Abstract
BACKGROUND
While prior studies highlight regional variations in out-of-hospital cardiac arrest (OHCA) survival, the underlying reasons remain unknown. We sought to characterize regional variations early and later survival to hospital discharge after OHCA.
METHODS
We studied adult, non-traumatic OHCA treated by 10 regional sites of the Resuscitation Outcomes Consortium (ROC) during 12/01/2005-6/30/2007. We compared 1) early survival (up to one calendar day after arrest), and 2) later conditional survival to hospital discharge (early survivors progressing to eventual hospital discharge) between ROC regional sites.
RESULTS
Among 3,763 VF/VT with complete covariates, site unadjusted early survival varied from 11.3-54.3%, and site unadjusted later survival varied from 33.3-70.5%. Compared with the largest site, adjusted VF/VT survival varied across sites: early survival OR 0.33 (95% CI: 0.17, 0.65) to 2.87 (2.20, 3.73), overall site variation p<0.001; later survival OR 0.29 (0.14, 0.59) to 1.21 (0.73, 2.00), p<0.001. Among 10,879 non-VF/VT with complete covariates, site unadjusted early survival varied from 6.6-14.3%, and site unadjusted later survival varied from 4.5-39.6%. Compared with the largest site, adjusted non-VF/VT survival varied across sites: early survival OR 1.02 (0.63, 1.64) to 2.43 (1.91, 3.12), p<0.001; later survival OR 0.11 (0.01, 0.82) to 1.56 (0.90, 2.70), p=0.02.
CONCLUSIONS
In this prospective multicenter North American series, there were regional disparities in early and later survival after OHCA, suggesting that there are underlying regional differences in out-of-survival must address both out-of-hospital and in-hospital care.
Keywords: cardiopulmonary arrest, emergency medical services, outcomes, post-arrest care
INTRODUCTION
Regional variations in disease patterns have been described for a range of medical conditions including stroke, heart disease, diabetes, obesity and sepsis.1-5 Regional variations may signal potential differences in population characteristics, health behaviors, and access to, delivery or quality of healthcare, among other factors. Nichol, et al. previously described regional variations in out-of-hospital cardiac arrest (OHCA) survival among sites of the Resuscitation Outcomes Consortium (ROC), finding survival to hospital discharge varying from 3.0% to 16.3%.6
To reduce disparities in OHCA survival, one must understand the underlying influences. Survival from OHCA requires timely out-of-hospital care complemented by quality post-arrest care in the hospital. Disparities in early and later survival may offer key perspectives to explain the observed regional variations in overall OHCA survival. For example, survival differences in the early period after cardiac arrest (-e.g., with the first day) may reflect variations in out-of-hospital care such as timely 9-1-1 activation and the provision of bystander CPR. Differences in later survival (-i.e., early survivors who progress to hospital discharge) may reflect differences in post-arrest care quality; for example, timely application of therapeutic hypothermia or cardiac catheterization, or the avoidance of premature withdrawal of care. In a prior effort using a different data set, we showed that while early OHCA survival was associated with out-of-hospital factors such as presenting ECG rhythm and resuscitation drug use; later long-term survival was associated with patient demographics such as age and sex.7 These perspectives could be useful to motivate or guide community-wide efforts to improve OHCA care and outcomes.
In an effort to characterize differences in out-of-hospital versus in-hospital care, in this study we sought to describe regional variations in early and later survival after OHCA.
MATERIALS AND METHODS
Study Design
This study was an analysis of prospectively collected OHCA data from the ROC Epistry - Cardiac Arrest (“Epistry”).8 Data for the ROC Epistry were collected in conformance with United States Department of Health and Human Services regulations for the protection of human subjects and provisions of the Canadian Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans. Additional reviews and approvals were obtained from the institutional review boards and research ethics boards for each community.
Setting
The ROC is a North American multicenter clinical trial network designed to conduct out-of-hospital interventional and clinical research in the areas of cardiac arrest and traumatic injury. Regional coordinating centers participating in the ROC included the following communities: Birmingham, AL; Dallas, TX; Des Moines, IA; Milwaukee, WI; Pittsburgh, PA; Portland, OR; San Diego, CA; Seattle/King County, WA; Vancouver, British Columbia, Canada; Ottawa, Ontario, Canada; and Toronto and adjacent regions, Ontario, Canada. In addition, a data and coordinating center was based in Seattle. Over 264 emergency medical services (EMS) agencies and 287 receiving hospitals in the consortium participated in the ROC Epistry - Cardiac Arrest project, a population based registry of consecutive cases of cardiac arrest at all ROC sites.8
Methods of Measurement – Data Collection
The objective of the ROC Epistry – Cardiac Arrest is to create a population-based registry characterizing OHCA occurring in the communities of 9 ROC sites.8, 9 All ROC sites except San Diego contributed to ROC Epistry – Cardiac Arrest. Study personnel at each site determined clinical details of each OHCA through review of dispatch logs, EMS patient care records, defibrillator files, and hospital and public death records. Data collected included information regarding the prehospital response, patient demographics, clinical information, prehospital interventions, prehospital disposition, hospital information and outcomes. Data collection and reporting methods adhered to Utstein standards.10 .
Selection of Participants
This study included all adult (≥18 years old), non-traumatic OHCA receiving resuscitation efforts by a participating ROC EMS agency during December 1, 2005 through June 30, 2007. Resuscitation efforts included individuals receiving attempts at external defibrillation by lay responders or EMS personnel, or chest compressions by EMS personnel. We excluded children (age<18 years), OHCA due to blunt, burn, or penetrating trauma, and those not receiving any resuscitation interventions.
Outcomes
The natural course of OHCA includes a large number of early deaths followed by a smaller number of later deaths.7 Therefore, the primary outcomes of this analysis were 1) early survival (defined as survival at least one calendar day after episode date) and 2) later survival (defined as early survivors who progressed to hospital discharge). The ROC Epistry – Cardiac Arrest data defined survival time in terms of calendar days; we could not ascertain shorter time intervals such as hours. By these definitions, early survivors were those who survived for at least 24-48 hours after the arrest event. For example, an individual suffering a cardiac arrest on a Monday would have to survive to at least Wednesday to be classified as an early survivor.
Data Analyses
We determined the rates of early and later OHCA survival for each ROC site, stratifying by initial cardiac arrest ECG rhythm. We classified initial ECG rhythm as ventricular fibrillation/pulseless ventricular tachycardia (VF/VT) and non-VF/VT (pulseless electrical activity or asystole). If an automated external defibrillator was used, we defined delivery of a shock as VF/VT and no shock as non-VF/VT. To compare the relative survival proportions between the sites, we used multivariable logistic regression, creating separate models for each outcome and initial ECG rhythm. We fit each model using the largest enrolling site as the reference, adjusting for age, sex, public location, witnessed arrest, bystander CPR or AED use, and EMS response time (time from 9-1-1 call to EMS arrival). To assess overall site effects we conducted likelihood-ratio tests with nine degrees of freedom for each model.
We conducted a series of sensitivity analyses. Individuals with missing discharge disposition were excluded from the primary analysis. We repeated the analysis classifying all cases with missing disposition as alive and subsequently as dead. We also repeated the analysis using Generalized Estimating Equations (GEE) to account for clustering by EMS agency. Because almost 39% of cardiac arrest cases were pronounced dead in the field, we could not cluster by hospital. We conducted all analyses using R (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
During the study period there were 15,765 adult, non-traumatic OHCA. These patients included 3,957 (25.9%) VF/VT, 11,336 (71.9%) non-VF/VT and 472 (3.0%) with unknown initial ECG rhythm. (Table) Public OHCA location, bystander and EMS witnessed arrest, bystander CPR and AED use, and initial ECG rhythm varied across sites. Complete outcome and covariate data were available for 3,763 VF/VT and 10,879 non-VF/VT patients. OHCA included in the analysis encompassed 219 EMS agencies and 216 hospitals.
TABLE.
Characteristics of out-of-hospital cardiac arrest in the Resuscitation Outcomes Consortium, stratified by site. Sites listed in order of descending case volume. Includes only cases without missing values for all characteristics.
| Characteristic | Site 1 (N=3,633) |
Site 2 (N=2,893) |
Site 3 (N=2,155) |
Site 4 (N=1,532) |
Site 5 (N=1,386) |
Site 6 (N=1,224) |
Site 7 (N=1,123) |
Site 8 (N=765) |
Site 9 (N=662) |
Site 10 (N=392) |
TOTAL (N=15,765) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years, mean) | 69.8 | 67.9 | 67.6 | 64.6 | 66.8 | 64.7 | 63.7 | 66.1 | 66.2 | 64.5 | 67.1 |
| Median (IQR) | 73 (59,82) | 70 (57,80) | 70 (57,80) | 65 (52,79) | 68 (55,80) | 65 (53,78) | 63 (51,77) | 67 (55,79) | 68 (54,79) | 65 (53,79) | 69(55,80) |
| Sex (male, %) | 62.6 | 65.4 | 68.9 | 58.2 | 63.4 | 64.1 | 58.9 | 64.4 | 60.8 | 57.4 | 63.4 |
| Public Location (%) | 15.1 | 13.7 | 19.6 | 12.5 | 19.6 | 17.2 | 13.4 | 17.1 | 14.5 | 14.4 | 15.7 |
| Witnessed Arrest | |||||||||||
| Not Witnessed (%) | 51.0 | 49.6 | 44.6 | 27.9 | 51.8 | 23.9 | 51.6 | 39.9 | 39.9 | 20.2 | 43.9 |
| EMS Witnessed (%) | 9.4 | 10.1 | 9.5 | 4.7 | 9.5 | 4.5 | 11.7 | 13.1 | 6.8 | 12.0 | 9 |
| Bystander Witnessed (%) | 38.5 | 39.5 | 44.7 | 19.5 | 37.3 | 50.1 | 36.7 | 40.1 | 41.8 | 44.4 | 38.7 |
| Unknown (%) | 1.1 | 0.8 | 1.2 | 48.0 | 1.4 | 21.6 | 0.0 | 6.9 | 11.5 | 23.5 | 8.4 |
| Bystander Resuscitation | |||||||||||
| CPR (%) | 28.0 | 26.9 | 37.6 | 19.5 | 49.1 | 45.4 | 21.8 | 31.7 | 36.9 | 25.8 | 31.5 |
| AED Use (%) | 1.4 | 2.0 | 1.2 | 1.4 | 3.4 | 3.2 | 2.3 | 6.0 | 8.3 | 3.1 | 2.4 |
| Unknown status (%) | 1.5 | 1.6 | 1.5 | 52.3 | 1.9 | 24.3 | 0.0 | 15.2 | 14.7 | 41.3 | 10.3 |
| Initial Rhythm (VF/VT, %)* | 22.2 | 26.4 | 31.7 | 16.6 | 31.0 | 34.8 | 21.1 | 28.2 | 22.1 | 28.6 | 25.9 |
| EMS Response Time | |||||||||||
| (9-1-1 to arrival on-scene; minutes, mean) |
6.6 | 6 | 7.5 | 5.9 | 5.3 | 5.2 | 4.4 | 5.1 | 6.5 | 7.2 | 6.1 |
| Median (IQR) | 6 (5,7) | 6 (4,7) | 6 (5,8) | 5 (4,7) | 5 (4,6) | 5 (4,6) | 4 (3,5) | 4 (3,6) | 6 (4,8) | 6 (4,8) | 5 (4,7) |
Based upon those with known initial ECG rhythm (total n = 15,293). IQR=interquartile range. EMS=Emergency Medical Services. CPR=cardiopulmonary resuscitation. AED=automated external defibrillator. VF/VT = ventricular fibrillation or pulseless ventricular tachycardia.
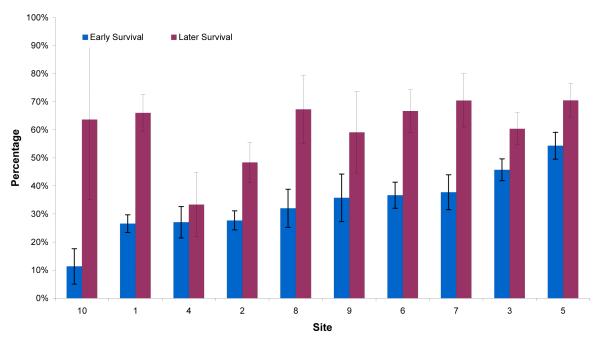
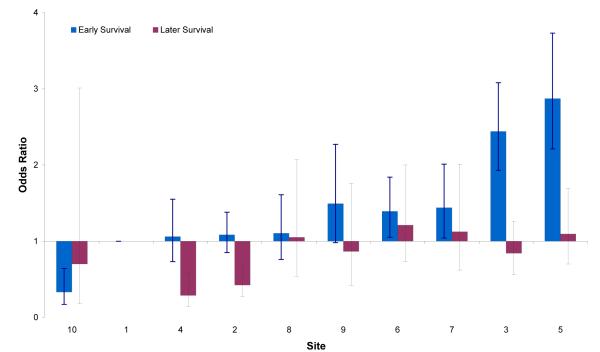
For VF/VT OHCA, unadjusted site-level survival ranged from 11.3-54.3% (median 33.9%) for early survival and 33.3-70.5% (median 64.8%) for later survival. (Figure 1, Appendix) After adjusting for Utstein confounders (age, sex, public location, witnessed arrest, bystander CPR or AED use, and the time from 9-1-1 call to EMS arrival), there were significant site-level variations in early and later survival after VF/VT OHCA (p<0.001 for both). (Figure 2) Of note were unique divergent site variations. While sites 3 and 5 demonstrated higher adjusted early survival, they also exhibited later adjusted survival similar to other sites. In contrast, while sites 2 and 4 demonstrated early adjusted survival similar to other sites, they exhibited slightly lower adjusted later survival.
FIGURE 1.
Unadjusted survival after ventricular fibrillation or pulseless ventricular tachycardia cardiac arrest. Stratified by Resuscitation Outcomes Consortium site. Early survival includes individuals surviving up to one calendar day after cardiac arrest. Later survival includes early survivors progressing to hospital discharge. Sites listed in order of early survival.
FIGURE 2.
Adjusted survival after ventricular fibrillation or pulseless ventricular tachycardia cardiac arrest. Stratified by Resuscitation Outcomes Consortium site. Early survival includes individuals surviving up to one calendar day after cardiac arrest. Later survival includes early survivors progressing to hospital discharge. Sites listed in order of unadjusted early survival to facilitate comparison with Figure 1. Odds ratios referenced to largest site (site 1) and adjusted for age, sex, public location, witnessed arrest, bystander CPR, bystander AED use and EMS response time. Adjusted survival varied across sites for early (p<0.001) and later survival (p<0.001). Detailed odds ratios listed in the Appendix.
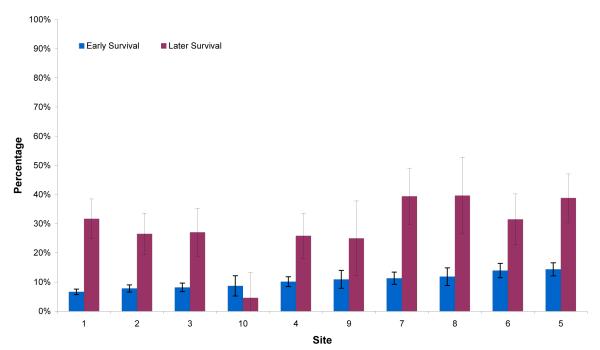
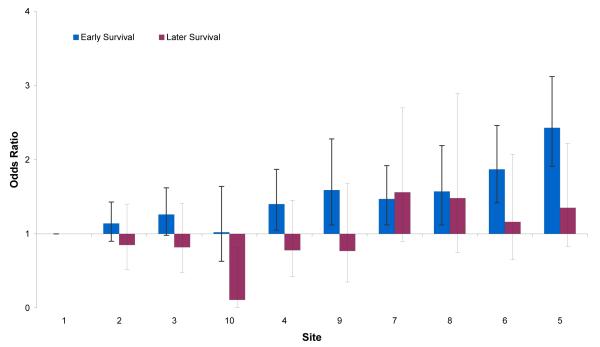
For non-VF/VT OHCA, unadjusted site-level survival ranged from 6.6-14.3% (median 10.5%) for early survival and 4.5-39.6% (median 29.3%) for later survival. (Figure 3, Appendix) After adjusting for Utstein confounders, there were significant site-level variations early (p<0.001) and later survival (p=0.02) after VF/VT OHCA. (Figure 4) There were site-level related discordant observations in the non-VF/VT group as well. While site 5 demonstrated slightly higher adjusted early survival than select sites, later adjusted survival was similar to other sites.
FIGURE 3.
Unadjusted survival after non-ventricular fibrillation/ventricular tachycardia cardiac arrest. Stratified by Resuscitation Outcomes Consortium site. Early survival includes individuals surviving up to one calendar day after cardiac arrest. Later survival includes early survivors progressing to hospital discharge. Sites listed in order of early survival.
FIGURE 4.
Adjusted survival after non-ventricular fibrillation/ventricular tachycardia cardiac arrest. Stratified by Resuscitation Outcomes Consortium site. Early survival includes individuals surviving up to one calendar day after cardiac arrest. Later survival includes early survivors progressing to hospital discharge. Sites listed in order of unadjusted early survival in order to facilitate comparison with Figure 3. Odds ratios referenced to largest site (site 1) and adjusted for age, sex, public location, witnessed arrest, bystander CPR, bystander AED use and EMS response time. Adjusted survival varied across sites for early (p<0.001) and later survival (p=0.02). Detailed odds ratios listed in the Appendix.
When repeating the analysis using GEE to account for clustering by EMS agency, we observed largely similar results in site-level odds ratios. There were 151 individuals (1.0%) with unknown discharge outcomes, varying from 0.1%-6.0% across sites. When repeating the analysis classifying cases with missing outcome as either 1) all alive or 2) all dead, we observed similar site-level variations in early and later survival. However, while reclassification in this manner had minimal impact for most sites, it did considerably change the estimates for site 10, which exhibited missing outcome for approximately 6%. In this latter site, re-classification of missing cases in the VF/VT cohort as “all-dead” would reduce adjusted later survival from OR 0.70 (95% CI: 0.18, 2.77) to OR 0.18 (0.06, 0.53). Similarly re-classification of missing cases in the non-VF/VT cohort as “all-alive” would increase adjusted early survival from OR 1.02 (0.63, 1.64) to OR 1.50 (1.00, 2.25), and adjusted later survival from OR 0.11 (0.01, 0.82) to OR 1.23 (0.56, 2.71).
DISCUSSION
In this study we modeled OHCA survival as consisting of two successive elements: early survival (defined as surviving at least one calendar day from the event), followed by later survival (defined as early survivors who progress to hospital discharge). Under this conceptual model. early survival may reflect out-of-hospital and Emergency Department care, and later survival may reflect hospital-based post-arrest care. An analysis limited to overall OHCA survival cannot differentiate the relative influences of each component. In addition to offering insights to partially explain regional variations in OHCA survival, our findings suggest potential target areas for community-level OHCA care improvement.
The notion of community-based OHCA care encompassing coordinated care among multiple EMS units and hospitals is plausible and supported by current models.11, 12 Early arrest recognition, bystander cardiopulmonary resuscitation chest compressions and use of AED, “9-1-1” activation, and quality EMS care are important components for improved OHCA survival.13 Recent attention has focused on the role of structured post-arrest care and the effect on OHCA outcomes, including the provision of therapeutic hypothermia, early cardiac catheterization and appropriate neurologic prognostication.14 The complexity of hospital care has spurred some communities to propose regionally-organized post-arrest care, directing the EMS transport or inter-facility transfer of OHCA patients to specially trained, equipped and experienced post-cardiac arrest care centers.11, 12, 15 The significant regional disparities in survival demonstrated in this study may be the first step towards quantifying the relative contributions of optimized community-based out-of-hospital care and high quality hospital-based post-arrest care.
For example, in the VF/VT subset, sites 3 and 5 exhibited higher early survival but similar later survival relative to site 1. Thus, one might attribute the higher overall survival in these communities to superior systems of early out-of-hospital and Emergency Department resuscitative care rather than to the quality or nature of hospital post-arrest care. In contrast, sites 2 and 4 exhibited lower later survival, suggesting that increased emphasis on hospital post-arrest care may present greater opportunities for improving overall survival.
In contrast, in the non-VF/VT subset, there were smaller differences in later survival across sites. The latter suggests either less practice variation across ROC sites or the limited opportunity for changes in-hospital care to influence the outcomes of these patients. These observations should not be surprising as patients with initial non-VF/VT rhythms tend to have poorer prognoses compared with those with initial VF/VT.16 Furthermore, there are fewer therapeutic options for non-VF/VT OHCA.
We emphasize that our study is intended to illustrate a conceptual framework and to generate hypotheses regarding OHCA care. Replication with an independent data set is important to validate the analytic approach. These results do not indicate the specific EMS or hospital-based interventions necessary for improving OHCA outcomes. Examples of community-based OHCA care improvement include optimizing the placement of AEDs and EMS units, expanding or standardizing the use of hospital therapeutic hypothermia, and leveraging EMS resources to optimize access to designated post-arrest care centers, among others.11, 17 However, our study affirms the influence of both early and later care upon overall OHCA survival and the importance of community focus on both components. This interpretation is consistent with current resuscitation guidelines emphasizing the coordination of the continuum between out-of-hospital and in-hospital OHCA care.18
LIMITATIONS
The current data originate from a large, established multi-center OHCA network generalizeable across 264 EMS services and 287 hospitals from the US and Canada providing data for the years 2005-2007 and represent the best data available. Our definition of early survival included up to one-calendar day after the cardiac arrest, a period which may have included a time period as short as 24 hours to as long as 48 hours. The ROC Epistry – Cardiac Arrest data could not define shorter time intervals. It is reassuring to note that of the 13,906 early deaths in the analysis, 93.8% occurred on the same calendar day as the cardiac arrest; only 806 (6.2%) deaths occurred on the subsequent calendar day.
While this analysis indicated disparities in early vs. later OHCA survival, we could not identify the specific elements of out-of-hospital or in-hospital care that affected outcomes. For example, we could not draw associations with chest compression fraction or use of therapeutic hypothermia and functional neurological survival as these data points were not collected in ROC Epistry – Cardiac Arrest. Due to limitations with the ROC Epistry – Cardiac Arrest data we were unable to determine associations with comorbidities or other medical conditions and detailed patient characteristics such as race (missing in over 60%), family risk factors, current drug therapies, past medical history, or presenting complaint of symptoms prior to cardiac arrest.
We were unable to account for differences in the initiation and termination of resuscitation or differences in practice pertaining to withdrawal of life sustaining therapy, which may vary significantly across ROC sites and have influenced both early and later survival.19 Because the ROC Epistry – Cardiac Arrest did not examine survival beyond hospital discharge nor neurological or functional outcome, we analyzed survival to hospital discharge only, without considering other endpoints such as 30-day or 6-month survival.
Some sites were relatively small, limiting the utility of inferences for these locations. There were considerable site differences in missingness for some important Utstein variables that predict outcome, such as bystander CPR and witnessed versus unwitnessed arrest. While multiple imputation is a common method for handling missing observations, there were systematic differences in the percent of missing outcomes across sites, violating the missing-at-random assumption necessary for this technique.20
CONCLUSION
We observed regional disparities in early and later survival after out-of-hospital cardiac arrest. These observations suggest underlying regional differences in out-of-hospital care and post-arrest care. Community efforts to improve OHCA survival must address both early out-of-hospital as well as later in-hospital elements of care.
Acknowledgments
FINANCIAL SUPPORT The ROC is supported by a series of cooperative agreements to nine regional clinical centers and one Data Coordinating Center (5U01 HL077863-University of Washington Data Coordinating Center, HL077866-Medical College of Wisconsin, HL077867-University of Washington, HL077871-University of Pittsburgh, HL077872-St. Michael’s Hospital, HL077873-Oregon Health and Science University, HL077881-University of Alabama at Birmingham, HL077885-Ottawa Health Research Institute, HL077887-University of Texas SW Medical Center/Dallas, HL077908-University of California San Diego) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research & Material Command, The Canadian Institutes of Health Research (CIHR) - Institute of Circulatory and Respiratory Health, Defence Research and Development Canada and the Heart, Stroke Foundation of Canada and the American Heart Association. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute or the National Institutes of Health.
APPENDIX.
Early vs. later survival to hospital discharge, stratified by site. Early survival includes individuals surviving up to one calendar day after cardiac arrest. Later survival includes early survivors progressing to hospital discharge. Odds ratios referenced to largest site and adjusted for age, sex, public location, witnessed arrest, bystander CPR, and bystander AED use. Based upon those with known initial ECG rhythm and with complete covariates.
| Early Survival |
Later Survival |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted Model |
Site Effect |
Adjusted Model |
Site Effect |
Unadjusted Model |
Site Effect |
Adjusted Model |
Site Effect |
|||||||
| Site | N | OR | 95% CI | p-value | OR | 95% CI | p-value | N | OR | 95% CI | p-value | OR | p-value | |
| Initial ECG VF/VT | ||||||||||||||
| 1 | 764 | (ref) | <0.001 | (ref) | <0.001 | 202 | (ref) | <0.001 | (ref) | <0.001 | ||||
| 2 | 671 | 1.06 | (0.84, 1.34) | 1.08 | (0.85, 1.38) | 186 | 0.48 | (0.32, 0.73) | 0.42 | (0.27, 0.66) | ||||
| 3 | 623 | 2.33 | (1.86, 2.92) | 2.44 | (1.93, 3.08) | 285 | 0.78 | (0.54, 1.14) | 0.84 | (0.56, 1.26) | ||||
| 4 | 244 | 1.02 | (0.74, 1.42) | 1.06 | (0.73, 1.54) | 66 | 0.26 | (0.14, 0.46) | 0.29 | (0.14, 0.59) | ||||
| 5 | 418 | 3.28 | (2.56, 4.22) | 2.87 | (2.20, 3.73) | 227 | 1.23 | (0.82, 1.84) | 1.09 | (0.70, 1.69) | ||||
| 6 | 409 | 1.60 | (1.24, 2.07) | 1.39 | (1.05, 1.84) | 150 | 1.03 | (0.66, 1.61) | 1.21 | (0.73, 2.00) | ||||
| 7 | 233 | 1.68 | (1.23, 2.29) | 1.44 | (1.04, 2.01) | 88 | 1.23 | (0.71, 2.11) | 1.12 | (0.62, 2.01) | ||||
| 8 | 181 | 1.30 | (0.92, 1.85) | 1.10 | (0.76, 1.60) | 58 | 1.06 | (0.57, 1.97) | 1.05 | (0.54, 2.07) | ||||
| 9 | 123 | 1.54 | (1.03, 2.30) | 1.49 | (0.98, 2.27) | 44 | 0.74 | (0.38, 1.45) | 0.86 | (0.42, 1.76) | ||||
| 10 | 97 | 0.35 | (0.18, 0.68) | 0.33 | (0.17, 0.65) | 11 | 0.90 | (0.26, 3.18) | 0.70 | (0.18, 2.77) | ||||
| Total | 3,763 | 1,318 | ||||||||||||
| Initial ECG non-VF/VT | ||||||||||||||
| 1 | 2,712 | (ref) | <0.001 | (ref) | <0.001 | 180 | (ref) | <0.001 | (ref) | 0.02 | ||||
| 2 | 1,891 | 1.19 | (0.95, 1.49) | 1.14 | (0.90, 1.43) | 147 | 0.78 | (0.48, 1.26) | 0.85 | (0.52, 1.40) | ||||
| 3 | 1,361 | 1.25 | (0.98, 1.60) | 1.26 | (0.98, 1.62) | 111 | 0.80 | (0.47, 1.35) | 0.82 | (0.48, 1.41) | ||||
| 4 | 1,223 | 1.59 | (1.25, 2.02) | 1.40 | (1.05, 1.87) | 124 | 0.75 | (0.45, 1.25) | 0.78 | (0.42, 1.45) | ||||
| 5 | 934 | 2.36 | (1.86, 2.98) | 2.43 | (1.91, 3.12) | 134 | 1.37 | (0.86, 2.19) | 1.35 | (0.83, 2.22) | ||||
| 6 | 776 | 2.27 | (1.77, 2.93) | 1.87 | (1.42, 2.46) | 108 | 0.99 | (0.59, 1.66) | 1.16 | (0.65, 2.07) | ||||
| 7 | 877 | 1.79 | (1.38, 2.32) | 1.47 | (1.12, 1.92) | 99 | 1.40 | (0.84, 2.34) | 1.56 | (0.90, 2.70) | ||||
| 8 | 447 | 1.89 | (1.37, 2.62) | 1.57 | (1.12, 2.19) | 53 | 1.42 | (0.75, 2.67) | 1.48 | (0.75, 2.89) | ||||
| 9 | 404 | 1.72 | (1.21, 2.43) | 1.59 | (1.12, 2.28) | 44 | 0.72 | (0.34, 1.52) | 0.77 | (0.35, 1.68) | ||||
| 10 | 254 | 1.33 | (0.84, 2.12) | 1.02 | (0.63, 1.64) | 22 | 0.10 | (0.01, 0.78) | 0.11 | (0.01, 0.82) | ||||
| Total | 10,879 | 1,022 | ||||||||||||
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICTS OF INTEREST The authors declare no conflicts of interest.
Contributor Information
Henry E. Wang, Department of Emergency Medicine, University of Alabama at Birmingham, Birmingham, Alabama.
Sean M. Devlin, Department of Epidemiology and Biostatistics, Memorial Sloan-Kettering Cancer Center, New York, NY.
Gena K. Sears, The Clinical Trials Center, Department of Biostatistics, University of Washington, Seattle, Washington.
Christian Vaillancourt, Department of Emergency Medicine and Ottawa Hospital Research Institute, University of Ottawa, Ottawa, Ontario.
Laurie J. Morrison, Rescu, Keenan Research Centre, Li Ka Shing Knowledge Institute, St Michael’s Hospital, Division of Emergency Medicine, Department of Medicine, University of Toronto, Toronto, Ontario.
Myron Weisfeldt, Department of Medicine, Johns Hopkins University, Baltimore, Maryland.
Clifton W. Callaway, Department of Emergency Medicine, University of Pittsburgh, Pittsburgh, Pennsylvania.
REFERENCES
- 1.Wang HE, Devereaux RS, Yealy DM, Safford MM, Howard G. National variation in united states sepsis mortality: A descriptive study. Int J Health Geogr. 2010;9:9. doi: 10.1186/1476-072X-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howard G. Why do we have a stroke belt in the southeastern united states? A review of unlikely and uninvestigated potential causes. Am J Med Sci. 1999;317:160–167. doi: 10.1097/00000441-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Ford ES, Mokdad AH, Giles WH, Galuska DA, Serdula MK. Geographic variation in the prevalence of obesity, diabetes, and obesity-related behaviors. Obesity Research. 2005;13:118–122. doi: 10.1038/oby.2005.15. [DOI] [PubMed] [Google Scholar]
- 4.Pickle LW, Gillum RF. Geographic variation in cardiovascular disease mortality in us blacks and whites. Journal of the National Medical Association. 1999;91:545–556. [PMC free article] [PubMed] [Google Scholar]
- 5.Pickle LW, Mungiole M, Gillum RF. Geographic variation in stroke mortality in blacks and whites in the united states. Stroke. 1997;28:1639–1647. doi: 10.1161/01.str.28.8.1639. [DOI] [PubMed] [Google Scholar]
- 6.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang HE, Min A, Hostler D, Chang CC, Callaway CW. Differential effects of out-of-hospital interventions on short- and long-term survival after cardiopulmonary arrest. Resuscitation. 2005;67:69–74. doi: 10.1016/j.resuscitation.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 8.Morrison LJ, Nichol G, Rea TD, Christenson J, Callaway CW, Stephens S, Pirrallo RG, Atkins DL, Davis DP, Idris AH, Newgard C. Rationale, development and implementation of the resuscitation outcomes consortium epistry-cardiac arrest. Resuscitation. 2008;78:161–169. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davis DP, Garberson LA, Andrusiek DL, Hostler D, Daya M, Pirrallo R, Craig A, Stephens S, Larsen J, Drum AF, Fowler R. A descriptive analysis of emergency medical service systems participating in the resuscitation outcomes consortium (roc) network. Prehosp Emerg Care. 2007;11:369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- 10.Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, Bossaert L, Delooz HH, Dick WF, Eisenberg MS, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: The Utstein style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991;84:960–975. doi: 10.1161/01.cir.84.2.960. [DOI] [PubMed] [Google Scholar]
- 11.Lick CJ, Aufderheide TP, Niskanen RA, Steinkamp JE, Davis SP, Nygaard SD, Bemenderfer KK, Gonzales L, Kalla JA, Wald SK, Gillquist DL, Sayre MR, Osaki Holm SY, Oakes DA, Provo TA, Racht EM, Olsen JD, Yannopoulos D, Lurie KG. Take heart america: A comprehensive, community-wide, systems-based approach to the treatment of cardiac arrest. Crit Care Med. 2011;39:26–33. doi: 10.1097/CCM.0b013e3181fa7ce4. [DOI] [PubMed] [Google Scholar]
- 12.Kajino K, Iwami T, Daya M, Nishiuchi T, Hayashi Y, Kitamura T, Irisawa T, Sakai T, Kuwagata Y, Hiraide A, Kishi M, Yamayoshi S. Impact of transport to critical care medical centers on outcomes after out-of-hospital cardiac arrest. Resuscitation. 2010;81:549–554. doi: 10.1016/j.resuscitation.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 13.Stiell IG, Wells GA, Field B, Spaite DW, Nesbitt LP, De Maio VJ, Nichol G, Cousineau D, Blackburn J, Munkley D, Luinstra-Toohey L, Campeau T, Dagnone E, Lyver M, Suppo OPAL Advanced cardiac life support in out-of-hospital cardiac arrest. New Engl J Med. 2004;351:647–656. doi: 10.1056/NEJMoa040325. [DOI] [PubMed] [Google Scholar]
- 14.Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabrielli A, Silvers SM, Zaritsky AL, Merchant R, Vanden Hoek TL, Kronick SL. Part 9: Post-cardiac arrest care 2010 american heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S768–S786. doi: 10.1161/CIRCULATIONAHA.110.971002. [DOI] [PubMed] [Google Scholar]
- 15.Donnino MW, Rittenberger JC, Gaieski D, Cocchi MN, Giberson B, Peberdy MA, Abella BS, Bobrow BJ, Callaway C. The development and implementation of cardiac arrest centers. Resuscitation. 2011;82:974–978. doi: 10.1016/j.resuscitation.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 16.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: A systematic review and meta-analysis. Circulation. Cardiovascular quality and outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 17.Stiell IG, Wells GA, Field BJ, Spaite DW, De Maio VJ, Ward R, Munkley DP, Lyver MB, Luinstra LG, Campeau T, Maloney J, Dagnone E. Improved out-of-hospital cardiac arrest survival through the inexpensive optimization of an existing defibrillation program: Opals study phase ii. Ontario prehospital advanced life support. JAMA. 1999;281:1175–1181. doi: 10.1001/jama.281.13.1175. [DOI] [PubMed] [Google Scholar]
- 18.Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabrielli A, Silvers SM, Zaritsky AL, Merchant R, Vanden Hoek TL, Kronick SL. Part 9: Post-cardiac arrest care: 2010 american heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S768–786. doi: 10.1161/CIRCULATIONAHA.110.971002. [DOI] [PubMed] [Google Scholar]
- 19.Lin S, Morrison LJ, Brooks SC. Development of a data dictionary for the strategies for post arrest resuscitation care (sparc) network for post cardiac arrest research. Resuscitation. 2011;82:419–422. doi: 10.1016/j.resuscitation.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 20.Newgard CD, Haukoos JS. Advanced statistics: Missing data in clinical research--part 2: Multiple imputation. Acad Emerg Med. 2007;14:669–678. doi: 10.1197/j.aem.2006.11.038. [DOI] [PubMed] [Google Scholar]