Abstract
Objective
To compare FP and GP performance of office-based procedures between urban and rural practices.
Design
Descriptive cohort study using health administrative data.
Setting
Ontario.
Participants
All FPs and GPs who billed the Ontario Health Insurance Plan for at least 1 office-based procedure between January 1 and December 31, 2006 (N = 8648).
Main outcome measures
Ontario Health Insurance Plan billings for office-based procedures were adjusted by full-time equivalent (FTE) so that the means are for 1 FTE. Office-based procedures were grouped into 1) surgical procedures, 2) injections and immunizations, 3) electrocardiograms (ECGs), and 4) venipunctures and laboratory tests. The analyses were stratified for FP and GP age, sex, rurality of practice, and participation in a primary care model.
Results
There were no substantial differences between FPs and GPs in rural practices compared with those in more urban practices with respect to surgical procedures. Rural FPs and GPs had lower mean numbers of injections and immunizations, ECGs, and venipunctures and laboratory tests than FPs and GPs practising in urban areas. Family physicians and GPs in primary care models had a lower mean number of surgical procedures but a higher adjusted mean number of injections and immunizations, ECGs, and venipunctures and laboratory tests.
Conclusion
For those procedures that are not dependent on specialist backup or access to more advanced technology, there were no substantial differences between rural and urban FPs and GPs. All comprehensive FPs and GPs should be able to provide these services to their patients. Training programs for all family medicine residents should ensure future FPs and GPs are able to perform these procedures.
Résumé
Objectif
Comparer les interventions qu’effectuent les médecins de famille (MF) et les omnipraticiens (OP) dans les cliniques urbaines par rapport aux rurales.
Type d’étude
Étude de cohorte descriptive à l’aide de données administratives.
Contexte
L’Ontario.
Participants
Tous les MF et les OP qui ont facturé au moins une intervention effectuée au bureau à l’assurance-santé de l’Ontario entre le premier janvier et le 31 décembre 2006 (N = 8648).
Principaux paramètres à l’étude
Toutes les facturations pour des interventions effectuées au bureau ont été ajustées en termes d’équivalent plein temps (ÉPT) de sorte que les moyennes correspondent à 1 ÉPT. Les interventions au bureau ont été regroupées en 1) interventions chirurgicales, 2) injections et vaccinations, 3) électrocardiogrammes (ECG) et 4) ponctions veineuses et examens de laboratoire. Pour les MF comme pour les OP, les analyses ont été stratifiées en fonction de l’âge, du sexe, de la nature rurale de la clinique et de la participation à un modèle de soins primaires.
Résultats
Pour les interventions chirurgicales, il n’y avait pas de différence importante entre les MF et les OP pratiquant en milieu rural et ceux exerçant plutôt en milieu urbain. Par rapport à ceux pratiquant en milieu urbain, les MF et les OP ruraux avaient un nombre moyen plus faible d’injections et de vaccinations, d’ECG ainsi que de ponctions veineuses et d’examens de laboratoire. Les MF et les OP des cliniques de soins primaires avaient un nombre moyen plus faible d’interventions chirurgicales, mais un nombre moyen ajusté plus élevé d’injections et de vaccinations, d’ECG ainsi que de ponctions veineuses et d’examens de laboratoire.
Conclusion
Pour les interventions qui n’exigent pas le soutien d’un spécialiste ni l’accès à une technologie plus complexe, il n’y avait pas de différence importante entre les MF et les OP ruraux et urbains. Dans l’ensemble, les MF et les OP devraient tous être capables de prodiguer ces services à leurs patients. Les programmes de formation en médecine familiale devraient s’assurer que tous les futurs MF et OP soient capables d’effectuer ces interventions.
Rural and urban practice pattern differences among FPs and GPs are influenced by a number of factors including the availability of health care support and technology, which includes other specialists, advanced radiologic testing, rehabilitation services, and home care services. In Canada, previous work has demonstrated differences in out-of-office care provided by urban and rural physicians, with rural FPs and GPs providing more obstetric, emergency department, and home care.1–3 In addition, rural FPs and GPs perform more advanced procedures such as endoscopies, surgical assistance, and anesthesia.2
An important component of family medicine is comprehensive care. While varying patient populations might influence the comprehensiveness of an individual physician’s practice, some office-based procedures, such as joint injections, small procedures, and immunizations, represent standard components of comprehensive care. These procedures are not as dependent on outside medical support and therefore should not be as influenced by the challenges of remote geographic access.
Patient expectation can also influence who performs an office procedure. In larger urban centres, where there is a greater availability of specialists such as dermatologists and plastic surgeons, some patients might prefer to have an office procedure performed by other specialists rather than their own FPs and GPs. Additionally, FPs and GPs might have their own comfort levels with respect to performing minor procedures, and some urban FPs and GPs might prefer to refer their patients.4
Therefore, the objective of this study was to compare the use of office-based procedures between urban and rural FPs and GPs practising in Ontario in 2006.
METHODS
Study design
This is a descriptive study using health administrative data from all FPs and GPs in Ontario who had at least 1 claim for an office-based procedure in 2006.
Data sources
The Institute for Clinical Evaluative Sciences (ICES) Physician Database is constructed using data from the Ontario Physician Human Resource Data Centre file of physicians in active practice in Ontario, the Ontario Health Insurance Plan (OHIP) Corporate Provider Database, and the OHIP file of physician billings. The ICES Physician Database includes information on physician demographic characteristics, medical training, and practice characteristics. It is completely anonymized, with all individual identifiers either removed or encrypted. It includes records for all physicians in practice in Ontario for the years 1992 to 2007.
The OHIP data include information on all physician claims for visits, procedures, and investigations. Ontario Health Insurance Plan billings were used to link patients with physicians. The Registered Persons Database provided information on patients’ age, sex, and geographic location. The Client Agency Program Enrolment (CAPE) database of patient enrolments with primary care groups and the OHIP Corporate Provider Database were used to identify physician group affiliations. Primary care reform became active in Ontario starting in 2003. The CAPE database identifies patients belonging to the newer primary care models of family health groups, family health networks, family health organizations, and family health teams. Patients attending community health centres (CHCs) are not included in the CAPE database.
Variable definitions
Rurality was defined using the Ontario Ministry of Health and Long-Term Care and Ontario Medical Association Rurality Index of Ontario (RIO) score. The RIO score is based on 10 community characteristics including travel time to different levels of care; community population characteristics; the presence of providers, hospitals, and ambulance services; social indicators; and weather conditions.5 Possible RIO scores range from 0 to 100, with 0 indicating the most urban practice and 100 the most rural practice. The Ontario Ministry of Health and Long-Term Care and the Ontario Medical Association use the RIO score as an eligibility criterion for program incentives that depend on a community’s degree of rurality. For example, some premiums are provided to FPs practising in rural communities with RIO scores greater than or equal to 45. For this reason we defined a rural area as having a RIO score greater than or equal to 45. To be consistent with other analyses that used the RIO score2 we further divided Ontario communities into major urban areas (RIO score 0 to 9) and nonmajor urban areas (RIO score 10 to 44).
The primary care groups include family health networks, family health groups, family health organizations, and family health teams. Not included are FPs and GPs practising in CHCs. Family physician and GP subspecialties were based on algorithms using OHIP billings and subdivided FP and GP care to include emergency department care, anesthesia, obstetrics, psychotherapy, palliative care and pain management, and sports medicine.1
Study population
The study population included all FPs and GPs in Ontario who had at least 1 OHIP billing for an office-based procedure from January 1 to December 31, 2006. Workload was measured using full-time equivalents (FTEs). The ICES FTE measure is based on the OHIP billings of physicians with the fee-for-service billings and adjusted shadow-billings acting as a proxy measure of services rendered. Full-time equivalent was based on the overall distribution of billings; all physicians whose total adjusted billings fell between the 40th and 60th percentiles are said to be working 1 FTE.
Office procedures
A list of the office procedures included in this study based on defining core procedures for family medicine residents is provided in Box 1.6 Office procedures were based on OHIP claims made by FPs and GPs in Ontario from January 1 to December 31, 2006. These office procedures were grouped in 4 categories: 1) surgical procedures, 2) injections and immunizations, 3) electrocardiograms (ECGs), and 4) venipunctures and laboratory tests. All the procedure totals were adjusted by FTE so that the means are for 1 FTE.
Box 1. Office-based procedures.
|
Data from Wetmore et al.6
Analysis
All analyses were stratified by FP and GP age, sex, rurality of practice, participation in a primary care model, and subspecialties. A univariate analysis of the procedure rates was done for each group according to physician subgroup (age, sex, participation in a primary care model). A bivariate analysis of procedure rates was done for each procedure group according to physician sex, age, and whether they were in a primary care model and by separating out rurality. Comparisons were tested for statistical significance using a 2-sided t test (with P < .05) and by calculating 95% CIs using SAS software, version 9.1.
This study received ethics approval from the Research Ethics Board at Sunnybrook Health Sciences Centre in Toronto, Ont.
RESULTS
There were 8648 FPs and GPs who made OHIP claims for at least 1 office-based procedure in 2006 (Table 1). Of these, 72.1% were from major urban centres, 19.6% were from nonmajor urban centres, and 8.3% were from rural areas. A higher proportion of male FPs and GPs and younger FPs and GPs were in rural practices. A lower proportion of FPs and GPs practising in major urban centres were in primary care models. All these differences were statistically significant (P < .05).
Table 1.
Study population characteristics
| CHARACTERISTIC | MAJOR URBAN, N (%) | NONMAJOR URBAN, N (%) | RURAL, N (%) | TOTAL, N |
|---|---|---|---|---|
| Overall cohort | 6231 (72.1) | 1698 (19.6) | 719 (8.3) | 8648 |
| Sex | ||||
| • Female | 2171 (34.8) | 544 (32.0) | 221 (30.7) | 2936 |
| • Male | 4060 (65.2) | 1154 (68.0) | 498 (69.3)* | 5712 |
| Age group, y | ||||
| • < 40 | 1379 (22.1) | 407 (24.0) | 201 (28.0)* | 1987 |
| • 40–49 | 1964 (31.5) | 576 (34.0) | 219 (30.5) | 2759 |
| • 50–59 | 1755 (28.2) | 466 (27.4) | 189 (26.3) | 2410 |
| •≥60 | 1133 (18.2) | 249 (14.6) | 110 (15.3)* | 1492 |
| Primary care model | ||||
| • Yes | 4041 (64.9) | 1217 (71.7) | 505 (70.3)* | 5763 |
| • No | 2190 (35.1) | 481 (28.3) | 214 (29.7) | 2885 |
| Subspecialties | ||||
| • FP emergency medicine | 467 (7.5) | 184 (10.8) | 94 (13.1)* | 745 |
| • FP obstetrics | 650 (10.4) | 192 (11.3) | 93 (12.9) | 935 |
| • FP anesthesia | S | S | S | 71 |
| • FP psychotherapy | 445 (7.1)* | 105 (6.2) | 38 (5.3) | 588 |
| • Palliative care and pain management | 350 (5.6) | 122 (7.2) | 50 (6.9) | 522 |
| • Sports medicine | 480 (7.7)* | 143 (8.4) | 34 (4.7) | 657 |
| • None | 3815 (61.2)* | 915 (53.9) | 400 (55.6) | 5130 |
S—suppressed due to low cell count.
Statistically different at P < .05.
A significantly higher proportion of FPs and GPs in rural practice provided emergency medicine (P < .05). A significantly higher proportion of the FPs and GPs in major urban centres had subspecialties in sport medicine or psychotherapy (P < .05). There were no differences among practice locations for FPs and GPs with subspecialties in palliative care and pain management, or anesthesia. Family physicians and GPs in major urban centres were more likely not to have subspecialties than FPs and GPs practising in nonmajor urban and rural locations.
Univariate analyses
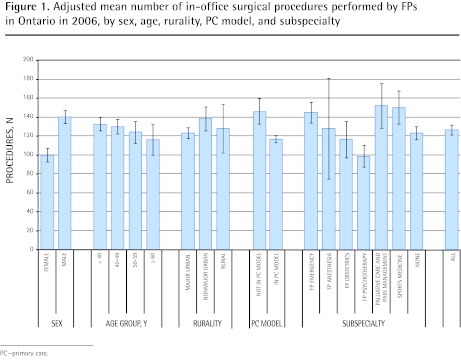
For office-based surgical procedures (Figure 1), there were no differences between FP and GP age and geographic location. Male FPs and GPs and those not in primary care models performed a higher mean number of surgical procedures (P < .05). Family physicians and GPs with a psychotherapy subspecialty had a significantly lower adjusted mean number of surgical procedures than FPs and GPs with emergency medicine, palliative care and pain management, or sports medicine subspecialties, or with no subspecialty (P < .05).
Figure 1.
Adjusted mean number of in-office surgical procedures performed by FPs in Ontario in 2006, by sex, age, rurality, PC model, and subspecialty
PC—primary care.
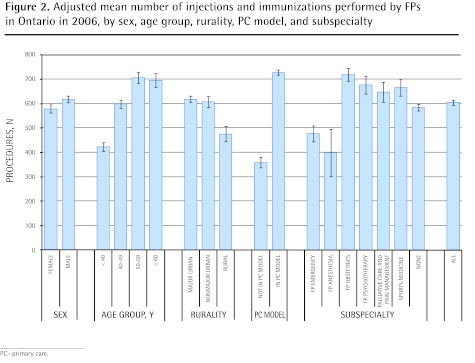
For injections and immunizations (Figure 2), the mean number increased with increasing age. Family physicians and GPs in primary care models had a significantly higher mean number of injections and immunizations, as did FPs and GPs with subspecialties in obstetrics, psychotherapy, or sports medicine (P < .05).
Figure 2.
Adjusted mean number of injections and immunizations performed by FPs in Ontario in 2006, by sex, age group, rurality, PC model, and subspecialty
PC—primary care.
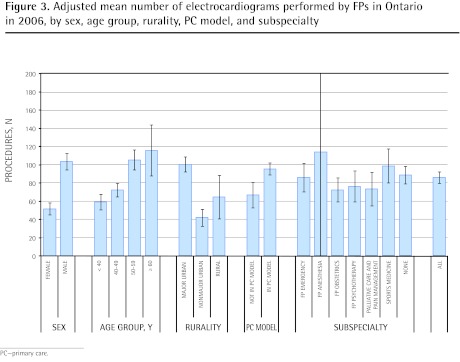
Office-based ECG use (Figure 3) was higher among male FPs and GPs, FPs and GPs older than 50 years of age, FPs and GPs practising in primary care models, and FPs and GPs practising in major urban centres. There were no significant differences in the adjusted mean number of ECGs among FP and GP subspecialties.
Figure 3.
Adjusted mean number of electrocardiograms performed by FPs in Ontario in 2006, by sex, age group, rurality, PC model, and subspecialty
PC—primary care.
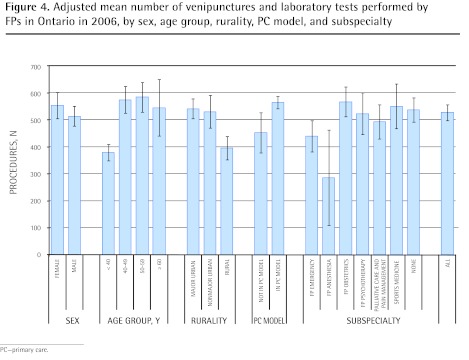
For venipuncture and laboratory tests (Figure 4), the adjusted mean number of procedures was lower among FPs and GPs younger than 40 years of age, rural-based FPs and GPs, and FPs and GPs not in primary care models (P < .05). There were no differences between men and women and little difference between FP and GP subspecialties.
Figure 4.
Adjusted mean number of venipunctures and laboratory tests performed by FPs in Ontario in 2006, by sex, age group, rurality, PC model, and subspecialty
PC—primary care.
Bivariate analyses
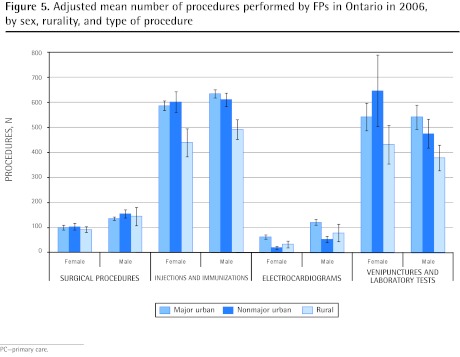
As shown in Figure 5, male FPs and GPs compared with female FPs and GPs in all geographic areas of Ontario had higher adjusted mean numbers of office-based surgical procedures. Male FPs and GPs compared with female FPs and GPs in major urban and nonmajor urban areas had higher adjusted mean numbers of ECGs, and male FPs and GPs in major urban centres had higher mean numbers of injections and immunizations than female FPs and GPs practising in rural centres. No differences between sexes were seen according to geography for venipunctures and laboratory tests.
Figure 5.
Adjusted mean number of procedures performed by FPs in Ontario in 2006, by sex, rurality, and type of procedure
PC—primary care.
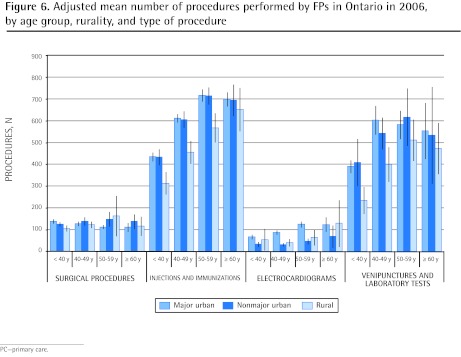
As shown in Figure 6, FPs and GPs younger than 40 years of age in major urban centres had a higher adjusted mean number of surgical procedures and, in addition to FPs and GPs in nonmajor urban centres, had higher immunization and injection rates, and venipuncture and laboratory test rates than those practising in rural areas. For FPs and GPs between 40 and 59 years of age, there was a higher mean number of ECGs performed in major urban centres compared with FPs and GPs practising in nonmajor urban and rural areas.
Figure 6.
Adjusted mean number of procedures performed by FPs in Ontario in 2006, by age group, rurality, and type of procedure
PC—primary care.
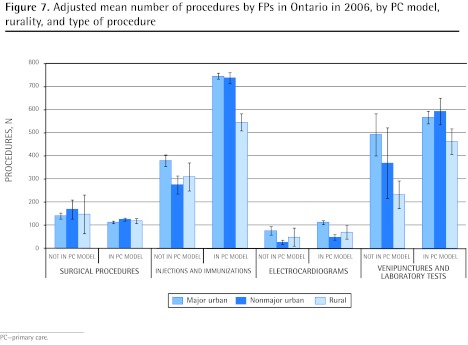
As shown in Figure 7, FPs and GPs not practising in primary care models in major urban centres compared with those practising in primary care models had a higher adjusted mean number of surgical procedures. Those FPs and GPs in primary care models in all geographic regions had a higher adjusted mean number of injections and immunizations. Family physicians and GPs in primary care models in major urban centres had a higher adjusted mean number of ECGs, and FPs and GPs in rural primary care models had a higher adjusted mean number of venipunctures and laboratory tests than FPs and GPs not affiliated with primary care models.
Figure 7.
Adjusted mean number of procedures by FPs in Ontario in 2006, by PC model, rurality, and type of procedure
PC—primary care.
DISCUSSION
The FPs and GPs in this study had similar characteristics to FPs and GPs described in other reports, with a lower proportion of female FPs and GPs and younger FPs and GPs practising in rural regions.1,2 There are known differences between rural and urban FPs and GPs with respect to their out-of-office scope of care.1 In this study, rural FPs and GPs were more involved with emergency medicine than FPs and GPs in major and nonmajor urban areas.
There were no substantial differences between FPs and GPs in rural practices compared with those in major and nonmajor urban practices with respect to surgical procedures. Rural FPs and GPs had lower rates of injections and immunizations, ECGs, and venipunctures and laboratory tests than FPs and GPs practising in major urban and nonmajor urban areas. One reason might be that these types of procedures are performed by other health care professionals such as nurses and nurse practitioners, and are therefore not billed by FPs and GPs. This might be more likely to occur in rural areas, where more medical care is provided by nurses and nurse practitioners. Also, public health units in rural areas might provide more immunization care than units in urban centres, thereby decreasing the number of immunizations performed by FPs and GPs.
Some of the differences seen between rural and urban FPs and GPs might actually be owing to the locations where patients are actually seen for procedures.7 For example, more rural FPs and GPs also work in emergency departments. These rural FPs and GPs might perform surgical procedures, laboratory testing, and ECGs more often in the emergency department, which means that examining the number of procedures done in the office setting might underestimate the total number of procedures.
In a similar study conducted in the United States, the overall number of outpatient procedures per 100 visits was higher among rural FPs than among urban FPs, but this was not statistically significant.8 They found that rural primary care physicians (including general internists) had higher overall outpatient procedure rates than their urban counterparts, but the procedural scope of practice showed more similarities than differences between rural and urban physicians.
Other studies have examined procedures performed by FP graduates. A survey of Canadian FP graduates did find a declining trend in the number of procedures done by graduates from metropolitan areas compared with rural regions, but this was not statistically significant.9 Another survey of FP graduates in Missouri found a cohort effect, with more recent FP graduates doing fewer procedures such as sigmoidoscopy, ultrasounds, vasectomy, endoscopy, and colposcopy.10 Colposcopy was performed more often in rural areas. Another US study found recent graduates were more likely to do office-based procedures that included colonoscopy and upper gastroesophageal endoscopy.11 However, the definitions of office-based procedures were different from the definitions used in this study.
In this study, FPs and GPs in primary care models had a lower adjusted mean number of surgical procedures, which was especially pronounced in major urban centres. Study FPs and GPs in primary care models had a higher adjusted mean number of injections and immunizations, ECGs, and venipunctures and laboratory tests. For rural areas, this might again be a reflection of the locations where minor surgical procedures are performed. In 1997, a US study examining the influence of payment models among FPs and GPs found that a fee-for-service model had a stronger economic incentive to perform procedures such as sigmoidoscopy and colposcopy compared with capitation models.12 However, more work needs to be done to compare procedure rates in Canadian models with respect to the influence of interdisciplinary care capitation and incentive payments.
Limitations
We are unable to capture billing data from CHC physicians, and encounter data from nurses and nurse practitioners. Community health centre physicians and nurse practitioners tend to work in underserviced areas, including rural areas, and with marginalized populations in urban areas. Currently, there are 73 CHCs in Ontario.13 We might also be underestimating work done by FPs and GPs who shadow-bill within certain primary care models. Also, some procedures are not fully funded by the government and might be underestimated. In this instance, patients might have to pay for these procedures. Whether this happens more or less in urban and rural areas is not clear. Finally, some FPs and GPs might practise in multiple locations (eg, locum physicians). Urban FPs and GPs might do locum work in rural areas and their practice patterns might be attributed to FPs and GPs who only work in rural areas.
Conclusion
For procedures that are not dependent on specialist backup or access to more advanced technology, there were no substantial differences between rural and urban FPs and GPs. All comprehensive FPs and GPs should be able to provide these services to their patients. Training programs for all family medicine residents should ensure future FPs are able to do these procedures.
Future work might include looking in more detail at the types of procedures provided by different primary care models as they mature in Ontario. Also, work that examines what facilitates or prevents FPs and GPs performing office-based procedures is necessary.
Acknowledgments
This work was a resident research project conducted by Dr Sood and supervised by Dr Jaakkimainen. It was presented at the Toronto East General Hospital family medicine resident research rounds in 2008.
EDITOR’S KEY POINTS
Differences between FP and GP rural and urban practice patterns are influenced by a number of factors, including the availability of health care support and technology. However, FPs and GPs offering comprehensive care should be able to provide their patients a range of office-based procedures.
Family physicians and GPs in primary care models had a higher adjusted mean number of injections and immunizations, electrocardiograms, and venipunctures and laboratory tests. These types of procedures are often performed by other health care professionals such as nurses and nurse practitioners, and are therefore not billed by FPs and GPs. This might be more likely to occur in rural areas. Also, public health units in rural areas might provide more immunization care than units in urban centres, thereby decreasing the number of immunizations performed by FPs and GPs.
For procedures that are not dependent on other specialists or access to more advanced technology, there were no substantial differences between rural and urban FPs and GPs.
POINTS DE REPÈRE DU RÉDACTEUR
Les différences entre les modes de pratique des MF et des OP ruraux et urbains sont influencées par divers facteurs comme le fait de disposer de certaines technologies et d’un soutien pour prodiguer les soins. Toutefois, les MF et les OP qui fournissent des soins complets devraient être capables d’effectuer un certain nombre d’interventions au bureau.
Les MF et les OP des cliniques de soins primaires avaient un nombre moyen ajusté plus élevé d’injections, de vaccinations, d’électrocardiogrammes et de ponctions veineuses et d’examens de laboratoire. Les interventions de ce type sont souvent effectuées par d’autres professionnels de la santé comme les infirmières ou les infirmières praticiennes, si bien qu’elles ne sont pas facturées par les MF et les OP. Cela risque davantage de se produire en milieu rural. De plus, les unités de santé publique des régions rurales effectuent probablement plus de vaccinations que celles des centres urbains, ce qui diminue le nombre de vaccinations effectués par les MF et les OP.
Pour ce qui est des interventions qui ne relèvent pas d’autres spécialistes ou de la disponibilité d’une technologie avancée, il n’y avait pas de différence appréciable entre les MF et les OP ruraux et urbains.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
All authors were involved in the conception and design of the study. Ms Schultz was primarily responsible for the data analysis. Dr Jaakkimainen prepared the first draft of the article. Dr Sood and Ms Schultz contributed to subsequent revisions. All of the authors reviewed the article and approved the final version.
Competing interests
None declared
References
- 1.Chan BT, Schultz SE. Supply and utilization of general practitioner and family physician services in Ontario. ICES investigative report. Toronto, ON: Institute for Clinical Evaluative Sciences; 2005. Available from: www.ices.on.ca/file/fp-gp_aug08_final.pdf. Accessed 2012 Sep 12. [Google Scholar]
- 2.Tepper JD, Schultz SE, Rothwell DM, Chan BT. Physician services in rural and northern Ontario. ICES investigative report. Toronto, ON: Institute for Clinical Evaluative Sciences; 2006. Available from: www.ices.on.ca/file/Physician_Services_in_Rural_and_Northern_Ontario.pdf. Accessed 2012 Sep 12. [Google Scholar]
- 3.Glazier RH, Zagorski BM, Rayner J. Comparison of primary care models in Ontario by demographics, case mix and emergency department use, 2008/09 to 2009/10. ICES investigative report. Toronto, ON: Institute for Clinical Evaluative Sciences; 2012. Available from: www.ices.on.ca/file/ICES_Primary%20Care%20Models%20English.pdf. Accessed 2012 Sep 27. [Google Scholar]
- 4.Rivet C, Ryan B, Stewart M. Hands on: is there an association between doing procedures and job satisfaction? Can Fam Physician. 2007;53:92–3. e.1–5. Available from: www.cfp.ca/content/53/1/92.full.pdf+html. Accessed 2012 Sep 12. [PMC free article] [PubMed] [Google Scholar]
- 5.Kralj B. Measuring “rurality” for purposes of health-care planning: an empirical measure for Ontario. Ont Med Rev. 2000;(10):33–52. [Google Scholar]
- 6.Wetmore SJ, Rivet S, Tepper J, Tatemichi S, Donoff M, Rainsberry P. Defining core procedure skills for Canadian family medicine training. Can Fam Physician. 2005;51:1364-5.e1–6. Available from: www.cfp.ca/content/51/10/1364.full.pdf+html. Accessed 2012 Sep 20. [PMC free article] [PubMed] [Google Scholar]
- 7.Wetmore SJ, Agbayani R, Bass MJ. Procedures in ambulatory care. Which family physicians do what in southwestern Ontario? Can Fam Physician. 1998;44:521–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Baldwin LM, Rosenblatt RA, Schneeweiss R, Lishner DM, Hart LG. Rural and urban physicians: does the content of their medicare practices differ? J Rural Health. 1999;15(2):240–51. doi: 10.1111/j.1748-0361.1999.tb00745.x. [DOI] [PubMed] [Google Scholar]
- 9.Chaytors RG, Szafran O, Crutcher RA. Rural-urban and gender differences in procedures performed by family medicine residency graduates. Fam Med. 2001;33(10):766–71. [PubMed] [Google Scholar]
- 10.Ringdahl E, Delzell JE, Jr, Kruse RL. Changing practice patterns of family medicine graduates: a comparison of alumni surveys from 1998 to 2004. J Am Board Fam Med. 2006;19(4):404–12. doi: 10.3122/jabfm.19.4.404. [DOI] [PubMed] [Google Scholar]
- 11.Young RA, Byrd AN. Practice patterns of rural Texas physicians trained in a full-service family practice residency program. Tex Med. 1995;(2):64–8. [PubMed] [Google Scholar]
- 12.Leider PJ, Solberg R, Nesbitt T. Family physician perception of economic incentives for the provision of office procedures. Fam Med. 1997;29(5):318–20. [PubMed] [Google Scholar]
- 13.Association of Ontario Health Centres [website] About us. Toronto, ON: Association of Ontario Health Centres; 2011. Available from: www.ontariochc.ca/index.php?ci_id=2341&la_id=1. Accessed 2011 Jun 1. [Google Scholar]