Abstract
Objectives
To determine the extent to which demographic and geographic disparities exist in post-acute rehabilitation care (PARC) use following hip fracture.
Design
Cross-sectional analysis of two years (2005–2006) of population-based, hospital discharge data.
Setting
All short-term acute care hospitals in four demographically and geographically diverse states (AZ, FL, NJ, WI).
Participants
Individuals 65 years and older (mean age of 82.9 years) admitted to the hospital with a hip fracture and who survived their inpatient stay (N=64,065). The sample was 75.1 percent female, 91.5 percent White, 5.8 percent Hispanic, and 2.7 percent Black.
Measurements
1) whether the subject received institutional PARC; 2) for subjects who did not receive institutional care, whether they received home health (HH) care; and 3) for subjects who received institutional care, whether they received skilled nursing facility (SNF) or inpatient rehabilitation facility (IRF) care. Multilevel logistic regression analyses were conducted to identify demographic and geographic disparities in PARC use.
Results
Considering PARC on a continuum from more to less hours of care per day (IRF→SNF→HH→no HH), we found that minorities and individuals of lower socioeconomic status (SES) generally received a lower volume of care. Individuals on Medicaid or who were uninsured were less likely to receive institutional care (OR=0.23 [95% CI: 0.18–0.30]) and to receive HH (OR=0.46 [0.30–0.70]) and more likely to receive SNF versus IRF care (OR=2.03 [1.36–3.05]). Hispanics were less likely to receive institutional care (OR=0.70 [0.62–0.79]); and Hispanics and Blacks were more likely to receive SNF versus IRF care (ORs of 1.31 and 1.49 respectively). Geographic differences in PARC were also present.
Conclusion
Several demographic and geographic disparities in PARC use were identified. Future research should confirm these findings and further elucidate factors that contribute to the observed disparities.
Keywords: hip fracture, healthcare disparities, rehabilitation
INTRODUCTION
Hip fracture is a common problem in older adults. In 2006, 316,000 individuals 65 and older were admitted to U.S. hospitals for hip fracture.1 While U.S. hip fracture rates have declined,2 the absolute number of fractures is expected to increase significantly as the population ages. The worldwide incidence of hip fractures in 2050 is estimated at 4.5 million,3 an increase of approximately 3 million from current estimates.
Mortality and morbidity associated with hip fracture is profound. Mortality rates in the first year following hip fracture range from 13–37 percent 4,5 with higher rates in men, minorities,6 and individuals of lower socioeconomic status (SES).7 Among those who survive the first year, 40 percent will be unable to walk independently and 60 percent will require assistance with activities of daily living.8,9 While literature on gender, racial/ethnic, and socioeconomic differences in hip fracture outcomes is limited, available evidence suggests that functional outcomes in Whites and males are slightly better 6 and that minorities and individuals of lower SES wait longer for surgery,7,10 which may lead to greater complications post-surgery.11
Rehabilitation is an important component of hip fracture care. Evidence on the effectiveness of different rehabilitation approaches is somewhat unclear, but generally suggests the most successful programs involve more intensive exercise and multidisciplinary care/inpatient rehabilitation (versus outpatient care), with no indication of harm in regard to patient outcome or cost.12–14 Rehabilitation following hip fracture begins in the acute care setting, but most occurs in post-acute care settings (i.e., skilled nursing facility (SNF), inpatient rehabilitation facility (IRF), home health (HH), and/or outpatient settings) .
Increases in the diversity of the U.S. population, evidence of racial and socioeconomic disparities in hip fracture outcomes, and the increasing incidence of hip fracture underscore the importance of improving our understanding of disparities in post-acute rehabilitation care (PARC). Few studies have specifically examined this issue. Those that have been conducted have focused on the use of institutional care versus discharge to home with or without HH.15–17 These studies generally found that minorities were more likely to be discharged home. Information on disparities in the use of SNF versus IRF care or HH versus no HH was not provided in any of these studies, nor was information on geographic disparities in PARC. Data examined in these studies also covered periods prior to and during implementation of prospective payment systems (PPS) in all post-acute settings. Evidence suggests that use of post-acute care has decreased in response to PPS and that these decreases are differentially larger for certain demographic subgroups.18,19
The objective of this study was to use population-based, hospital discharge data to determine the extent to which demographic and geographic disparities exist in PARC use following hip fracture. Considering PARC on continuum from more to less hours of care per day or per week (IRF→SNF→HH→no HH), 18,20 we hypothesized that demographic and geographic disparities in the amount of care received would be present. This study extends previous research by using post-PPS data, examining different types of PARC, and including additional important covariates (e.g., supply of PARC, hospital characteristics) that may explain variation in PARC use.
METHODS
Research Design
We conducted a cross-sectional analysis of two years (2005, 2006) of population-based, hospital discharge data from short-term, acute care hospitals in four demographically and geographically diverse states (AZ, FL, NJ, WI). Records on patients admitted with a primary diagnosis of hip fracture were identified and merged with hospital, ZIP code, and county-level data.
Data Sources
Our primary source of data was the 2005–2006 State Inpatient Databases (SIDs) from AZ, FL, NJ, and WI.21 These states were selected based on the availability of key data elements (e.g., race) and to represent the four U.S. census regions. 2006 data on hospital characteristics were obtained from: the American Hospital Association Annual Survey Database; the Centers for Medicare and Medicaid Services (CMS) Provider of Services File; and CMS Hospital Cost Reports. We used the 2006 update of Census 2000 data from Claritas, Inc. to obtain ZIP code-level data and 2006 Area Resource File data to obtain county-level data.
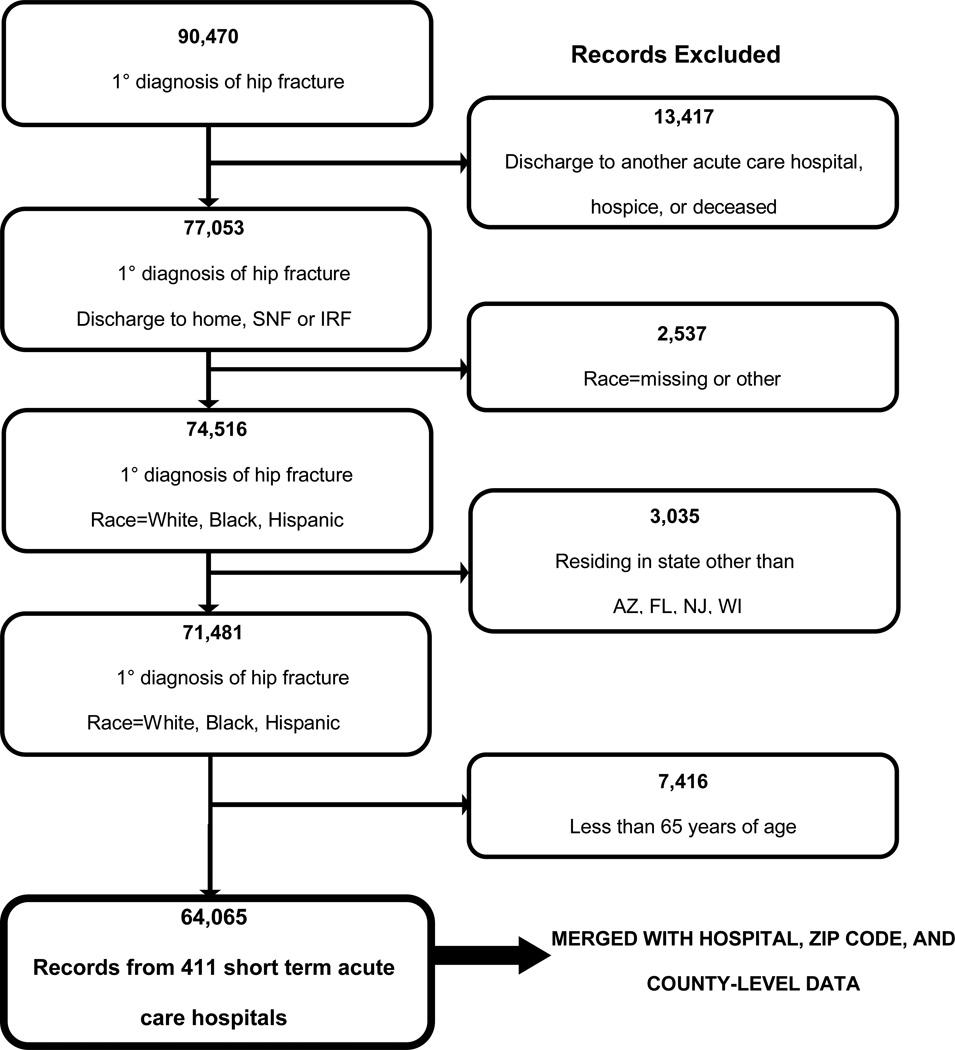
Sample
Our sample was limited to individuals 65 years and older who admitted to the hospital with a primary diagnosis of hip fracture (ICD-9-CM codes 820.0x-820.9x, 821.0x-821.3x). Figure 1 outlines our exclusion criteria.
Figure 1.
Creation of Final Sample
Study Variables
We hypothesized that factors at the individual (e.g., demographic, clinical), hospital (e.g., staffing), community (e.g., availability of PARC), and state levels (e.g., practice patterns) influence the type of PARC received following hip fracture.22 Our final variable selection was based on this concept, as well data availability. We created three dichotomous dependent variables: 1) whether the subject received institutional care; 2) for subjects who did not receive institutional care, whether they received home health care; and 3) for subjects who received institutional care, whether they received SNF or IRF care.
Our primary independent variables were race, sex, age, socioeconomic status (SES), metropolitan status of residence, and state. The subject’s SES was represented by insurance (being uninsured or on Medicaid, relative to Medicare/private insurance) and median household income in the subject’s ZIP code.23 We created a three-level categorization for the counties in which cases resided: large metropolitan; medium/small metropolitan; or micropolitan/non-micropolitan24 and controlled for the state in which the subject resided.
To account for clinical factors that may influence PARC use we included variables for: Emergency Department admission; length of stay (categorized based on tertile distribution as ≤3 days; 4–6 days; 6 or more days); joint replacement;25 illness severity and mortality risk;26 and comorbidities.27 We created an indicator variable for individuals who had 4 or more comorbidities as well as indicators for select comorbidities based on conditions identified in the literature and those that were correlated with the outcome in preliminary analyses. These included: diabetes with complications, hypertension, obesity, congestive heart failure, peripheral vascular disease, chronic pulmonary disease, rheumatoid arthritis, osteoarthritis, cancer (malignancy), weight loss, and depression.
We included several hospital variables as proxies for quality of care: volume of hip fractures (i.e., number of hip fracture admissions averaged across the two years),28 whether the hospital had a major medical school affiliation,29 registered nurse (RN) FTEs per 100 admissions,18, 30 and physical and occupational therapists FTEs per 1000 admissions. We also included a variable to indicate the for-profit status of the hospital. To control for PARC supply, we included variables to indicate whether the hospital maintained a SNF, HH agency, or IRF; and county-level measures of the number of PTs/OTs, HH agencies, SNF beds, and IRFs, each standardized to the county population.
Data Analysis
All analyses were conducted using Stata (10.1) and multilevel mixed effects logistic regression models to account for the correlation of patients within hospital and to examine the associations between our independent variables and PARC use. We estimated three separate, models, one for outcome. Because SIDs in FL did not distinguish between the use of SNFs and IRFs in 2005, FL data from this year were excluded from the SNF/IRF analysis.
For each outcome, the first level of our models included all independent variables at the patient, hospital, and county level (fixed effects). To account for unobserved heterogeneity in PARC use by hospital, we included hospital-specific random intercepts. To quantify the heterogeneity across hospitals, we calculated the median odds ratio (MOR).31An MOR of 1 indicates no variation in PARC use due to unobserved factors between hospitals. The larger the MOR, the greater the variation in hospital intercepts. We also explored the interaction of race and income.
RESULTS
Our sample was 92 percent White and 75 percent female with a mean age of 80.1 years (Table 1). Ninety percent of the sample used institutional care. Of those discharged to an institution, 81 percent received SNF care. Of those discharged home, 55 percent received HH. Differences by type of PARC were apparent in the descriptive analyses.
Table 1.
Demographic, Geographic, & Clinical Characteristics of Sample (N=64,065)
| By Discharge Status * |
|||||
|---|---|---|---|---|---|
| Home (9.9%) N=6,350 |
Institution (90.1%) N=57,715 |
||||
| Entire Sample (100%) |
Home (45.3%) |
HH (54.7%) |
SNF† (80.5%) |
IRF† (19.5%) |
|
| DEMOGRAPHIC & GEOGRAPHIC | |||||
| Female (%) | 75.1 | 69.0# | 71.5# | 76.2 | 73.9 |
| Race (%) | |||||
| White | 91.5 | 86.1# | 87.2# | 93.0 | 91.2 |
| Black | 2.7¶ | 2.1# | 3.0# | 2.6** | 2.1** |
| Hispanic | 5.8 | 11.8 | 9.8 | 4.4 | 6.7 |
| Mean(±SD) Age, y | 82.9(7.5) | 79.9(8.2) | 79.2(8.2) | 83.7(7.3) | 81.4(7.3) |
| Insurance (%) | |||||
| Medicare/Private | 98.8 | 94.5 | 97.0 | 99.3** | 99.1** |
| Medicaid | 0.6 | 3.1 | 1.8 | 0.5** | 0.5** |
| None/Self-Pay | 0.5 | 2.4 | 1.2 | 0.5 | 0.2 |
| Median Household Income‡ (%) | |||||
| Highest quartile | 23.8 | 22.5 | 18.9 | 26.6 | 34.4 |
| Quartile 3 | 24.3 | 27.2 | 24.5 | 24.9** | 23.9** |
| Quartile 2 | 28.0¶ | 25.4 | 28.6 | 28.0 | 21.7 |
| Lowest quartile | 24.0 | 25.1 | 28.1 | 20.6** | 20.1** |
| Patient residence§ (%) | |||||
| Micropolitan, non-metro area | 9.7 | 17.2 | 9.7 | 11.4 | 5.4 |
| Medium-small metro area | 30.0 | 26.4 | 34.5 | 27.8 | 31.5 |
| Large metro area | 60.2 | 56.3 | 55.8 | 60.8 | 63.1 |
| Patient State (%) | |||||
| Arizona | 14.2 | 27.3# | 25.1# | 16.3** | 16.8** |
| Florida | 50.5 | 38.1 | 60.1 | 37.4 | 29.8 |
| New Jersey | 20.8 | 13.2 | 7.2 | 25.0 | 43.0 |
| Wisconsin | 14.5 | 21.4 | 7.6 | 20.8 | 10.9 |
|
CLINICAL | |||||
| ED admission (%) | 81.8 | 71.1# | 70.5# | 80.8 | 87.1 |
| Mean (±SD) length of stay, days | 6.2 (4.0) | 6.5 (5.8)# | 6.8 (5.2)# | 6.2 (3.9) | 5.9 (3.4) |
| Fracture with a joint replacement (%) | 33.0 | 26.6# | 24.2# | 33.2 | 36.9 |
| APR-DRG severity measure (%) | |||||
| Minor | 24.2 | 27.8# | 28.2# | 24.8 | 29.2 |
| Moderate | 48.5 | 47.6 # | 46.4# | 47.7** | 47.7** |
| Major/extreme | 27.3 | 24.5 # | 25.4# | 27.5 | 23.1 |
| APR-DRG mortality risk (%) | |||||
| Minor | 28.6 | 40.6# | 41.9# | 25.5 | 35.0 |
| Moderate | 54.6 | 44.5# | 44.4# | 56.7 | 50.2 |
| Major/extreme | 16.8 | 14.9# | 13.7# | 17.8 | 14.8 |
| Comorbidities (%) | |||||
| Diabetes with complications | 2.3 ¶ | 1.8 # | 2.0# | 2.3 | 3.0 |
| Obesity | 1.9 ¶ | 1.2 # | 2.0# | 1.9** | 2.2** |
| Hypertension | 64.3 | 59.4# | 59.6# | 65.4** | 66.4** |
| Congestive heart failure | 15.8 | 10.2 # | 11.5# | 17.4 | 13.2 |
| Peripheral vascular disorders | 5.6 | 5.0# | 5.8# | 5.9** | 5.5** |
| Chronic pulmonary disease | 21.5 | 20.5 # | 20.1# | 21.4** | 21.3** |
| Rheumatoid arthritis | 3.1 ¶ | 3.4 # | 3.7# | 3.1** | 3.5** |
| Osteoarthritis | 11.5¶ | 10.7 | 13.4 | 11.1 | 12.9 |
| Cancer | 2.7 ¶ | 3.2 # | 2.8# | 2.7** | 2.7** |
| Weight loss | 2.4 | 3.9 | 5.5 | 2.4 | 1.4 |
| Depression | 9.9 | 6.9# | 7.7# | 11.0 | 9.3 |
| 4 or more comorbidities | 26.6 | 19.6# | 20.1# | 29.3 | 25.1 |
HH=home health; SNF=skilled nursing facility; IRF=inpatient rehabilitation facility; APR-DRG=All patient refined diagnosis related group
all comparisons significantly different (p<.01) unless indicated;
only 2006 FL data are included, in 2005 the FL State Inpatient Database did not distinguish between IRF and SNF discharges;
based on patient zip-code;
based on patient county of residence;
no statistically significant difference in proportion discharged to institution vs home;
no statistically significant difference in proportion discharged to home with HH vs no HH;
no statistically significant difference in proportion discharged to IRF vs SNF
Results of multilevel analyses are presented in Table 2. There was no evidence of an interaction between race and income in any model. The full models are presented online.
Table 2.
Results of Mixed Effect Logistic Regression Analyses
| Institution vs Home (base category) N=63,626† |
Home Health vs Home (base category) N=6,291† |
Skilled Nursing Facility vs IRF (base category) N=44,333† |
|||||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | ||
| Sociodemographic | |||||||
| Race (ref. White): | Black | 0.99 (0.82 – 1.19) | 0.91 | 1.86 (1.23 – 2.82) | <0.01 | 1.49 (1.22 – 1.83) | <0.01 |
| Hispanic | 0.70 (0.62 – 0.79) | <0.01 | 0.96 (0.74 – 1.24) | 0.74 | 1.31 (1.13 – 1.52) | <0.01 | |
| Female | 1.18 (1.11 – 1.26) | <0.01 | 1.15 (1.01 – 1.32) | 0.04 | 1.19 (1.11 – 1.27) | <0.01 | |
| Age/10 ‡ | 1.86 (1.78 – 1.93) | <0.01 | 0.91 (0.84 – 0.99) | 0.02 | 1.64 (1.58 – 1.71) | <0.01 | |
| Insurance (ref. Mdcr./private): | Medicaid | 0.23 (0.18 – 0.30) | <0.01 | 0.46 (0.30 – 0.70) | <0.01 | 2.03 (1.36 – 3.05) | <0.01 |
| Uninsured | 0.21 (0.16 – 0.28) | <0.01 | 0.39 (0.24 – 0.63) | <0.01 | 2.36 (1.33 – 4.19) | <0.01 | |
| Income§ (ref quartile 4): | Quartile 3 | 1.13 (1.02 – 1.24) | 0.02 | 0.91 (0.74 – 1.11) | 0.34 | 1.08 (0.98 – 1.18) | 0.11 |
| Quartile 2 | 1.19 (1.08 – 1.32) | <0.01 | 0.99 (0.80 – 1.22) | 0.93 | 1.07 (0.97 – 1.19) | 0.18 | |
| Quartile 1 | 1.27 (1.14 – 1.42) | <0.01 | 0.98 (0.79 – 1.22) | 0.86 | 1.27 (1.14 – 1.42) | <0.01 | |
| Geographic | |||||||
| Metro Status (ref. micro/rural): | Med. metro | 1.30 (1.09 – 1.55) | <0.01 | 1.46 (1.02 – 2.09) | 0.04 | 0.96 (0.75 – 1.22) | 0.72 |
| Lg. metro | 1.38 (1.15 – 1.66) | <0.01 | 0.97 (0.68 – 1.40) | 0.89 | 1.26 (0.97 – 1.65) | 0.09 | |
| State (ref. Wisconsin): | Arizona | 0.48 (0.34 – 0.67) | <0.01 | 1.89 (1.00 – 3.57) | 0.05 | 0.40 (0.14 – 1.18) | 0.10 |
| Florida | 0.66 (0.49 – 0.89) | 0.01 | 5.03 (2.86 – 8.86) | <0.01 | 0.73 (0.28 – 1.91) | 0.53 | |
| New Jersey | 1.44 (1.06 – 1.96) | 0.02 | 1.15 (0.64 – 2.08) | 0.64 | 0.05 (0.02 – 0.13) | <0.01 | |
OR=odds ratio; IRF=inpatient rehabilitation facility
records with missing observations dropped;
age divided by 10 to assist in interpretation of odds ratio;
median household income for the zip code of patient’s residence
Use of Institutional Care
Females, older individuals, those on Medicare/Private insurance, those with lower incomes, and those living in metropolitan areas were more likely to receive institutional care. Subjects living in NJ were most likely to receive institutional care and those in AZ were least likely. Hispanics, the uninsured, and those on Medicaid were less likely to receive institutional care.
None of the measured hospital characteristics and only one PARC supply variable (SNF beds) was associated with institutional PARC (online tables). The MOR was 1.82 indicating heterogeneity across hospitals in the propensity for individuals with similar characteristics to receive institutional PARC. The proportion of the unobserved variation in institutional PARC attributable to unobserved (i.e., unmeasured) hospital characteristics was 11 percent while that attributable to unobserved individual characteristics was 89 percent.
Use of HH Care
Blacks, those on Medicare/private insurance, and those living in FL were more likely to receive HH (Table 2). Uninsured individuals and those on Medicaid were less likely. Patients seen at hospitals that treated a higher volume of hip fractures or that lived in counties with more PTs/OTs were more likely to receive HH (online table). No other hospital or supply variables were associated with HH use. The MOR was 2.80 and the proportion of the unobserved variation in discharge status attributable to unobserved hospital characteristics was 26 percent.
Use of SNF versus IRF Care
Blacks, females, older individuals, the uninsured, those on Medicaid, and those with lower incomes were more likely to use SNF care. NJ residents were much more likely to receive IRF care. No hospital characteristics were associated with IRF use. Patients seen in hospitals with an IRF or counties with more IRFs were more likely to receive IRF care. The supply of SNF beds was associated with SNF care. The MOR was 8.07, indicating considerable heterogeneity across hospitals in the propensity of an individual to use SNF versus IRF care. The proportion of unobserved variation in SNF versus IRF care attributable to unmeasured hospital characteristics was 59 percent.
DISCUSSION
Considering PARC as a continuum of more to less hours of care per day or per week (ie, IRF→SNF→HH→no HH) 18,20, we found some consistent findings indicating that minorities and individuals of lower SES received a lower volume of PARC. Individuals on Medicaid or who were uninsured were more likely to receive a lower volume of PARC in all models. Hispanics in the institution/home model and Hispanics and Blacks in the SNF/IRF model were more likely to receive a lower volume of PARC. Individuals with lower income were also more likely to receive a lower volume of PARC in the SNF/IRF model. Others have reported that minorities with hip fracture are more likely to be discharged home.15–17 Data on racial disparities between SNF and IRF care for hip fracture, however, are limited.
We also identified some geographic differences in use of PARC following hip fracture, most notably that individuals living in non-metropolitan areas were more likely to receive a lower volume of care in the institution/home model. State to state variation in PARC use was also apparent. These state effects were large even though our models included PARC supply variables and hospital-specific intercepts. These findings are consistent with a large body of literature suggesting that where you live impacts the intensity and quality of care you receive.
Few of the measured hospital characteristics were associated with PARC use. Patients seen at hospitals that treated a higher volume of hip fractures were more likely to receive HH if discharged home. Hip fracture volume may be a marker for higher quality of care.28 As evidenced by the MOR’s, there was considerable heterogeneity across hospitals in unmeasured hospital characteristics associated with PARC use. Heterogeneity across hospitals in the propensity of individuals with similar demographic and clinical characteristics to receive the same type of PARC was greatest in the SNF/IRF model and least in the institution/home model. These findings may reflect greater uncertainty about the use and effectiveness of SNF versus IRF care relative to institution versus home care. Future work should aim to better understand the sources of variation in PARC use, at both the hospital and healthcare provider levels, and ultimately develop strategies to minimize variation due to non-clinical factors.
Some of the PARC supply variables were associated with PARC use in the expected directions. Local availability of PARC is a major determinant of whether an individual receives that type of care. The non-significant findings with some of our supply measures may be due to their lack of precision. For example, we only had a count of HH agencies which does not take into account the number of staff or number of therapists working at the agency.
Strengths of this study include the analysis of population-based data that were collected post implementation of PPS in post-acute care settings; a more complete analysis of the use of various types of PARC; and the inclusion of important covariates. Despite these strengths, our study had several limitations. We examined data from only four states and found PARC use varied considerably by state. Our findings may not be generalizable to other states. We also did not have any direct measures of the patient’s functional status, nor did we have a measure of outpatient therapy use. It is unclear whether individuals who did not receive HH received outpatient therapy. In addition, we did not directly measures hours of PARC use. Our measure of income was also imprecise (at ZIP code level) and we did not have a measure of education, an additional SES variable. Finally, our models lacked direct measures of patient preferences and provider characteristics.
Despite these limitations, this study adds to the limited, recent literature on disparities in PARC for hip fracture. Documenting healthcare disparities can inform healthcare policy and the conduct of future studies examining strategies to minimize these disparities. While eliminating healthcare disparities requires comprehensive approaches and well-designed interventions at the practice, institutional, community, state, and national levels, our findings suggest that efforts at the hospital (e.g., modifying structural aspects of care, improving provider communication/cultural competence), and state-levels (e.g., financial aspects of healthcare delivery) may be most effective in minimizing PARC disparities. The interplay between individual (patient and provider) and contextual factors also needs further exploration and could be a critical determinant in PARC use.
Conclusions
After controlling for illness severity/comorbidities, hospital characteristics, and community-level factors, demographic and geographic differences in PARC use following hip fracture remained. Some of these differences appear to be indicative of racial, socioeconomic, and geographic disparities in care. Because minorities and individuals of lower SES may experience higher rates of mortality and surgical complications post-fracture, efforts to minimize these disparities and increase our understanding of the reasons behind them are needed.
Supplementary Material
ACKNOWLEDGMENTS
Conflict of Interest: This study was supported by funding from the National Center for Medical Rehabilitation Research, National Institute of Child Health and Human Development (NICHD), National Institutes of Health, grant R21 HD057980.
Dr. Freburger & Dr. Holmes received funding from the National Center for Medical Rehabilitation Research, NIH, to conduct this study. Dr. Freburger is a volunteer member of the American Physical Therapy Association’s (APTA) Health Policy/Workforce Task Force and is a past volunteer member of APTA's Research Advisory Board. Dr. Holmes is a volunteer member of the APTA’s Research Advisory Board.
Sponsor’s Role: The sponsor did not play any role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Study concept and design (JKF, GMH); acquisition of subjects and/or data (JKF); analysis and interpretation of data (JKF, LEK, GMH); preparation of manuscript (JKF, LEK, GMH).
REFERENCES
- 1. [Accessed September 8, 2011];Hip Fractures Among Older Adults. Centers for Disease Control and Prevention (online) Available at http://www.cdc.gov/HomeandRecreationalSafety/Falls/adulthipfx.html.
- 2.Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302:1573–1579. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407–413. doi: 10.1007/pl00004148. [DOI] [PubMed] [Google Scholar]
- 4.Leibson CL, Tosteson AN, Gabriel SE, et al. Mortality, disability, and nursing home use for persons with and without hip fracture: A population-based study. J Am Geriatr Soc. 2002;50:1644–1650. doi: 10.1046/j.1532-5415.2002.50455.x. [DOI] [PubMed] [Google Scholar]
- 5.Zuckerman JD. Hip fracture. N Engl J Med. 1996;334:1519–1525. doi: 10.1056/NEJM199606063342307. [DOI] [PubMed] [Google Scholar]
- 6.Sterling RS. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop Relat Res. 2011;469:1913–1918. doi: 10.1007/s11999-010-1736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barone AP, Fusco D, Colais P, et al. Effects of socioeconomic position on 30-day mortality and wait for surgery after hip fracture. Int J Qual Health Care. 2009;21:379–386. doi: 10.1093/intqhc/mzp046. [DOI] [PubMed] [Google Scholar]
- 8.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55:M498–M507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 9.Magaziner J, Simonsick EM, Kashner TM, et al. Predictors of functional recovery one year following hospital discharge for hip fracture: A prospective study. J Gerontol . 1990;45:M101–M107. doi: 10.1093/geronj/45.3.m101. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen-Oghalai TU, Kuo YF, Wu H, et al. The impact of race/ethnicity on preoperative time to hip stabilization procedure after hip fracture. South Med J. 2010;103:414–418. doi: 10.1097/SMJ.0b013e3181d7ba2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simunovic N, Devereaux PG, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: Systematic review and meta-analysis. CMAJ. 2010;182:1609–1616. doi: 10.1503/cmaj.092220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Handoll HH, Cameron ID, Mak JC, et al. Multidisciplinary rehabilitation for older people with hip fractures. Cochrane Database Syst Rev. 2009;(4):CD007125. doi: 10.1002/14651858.CD007125.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Handoll HH, Sherrington C, Mak JC. Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database Syst Rev. 2011;(3):CD001704. doi: 10.1002/14651858.CD001704.pub4. [DOI] [PubMed] [Google Scholar]
- 14.Stott D, Handoll H. Rehabilitation of older people after hip (proximal femoral) fracture. Cochrane Database Syst Rev. 2011;(8):ED000023. doi: 10.1002/14651858.ED000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aharonoff GB, Barsky A, Hiebert R, et al. Predictors of discharge to a skilled nursing facility following hip fracture surgery in New York State. Gerontology. 2004;50:298–302. doi: 10.1159/000079127. [DOI] [PubMed] [Google Scholar]
- 16.Ganesan K, Pan D, Teklehaimenot S, et al. Racial diferences in institutionalization after hip fractures: California hospital discharge data. Ethn Dis. 2005;15(S5):30–33. [PubMed] [Google Scholar]
- 17.Nguyen-Oghalai TU, Ottenbacher KJ, Kuo YF, et al. Disparities in utilization of outpatient rehabilitative care following hip fracture hospitalization with respect to race and ethnicity. Arch Phys Med Rehabil. 2009;90:560–563. doi: 10.1016/j.apmr.2008.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.FitzGerald JD, Mangione CM, Boscardin J, et al. Impact of changes in Medicare Home Health care reimbursement on month-to-month Home Health utilization between 1996 and 2001 for a national sample of patients undergoing orthopedic procedures. Med Care. 2006;44:870–878. doi: 10.1097/01.mlr.0000220687.92922.64. [DOI] [PubMed] [Google Scholar]
- 19.Zhu CW. Effects of the balanced budget act on Medicare home health utilization. J Am Geriatr Soc. 2004;52:989–994. doi: 10.1111/j.1532-5415.2004.52270.x. [DOI] [PubMed] [Google Scholar]
- 20.DeJong G, Hsieh CH, Gassaway J, et al. Characterizing rehabilitation services for patients with knee and hip replacement in skilled nursing facilities and inpatient rehabilitation facilities. Arch Phys Med Rehabil. 2009;90:1269–1283. doi: 10.1016/j.apmr.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 21. [Accessed September 1, 2011];Overview of the State Inpatient Databases. Agency for Healthcare Research and Quality (online) Availabe at http://www.hcup-us.ahrq.gov/sidoverview.jsp.
- 22.Freburger JK, Holmes GM, Ku LJ, et al. Disparities in post-acute rehabilitation care for joint replacement. Arthritis Care Res. 2011;63:1020–1030. doi: 10.1002/acr.20477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krieger N. Overcoming the absence of socioeconomic data in medical records: Validation and application of a census-based methodology. Am J Public Health. 1992;82:703–710. doi: 10.2105/ajph.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ingram DD, Franco S. NCHS Urban-Rural Classification Scheme for Counties. Hyattsville, MD: National Center for Health Statistics; 2006. [PubMed] [Google Scholar]
- 25.Hoverman C, Shugarman LR, Saliba D, et al. Use of postacute care by nursing home residents hospitalized for stroke or hip fracture: How prevalent and to what end? J Am Geriatr Soc. 2008;56:1490–1496. doi: 10.1111/j.1532-5415.2008.01824.x. [DOI] [PubMed] [Google Scholar]
- 26.Averill RF, Goldfield N, Hughes JS, et al. All Patient Refined Diagnosis Related Groups (APR-DRGs), Methodology Overview. Wallingford, CT: 3M Health Information Systems; 2003. [Google Scholar]
- 27.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Shervin N, Rubash HE, Katz JN. Orthopaedic procedure volume and patient outcomes: A systematic literature review. Clin Orthop Relat Res. 2007;457:35–41. doi: 10.1097/BLO.0b013e3180375514. [DOI] [PubMed] [Google Scholar]
- 29.Ayanian JZ, Weissman JS. Teaching hospitals and quality of care: A review of the literature. Milbank Q. 2002;80:569–593. doi: 10.1111/1468-0009.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kane RL, Shamliyan TA, Mueller C, et al. The association of registered nurse staffing levels and patient outcomes: Systematic review and meta-analysis. Med Care. 2007;45:1195–1204. doi: 10.1097/MLR.0b013e3181468ca3. [DOI] [PubMed] [Google Scholar]
- 31.Larsen K, Petersen JH, Budtz-Jorgensen E, et al. Interpreting parameters in the logistic regression model with random effects. Biometrics. 2000;56:909–914. doi: 10.1111/j.0006-341x.2000.00909.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.