acetaminophen, ethanol, and salicylates were performed with negative results, including cannabinoids. His serum chemistry results were normal with the exception of serum potassium of 2.5 mEq/L (normal range 3.5 to 5 mEq/L). The patient was placed on continuous telemetry and maintenance intravenous fluids containing potassium. Overnight, the patient's heart rate, blood pressure, and serum potassium levels normalized. The following morning, he was at his mental baseline and was discharged home with outpatient substance abuse follow-up.
DISCUSSION
“K2” or “Spice” intoxication continues to be a growing health concern. Several studies in adults have linked the use of synthetic cannabinoids to cardiovascular and neurological symptoms, while limited reports have been published in the pediatric population.4–8,11,14 The youngest patients in those case reports were 16 years of age.11 The three patients experienced several days of chest pain requiring presentation to the ED. All three patients developed ST segment changes and elevations in troponin values, consistent with myocardial infarction. These symptoms developed several days after ingestion of “K2.”11
The use of marijuana and its active compound THC have been linked to tachycardia, hypertension, cardiac arrhythmias, myocardial infarction, transient ischemic attacks, and ST segment abnormalities.3,15–20 As seen in our patients, use of synthetic cannabinoids such as “K2” can cause symptoms similar to marijuana use.7,8
Synthetic cannabinoids were originally developed for potential medicinal purposes and to study the effects of cannabinoid receptors.20 Since the initial reports of its abuse in 2008, additional information has been gathered regarding the pharmacology and toxicity of these products. Synthetic cannabinoids appear to be 4 to 5 times more potent and appear to have more pronounced and severe cardiovascular adverse effects than traditional marijuana. Various case reports suggest heart palpitations, tachycardia, hypertension, chest pain, hallucinations, and seizures are common adverse effects associated with these compounds.4–8,11,14,20 Additionally, case reports have hinted at the rapid development of tachyphylaxis after only a few doses, potentially leading to an increased risk of overdose with continued use.4,20,21 In theory, these products may also have weak monoamine oxidase inhibition activity at large doses, resulting in the risk for serotonin syndrome.20,21 Analysis of several “K2” products has suggested the presence of high concentrations of other chemicals, including vitamin E and clenbuterol, a potent β2-agonist.20,21 The cardiac arrhythmias seen may be attributed to the β-agonist activity of clenbuterol. In addition to the immediate toxicities reported with “K2,” there is concern over the potential long-term effects of chronic long-term use of large amounts of marijuana as this has been associated with increased rates of schizophrenia and possible memory loss.22,23
Routine urine drug screens for cannabinoids may be negative for these synthetic compounds. Although there is not a specific toxidrome associated with synthetic THC products, patients will often present with altered mental status, including anxiety, euphoria, or frank loss of consciousness, significant tachycardia, and injected conjunctivae.4–8,11,14 Clinical testing for these compounds is currently under development.24 It is unknown at this time when these tests will become commercially available. This testing may provide a better appreciation for the spectrum of adverse effects associated with these compounds and improved patient education regarding the risks of “K2” abuse. However, these clinical tests will most likely only detect the most common synthetic cannabinoids. The authors encourage pediatricians to stay abreast of the growing trend toward synthetic cannabinoid use as an alternative means of “getting high.” Initial management of these patients should include monitoring telemetry for arrhythmia, myocardial ischemia, and serum electrolytes, ensuring a secure airway, and screening for other substances potentially ingested. Recommended supportive care includes benzodiazepines as needed for hallucinations and agitation and intravenous fluids and electrolytes to manage volume and electrolyte disturbances. Despite the recent DEA restrictions placed on these compounds, the authors believe the ease of attainment on the Internet creates the potential for “K2” to quickly become an escalating, serious drug of abuse by the pediatric population in the United States.
ABBREVIATIONS
- BPM
beats per minute
- CK-MB
creatine kinase-MB subtype
- DEA
Drug Enforcement Agency
- ED
emergency department
- EKG
electrocardiogram
- EMS
emergency medical services
- GCS
Glasgow Coma Scale
- PICU
pediatric intensive care unit
- THC
tetrahydrocannabinol
Footnotes
DISCLOSURE The authors declare no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria.
REFERENCES
- 1.O'Malley PM, Bachman JG, Schulenberg JE. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2012. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2011. [Google Scholar]
- 2.Committee on Substance Abuse. Marijuana: a continuing concern for pediatricians. Pediatrics. 1999;104:982–985. [PubMed] [Google Scholar]
- 3.Kalant H. Adverse effects of cannabis on health: an update of the literature since 1996. Prog Neuropsychopharmacol Biol Psychiatry. 2004;28:849–863. doi: 10.1016/j.pnpbp.2004.05.027. [DOI] [PubMed] [Google Scholar]
- 4.Vardakou I, Pistos C, Spiliopoulou C. Spice drugs as a new trend: mode of action, identification and legislation. Toxicol Lett. 2010;197:157–162. doi: 10.1016/j.toxlet.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 5.Atwood BK, Huffman J. Straiker, et al. JWH018, a common constituent of “Spice” herbal blends, is a potent and efficacious cannabinoid CB1 receptor agonist. Br J Pharmacol. 2010;160:585–593. doi: 10.1111/j.1476-5381.2009.00582.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Auwärter V, Dresen S, Weinmann W, et al. Spice and other herbal blends: harmless incense or cannabinoid designer drugs? J Mass Spectrom. 2009;44:832–837. doi: 10.1002/jms.1558. [DOI] [PubMed] [Google Scholar]
- 7.Jiang W, Zhang Y, Xiao L, et al. Cannabinoids promote embryonic and adult hippocampus neurogenesis and produce anxiolytic- and antidepressant-like effects. J Clin Invest. 2005;115:3104–3116. doi: 10.1172/JCI25509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zimmermann US, Winkelmann PR, Pilhatsch M, et al. Withdrawal phenomena and dependence syndrome after the consumption of “Spice Gold.”. Deutsches Aerzteblatt Intern. 2009;106:464–467. doi: 10.3238/arztebl.2009.0464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moussouttas M. Cannabis use and cerebrovascular disease. Neurology. 2004;10:47–53. doi: 10.1097/01.nrl.0000107493.19282.b0. [DOI] [PubMed] [Google Scholar]
- 10.Müller H, Sperling W, Köhrmann M, et al. The synthetic cannabinoid Spice as a trigger for an acute exacerbation of cannabis induced recurrent psychotic episodes. Schizophr Res. 2010;118:309–310. doi: 10.1016/j.schres.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Mir A, Obafemi A, Young A, Cane C. Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics. 2011;128:e1622–e1627. doi: 10.1542/peds.2010-3823. [DOI] [PubMed] [Google Scholar]
- 12.Bronstein AC, Spyker DA, Cantilena LR, et al. 2010 Annual report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 28th annual report. Clin Tox. 2011;49:910–941. doi: 10.3109/15563650.2011.635149. [DOI] [PubMed] [Google Scholar]
- 13.United States Drug Enforcement Administration. Washington, DC: US DEA; 2010. 2012. DEA Moves to Emergency Control Synthetic Marijuana: Agency Will Study Whether To Permanently Control Five Substances. November 24. http://www.justice.gov/dea/pubs/pressrel/pr112410p.html. Accessed July 14. [Google Scholar]
- 14.Vearrier D, Osterhoudt KC. A teenager with agitation: higher than she should have climbed. Pediatr Emerg Care. 2010;26:462–465. doi: 10.1097/PEC.0b013e3181e4f416. [DOI] [PubMed] [Google Scholar]
- 15.Daccarett M, Freih M, Machado C. Acute cannabis intoxication mimicking brugada-like ST segment abnormalities. Int J Cardiol. 2007;119:235–236. doi: 10.1016/j.ijcard.2006.07.114. [DOI] [PubMed] [Google Scholar]
- 16.Mittleman MA, Lewis RA, Maclure M, et al. Triggering myocardial infarction by marijuana. Circulation. 2001;193:2805–2809. doi: 10.1161/01.cir.103.23.2805. [DOI] [PubMed] [Google Scholar]
- 17.Kosior DA, Filipiak KJ, Stolarz P, et al. Paroxysmal atrial fibrillation in a young female patient following marijuana intoxication—a case report of possible association. Med Sci Monit. 2000;6:386–389. [PubMed] [Google Scholar]
- 18.Wilens TE, Biedermann J, Spencer TJ. Case study: adverse effects of smoking marijuana while receiving tricyclic antidepressants. J Am Acad Child Adolesc Psych. 1997;36:45–48. doi: 10.1097/00004583-199701000-00016. [DOI] [PubMed] [Google Scholar]
- 19.Mouzak A, Agathos P, Kerezoudi E, et al. Transient ischemic attack in heavy cannabis smokers-how “safe” is it? Eur Neurol. 2000;44:42–44. doi: 10.1159/000008191. [DOI] [PubMed] [Google Scholar]
- 20.Wells DL, Ott CA. The “new” marijuana. Ann Pharmacother. 2011;45(3):414–417. doi: 10.1345/aph.1P580. [DOI] [PubMed] [Google Scholar]
- 21.European Monitoring Centre for Drugs and Drug Addiction. Synthetic cannabinoids and “Spice.”. 20112012 September 15. http://www.emcdda.europa.eu/publications/drug-profiles/synthetic-cannabinoids/. Accessed July 14. [Google Scholar]
- 22.Cyril D'Souza D, Sewell RA, Ranganathan M. Cannabis and psychosis/schizophrenia: human studies. Eur Arch Psychiatry Clin Neurosci. 2009;259:413–431. doi: 10.1007/s00406-009-0024-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yucel M, Solowij N, Respondek C, et al. Regional brain abnormalities associated with long-term heavy cannabis use. Arch Gen Psychiatry. 2008;65:694–701. doi: 10.1001/archpsyc.65.6.694. [DOI] [PubMed] [Google Scholar]
- 24.Sobolevsky T, Prasolov I, Rodchenkov G. Detection of JWH-018 metabolites in smoking mixture post-administration urine. Forensic Sci Int. 2010;200:141–147. doi: 10.1016/j.forsciint.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 25.Herbal Smoke Blend. Featuring the Extreme Herbal Smoke Blends and Legal Buds. Website. 2012 http://www.herbalsmokeblend.com/index.html. Accessed July 14. [Google Scholar]
- 26.National Center for Biotechnology Information PubChem Compound. CID=16078, 10382701, 107778, 125835. 2012 http://www.ncbi.nlm.nih.gov/pccompound?term=16078%2C%2010382701%2C%20107778%2C%20125835%20%5Buid%5D. Accessed July 23. [Google Scholar]