Abstract
Objective
This study aimed to determine if and to what extent: (1) socioeconomic disparities exist in the health-related quality of life (QOL) of children with cancer or brain tumors and healthy children; and (2) family functioning and burden mediate the relationship between socioeconomic status and children’s QOL.
Methods
In this cross-sectional study, parents of children ages 2–18 with (n=71) and without (n=135) cancer or brain tumors completed in-person interviewer-assisted surveys assessing sociodemographics (including income and parental education), child QOL (measure: PedsQL), family functioning (measure: FACES IV) and burden (measure: Impact on the Family Scale). For children with cancer, clinical characteristics were captured through medical record abstraction. Multiple linear regression was used to determine the relationship between income and child QOL; the interaction between group status and income was assessed. Staged multivariate regression models were used to assess the role of family factors in this relationship among children with cancer.
Results
In multivariate analyses, the effect of income differed by cancer status; lower income was associated with worse QOL in children with cancer, but not among healthy children. Among children with cancer, this relationship was significantly attenuated by family burden.
Conclusions
Significant socioeconomic disparities exist in the QOL of children with cancer. Family factors partially explain the relationship between low income and poor QOL outcomes among these children. Lower income families may have fewer resources to cope with their child’s cancer. Increased support, monitoring, and referrals to reduce burden for these families may lead to improved QOL in children with cancer.
Keywords: cancer, oncology, quality of life, family functioning, burden, socioeconomic disparities
INTRODUCTION
As treatment advances and survival rates have improved for childhood cancer [1], it has become increasingly important to understand the factors that influence health-related quality of life (QOL) among survivors. Disease and treatment-related factors are known to influence the QOL of children with and survivors of childhood cancer. However, little is known about the family-level effects on QOL [2]. In particular, family socioeconomic status (SES) and family functioning have each been shown to be associated with worse child health [3–5], and may be important predictors of the QOL of children with cancer.
Few studies have explicitly explored the effect of SES on child QOL. Among studies of children with cancer or survivors of childhood cancer, no study has explicitly focused on the impact of SES on child QOL as a primary aim of the study. Extant studies have included SES as one of many demographic predictors of child QOL [6–9] or have utilized SES as a control variable in their analyses [10; 11] without explicitly examining this factor. Findings from these studies have also been inconsistent; of the five studies reporting the unadjusted (i.e., bivariate) association between SES and child QOL, two [8; 10] found that lower SES was associated with worse child QOL, while three [7; 9; 11] found no such association. Only two studies reported the adjusted association between these factors, controlling for confounding variables, and reported contradictory findings [6; 8]. These inconsistencies are likely due to methodological differences, including variation in the population under examination (based both in the US and abroad, and at various stages of the cancer and survivorship trajectory) and the covariates considered. Further, these studies used various measures of SES, including parental income [6; 7], adjusted household income thresholds [8], paternal occupation, and maternal education [9]. Studies also often collapsed these SES variables into a summary measure or composite of SES [10; 11] or dichotomized these variables in their analyses [6; 7]. Studies are needed to test the relationship between SES and child QOL that employ continuous or multi-category measures of SES (e.g., family income and parental education), as this would enable a more nuanced evaluation this potential association.
This study explicitly explored the relationship between SES and child QOL. Theory suggests that family functioning may mediate the relationship between low SES and adverse QOL outcomes. Specifically, social-ecological systems theory supports the idea that children and parents are nested within families and that stress on the family system has a major influence on the health and functioning of all family members [12–14]. Few studies, however, have examined the role of family functioning in child QOL (e.g., [15]) and none has explored it as a mediator of the SES-QOL relationship, despite the well-established association between low SES and poor family functioning [16–19].
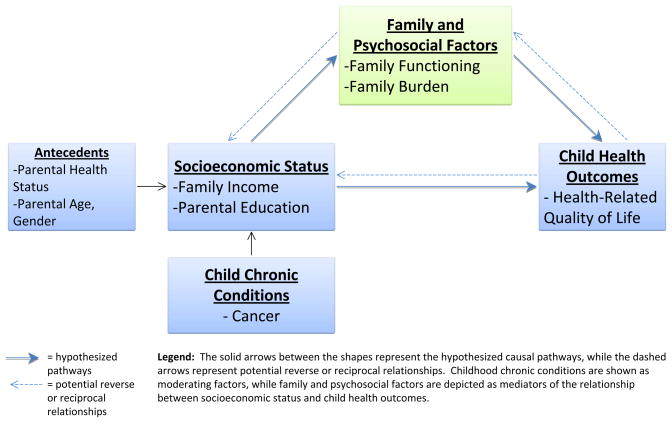
Based on this background and theory, Figure 1 presents the conceptual model utilized in this study. The model highlights the potential moderating role of childhood cancer in the association between family SES and child health, the hypothesized mediating role of family functioning and burden, and the potential bi-directional or reciprocal relationships between these factors (as indicated by the dashed arrows). Moreover, the effect of family functioning as a mediator may differ for children with cancer and healthy children, suggesting a moderated mediation model.
Figure 1.
Conceptual Model of the Impact of Socioeconomic Status on Child Health Outcomes: the Role of Moderators and Mediators
To our knowledge, no study has evaluated the role of family functioning in the relationship between low SES and poor QOL among children with cancer. To address this gap in the literature, the purpose of this study was to: (1) evaluate the relationship between SES and child QOL outcomes among families of children with and without cancer or brain tumors; and (2) evaluate if and to what extent family functioning and burden mediated this relationship. We hypothesized that children from higher SES families would have better QOL than children from lower SES families, that family factors would attenuate this association, and that this association would differ for children with cancer and healthy children. Understanding if such disparities exist and what factors may mitigate this relationship will be essential in improving child outcomes across the income spectrum.
METHODS
Study Design, Population, and Data Sources
This research used a cohort study design and enrolled parents and their children with cancer or a brain tumor and a comparison group of parents and their healthy children. The parent who was the most involved in providing support and care to the child was recruited into the study. Parents in this study were defined as biological, step, adoptive or foster parents, grandparents, or legal guardians of the child.
Participants
Participant recruitment and selection and data collection have been reported in detail elsewhere [20]. Briefly, parents and children with cancer, including malignant or non-malignant brain tumors, were eligible to participate in the study if the child (aged 2–18 years) was currently or previously receiving cancer or brain tumor care at a local pediatric hematology and oncology clinic, as determined from the medical record or clinic database; children at any stage of treatment or survivorship were eligible. Eligible families were invited to participate by clinical staff if they attended one of the following during the study period: 1) the child’s cancer or brain tumor outpatient visit or inpatient stay at the hospital; 2) a parent-provider advisory board meeting; 3) the hospital support groups for parents; or 4) a childhood cancer survivor reunion. In addition, clinical staff mailed an invitation letter to eligible families in the clinic’s patient database who could not be contacted in-person (either because they did not attend an appointment, advisory board meeting, support group, or reunion during the study period, or could not be approached in person during their visit). Of the 162 families of children with cancer invited to participate in the study, 46 declined participation, 24 did not respond to the invitation, 2 were ineligible, and 8 could not be scheduled to participate within the study timeframe. Eighty (50% of those eligible) ultimately participated. Of those, 9 surveys were missing data and were removed from this analysis, resulting in a final sample of 71 children with cancer and their parents.
Comparison dyads of healthy children ages 2 to 18 and their parents (hereafter referred to as “comparison” group) were recruited by mail from two community-based research registries. Comparison families were eligible to participate if they resided in the greater metropolitan area and if no child in the family had cancer, a brain tumor, a chronic condition, or an activity limitation or special healthcare need; eligibility was confirmed during a telephone screening with trained interviewers. Of the 768 comparison families invited to participate in the study, 344 responded to the invitation. Of these 122 declined to participate, 50 were not eligible based on the health of one of the children in the family, and 31 could not be scheduled for participation before the end of the study period. 141 (41%) eligible comparison families ultimately participated. Six participants were removed from this analysis due to missing data, resulting in a final comparison sample of 135.
Procedures
This study was approved by the Health Sciences Institutional Review Board of the University of Wisconsin-Madison. Written informed consent was obtained from all participants. Parents of children with cancer provided written Health Insurance Portability and Accountability Act Privacy Rule (HIPAA) authorization for abstraction of the child’s medical record. All participating parents completed an in-person interviewer-assisted survey that included items about sociodemographic characteristics and a series of validated self-reported measures. Interviews were completed between September 2008 and July 2009.
Measures
Outcome Measures
Children’s QOL was measured using the Pediatric Quality of Life Index (PedsQL) Generic Core Scale [21]. The PedsQL measures child QOL using 23 questions addressing problems children may have with physical, social, emotional, and school functioning. Problems in the past week are measured on a 5-point Likert scale ranging from 0 (never) to 4 (almost always). Items were reverse coded such that a higher score indicates better QOL, and translated to a scale of 0–100. An overall summary score of child QOL was then calculated as the mean of all items answered. All parents in this study proxy-reported QOL for their child.
Independent Variable
Socioeconomic status was evaluated both as family income and parents’ education. Since income was highly skewed in this sample, the natural log of family income was used in the analyses. Parents’ education level was categorized as high school or less, some college, college degree, or professional or graduate degree.
Mediating Variables
Family functioning was evaluated using the Family Adaptability and Cohesion Evaluation Scale (FACES) IV [22], a measure that operationalizes the circumplex model [23] to evaluate family cohesion, or “the emotional bonding that family members have toward one another,” and flexibility, defined as the “quality and expression of leadership and organization, role relationship, and relationship rules and negotiations” [22, p. 65]. Under the circumplex model, extreme high or low levels of cohesion (enmeshed and disengaged, respectively) and flexibility (chaotic and rigid) are detrimental to family functioning. Parent’s responses to the 52 questions were recorded on a 5-point Likert scale (1=Strongly Disagree, 5=Strongly Agree); scores were used to create Cohesion, Flexibility, and Total Circumplex Ratio Scores. Specifically, the cohesion ratio was calculated by dividing the balanced cohesion score by the average of the disengaged and enmeshment scores, the flexibility ratio was calculated by dividing the balanced flexibility scale score by the average of the rigid and chaotic scores, and the total circumplex ratio was calculated by averaging the balanced cohesion and balanced flexibility scores. The level of balance versus unbalance in the family system was used to assess family functioning. Balance versus unbalance ratio scores further above one indicated better family functioning, whereas ratio scores below one were indicative of problematic family functioning.
Among children with cancer and their parents only, family burden was evaluated using the Impact on the Family Scale [24]. Parents self-reported to what extent their child’s illness impacted their family in four subscales: financial, familial/social, personal strain, and mastery. For this study, a 4-point Likert scale ranging from 1 (not at all) to 4 (a great deal) was used. Subscale scores were created by summing the items in each subscale. A summary score ranging from 24 to 96 was calculated as the sum of the 24 items in the measure. Higher scores indicate greater impact of the illness on the family.
Covariates
Parent/Family Characteristics
Parental age, gender, single parent household status, household composition (number of adults and children in the household), and employment status (full-time work, part-time work, or not working outside the home), were evaluated in the survey. Parents also reported their children’s age and gender.
Child clinical characteristics
Key diagnosis and treatment variables were abstracted from the child’s medical record by a trained and licensed clinician. These factors included type of cancer (leukemia/lymphoma, Central Nervous System (CNS) tumor, or non-CNS tumor), time since diagnosis (years between the date of diagnosis and date of interview), and any type of treatment received (chemotherapy, radiation, surgery, and/or transplant).
Data Analyses
Parent, family, and child characteristics for the full sample and for families of children with cancer only were summarized using descriptive statistics. Cross-tabulations and chi-square analyses were used to compare children with cancer against the comparison group on sociodemographic characteristics of parents and children. T-tests were performed to test for mean differences in household composition, parent and child age, family functioning and burden, and child QOL. The Whitney-Mann U-test was performed to test for mean differences in family income.
Bivariate and multiple linear regression analyses were conducted to evaluate the relationship between SES factors (family income and parental education) and child QOL among both families of children with cancer and comparison families, adjusting for sociodemographic factors. An interaction term was included in this regression to evaluate whether the relationship between income and QOL was different for families of children with cancer than for comparison families. Parsimonious models were constructed for the families of children with cancer only using linear regression. Specifically, single covariates that were statistically significant or impacted the QOL point estimate for income were included in the final models (Model 1); variables tested included parental age, gender, and employment status, household composition (number of adults and children), single parent household status, child age, gender and insurance status, type of cancer, time since diagnosis and treatment status (on active/maintenance treatment or off treatment), and type and number of treatments received. Family functioning and family burden were then added to the models independently (Models 2 and 3, respectively) and jointly (Model 4) to test if these factors reduced the QOL point estimate for income, indicating mediation. The final models report empirical standard errors to correct for unequal variance of the regression residuals. Sobel tests [25] were performed to confirm statistically significant mediation of the relationship between income and QOL by each family factor using the bootstrapping approach recommended by Preacher and Hayes [26]. In order to determine which factors of family burden were influencing the relationship between family income and child QOL, we conducted additional regression analyses using the subscales of the Impact on the Family Scale.
RESULTS
Table 1 summarizes the sociodemographic and family characteristics of families of children with cancer and comparison families. Parents of children with cancer were more likely to be single parents, less educated, and have a lower mean income than comparison parents; children with cancer had significantly worse QOL than comparison children. Additionally, families of children with cancer experienced significantly worse family functioning than comparison families. Among children with cancer, nearly half had been diagnosed with leukemia or lymphoma and an additional 36% of patients experienced a CNS tumor. Time since initial diagnosis ranged from less than a year to more than ten years. Among families of children with cancer, family burden scores ranged from 34 to 81, with a mean of 52.2. Families of children with cancer and comparison families did not differ significantly in age, gender, race/ethnicity, household composition or employment status of the primary caregiver; children with cancer and comparison children did not differ significantly on age or gender.
Table 1.
Characteristics of parents and children with and without cancer
| Full Sample N=206 | Controls N=135 | Cases N=71 | P-value (Controls v Cases) | |
|---|---|---|---|---|
| Parent/Family Characteristics | ||||
| Age, Mean (SD) | 42.6 (5.7) | 43.0 (5.8) | 42.0 (5.7) | 0.25 |
| Gender, % | 0.55 | |||
| Male | 10.2% | 11.1% | 8.5% | |
| Female | 89.8% | 88.9% | 91.6% | |
| Race/Ethnicity, % | 0.29 | |||
| White (non-Hispanic) | 95.1% | 96.3% | 93.0% | |
| Other | 4.9% | 3.7% | 7.0% | |
| Income, Mean (SD) | 110,566 (99,677) | 122,778 (117,067) | 87,346 (45,031) | 0.02 |
| Single Parent Household, % | 8.7% | 5.2% | 15.5% | 0.01 |
| Household Composition, Mean (SD) | ||||
| # Adults | 2.0 (0.4) | 2.0 (0.3) | 2.0 (0.6) | 0.62 |
| # Children | 2.3 (0.9) | 2.3 (0.8) | 2.3 (1.1) | 1.00 |
| Education, % | 0.02 | |||
| High School Graduate or Less | 7.3% | 5.2% | 11.3% | |
| Some College | 24.3% | 19.3% | 33.8% | |
| College Graduate | 38.4% | 43.0% | 29.6% | |
| Professional or Graduate Degree | 30.1% | 32.6% | 25.4% | |
| Employment Status, % | 0.88 | |||
| Employed Full-Time | 47.1% | 48.2% | 45.1% | |
| Employed Part-Time | 38.8% | 38.5% | 39.4% | |
| Not Employed Outside the Home | 14.1% | 13.3% | 15.5% | |
| Family Functioning, Mean (SD) | 2.3 (0.6) | 2.4 (0.6) | 2.1 (0.6) | 0.001 |
| Family Burden§, Mean (SD) | ||||
| Summary Score | -- | -- | 52.2 (11.6) | -- |
| Financial Subscale | -- | -- | 7.8 (3.2) | -- |
| Familial/Social Subscale | -- | -- | 16.2 (6.2) | -- |
| Strain Subscale | -- | -- | 11.2 (4.3) | -- |
| Mastery Subscale | -- | -- | 17.0 (2.2) | -- |
| Child Characteristics | ||||
| Age, Mean (SD) | 10.0 (4.1) | 9.6 (3.8) | 10.7 (4.4) | 0.07 |
| Gender, % | 0.88 | |||
| Male | 51.5% | 51.8% | 50.7% | |
| Female | 48.5% | 48.2% | 49.3% | |
| Quality of Life, Mean (SD) | 79.8 (15.0) | 86.2 (7.7) | 67.5 (17.9) | 0.0001 |
| Clinical Characteristics | ||||
| Type of Cancer§ | ||||
| Leukemia/Lymphoma | -- | -- | 49.3% | -- |
| CNS Tumor | -- | -- | 36.2% | -- |
| Non-CNS Tumor | -- | -- | 14.5% | -- |
| Time Since Diagnosis§ | ||||
| < 1 year | -- | -- | 16.9% | -- |
| 1 year to < 2 years | -- | -- | 15.5% | -- |
| 2 years to < 5 years | -- | -- | 28.2% | -- |
| 5 years to < 10 years | -- | -- | 25.4% | -- |
| 10+ years | -- | -- | 14.1% | -- |
| Treatment Factors§¤ | ||||
| Received Chemotherapy | -- | -- | 87.0% | -- |
| Received Radiation | -- | -- | 18.8% | -- |
| Received Surgery | -- | -- | 49.3% | -- |
| Received Transplant | -- | -- | 5.8% | |
| Number of Treatment Types | -- | -- | 1.6 (0.9) | -- |
Note: “Cases” refers to children with cancer or brain tumors and their families; “controls” refers to healthy children and their families
SD: Standard Deviation
Data only available on cases
Categories not mutually exclusive
Results from bivariate (unadjusted) and multivariate (adjusted for confounders) linear regression analysis are reported in Table 2. In the unadjusted (bivariate) analyses, both cancer status and log family income were significantly associated with child QOL (p<0.001); parent’s education was not significantly associated with child QOL. Multivariable linear regression among both families of children with cancer and comparison families indicated that children with cancer had worse QOL than their healthy counterparts (17.1 points lower, on average, p<0.0001). Table 2 also reveals a significant interaction between cancer status and family income, such that the relationship between income and child QOL is much steeper among families of children with cancer than among comparison families. A 50% increase in income was associated with a 0.3 point increase in child QOL among healthy children, but a 4.3 point increase among children with cancer, controlling for parental education, employment, and child insurance status (p=0.001). A stratified analysis revealed that the effect of log income on child QOL was statistically significant among families of children with cancer (p=0.002) but not among comparison families (p=0.65, data not shown). As such, subsequent analyses were conducted only among the children with cancer.
Table 2.
Unadjusted and adjusted associations between income, sociodemographic factors, and quality of life in children with and without cancer or brain tumors
| Unadjusteda | Adjustedb | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Beta | SE | P-value | Beta | SE | P-value | |
| Intercept | 95.9 | 7.5 | ||||
| Case Status (1=child with cancer/brain tumor) | −18.7 | 2.2 | <.0001 | −17.1 | 2.1 | <.0001 |
| Log Family IncomeŦ | 6.9 | 2.0 | 0.001 | 0.7 | 1.3 | 0.563 |
| Interaction (Case Status by Log Income) | 10.2 | 3.8 | 0.008 | |||
| Parent’s Education | ||||||
| High School Graduate or Less | REF | REF | ||||
| Some College | 0.2 | 4.4 | 0.957 | −2.2 | 4.4 | 0.619 |
| College Graduate | 6.0 | 4.0 | 0.137 | −0.7 | 4.3 | 0.867 |
| Professional or Graduate Degree | 5.8 | 4.2 | 0.167 | −1.1 | 4.3 | 0.798 |
| Parent’s Employment Status | ||||||
| Employed Full-Time | REF | REF | ||||
| Employed Part-Time | −3.3 | 2.3 | 0.145 | −3.4 | 1.7 | 0.049 |
| Not Employed Outside the Home | −0.6 | 3.1 | 0.841 | −0.6 | 2.4 | 0.806 |
| Child’s Insurance Status | ||||||
| Private Insurance | 10.5 | 8.1 | 0.195 | −7.4 | 6.4 | 0.248 |
| Public Insurance | REF | REF | ||||
bivariate analyses;
multivariate analyses, controlling for all variables in the table
Centered at the full-sample mean
SE: Standard Error
Among families of children with cancer only (Table 3), log family income was significantly associated with child QOL such that a 50% increase in income was associated with a 3.9 point increase in child QOL (Model 1), controlling for sociodemographic factors and time since the child’s diagnosis. Other clinical confounders (e.g., type of cancer) and parent’s education were not found to influence the relationships of interest, and were therefore excluded from the final parsimonious models. When family functioning was added to the model (Model 2), this association was attenuated to a 3.6 point increase in QOL per 50% increase in income, and family functioning was independently associated with child QOL. The Sobel test revealed that this attenuation was not statistically significant (data not shown; z=0.5, p=0.60). Alternatively, including family burden in the model (Model 3) reduced the effect of log income on child QOL and eliminated its statistical significance (2.4 point increase in child QOL per 50% increase in income, NS). The Sobel test revealed this attenuation to also be statistically significant (z=2.1, p=0.03). In this model, family burden was independently associated with child QOL. Including both family factors in the model simultaneously (Model 4) also eliminated the statistical significance of the coefficient for log income. In this model, family burden remained statistically significant (p <0.0001) while family functioning did not. In all models, time since the child’s diagnosis and child age were independently associated with child QOL.
Table 3.
Impact of income and family functioning on quality of life among children with cancer or brain tumors
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Beta | SE | P-value | Beta | SE | P-value | Beta | SE | P-value | Beta | SE | P-value | |
| Intercept | 61.9 | 17.4 | 46.0 | 19.3 | 102.6 | 17.6 | 92.8 | 19.0 | ||||
| Log Family IncomeŦ | 9.6 | 4.1 | 0.02 | 8.9 | 4.2 | 0.04 | 5.9 | 3.1 | 0.06 | 5.9 | 3.2 | 0.07 |
| Time Since Diagnosis (Years) | 1.1 | 0.5 | 0.05 | 1.2 | 0.5 | 0.03 | 1.1 | 0.5 | 0.03 | 1.1 | 0.5 | 0.02 |
| Child Age | −1.0 | 0.5 | 0.04 | −1.0 | 0.4 | 0.02 | −1.5 | 0.4 | 0.0001 | −1.5 | 0.4 | 0.0001 |
| Parental Age | 0.4 | 0.4 | 0.27 | 0.5 | 0.4 | 0.24 | 0.5 | 0.3 | 0.13 | 0.5 | 0.3 | 0.13 |
| Child’s Insurance Status | ||||||||||||
| Private Insurance | −5.5 | 9.6 | 0.57 | −5.9 | 9.3 | 0.53 | −4.3 | 6.8 | 0.53 | −4.5 | 6.9 | 0.51 |
| Public Insurance | REF | REF | REF | REF | ||||||||
| Family Functioning (per SD) | -- | -- | -- | 4.2 | 3.4 | 0.05 | -- | -- | -- | 1.9 | 3.0 | 0.30 |
| Family Burden (per SD) | -- | -- | -- | -- | -- | -- | −8.7 | 0.2 | <.0001 | −8.2 | 0.2 | <.0001 |
Centered at the full-sample mean
SD: Standard Deviation; SE: Standard Error
In order to determine which factors of family burden accounted for the relationship between family income and child QOL, we conducted additional regression analysis using the subscales of the Impact on the Family Scale (data available upon request). Results revealed that while financial impact, familial/social impact, and personal strain were all independently significantly associated with child QOL, only the financial subscale significantly attenuated the association between log family income and child QOL (Sobel test: z=2.9, p=0.003). When including the financial subscale only, a 50% increase in income was associated with a 1.4 point increase in QOL and this association was no longer statistically significant.
DISCUSSION
To our knowledge, ours was the first study to explicitly investigate socioeconomic disparities in the QOL of children with cancer and healthy children. Furthermore, we also examined the mediating role of family factors on socioeconomic status and children’s QOL. Our results reveal that significant socioeconomic disparities exist in the QOL of children with cancer, such that children from families with lower incomes have worse QOL than children from wealthier families. Moreover, family burden appears to mediate this relationship, suggesting a potential pathway by which SES affects the QOL of children with cancer. This information will be crucial in developing family-level interventions aimed at improving the health and QOL outcomes of children with cancer and childhood cancer survivors.
Pronounced socioeconomic disparities in child health are prevalent [27–29]; however, little is known about such differences among children with cancer. Our study shows that SES differentially affects the QOL of children with cancer, such that additional income was associated with better QOL of these children. Higher incomes for families of children with cancer may be particularly vital as such resources may facilitate access to adequate health care and reduce children’s exposure to stressful conditions.
Our study highlights an important pathway through which income may affect the QOL of children with cancer, specifically family functioning and burden. To our knowledge, this is the first study to examine these factors as mediators of the SES-QOL relationship among children with cancer. Our findings support previous work indicating that better family functioning is associated with improved QOL in some children with cancer [15; 30] and other conditions [31]. Lower income families may have fewer resources to cope with their child’s cancer, which may increase the burden experienced by these families. Indeed, additional analyses in this study revealed that family financial burden, specifically, was a key factor in mediating the SES-QOL relationship. This is unsurprising, as low-income families may be disproportionately likely to experience financial burden when caring for a child with an activity limitation [32]. The financial stress and burdens associated with caring for a child with cancer may in turn negatively impact child QOL as they reverberate throughout the family.
Although many factors influence QOL among children with cancer and childhood cancer survivors, family-level and contextual factors offer important and often overlooked opportunities for intervention. Although no studies have yet examined the impact of family burden interventions on SES disparities or QOL in children with cancer, evidence from other intervention studies suggests that such approaches may be both feasible and effective at improving family functioning and child depression scores [33], and child well-being [34]. Future research will need to evaluate how family-level interventions impact health and QOL outcomes, particularly among children with cancer.
The findings from this study have important clinical and policy implications. Lower-income families, especially, may benefit from increased support, monitoring, and referrals in the clinical setting. Family-centered care [35; 36] may be one vehicle to help identify and provide support for these families [37]. In addition, tracking family factors and QOL over time may prove essential in identifying emerging problems for families as they arise. Further, psychosocial oncology programs (as described by Kazak [38]) or coordination of care may be especially beneficial at connecting lower-income families with financial, interpersonal, and psychosocial resources that may help improve their family functioning or limit their burden. Finally, implicit class bias among clinicians may negatively influence family-provider communication, care decisions, or outcomes among low-SES families [39] and may negatively influence QOL; as such, provider education that addresses social class bias among clinicians may be important for reducing these disparities.
The SES disparities identified in this paper, if confirmed, suggest that policy may be needed to provide lower-income families with more resources for catastrophic illnesses such as pediatric cancer. Although Medicaid and state-based health-care programs protect the lowest income families, those who are ineligible for this benefit may be underinsured [40]. Improving the provision and coverage of mental health services may also prevent family burden and improve family functioning. This may be especially important in the outpatient setting, where such services may not be as accessible for patients and their families. Further, policies that provide additional resources to these families, such as those supporting the provision of paid time off work, may help mitigate families’ financial burden.
This study has important strengths and limitations. To our knowledge, this is the first study to evaluate the role of family factors in the relationship between SES and QOL among children with cancer. In addition, while most existing studies utilized composite measures of SES or dichotomized their SES variables, this study instead explored these as continuous variables. Due to limitations in the dataset, however, we could not explore other indicators of SES in these families, such as type of employment. Second, child QOL is based on parent reports, which may be influenced by parents’ own health and mental health status. However, parents are often the best source of information about their children, and the instrument used in this study was developed and validated as a parent-reported measure of child QOL [21]. In addition, the cross-sectional design of the study limited our ability to fully evaluate the temporality of these associations (e.g., children with greater impairment or late effects following cancer treatment may create burden for caregivers that necessitates less workforce participation thereby adversely influencing income). Our research questions and findings, however, are supported by theories of the impact of stress in the family system [12–14; 41]. Additionally, we were unable to evaluate subgroups of children in this study, such as those diagnosed with CNS tumors or children at various stages of their treatment and survivorship trajectory. Future work should use longitudinal data and advanced statistical methods to more fully evaluate the interrelationships between SES, family factors, and child QOL, and should evaluate whether these effects differ throughout the cancer treatment and survival trajectory. Finally, this study was conducted in a single metropolitan area and may not be generalizable to other populations. However, as the mean income and education were quite high, the findings from this study are likely conservative. Future studies should utilize a population based and should consider employing a moderated mediation model.
CONCLUSIONS
Not only does this study identify children with cancer from lower-income families as being at a higher risk of poor QOL, it also implicates family burden as a potential mechanism for this association and identifies a potential point of intervention. As such, reducing family burden, potentially brought about by improved monitoring and referral of such families to additional support services, stands to improve QOL and health outcomes for these children and their families.
Acknowledgments
We would like to thank the families who participated in this study. Special thanks go out to Kristin Casey, Beth Severson, and Peter Knight, who were instrumental in study recruitment. The follow-up portion of this study was administered by Survey Research Shared Services of the University of Wisconsin Carbone Cancer Center (UWCCC), with the help of Nathan Jones and Kathy Peck. This research was supported by a grant from the National Institute of Child Health and Human Development (HD049533, W.P. Witt, Principal Investigator and Waisman Center P30 HD03352, M.M. Seltzer, Principal Investigator), UWCCC Investigator Initiated Trial, and the University of Wisconsin Care for Kids Foundation. We would also like to thank the editor of the journal and the three anonymous reviewers for their comments and suggestions that significantly strengthen our paper.
Footnotes
Disclosure: None of the authors has a conflict of interest with this research.
References
- 1.American Cancer Society. Cancer Facts and Figures 2009. Atlanta: American Cancer Society; 2009. [Google Scholar]
- 2.Klassen AF, Anthony SJ, Khan A, Sung L, Klaassen R. Identifying determinants of quality of life of children with cancer and childhood cancer survivors: a systematic review. Support Care Cancer. 2011:1–13. doi: 10.1007/s00520-011-1193-x. [DOI] [PubMed] [Google Scholar]
- 3.Case A, Lubotsky D, Paxson C. Economic Status and Health in Childhood: The Origins of the Gradient. Am Econ Rev. 2002:1308–1334. doi: 10.1257/000282802762024520. [DOI] [PubMed] [Google Scholar]
- 4.Currie J, Stabile M. Socioeconomic status and health: why is the relationship stronger for older children? Am Econ Rev. 2003;93(5):1813–1823. doi: 10.1257/000282803322655563. [DOI] [PubMed] [Google Scholar]
- 5.Lavigne JV, Faier-Routman J. Correlates of psychological adjustment to pediatric physical disorders: A meta-analytic review and comparison with existing models. J Dev Behav Pediatr. 1993;14(2):117–123. [PubMed] [Google Scholar]
- 6.Zebrack BJ, Chesler MA. Quality of life in childhood cancer survivors. Psycho Oncology. 2002;11(2):132–141. doi: 10.1002/pon.569. [DOI] [PubMed] [Google Scholar]
- 7.Sitaresmi MN, Mostert S, Gundy CM, Sutaryo, Veerman AJ. Health-related quality of life assessment in Indonesian childhood acute lymphoblastic leukemia. Health Qual Life Outcomes. 2008;6:96. doi: 10.1186/1477-7525-6-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sung L, Klaassen RJ, Dix D, Pritchard S, Yanofsky R, Dzolganovski B, Almeida R, Klassen A. Identification of paediatric cancer patients with poor quality of life. Br J Cancer. 2009;100(1):82–88. doi: 10.1038/sj.bjc.6604826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Landolt MA, Vollrath M, Niggli FK, Gnehm HE, Sennhauser FH. Health-related quality of life in children with newly diagnosed cancer: a one year follow-up study. Health Qual Life Outcomes. 2006;4:63. doi: 10.1186/1477-7525-4-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Russell KM, Hudson M, Long A, Phipps S. Assessment of health-related quality of life in children with cancer: consistency and agreement between parent and child reports. Cancer. 2006;106(10):2267–2274. doi: 10.1002/cncr.21871. [DOI] [PubMed] [Google Scholar]
- 11.Meeske K, Katz ER, Palmer SN, Burwinkle T, Varni JW. Parent proxy-reported health-related quality of life and fatigue in pediatric patients diagnosed with brain tumors and acute lymphoblastic leukemia. Cancer. 2004;101(9):2116–2125. doi: 10.1002/cncr.20609. [DOI] [PubMed] [Google Scholar]
- 12.Pless IB, Pinkerton P. Chronic childhood disorder: Promoting patterns of adjustment. H. Kimpton; 1975. [Google Scholar]
- 13.Moos RH, editor. Coping with physical illness. Oxford, England: Plenum; 1977. [Google Scholar]
- 14.Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 15.Maurice-Stam H, Grootenhuis MA, Brons PP, Caron HN, Last BF. Psychosocial indicators of health-related quality of life in children with cancer 2 months after end of successful treatment. J Pediatr Hematol Oncol. 2007;29(8):540–550. doi: 10.1097/MPH.0b013e3181256b66. [DOI] [PubMed] [Google Scholar]
- 16.Georgiades K, Boyle MH, Jenkins JM, Sanford M, Lipman E. A multilevel analysis of whole family functioning using the McMaster Family Assessment Device. J Fam Psychol. 2008;22(3):344. doi: 10.1037/0893-3200.22.3.344. [DOI] [PubMed] [Google Scholar]
- 17.Piazza-Waggoner C, Modi AC, Powers SW, Williams LB, Dolan LM, Patton SR. Observational assessment of family functioning in families with children who have type 1 diabetes mellitus. J Dev Behav Pediatr. 2008;29(2):101. doi: 10.1097/DBP.0b013e31815f24ce. [DOI] [PubMed] [Google Scholar]
- 18.Conger RD, Donnellan MB. An interactionist perspective on the socioeconomic context of human development. Annu Rev Psychol. 2007;58:175–199. doi: 10.1146/annurev.psych.58.110405.085551. [DOI] [PubMed] [Google Scholar]
- 19.Hayden LC, Schiller M, Dickstein S, Seifer R, Sameroff S, Miller I, Keitner G, Rasmussen S. Levels of family assessment: I. Family, marital, and parent–child interaction. J Fam Psychol. 1998;12(1):7. [Google Scholar]
- 20.Witt WP, Litzelman K, Wisk LE, Spear HA, Catrine K, Levin N, Gottlieb CA. Stress-mediated quality of life outcomes in parents of childhood cancer and brain tumor survivors: a case-control study. Qual Life Res. 2010;19(7):995–1005. doi: 10.1007/s11136-010-9666-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39(8):800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Olson D. FACES IV and the Circumplex Model: validation study. J Marital Fam Ther. 2011;37(1):64–80. doi: 10.1111/j.1752-0606.2009.00175.x. [DOI] [PubMed] [Google Scholar]
- 23.Olson DH, Gorall DM. Circumplex Model of Marital and Family Systems. In: Walsh F, editor. Normal Family Processes. 3. New York: Guilford; 2003. pp. 514–546. [Google Scholar]
- 24.Stein R, Jessop D. The impact on family scale revisited: further psychometric data. J Dev Behav Pediatr. 2003;24(1):9. [PubMed] [Google Scholar]
- 25.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 26.Preacher K, Hayes A. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior research methods, instruments, & computers: a journal of the Psychonomic Society, Inc. 2004;36(4):717. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 27.Starfield B, Robertson J, Riley AW. Social class gradients and health in childhood. Ambul Pediatr. 2002;2(4):238–246. doi: 10.1367/1539-4409(2002)002<0238:scgahi>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 28.Brooks-Gunn J, Duncan GJ. The effects of poverty on children. Future Child. 1997;7(2):55–71. [PubMed] [Google Scholar]
- 29.Bauman LJ, Silver EJ, Stein RE. Cumulative social disadvantage and child health. Pediatrics. 2006;117(4):1321–1328. doi: 10.1542/peds.2005-1647. [DOI] [PubMed] [Google Scholar]
- 30.Barakat LP, Marmer PL, Schwartz LA. Quality of life of adolescents with cancer: family risks and resources. Health Qual Life Outcomes. 2010;8(1):63. doi: 10.1186/1477-7525-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kulkarni AV, Cochrane DD, McNeely PD, Shams I. Medical, social, and economic factors associated with health-related quality of life in Canadian children with hydrocephalus. J Pediatr. 2008;153(5):689–695. doi: 10.1016/j.jpeds.2008.04.068. [DOI] [PubMed] [Google Scholar]
- 32.Witt WP, Litzelman K, Mandic CG, Wisk LE, Hampton JM, Creswell PD, Gottlieb CA, Gangnon RE. Healthcare-Related Financial Burden among Families in the U.S.: The Role of Childhood Activity Limitations and Income. J Fam Econ Issues. 2011;32(2):308–326. doi: 10.1007/s10834-011-9253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thastum M, Munch-Hansen A, Wiell A, Romer G. Evaluation of a focused short-term preventive counselling project for families with a parent with cancer. Clin Child Psychol Psychiatry. 2006;11(4):529–542. doi: 10.1177/1359104506067875. [DOI] [PubMed] [Google Scholar]
- 34.Kazak AE, Simms S, Barakat L, Hobbie W, Foley B, Golomb V, Best M. Surviving cancer competently intervention program (SCCIP): a cognitive-behavioral and family therapy intervention for adolescent survivors of childhood cancer and their families. Fam Process. 1999;38(2):175–191. doi: 10.1111/j.1545-5300.1999.00176.x. [DOI] [PubMed] [Google Scholar]
- 35.Allen RI, Petr CG. Rethinking Family Centered Practice. Am J Orthopsychiatry. 1998;68(1):4–15. doi: 10.1037/h0080265. [DOI] [PubMed] [Google Scholar]
- 36.Rosenbaum P, King S, Law M, King G, Evans J. Family-Centred Service: A Conceptual Framework and Research Review. Phys Occup Ther Pediatr. 1998;18(1):1–20. [Google Scholar]
- 37.Davis K, Gavidia-Payne S. The impact of child, family, and professional support characteristics on the quality of life in families of young children with disabilities. J Intellect Dev Disabil. 2009;34(2):153–162. doi: 10.1080/13668250902874608. [DOI] [PubMed] [Google Scholar]
- 38.Kazak AE. Children’s Services: Social Policy, Research, & Practice. 2001. Comprehensive care for children with cancer and their families: A social ecological framework guiding research, practice, and policy. [Google Scholar]
- 39.Schnittker J, Bhatt M. The role of income and race/ethnicity in experiences with medical care in the United States and United Kingdom. International journal of health services: planning, administration, evaluation. 2008;38(4):671. doi: 10.2190/HS.38.4.f. [DOI] [PubMed] [Google Scholar]
- 40.Banthin JS, Cunningham P, Bernard DM. Financial burden of health care, 2001–2004. Health Aff (Millwood) 2008;27(1):188. doi: 10.1377/hlthaff.27.1.188. [DOI] [PubMed] [Google Scholar]
- 41.Patterson JM. Families experiencing stress: I. The Family Adjustment and Adaptation Response Model: II. Applying the FAAR Model to health-related issues for intervention and research. Fam Syst Med. 1988;6(2):202. [Google Scholar]