Abstract
Background
Saving bone by resurfacing the femoral head is not a new concept and the appeal for this type of hip replacement has remained despite the difficulties to find a bearing material suitable for this procedure.
Purpose
In this article, the unique experience of a surgeon who has been performing hip resurfacing since its early development is presented, along with a comparative analysis of the performance of successive designs.
Results
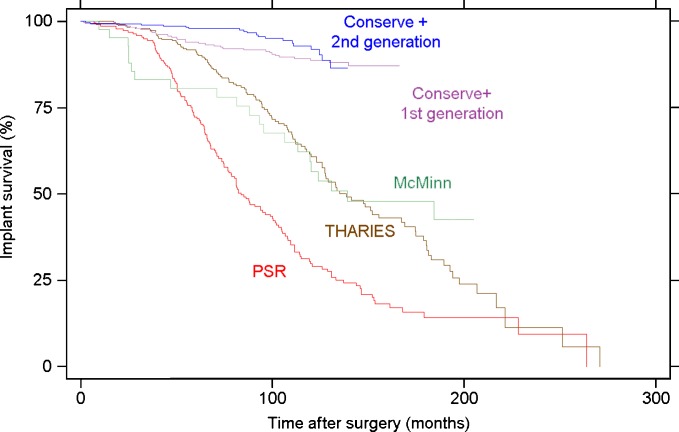
The overall 10-year Kaplan–Meier survivorship of the early designs with polyethylene bearings did not exceed 62% while that of the current Conserve®Plus metal-on-metal hybrid design implanted with second generation surgical technique is in excess of 92%. Further exceptional, in the 10-year survivorship, 99.7% has been achieved with femoral size of 46 mm and good bone quality. Cementless acetabular components provide better enduring fixation than cemented designs.
Discussion
Metal-on-metal is currently and fortunately the only highly successful bearing material that can combine low wear rates and the manufacturing of a thin acetabular component to preserve bone and still accommodate the large femoral head of a hip resurfacing. The adverse local tissue reactions (ALTR) associated with metal-on-metal devices are not a bearing material issue per se but one of the device design and surgical technique. Almost all of ALTR and the rare events of systemic toxicity are due to abnormal wear patterns which can be prevented by proper acetabular component design and precise socket orientation in both the coronal and sagittal planes. Further improvements of the long-term durability with hip resurfacing can be anticipated with the use of recently developed trabecular bone-like tantalum or titanium porous coatings and with proper training of the surgeons interested in performing hip resurfacing arthroplasty.
Keywords: hip resurfacing, long term, survivorship, history
Introduction
Today, younger and more active patients seek hip replacement in an attempt to restore a lifestyle lost to the debilitating effect of hip arthritis. With this change in patient population, the likelihood of revision and replacement surgery increases even though the advent of better performing devices has enhanced the durability and reduced the complication rates of total hip replacement (THR). The need to develop a more conservative hip replacement procedure, improve component fixation and bearing couple performance and to design physiologic components with biocompatible materials stimulated our interest 40 years ago in the development of surface arthroplasty. By being less invasive, a revision from resurfacing when necessary could be carried out more simply with potentially improved results. The origin of hip resurfacing is generally attributed to Smith-Petersen and his interposition cup [42]. The early history of hip resurfacing has been well chronicled in peer-reviewed literature [2, 3, 10] and various book chapters [4, 6]. The senior author's experience with resurfacing is unique as it started in 1975, with an all cemented double cup arthroplasty design and continued through the entire evolution of the concept. The purposes of this article were to evaluate the progresses made overtime, provide an overview of the lessons learned from each consecutive design after long-term follow-up, and describe the current status of hip resurfacing arthroplasty.
Prosthetic Designs and Patient Demographics
Our experience started with the total hip articular replacement using internal eccentric shells (THARIES), which was developed at the University of California-Los Angeles (UCLA) Medical Center by Amstutz and Clarke and became available in 1975 [9]. The femoral component was made of CoCr with a chamfered cylinder internal shape and articulated with an all-polyethylene acetabular component. Both components were cemented. Three hundred thirty-three THARIES were implanted in 301 patients with a mean age of 52.3 years (range 14 to 80 years), between 1975 and 1984 by the senior author (Table 1). All surgeries were performed using a transtrochanteric approach.
Table 1.
Demographics of the patient cohorts
| MMRA design | THARIES | PSR | MCMINN | Conserve Plus 1st generation | Conserve Plus 2nd generation |
|---|---|---|---|---|---|
| Years of implantation | 1975 to 1984 | 1983 to 1992 | 1993 to 1996 | 1996 to 2000 | 2000 to 2004 |
| Number of hips (patients) | 333 (301) | 222 (197) | 42 (39) | 300 (263) | 370 (324) |
| Male/Female (%) | 55/45 | 63/37 | 57/43 | 75/25 | 70/30 |
| Age (years) | 52.3 (14 to 80) | 51.0 (15 to 79) | 47.5 (22 to 69) | 48.4 (15 to 71) | 49.6 (14 to 78) |
| Weight (kg) | 75 (36 to 200) | 77.5 (43 to 123) | 82.2 (39 to 118) | 85.4 (49 to 164) | 82.4 (42 to 135) |
| Etiology (%) | |||||
| OA | 53 | 53 | 55 | 67 | 66 |
| ON | 15 | 16 | 17 | 9 | 6 |
| DDH | 10 | 13 | 10 | 10 | 11 |
| Rheumatoid | 6 | 4 | 5 | 3 | 2 |
| Trauma | 5 | 7 | 0 | 7 | 8 |
| Other | 11 | 7 | 13 | 4 | 7 |
In the early 1980s, the development of cementless fixation for resurfacing devices derived from the belief that cement was the main cause of implant failure. The porous surface replacement (PSR) succeeded to the THARIES and featured a three-part prosthetic design. A porous-coated metallic acetabular shell received a ultra-high-molecular-weight polyethylene (UHMWPE) insert articulating with a CoCr porous-coated femoral component. Two versions of the PSR were used in our series: one using a chamfered cylinder-shaped acetabular shell and a titanium mesh for bone fixation (PSR, Zimmer, Warsaw, IN) and the other using a low profile hemispherical acetabular component and sintered CoCr beads for bone fixation (PSR, Depuy, Warsaw, IN). On the femoral side, a gentle 3° taper was introduced in 1990 to facilitate seating without tilting. A total of 222 hips (197 patients) were implanted with these designs by the senior author starting in 1983. The patients' mean age at surgery was 51.0 (range, 15 to 79). The surgeries were also performed through a transtrochanteric approach.
By 1992, the role of polyethylene wear debris in the formation of periprosthetic osteolysis and implant aseptic failure had been established and both THR and hip resurfacing benefited from the development of alternate bearing materials to UHMWPE. However, one of the main criticisms directed toward resurfacing was that the procedure did not conserve bone on the acetabular side compared with a conventional THA because of the need to accommodate for a femoral head of a larger diameter.
Metal-on-metal became the material of choice for hip resurfacing. From 1993 to 1996, a pilot study of 42 hips (39 patients) was initiated at our institution using the McMinn design. All femoral components were cemented while 19 hips received a cemented acetabular component and 23 hips were reconstructed with cementless acetabular fixation. The mean patient age was 47.5 years (range, 22 to 69). Thirteen procedures were performed through a transtrochanteric approach while the remaining 29 were done with a posterior approach. The senior author also used the all cementless M/M resurfacing developed in the early 1990s by Heinz Wagner [30] but this system had a very complicated insertion technique including hemispherical reaming for the femoral component and was only satisfactory for patients with ideal bone quality. Only four were implanted. Two survive at 18 years but the numbers are too small to allow any valid comparison with the other larger series.
The first Conserve®Plus (Wright Medical Technology, Arlington, TN) was implanted in November of 1996. The components were made of CoCr and the design was hybrid (i.e., porous fixation with sintered beads on the acetabular side and cemented on the femoral side). Progressive modifications to the bone preparation and cementing technique of the femoral component were made throughout the first 300 hips implanted in 263 patients [5]. The mean patient age was 48.4 years (range, 15 to 71). This series of surgeries is referred to as the first generation. The procedures were performed using a posterior approach [1] except in three hips for which a transtrochanteric approach was used.
The second generation of Conserve®Plus featured the use of dome and trochanteric suction during cementing, an increased number of fixation holes in the dome and chamfered areas of the femoral head, and a careful removal of all cystic material using a high speed burr. Three hundred and seventy hips (324 patients) were implanted using this technique from March 2000 until April 2004. The mean patient age was 49.6 years (range, 14 to 78). All surgeries were performed through a posterior approach.
Results
Using the time to revision surgery for any reason as end point, substantial differences in survivorship were observed between the five consecutive series of hip resurfacing (Fig. 1). These differences were significant (log rank test p = 0.0000) (Table 2). The modes of failure of the various prostheses evolved over time, illustrating the effects of design and surgical technique modifications (Table 3).
Fig. 1.
Kaplan–Meier survivorship of the five resurfacing designs used by the senior author since 1975. Although the follow-up time of the recent designs is limited, the improvement over time is substantial. For the Conserve®Plus design, the effects of the second generation surgical changes were essentially felt on hips with risk factors (femoral component size ≤46 mm and/or femoral head defects >1 cm) because the 10-year survivorship of hip without these risk factors has been 99.7%, even with the early surgical technique
Table 2.
Survivorship results of the five series of resurfacing
| 5 year survival | 95% CI | 10 year survival | 95% CI | 15 year survival | 95% CI | |
|---|---|---|---|---|---|---|
| THARIES | 91.7% | 87.8 to 94.4% | 61.5% | 54.1 to 68.1% | 36.5% | 27.7 to 45.2% |
| PSR | 72.2% | 65.6 to 77.8% | 30.5% | 23.8 to 37.4% | 14.2% | 8.5 to 21.2% |
| MCMINN | 80.6% | 64.9 to 89.6% | 59.4% | 42.3 to 72.9% | 47.9% | 31.3 to 62.7% |
| Conserve Plus 1st generation | 94.0% | 90.5 to 96.2% | 89.2% | 84.8 to 92.4% | N/A | N/A |
| Conserve Plus 2nd generation | 97.9% | 95.6 to 99.0% | 92.9% | 88.3 to 95.7% | N/A | N/A |
Table 3.
Summary of the incidence of revision, presented by mode of failures and in association with each design
| Acetabular Loosening | Femoral Loosening | Femoral neck Fracture | Sepsis | Wear related or ALTR | Instability | Other | |
|---|---|---|---|---|---|---|---|
| THARIESa | 86 (25.8%) | 1 (0.3%) | 0 (0%) | N/A | 0 (0%) | 7 (2.1%) | |
| PSRa | 28 (12.6%) | 23 (12.4%) | 1 (0.5%) | N/A | 2 (0.9%) | 28 (12.6%) | |
| MCMINN | 16 (38.1%) | 3 (7.1%) | 1 (2.4%) | 1 (2.4%) | 1 (2.4%) | 0 (0%) | 0 (0%) |
| Conserve Plus 1st generation | 2 (0.7%) | 22 (7.3%) | 4 (1.3%) | 1 (0.3%) | 3 (1%) | 1 (0.3%) | 1 (0.3%) |
| Conserve Plus 2nd generation | 5 (1.4)% | 4 (1.1%) | 3 (0.8)% | 0 (0%) | 4 (1.1%) | 0 (0%) | 0 (0%) |
aThe information provided by the senior author's database did not allow to differentiate femoral from acetabular aseptic loosening. Also, the values indicated for THARIES and PSR designs are underestimated as information on the mode of failure was missing for a number of hips revised outside our institution
Discussion
The Metal-on-Polyethylene Era
The comparative survivorship results between designs clearly show areas of improvement over time as each series benefited from the knowledge derived from the previous experiences. These improvements can certainly be attributed not only to the evolution of the prosthetic designs but also to the modification of surgical technique as shown by the superior results of the Conserve Plus devices implanted with the second generation technique over those implanted with the first generation technique.
The primary mode of failure associated with the THARIES design was aseptic loosening of the acetabular component, with femoral or combined loosening next, but neck fractures were rare. The failure rates of the all cemented system were later explained by the effects of increased polyethylene wear debris generated by large femoral heads articulating with UHMWPE, sterilized in air. Acrylic fragmentation however, was initially thought to be the main cause contributing to osteolysis. The hips of males patients with OA had much higher survivorship at 10 years (76.4%; 95% CI, 62 to 86%) compared with the rest of the series (55.1%; 95% CI, 46 to 63%). This was explained by a greater area for fixation and usually better bone quality in this category of patients. The procedure was largely abandoned after reports of poorer results from other centers [22, 25, 33].
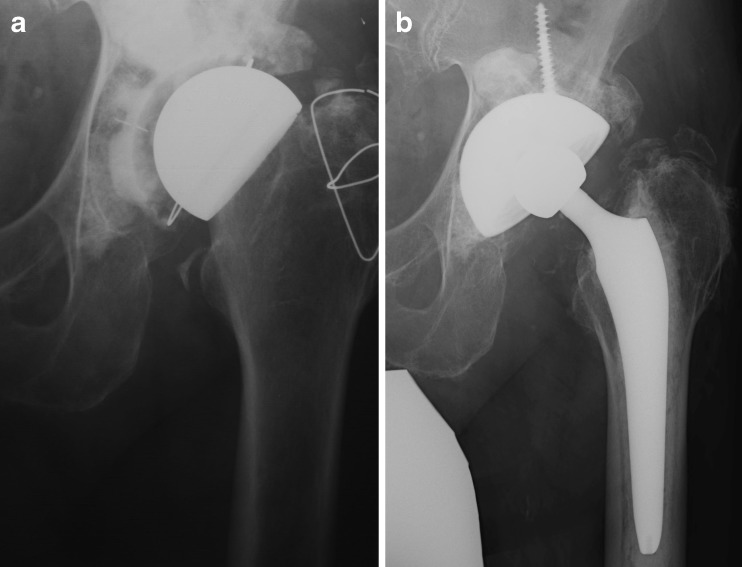
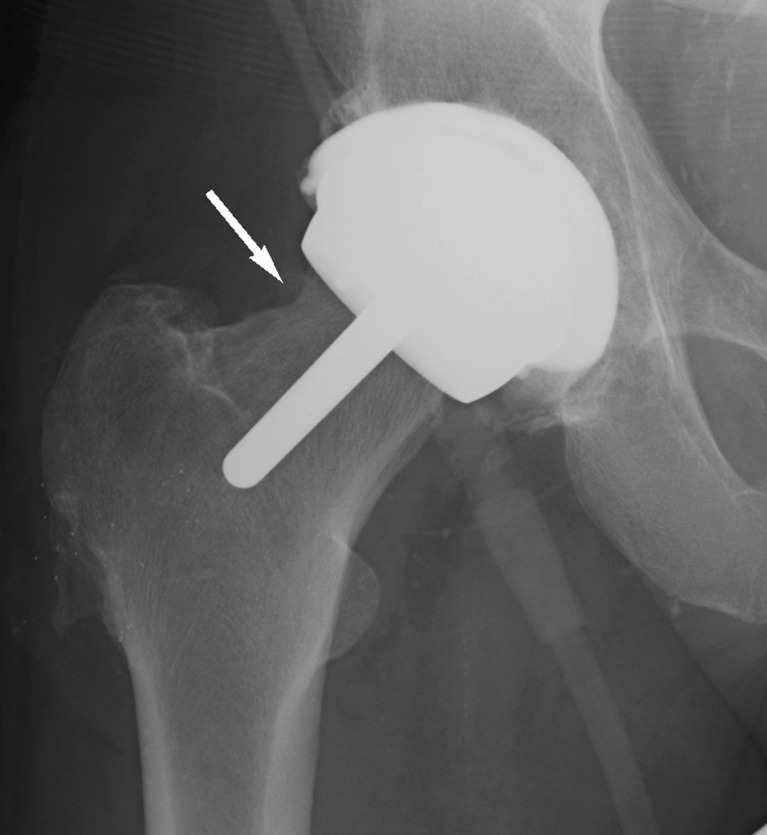
The cementless PSR design showed greatly improved initial femoral and socket fixation. The Zimmer CCD socket design with titanium mesh contained the migration of polyethylene (PE) debris to the acetabulum so that fixation remained intact but the primary mode of failure became femoral loosening or insufficiency fracture due to neck osteolysis through a path of least resistance of the particulate debris. However, a change from molded polyethylene to machined polyethylene may have been an additional factor decreasing the wear performance of the first generation polyethylene sterilized in air. The highly improved socket survival and the ability of revision requiring only a liner change was a substantial advantage [14]. The Depuy low profile socket with screw fixation facilitated the implantation but the debris for the first time in the cementless era entered into the surrounding acetabulum through the screw holes of the component. Although the acetabular durability improved considerably, the overall survivorship performance of these devices did not improve compared with the THARIES because of the high wear rate of femoral failure due to UHMWPE particulate debris-induced osteolysis. When revision became necessary, the patients still benefited from newer and more advanced implants which had become available, including cementless acetabular components for THARIES revisions (Fig. 2) and often just a liner exchange for the PSR devices. Cementless femoral stem-type components for revision of both systems became available in the 1980s. The stem-type device could then be implanted into a virgin femoral canal and excellent functional outcomes were generally achieved for these patients, most of whom were still young and active [14, 41]. Indeed, for patients with modest activity levels, some of those prostheses are still functioning 25 years after index surgery (Fig. 3).
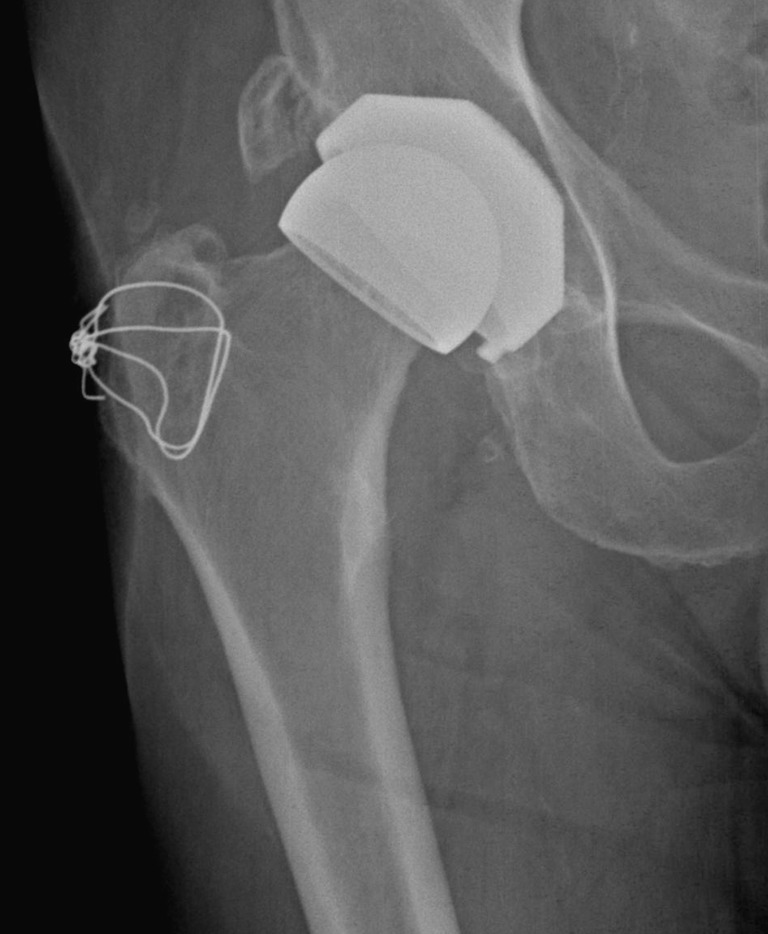
Fig. 2.
a Pre-revision radiograph of a THARIES resurfacing device taken 18 years after surgery. b The cemented design of the THARIES did not allow a bone-conserving revision on the acetabular side and required extensive reaming to secure a large cementless acetabular shell. The patient is doing well 12 years after conversion to THR
Fig. 3.
Antero-posterior radiograph of a PSR CCD design (Zimmer, Warsaw, IN) 20 years after implantation. Polyethylene wear is suggested by the asymmetric position of the femoral head with respect to the acetabular component. However, there are no osteolytic lesions visible and the component fixation is pristine. The patient UCLA activity score remained moderate throughout the follow-up period with a maximum value of 7. The reconstruction still has not been revised 25 years after surgery.
From these early resurfacing designs with PE bearings, several lessons can be drawn:
Hip resurfacing preserves femoral bone stock.
The increased stability due to the large ball size was associated with a markedly reduced prevalence of dislocation compared with THA
The procedure did not cause femoral head necrosis [16].
There were very few short-term neck fracture failures, but these appeared to be related to bone stock and technique.
Longer-term femoral neck fractures seen with the PSR design were explained by PE wear debris following the “path of least resistance” to the femoral neck and the technical difficulty to properly seat the femoral component (absence of centralizing system), leaving gaps and access to particulate debris between the neck and the component [8].
Although acrylic fragmentation was a factor in the cemented versions, the majority of the failures were due to component loosening secondary to polyethylene debris-induced osteolysis [7, 17, 24, 31].
Femoral fixation was critical due to a small fixation area, and larger diameter components showed better survivorship [30].
Revision to a conventional stem-type device for the femoral component was easy because the femoral canal was left intact by the resurfacing procedure.
Although socket loosening was dramatically reduced with cementless components, the device did not conserve acetabular bone stock because of the thickness of the two-component system (a metallic shell and a liner insert).
The Metal-on-Metal Hip Resurfacing Era
The combination of a need for a more bone-conserving acetabular component and low wear bearing material leads the development of hip resurfacing towards the use of metal-on-metal devices. Currently, only metallic devices can provide sufficient strength for a thin, one-piece shell that will accommodate a large femoral head without reaming the acetabulum beyond what would be needed for a conventional THA [44, 47].
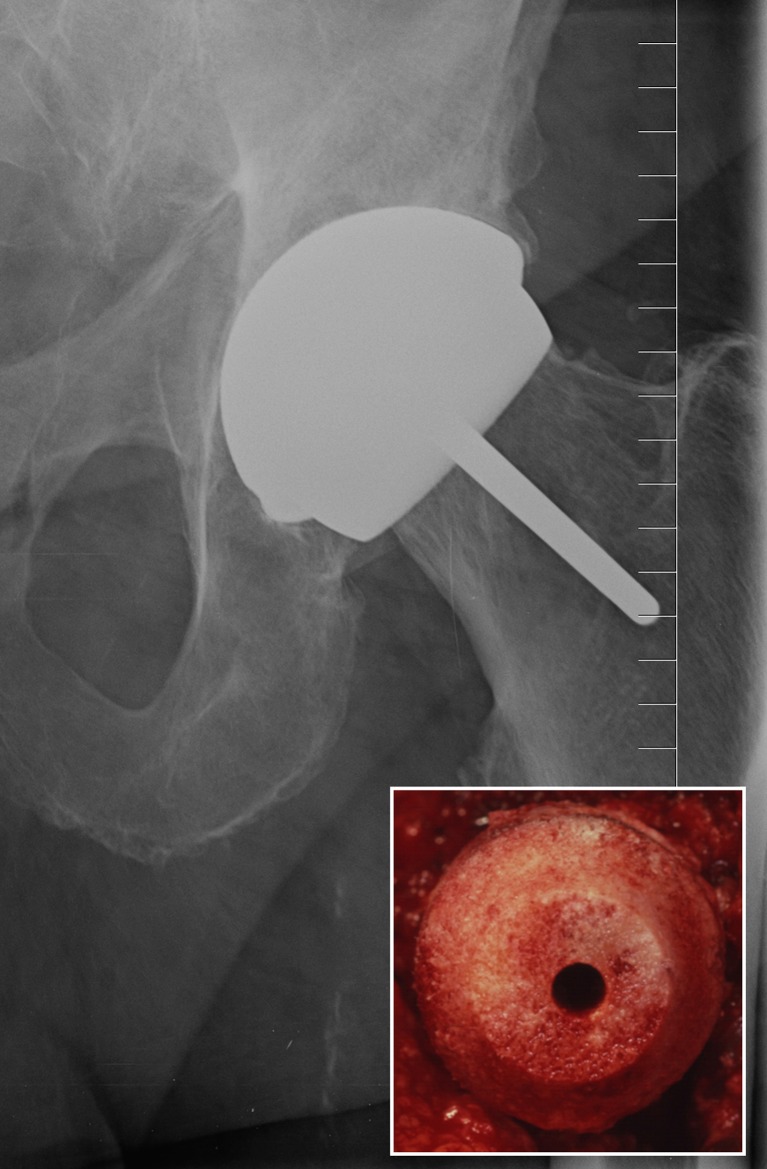
Our pilot study using the McMinn device clearly showed the superiority of a cementless fixation over a cemented fixation on the acetabular side [15] (Fig. 4). It also demonstrated the usefulness of a short metaphyseal stem to control the orientation of the femoral component as well as the potential for durability of hybrid designs using a chamfered cylinder-shaped femoral reaming (similar to that of the THARIES).
Fig. 4.
Fifteen-year radiographic follow-up of a McMinn resurfacing prosthesis with a “double socket” construct on the acetabular side. Fixation is secure. A small “divot sign” (arrow) on the lateral femoral neck indicates a possible repetitive impingement of the neck with the acetabular component [21]. The patient is asymptomatic
The comparative results between our first and second generation of Conserve + resurfacings show the efficacy of a series of technical changes made in the preparation of the femoral head (use of dome and trochanteric suction, increase in number of drilled holes, and use of burr in removal of bone defects) [5]. However, these improvements essentially had an effect on the durability of the device implanted in hips with risk factors because the survivorship results of hips with no femoral defect implanted with femoral components 48 mm or larger have been excellent from the beginning of the series (Fig. 5) and arguably the best ever of any joint replacement with a 10-year Kaplan–Meier survivorship of 99.7% (95% C.I., 98.1–99.9%) [11]. There have been only two revisions in 468 hips, one 13.1 months post-op (sepsis) and the other 11.6 years post-op (femoral loosening). Ten-year minimum results of hip resurfacing are few in the published literature, but Treacy et al. reported 98% survivorship in male patients operated with the Birmingham hip resurfacing (Smith and Nephew, Warwick, UK) [46].
Fig. 5.
Fourteen-year radiographic follow-up of a Conserve®Plus hip resurfacing. The patient was an “ideal” candidate for the procedure, with no femoral defects (insert) and treated with a large femoral component (52 mm)
What has perhaps been even more impressive has been the virtual elimination of neck fractures and femoral loosening despite continuing to resurface hips in young patients with serious cystic defects. This has been achieved by improving our technique of femoral head preparation and cementing in the metaphyseal stem. Although we anticipate further improvement in results with third generation techniques in these difficult cases, they are unlikely to match those of patients with good bone quality. However, older men and women with good bone quality are performing as well in the younger patients and still retain the benefits of resurfacing.
Adverse Local Tissue Reactions
While the results of hip resurfacing have dramatically improved, a new mode of failure has emerged and has become the main focus of patients and surgeons today [40]. In the past 3 years, the report of numerous adverse local tissue reactions (ALTR) has raised serious doubts in the orthopedic community over the benefits of metal-on-metal implants, in particular when used with stem-type devices. Failure rates as high as 48.8% at 6 years were reported for the articular surface replacement (ASR) Excel (a stem-type device with large femoral head manufactured by Depuy, Warsaw, IN) [27], even higher than those of the ASR hip resurfacing. Higher blood metal ion concentrations were also reported, probably associated with corrosion products from the stem and generated at the ball-stem-tapered interface [20]. Even though other large head metal-on-metal systems have performed better, THR with other bearing materials can now increase ball size sufficiently to minimize the risk of dislocation, except in very small hips.
The recall of poorly performing ASR devices has precipitated an unprecedented rash of unbalanced media articles questioning the rationale of the metal-on-metal bearing itself which, along with improved fixation, is the reason for the dramatic improvement of hip resurfacing results.
At the moment, there is a lack of understanding among surgeons, patients, and especially the media about the real cause of ALTR in resurfaced hips. The literature clearly shows that the primary cause of increased wear is insufficient coverage of the ball by the socket, coming from poorly positioned or poorly designed components or both [18]. The acetabular components with the largest femoral head coverage have been associated with lower production of metal ions and ALTR [28]. However, the failure of reports in the literature to include all the possible risk factors for increased wear (socket anteversion, abduction, and component size and design) as well as their synergistic influence has led the lay audience to draw simplistic conclusions about the problem and to an overall condemnation of the bearing material itself despite the fact that the vast majority of resurfacing devices other than the ASR and the withdrawn Durom (Zimmer, Warsaw, IN) are functioning well with up to 15 years of follow-up.
Often misunderstood, the hypersensitivity or allergic reactions to metal are a very rare occurrence and while cases have been reported with other devices, we have not identified a histologically proven case with the Conserve®Plus design in USA.
Systemic toxicity after metal-on-metal arthroplasty is rare and has been documented in only two reports of extremely rare cases of cobaltism in association with extremely high wear of ASR metal-on-metal THR devices [32, 45]. It must also be said that most cases of cobalt toxicity reported in association with hip arthroplasty were observed in conventional THR featuring bearing materials other than metal-on-metal [23, 36–38, 43].
The debate around metal-on-metal bearings has so far been about the wear properties of the material. However the problems associated with these new devices, unlike those observed in the resurfacing designs using polyethylene bearings, are not a bearing material issue per se, but one of the device design and surgical technique. Almost all of ALTR and the rare events of systemic toxicity are due to abnormal wear patterns which can be prevented by proper acetabular component design and precise socket orientation in both the coronal and sagittal planes. While the sensitivity of head coverage by the socket was initially underappreciated, improved understanding could lead to near elimination of ALTR which has plagued all evolutionary devices, THR as well as hip resurfacing.
Metal-on-metal hip resurfacing is not a new technology anymore and the devices that have been approved by the FDA after sufficient clinical trials have been available for well over a decade. It is important to avoid making statements about a procedure based on the poor results of subsequent designs which have been recalled or withdrawn while they were still in their experimental phase.
Conclusion
The need for a bone-conserving procedure to treat the young patient with end-stage osteoarthritis has been present since the inception of hip resurfacing and will remain or continue to grow. This is why hip resurfacing is a treatment option that is worth pursuing and improving. When comes the time for revision surgery, as should be expected for most young and active patients, whether treated with a resurfacing or a primary THR, the preserved bone stock with hip resurfacing provides more favorable conditions for a successful surgery and the technical difficulty of the conversion is comparable to that of a primary THR [12, 19, 39, 48]. This enables patients seeking to restore their previous lifestyle to be more active than with a THR, and numerous authors have reported high levels of physical activity in patients after hip resurfacing [13, 29, 34, 35].
Tremendous progress has been made in a relatively short time (less than 40 years) and this compares favorably with the progress accomplished with conventional THR in a much longer 70-year history. The current results of our Conserve®Plus hip resurfacing series are already exceeding our initial expectations. However several avenues can lead to future improvements of the concept. Progress in the precision of component placement can be achieved by using systems where the instrumentation provides the surgeon with the tools to implant the socket with a 42° ± 10° abduction angle and a 15° ± 10° anteversion angle. A case could certainly be made for the use of navigation systems which have shown efficacy in positioning accurately the acetabular component in conventional THA [26]. This could be particularly useful for surgeons who have difficulty in achieving satisfactory orientation.
The porous fixation of the acetabular components could also be improved by the use of porous tantalum or titanium material mimicking trabecular bone. FDA approval of such technology for resurfacing has not been granted yet. Improving the socket designs of already existing devices to provide larger femoral head coverage by the socket would give the surgeon more flexibility of implantation orientation and lessen the likelihood of abnormal wear. In addition, porous femoral fixation may further improve long-term durability but currently awaits FDA approval in USA.
We continue to believe that hip resurfacing ultimately will be the primary replacement for most arthritic hips with improved devices but this will require the mastery of implantation techniques by more surgeons.
Disclosures
One or more of the authors (HCA and MDL) certifies that he or she has or may receive payments or benefits from a commercial entity (Wright Medical Technology) related to this work. The institutions of the authors have received funding from Wright Medical Technology, Inc. In addition, funding for this study was provided by the Saint Vincent Medical Center Foundation, Los Angeles.
Footnotes
Level of Evidence: Therapeutic Study Level IV
References
- 1.Amstutz H, Beaulé P, Dorey F, Duff M, Campbell P, Gruen T. Metal-on-metal hybrid surface arthroplasty—surgical technique. J Bone and Joint Surg. 2006;88 A(suppl 1 part 2):234–249. doi: 10.2106/JBJS.F.00273. [DOI] [PubMed] [Google Scholar]
- 2.Amstutz H, Grigoris P, Dorey F. Evolution and future of surface replacement of the hip. J Orthop Sci. 1998;3(3):169–86. doi: 10.1007/s007760050038. [DOI] [PubMed] [Google Scholar]
- 3.Amstutz H, Duff M. Background of metal-on-metal resurfacing. Proc Inst Mech Eng [H] 2006;220(2):85–94. doi: 10.1243/095441105X69088. [DOI] [PubMed] [Google Scholar]
- 4.Amstutz H, Duff M. Evolution of hip resurfacing. In: Amstutz HC, editor. Hip Resurfacing: Principles, Indications, Technique and Results. Philadelphia: Elsevier; 2008. pp. 1–15. [Google Scholar]
- 5.Amstutz H, Duff M, Campbell P, Dorey F. The effects of technique changes on aseptic loosening of the femoral component in hip resurfacing. Results of 600 Conserve Plus with a 3–9 year follow-up. J Arthroplasty. 2007;22(4):481–9. doi: 10.1016/j.arth.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Amstutz HC. Surface replacement arthroplasty. In: Amstutz HC, editor. Total Hip Arthroplasty. New York: Churchill Livingstone; 1991. pp. 295–332. [Google Scholar]
- 7.Amstutz, H. C.; Campbell, P.; Kossovsky, N.; and Clarke, I. C.: Mechanism and clinical significance of wear debris-induced osteolysis. Clin Orthop, (276): 7–18, 1992. [PubMed]
- 8.Amstutz HC, Campbell P, Nasser S, Kossovsky N. Modes of failure of surface replacements. In: Amstutz HC, editor. Hip Arthroplasty. New York: Churchill Livingstone; 1991. pp. 507–534. [Google Scholar]
- 9.Amstutz, H. C.; Clarke, I. C.; Christie, J.; and Graff-Radford, A.: Total hip articular replacement by internal eccentric shells: the tharies approach to total surface replacement arthroplasty. Clin Orthop, (128): 261–84., 1977. [PubMed]
- 10.Amstutz HC, Sparling EA, Grigoris P, Campbell PA, Dorey FJ. Surface replacement: the hip replacement of the future. Hip International. 1998;8(4):187–207. [Google Scholar]
- 11.Amstutz HC, Takamura K, Duff M. The effect of patient selection and surgical technique on the results of Conserve® Plus hip resurfacing—3.5- to 14-year follow-up. Orthop Clin North Am. 2011;I42(2):133–42. doi: 10.1016/j.ocl.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Ball S, Duff M, Amstutz H. Early results of conversion of a failed femoral component in hip resurfacing arthroplasty. J Bone and Joint Surg Am. 2007;89:735–41. doi: 10.2106/JBJS.F.00708. [DOI] [PubMed] [Google Scholar]
- 13.Banerjee M, Bouillon B, Banerjee C, Bäthis H, Lefering R, Nardini M, Schmidt J. Sports activity after total hip resurfacing. Am J Sports Med. 2010;38(6):1229–36. doi: 10.1177/0363546509357609. [DOI] [PubMed] [Google Scholar]
- 14.Beaulé P, Dorey F, Duff M. Fate of cementless acetabular components retained during revision of a femoral component of a total hip arthroplasty. Journal of Bone and Joint Surgery. 2003;85-A(12):2288–93. doi: 10.2106/00004623-200312000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Beaulé P, Duff M, Campbell P, Dorey F, Park S, Amstutz H. Metal-on-metal surface arthroplasty with a cemented femoral component: A 7–10 year follow-up study. J Arthroplasty. 2004;19(12):17–22. doi: 10.1016/j.arth.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 16.Campbell, P.; Mirra, J.; and Amstutz, H. C.: Viability of femoral heads treated with resurfacing arthroplasty. J Arthroplasty, 15(1):120–2, 2000. [DOI] [PubMed]
- 17.Cooper RA, McAllister CM, Borden LS, Bauer TW. Polyethylene debris-induced osteolysis and loosening in uncemented total hip arthroplasty. A cause of late failure. Journal of Arthroplasty. 1992;7(3):285–90. doi: 10.1016/0883-5403(92)90050-Z. [DOI] [PubMed] [Google Scholar]
- 18.Haan R, Pattyn C, Gill H, Murray D, Campbell P, Smet K. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br. 2008;90(10):1291–7. doi: 10.1302/0301-620X.90B10.20533. [DOI] [PubMed] [Google Scholar]
- 19.Eswaramoorthy V, Biant L, Field R. Clinical and radiological outcome of stemmed hip replacement after revision from metal-on-metal resurfacing. J Bone Joint Surg Br. 2009;91(11):1454–8. doi: 10.1302/0301-620X.91B11.22651. [DOI] [PubMed] [Google Scholar]
- 20.Garbuz D, Tanzer M, Greidanus N, Masri B, Duncan C. The John Charnley Award: Metal-on-Metal Hip Resurfacing versus Large-diameter Head Metal-on-Metal Total Hip Arthroplasty: A Randomized Clinical Trial. Clin Orthop Relat Res. 2010;468(2):318–25. doi: 10.1007/s11999-009-1029-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gruen T, Duff M, Wisk L, Amstutz H. Prevalence and clinical relevance of radiographic signs of impingement in metal-on-metal hybrid hip resurfacing. J Bone and Joint Surg Am. 2011;93(16):1519–26. doi: 10.2106/JBJS.I.01723. [DOI] [PubMed] [Google Scholar]
- 22.Head WC. The Wagner surface replacement arthroplasty. Orthop Clin North Am. 1982;13(4):789–97. [PubMed] [Google Scholar]
- 23.Ikeda T, Takahashi K, Kabata T, Sakagoshi D, Tomita K, Yamada M. Polyneuropathy caused by cobalt–chromium metallosis after total hip replacement. Muscle Nerve. 2010;42(1):140–3. doi: 10.1002/mus.21638. [DOI] [PubMed] [Google Scholar]
- 24.Jasty M, Bragdon C, Jiranek W, Chandler H, Maloney W, Harris WH. Etiology Of Osteolysis Around Porous-Coated Cementless Total Hip Arthroplasties. Clinical Orthopaedics and Related Research. 1994;308(NOV):111–126. [PubMed] [Google Scholar]
- 25.Jolley M, Salvati E, Brown G. Early Results and Complications of Surface Replacement of the Hip. J Bone Joint Surg [AM] 1982;64(3):366–377. [PubMed] [Google Scholar]
- 26.Kumar M, Shetty M, Kiran K, Kini A. Validation of navigation assisted cup placement in total hip arthroplasty. Int Orthop. 2012;36(1):17–22. doi: 10.1007/s00264-011-1268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Langton D, Jameson S, Joyce T, Gandhi J, Sidaginamale R, Mereddy P, Lord J, Nargol A. Accelerating failure rate of the ASR total hip replacement. J Bone Joint Surg Br. 2011;93(8):1011–6. doi: 10.1302/0301-620X.93B8.26040. [DOI] [PubMed] [Google Scholar]
- 28.Langton D, Sprowson A, Joyce T, Reed M, Carluke I, Partington P, Nargol A. Blood metal ion concentrations after hip resurfacing arthroplasty: a comparative study of articular surface replacement and Birmingham Hip Resurfacing arthroplasties. JBJS Br. 2009;91(10):1287–95. doi: 10.1302/0301-620X.91B10.22308. [DOI] [PubMed] [Google Scholar]
- 29.Duff M, Amstutz HC. Sporting activity after hip resurfacing: Changes over time. Orthop Clin North Am. 2011;42(2):161–7. doi: 10.1016/j.ocl.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 30.Mai MT, Schmalzried TP, Dorey FJ, Campbell PA, Amstutz HC. The contribution of frictional torque to loosening at the cement–bone interface in Tharies hip replacements. J Bone Joint Surg Am. 1996;78(4):505–11. doi: 10.2106/00004623-199604000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Maloney WJ, Smith RL. Periprosthetic osteolysis in total hip arthroplasty: the role of particulate wear debris. Journal of Bone and Joint Surgery. American Volume. 1995;77A(September):1448–1461. [PubMed] [Google Scholar]
- 32.Mao X, Wong A, Crawford R. Cobalt toxicity—an emerging clinical problem in patients with metal-on-metal hip prostheses? Med J Aust. 2011;194(12):649–51. doi: 10.5694/j.1326-5377.2011.tb03151.x. [DOI] [PubMed] [Google Scholar]
- 33.Murray, W. R., and Van Meter, J. W.: Surface replacement hip arthroplasty: results of the first seventy-four consecutive cases at the University of California, San Francisco. Hip: 156–66, 1982. [PubMed]
- 34.Naal F, Maffiuletti N, Munzinger U, Hersche O. Sports After Hip Resurfacing Arthroplasty. Am J Sports Med. 2007;35(5):705–711. doi: 10.1177/0363546506296606. [DOI] [PubMed] [Google Scholar]
- 35.Narvani A, Tsiridis E, Nwaboku H, Bajekal R. Sporting activity following Birmingham hip resurfacing. Int J Sports Med. 2006;27(6):505–7. doi: 10.1055/s-2006-924199. [DOI] [PubMed] [Google Scholar]
- 36.Oldenburg M, Wegner R, Baur X. Severe cobalt intoxication due to prosthesis wear in repeated total hip arthroplasty. J Arthroplasty. 2009;24(5):825.e 15–20. doi: 10.1016/j.arth.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 37.Pazzaglia U, Apostoli P, Congiu T, Catalani S, Marchese M, Zarattini G. Cobalt, chromium and molybdenum ions kinetics in the human body: data gained from a total hip replacement with massive third body wear of the head and neuropathy by cobalt intoxication. Arch Orthop Trauma Surg. 2011;131(9):1299–308. doi: 10.1007/s00402-011-1268-7. [DOI] [PubMed] [Google Scholar]
- 38.Rizzetti M, Liberini P, Zarattini G, Catalani S, Pazzaglia U, Apostoli P, Padovani A. Loss of sight and sound. Could it be the hip? Lancet. 2009;373(9668):1052. doi: 10.1016/S0140-6736(09)60490-6. [DOI] [PubMed] [Google Scholar]
- 39.Sandiford N, Muirhead-Allwood S, Skinner J. Revision of failed hip resurfacing to total hip arthroplasty rapidly relieves pain and improves function in the early post operative period. J Orthop Surg Res. 2010;5(1):88. doi: 10.1186/1749-799X-5-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schmalzried, T.: Metal–metal bearing surfaces in hip arthroplasty. Orthopedics., 32(9): E-publication, 2009. [DOI] [PubMed]
- 41.Schmalzried, T. P.; Fowble, V. A.; and Amstutz, H. C.: The fate of pelvic osteolysis after reoperation. No recurrence with lesional treatment. Clin Orthop, (350): 128–37, 1998. [PubMed]
- 42.Smith-Petersen M. Evolution of mould arthroplasty of the hip joint. J. Bone Joint Surg. 1948;30 B:59–75. [PubMed] [Google Scholar]
- 43.Steens W, Foerster G, Katzer A. Severe cobalt poisoning with loss of sight after ceramic–metal pairing in a hip—a case report. Acta Orthop. 2006;77(5):830–2. doi: 10.1080/17453670610013079. [DOI] [PubMed] [Google Scholar]
- 44.Su E, Sheehan M, Su S. Comparison of Bone Removed During Total Hip Arthroplasty With a Resurfacing or Conventional Femoral Component: A Cadaveric Study. J Arthroplasty Suppl. 2010;25(2):325–9. doi: 10.1016/j.arth.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 45.Tower, S.: Arthroprosthetic Cobaltism: Neurological and Cardiac Manifestations in Two Patients with Metal-on-Metal Arthroplasty: A Case Report. J Bone Joint Surg Am., 92(7): 2847–51, 2010. [DOI] [PubMed]
- 46.Treacy R, McBryde C, Shears E, Pynsent P. Birmingham hip resurfacing: A MINIMUM FOLLOW-UP OF TEN YEARS. J Bone Joint Surg Br. 2011;93(1):27–33. doi: 10.1302/0301-620X.93B1.24134. [DOI] [PubMed] [Google Scholar]
- 47.Vendittoli P, Lavigne M, Girard J, Roy A. A randomised study comparing resection of acetabular bone at resurfacing and total hip replacement. J Bone Joint Surg Br. 2006;88(8):997–1002. doi: 10.1302/0301-620X.88B8.17615. [DOI] [PubMed] [Google Scholar]
- 48.Wera G, Gillespie R, Petty C, Petersilge W, Kraay M, Goldberg V. Revision of hip resurfacing arthroplasty. Am J Orthop (Belle Mead NJ) 2010;39(8):E78–83. [PubMed] [Google Scholar]