Abstract
Objective
To examine in a pilot cohort factors associated with functional outcome at discharge and three-month follow-up following discharge from inpatient rehabilitation in children with severe traumatic brain injury (TBI) who entered rehabilitation with the lowest level of functional skills.
Participants
39 children and adolescents (3 to 18 years) who sustained a severe TBI and had the lowest possible rating at rehabilitation admission on the Functional Independence Measure for Children (WeeFIM total score = 18).
Methods
Retrospective review of data collected as part of routine clinical care.
Results
At discharge, 59% of the children were partially dependent for basic activities while 41% remained dependent for basic activities. Initial Glasgow Coma Scale score, time to follow commands, and time from injury to rehabilitation admission were correlated with functional status at discharge. Time to follow commands and time from injury to rehabilitation admission were correlated with functional status at three-month follow-up. Changes in functional status during the first few weeks of admission were associated with functional status at discharge and follow-up.
Conclusion
Even children with the most severe brain injuries, who enter rehabilitation completely dependent for all daily activities, have the potential to make significant gains in functioning by discharge and in the following few months. Assessment of functional status early in the course of rehabilitation contributes to the ability to predict outcome from severe TBI.
Keywords: traumatic brain injury, children and adolescents, functional independence measure, outcome, rehabilitation
Early, accurate prediction of outcome following pediatric traumatic brain injury (TBI) is important for many aspects of inpatient rehabilitation care including discharge planning for home management, educational programming, community re-entry, long-term treatment planning, insurance authorization, and family adjustment and coping. Planning is particularly crucial for those children who are totally dependent for all aspects of care at the time of admission to rehabilitation, yet very little is known about predicting outcome in this group. Functional outcome is known to vary widely across the spectrum of children with TBI who require inpatient rehabilitation care1, and although a number of predictors of outcome have been identified, no combination adequately accounts for the observed variability in outcomes.
Several clinical measures of injury severity have been found to be reliable predictors of functional outcome in children with TBI who require inpatient rehabilitation. Studies have documented that higher early Glasgow Coma Scale (GCS) score predicts better outcome in children with TBI who require inpatient rehabilitation2,3. Time to follow commands (TFC) was the best predictor of overall functional outcome as measured by the Functional Independence Measure for Children (WeeFIM®) at discharge and follow-up in a sample of children with moderate to severe TBI requiring inpatient rehabilitation3. Shorter time from injury to rehabilitation admission has also been associated with shorter inpatient stays and better functional outcomes at discharge1. Time from injury to rehabilitation admission is considered an indirect measure of injury severity, as length of acute medical hospitalization is primarily determined by medical severity4, and individuals who are transferred to rehabilitation earlier tend to be less medically complex than those transferred later5.
Studies of children with TBI who receive inpatient rehabilitation also revealed that early course of recovery predicts later outcome. For instance, in a descriptive analysis of a nationwide sample of children with TBI requiring inpatient rehabilitation, children with better functional status at admission (higher WeeFIM scores) had shorter inpatient stays and better functional outcomes at discharge1. Forsyth and colleagues modeled recovery trajectories in a heterogeneous sample of children with TBI using non-linear mixed effects modeling and found that children who demonstrate faster early progress also make better ultimate recoveries (i.e., have higher WeeFIM scores at discharge)6. However, this study examined children with a range of injury severity and range of functioning at admission, and did not specifically examine children with the most severe injuries.
The association between demographic variables and functional outcome at discharge from inpatient admission remains unclear in pediatric TBI; of demographic variables, age has been the best studied. Older age has been associated with better functional outcome in some 1,2 but not all 6,7 studies. Across the more general TBI literature, there is evidence that younger children are at an increased risk for adverse outcomes, but these differences are most consistently apparent when children under age seven are compared to older children and adolescents8.
While there is some information to guide prediction of outcome in the full range of children admitted to inpatient rehabilitation following TBI, less is known about predicting outcomes for children who enter rehabilitation with the lowest levels of functional skills, such as children with disorders of consciousness (DOC)9. The adult TBI literature suggests that prognosis is poorer if DOC persist with the passage of time. Among adults with DOC, those with even minimal signs of consciousness at one month after injury have a greater chance of demonstrating functional improvements than those without improvements in consciousness at that time, and better functional outcomes are associated with earlier returns of consciousness5,10. In addition, shorter time between injury and admission to inpatient rehabilitation and lower Disability Rating Scale (DRS) score at admission were found to predict better outcome (i.e., lower DRS score) at 6 weeks post-admission11 and lower DRS score at 16 weeks post-injury5. Rate of functional change during the first two weeks of inpatient rehabilitation was also predictive of DRS score at 16 weeks post-injury, with greater early improvement associated with better outcome5.
The present pilot study examined factors associated with functional outcome (WeeFIM scores) at discharge from inpatient rehabilitation and at three-month follow-up after discharge within a small cohort of children with severe TBI who enter rehabilitation with the lowest level of functional skills as measured by the WeeFIM. First, we hypothesized that greater injury severity (as measured by initial GCS score, TFC, and time from injury to admission to rehabilitation) would be associated with worse functional status at discharge from inpatient rehabilitation and at three-month follow-up. Second, we hypothesized that changes in functional status during the early course of a child’s rehabilitation admission would be associated with functional status at discharge and three-month follow-up.
METHODS
Participants
Data were collected from children admitted to a tertiary-care affiliated acute brain injury rehabilitation unit between January 1998 and October 2010. Participants had sustained severe accidental TBI and upon admission had WeeFIM raw scores of 18, the lowest possible rating on the WeeFIM (see below for additional information regarding WeeFIM). Children were included in this study if they were between the ages of 3 and 18 at the time of injury. In the age range of this sample, WeeFIM raw scores of 18 are equivalent to Developmental Functional Quotients (DFQ) scores ranging from 14-18. Sixty children in the database met inclusion criteria. Of these, 19 were missing data from two-week intervals, and 2 children were excluded who had undergone initial inpatient rehabilitation at a different facility prior to admission to our institution. Children excluded from the sample did not differ significantly from children who were included (n=39) on any demographic or injury-related variables. The children without interval data were all admitted to the unit prior to 2003 when institute policies were changed to require consistent recording of interval scores for all children for program evaluation purposes.
Demographic characteristics of the children in the study sample are presented in Table 1. The 39 children ranged in age from 3 to 18 years at the time of injury. Twenty-five children were boys (64%). Thirty children (77%) were Caucasian, seven (17%) were African American, one (3%) was Asian, and one child’s ethnicity (3%) was classified as Other. One child in the cohort had a penetrating injury due to an accidental bb gunshot to the head. Other children in the cohort had depressed skull fractures with local penetration of bone into brain matter.
Table 1.
Patient characteristics
| Full Sample (n=39) | Subset with CALS (n=13) | Subset with Follow-Up WeeFIM (n=16) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean ± SD | Range | Mean ± SD | Range | Mean ± SD | Range | |
| Age at injury (years) | 11.9 ± 4 | 3-18 | 13.8 ± 4 | 7-18 | 11.7 ± 4 | 3-18 |
| Initial GCS score | 4.3 ± 2 | 3-8 | 4.2 ± 2 | 3-7 | 4.3 ± 1 | 3-7 |
| Time to follow commands (days) | 50.2 ± 47 | 5-246 | 46.3 ± 36 | 5-129 | 44.1 ± 35 | 5-129 |
| Time from injury to admission (days) | 28.1 ± 19 | 5-117 | 33.7 ± 26 | 5-117 | 24.4 ± 10 | 5-38 |
| Length of admission (days) | 98.1 ± 57 | 14-255 | 109.9 ± 53 | 49-220 | 97.0 ± 61 | 34-254 |
| Admission WeeFIM DFQ | 14.4 ± .9 | 14-18 | 14.1 ± .3 | 14-15 | 14.4 ± 1 | 14-18 |
| Month 1 WeeFIM DFQ | 19.4 ± 12a | 14-60 | 15.3 ± 2 | 14-21 | 19.5 ± 12 | 14-47 |
| Month 2 WeeFIM DFQ | 21.5 ± 12b | 14-54 | 19.4 ± 9 | 14-44 | 23.5 ± 14 | 14-54 |
| Discharge WeeFIM DFQ | 41.49 ± 23 | 14-75 | 34.7 ± 22 | 15-75 | 39.6 ± 24 | 15-75 |
Abbreviations: DFQ = Developmental Functional Quotient (percent of age-appropriate functioning); CALS = Cognitive and Linguistic Scale
A subset of 38 children has Month 1 scores.
A subset of 36 children has Month 2 scores.
Measures
Functional Independence Measure for Children (WeeFIM)
Functional outcomes were quantified using the Functional Independence Measure for Children (WeeFIM®, Uniform Data System for Medical Rehabilitation, Buffalo, NY), an 18-item performance-based instrument that assesses mobility, self-care, and cognitive abilities12. The WeeFIM has been validated in children with normal development13, developmental disabilities14,15, and acquired brain injury15. While the WeeFIM was initially designed to describe major levels of independence across typically developing children aged 6 months to 8 years13, it has been validated for use in adolescents with cerebral palsy up to age 16 years16 and is commonly used to evaluate older children and young adults with TBI up to 21 years of age1,17,18. Raw scores on the WeeFIM range from 18 to 126.
Raw WeeFIM scores were used to identify those children with the lowest possible total score (18) for inclusion in the study. Given the wide age range of children evaluated in the current study and the effect of age on WeeFIM ratings in children below the age of 7 years due to the developmental nature of the functional abilities assessed13, WeeFIM DFQs19 were used as the measure of functional status in all data analyses. DFQs reflect percent of “normal” or “age-appropriate” functioning, allowing comparison across age groups. Each WeeFIM item is rated on a scale from 1-7, and total DFQs can range from 14 (for a child who receives scores of 1 on items for which the age-based norm is 7) to greater than 100 (for a child who performs at a level exceeding the age-based norm).
As part of routine clinical care, WeeFIM ratings were obtained from each child’s primary therapists at admission, at two-week intervals during admission, and at discharge. The first two interval administrations were identified to be of interest in this investigation and were operationalized as follows: for each child, an interval administration was classified as “Month 1” if it occurred within the first 28 days after admission, and as “Month 2” if it occurred within 29 to 56 days after admission.
Follow-up WeeFIM ratings were obtained by interview three months after the child’s discharge from inpatient rehabilitation. Historically at our institution, data were collected by a trained interviewer during a child’s follow-up visit to an outpatient clinic, if timing permitted. More recently our institution has adopted as standard practice obtaining WeeFIM data through the use of a private company with trained interviewers using a standardized phone protocol three months following the child’s discharge from inpatient rehabilitation. In addition, if a child participated in our institute’s day-rehabilitation treatment program or community-based outpatient therapy program and was administered the WeeFIM by staff as part of routine clinical care between 80 and 110 days after discharge, that score was used for follow-up data. Nevertheless, as routine collection of follow-up WeeFIM data was only recently initiated at our institution, only a subset of children in this cohort had follow-up WeeFIM data.
Cognitive and Linguistic Scale (CALS)
The CALS is a clinician-rated assessment instrument developed to quantify cognitive and linguistic changes following pediatric traumatic or acquired brain injury. The CALS was designed for serial administration by varying members of an interdisciplinary treatment team in order to track recovery and assess outcome during inpatient rehabilitation20. The CALS consists of 20 items that assess arousal, responsivity, emotional regulation, inhibition, attention, response time, orientation, memory, simple and complex receptive and expressive language, initiation, pragmatics, simple and complex problem solving, visuoperceptual ability, visuospatial ability, self-monitoring, and cognitive safety. Scoring for each item ranges from 1 to 5; the total possible score ranges from 20 to 100 with higher scores reflecting better performance. The items were developed to track subtle improvements in cognitive and linguistic functioning, especially in minimally responsive children20. The CALS was designed to be easily adapted for use with children with severe motor or communication impairments20.
As the CALS was recently developed and updated, only a subset of the children in this sample have CALS scores in addition to WeeFIM scores (children admitted after April 2005). For those children, CALS ratings were obtained by each child’s primary speech and language and neuropsychology therapists as part of routine clinical care on the same schedule as the WeeFIM ratings, as reported above.
Glasgow Coma Scale (GCS)
GCS was defined as the earliest available GCS score documented at the scene of injury, in transit, or upon arrival to the Emergency Department21.
Time to Follow Commands (TFC)
TFC was defined as the ability to follow verbal commands twice in a 24-hour period as observed by hospital staff. TFC was obtained based on medical record review if the child began to follow simple, one-step commands prior to admission to inpatient rehabilitation or by staff report and documentation of following two simple commands during a 24-hour period during the child’s rehabilitation admission. For children who were not noted to follow commands during the inpatient rehabilitation stay (n=4), outpatient chart reviews were conducted to determine a window during which command following occurred, and the first day of that window was used to estimate TFC.
Time from injury to admission (TTA)
This variable is defined as the total number of days from injury onset to initial admission to inpatient rehabilitation.
Length of rehabilitation stay (LOS)
The total number of days that a child is admitted to inpatient rehabilitation is the length of rehabilitation stay. If a child is transferred to an acute medical facility (e.g., due to medical instability or to undergo a surgical procedure) and then is re-admitted to the unit within 30 days to continue rehabilitation under the initial treatment plan, the re-admission is considered part of the initial stay.
Procedure
All data were collected as part of routine clinical care and entered into a program evaluation database. The Johns Hopkins School of Medicine’s Institutional Review Board granted exempt status approval for a separate research database to be created for this study that was stripped of all patient identifiers and protected health information. The IRB approval also granted access to medical records. For the exploratory analyses described below, a brief clinical record review was conducted to locate clinical data not entered into the database in order to describe the clinical presentation of the children.
Description of subgroups
Thirty-eight of the 39 children had Month 1 WeeFIM ratings. Three children were transferred to an acute medical facility within their first month of rehabilitation admission due to medical instability and were re-admitted to the rehabilitation unit within two weeks. Due to therapy interruption, their first interval assessment occurred at least four weeks after admission, within the window for “Month 2” scores. For two of these children, their functional status did not change during this time period as evidenced by stable WeeFIM scores from admission to Month 2. As such, the same score was reported for Month 1. In contrast, the third child made gains in functional status prior to his first assessment. His first interval WeeFIM score was thus included with Month 2 data, resulting in missing data for Month 1 scores.
Thirty-six of the 39 children in the sample had Month 2 scores. The three children without Month 2 scores had faster recovery trajectories compared to the rest of the sample. They had significantly higher WeeFIM Total DFQ scores at Month 1 (mean DFQ=53 versus mean DFQ=16; t[36]=-11.9, p<.001) and were discharged shortly after the Month 1 assessment, resulting in shorter LOS (mean=25 days versus mean=104 days; (t[37]=2.5, p=.02). As a result, these children do not have Month 2 data. These three children were significantly younger at the time of injury compared to the larger sample (mean age=4.6 years versus mean=12.5 years; t[37]=3.7, p=.001), and were admitted to rehabilitation shortly after their injuries (mean TTA=8 days versus mean=30 days; t[37]=2.0, p=.05).
Month 1 assessment occurred an average of 19 days after admission (range 12 to 27 days). Month 2 assessment occurred an average of 34 days after admission (range 29 to 48 days), and an average of 73 days prior to discharge (range 9 to 254 days).
Of the 39 children with usable data, 13 had CALS scores in addition to WeeFIM Total DFQ scores. The subset of children with CALS scores was significantly older than children with only WeeFIM scores [t(37)=1.34, p=.04] but did not significantly differ on any other demographic or injury-related variables.
Sixteen children had follow-up WeeFIM Total DFQ scores obtained three months after discharge (mean 90 days after discharge, range 81-110 days). The subset of children with follow-up WeeFIM Total DFQ scores did not differ significantly from children without follow-up data on any demographic or injury-related variables. Nine children overlapped in the CALS and follow-up groups.
Data analysis
All statistical analyses were completed using SPSS 18.0 (www.spss.com), and alpha was set at p≤.05 for all analyses. Descriptive statistics were calculated to examine demographic, injury severity, and rehabilitation variables. Group comparisons were made using the Fisher exact test for categorical variables (sex and race) and t test for continuous variables (age, initial GCS, TFC, time to admission, length of stay, WeeFIM Total DFQ scores, and CALS scores). Bivariate correlation analyses were conducted to investigate associations between demographic, injury-related, and rehabilitation variables and 1) discharge WeeFIM Total DFQ scores and 2) follow-up WeeFIM DFQ scores, where available.
Visual inspection of plotted WeeFIM Total DFQ scores (Figure 1) revealed two groups of children based on functional status at discharge, prompting exploratory analyses to identify patterns of early change in WeeFIM scores with clinical relevance for predicting group status at discharge.
Figure 1.
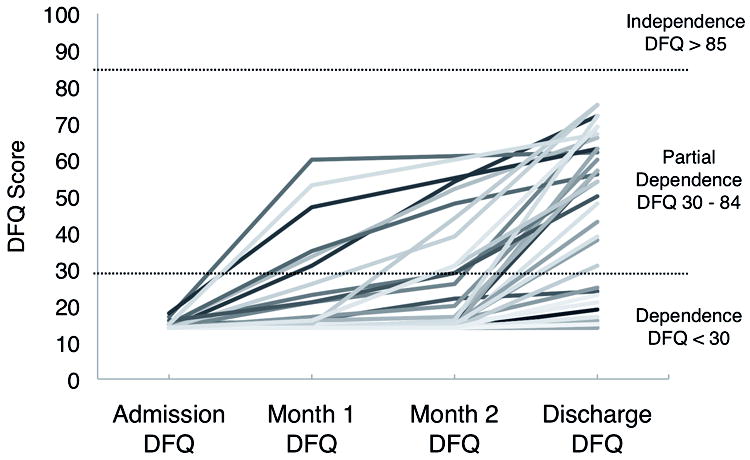
Change in functional status during admission across timepoints for all 39 children. Each line represents an individual child.
To further characterize the clinical features associated with differing patterns of recovery, descriptive data were collected for the subset of children with three-month follow-up data. All data were directly extracted from available records, with the exception of state of consciousness [vegetative state (VS), minimally conscious state (MCS) or conscious state (CS)], which was not historically documented at our institution. Individuals were designated as being in VS, MCS, or CS based on the description of their function in clinical records and the definitions from the Aspen Workgroup10,22,23.
RESULTS
Recovery Patterns
WeeFim
Figure 1 depicts changes in WeeFIM Total DFQ scores over the course of rehabilitation admission. The majority of children made gains in functional status with an average improvement in WeeFIM Total DFQ scores from admission to discharge of 27 percentage points (range 0 to 61 points). Visual examination of Figure 1 revealed two distinct groups: Sixteen children (41%) had discharge WeeFIM Total DFQ scores below 30 (Dependence group) and 23 children (59%) had discharge scores above 30 (Partial Dependence group). Children in the former group could generally be described as requiring maximum to total assistance from others to complete functional activities. Review of clinical records indicated that these children were severely limited in their ability to interact with their environment. Children in the latter group could generally be described as partially dependent on others to complete activities, with needed support ranging from moderate assistance to supervision. No children in our sample had discharge WeeFIM Total DFQ scores above 85, which would be within normal limits of functioning for the child’s age and consistent with an age-appropriate level of functioning.
CALS
All thirteen children with CALS data demonstrated improvements in CALS scores over the course of rehabilitation admission (average improvement of 34 points with a range of 3 to 64). CALS scores were as follows: Admission Mean (M)=24.7, Standard Deviation (SD)=3; Month 1 M=30.3, SD=13; Month 2 M=38.2, SD=21; and Discharge M=58.3, SD=26.
Correlations between demographic and rehabilitation variables and WeeFIM outcomes
Table 2 presents correlations between variables of interest. Given that all children entered rehabilitation at the same level of functioning, admission WeeFIM Total DFQ scores were restricted in range and not correlated with functional status at discharge or follow-up three months after discharge. Admission CALS scores had a wider range of values (20 to 31) and were moderately correlated with discharge WeeFIM Total DFQ scores, although this association was not statistically significant. The strongest correlations with functional status at discharge were with interval WeeFIM Total DFQ scores and interval CALS, with scores obtained closer to discharge (i.e., at Month 2) more strongly correlated with discharge scores. A similar pattern was observed for functional status at follow-up. The strongest correlations with follow-up WeeFIM Total DFQ scores were with WeeFIM Total DFQ score at discharge and with CALS score at discharge. Month 2 WeeFIM and CALS scores were also significantly correlated with follow-up functional status.
Table 2.
Correlations with functional status at discharge and follow-up
| n | Discharge WeeFIM Total DFQ | n | Follow-Up WeeFIM Total DFQ | |
|---|---|---|---|---|
| Admission DFQ | 39 | .26 | 16 | .21 |
| Month 1 DFQ | 38 | .48** | 16 | .51* |
| Month 2 DFQ | 36 | .67** | 16 | .80** |
| Discharge DFQ | - | - | 16 | .96** |
| Admission CALS | 13 | .48 | 9 | .36 |
| Month 1 CALS | 13 | .70** | 9 | .65 |
| Month 2 CALS | 13 | .91** | 9 | .96** |
| Discharge CALS | 13 | .88** | 9 | .89** |
| Age | 39 | -.27 | 16 | -.15 |
| GCS | 39 | .37* | 16 | .34 |
| TFC | 39 | -.58** | 16 | -.61* |
| Time to admission | 39 | -.32* | 16 | -.60* |
| Length of stay | 39 | -.44* | 16 | -.63** |
Abbreviations: DFQ = WeeFIM Developmental Functional Quotient (percent of age-appropriate functioning); CALS = Cognitive and Linguistic Scale; GCS = Glasgow Coma Scale; TFC = Time to follow commands
p≤.05
p≤.01
Greater injury severity was generally associated with poorer functional status at discharge and follow-up. Longer TFC and TTA were both associated with lower WeeFIM DFQ scores at discharge and follow-up. GCS score was significantly correlated with discharge but not follow-up WeeFIM DFQ scores. Length of stay was inversely correlated with functional status at both discharge and follow-up, as children who made swift recoveries were discharged earlier from inpatient rehabilitation. Age at injury was not significantly correlated with either discharge or follow-up WeeFIM Total DFQ scores.
Exploratory Analyses: Accuracy of early change in the classification of discharge status
As early measures of functional status were associated with functional status at discharge and two distinct patterns of recovery were identified, exploratory analyses were performed to examine the accuracy of the presence of change in functional status in classifying discharge status on an individual case level. Thirty-eight children were included in the Month 1 analysis (22 with partial dependence at discharge). The one child missing Month 1 data was only included in the Month 2 analysis and fell within the partial dependence range of function at discharge. All 39 children were included in the Month 2 analysis (23 with partial dependence at discharge). For the purpose of these exploratory analyses, the three children who had recovered rapidly and were discharged prior to Month 2 data collection were included as children who had made change by the Month 2 assessment and whose discharge functioning was in the partially dependent range. To transform these findings into information that could potentially be applied at the level of the individual, we cast our data into the 2×2 tables depicted in Figure 2 and performed two series of contingency table analyses according to Chelune24.
Figure 2.
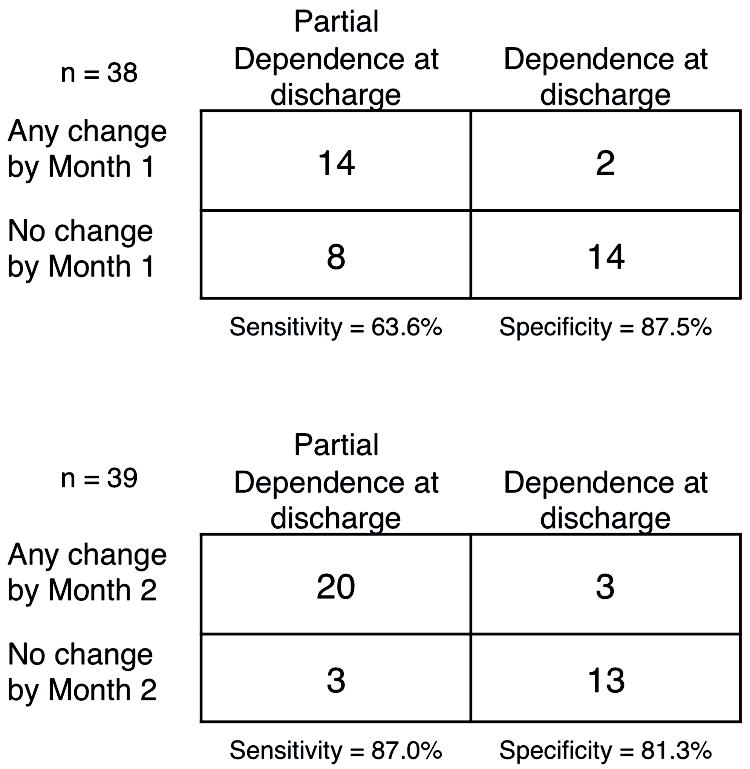
Contingency tables showing frequency of children in each discharge group by presence or absence of change in raw WeeFIM Total scores by Month 1 (n = 38) or Month 2 (n = 39).
We defined our first test factor as whether or not a patient made any absolute change in total WeeFIM raw score by Month 1 and used group status (Dependence or Partial Dependence) as our condition of interest. The resulting sensitivity - the ability to detect individuals who showed any WeeFIM change and were in the Partial Dependence group at discharge - was 14/22 (63.6%). The specificity - the ability to identify individuals who did not show WeeFIM change by Month 1 and were in the Dependence group at discharge - was 14/16 (87.5%). Examination of the likelihood ratio indicated that if a child made any change by Month 1, they were five times more likely to be in the Partial Dependence group at discharge (LR = 5.1; 95% CI [1.3, 19.3]). Overall, these results suggest that any change in functional status by Month 1 is associated with advancing to the Partial Dependence group by discharge. However, the false negative rate for this test factor is 8/22 (36.4%), suggesting that some children who do not make changes in WeeFIM by Month 1 have the potential to continue to make gains in functional status.
The above analyses were then repeated using absolute change in total WeeFIM score by Month 2 as the test factor. The resulting sensitivity was 20/23 (87.0%), suggesting that early change in WeeFIM scores by Month 2 is a sensitive measure of functional status at discharge and that any change by Month 2 is associated with being in the Partial Dependence group at discharge. The specificity of the measure was also high at 13/16 (81.3%), as most patients in the Dependence group at discharge did not change in WeeFIM scores by Month 2. If a child made any change by Month 2, they were over four times more likely to be in the Partial Dependence group at discharge (LR = 4.6; 95% CI [1.7, 13.0]). Any change in functional status by the Month 2 assessment accurately identified the discharge status of 85% of the children in this sample as being in the Partial Dependence group versus the Dependence group, although some children continued to be incorrectly classified using this method (false negative rate is 3/23, 13%; false positive rate is 3/16, 19%).
Exploratory Analyses: Comparison of outcome groups
Of the sixteen children with follow-up data from three months post discharge, those who gained functional skills during rehabilitation admission continued to improve along the same trajectory after discharge from inpatient rehabilitation, while the children who made minimal gains in functional status during admission generally continued to make slow gains following discharge (see Figure 3). All children with follow-up data were discharged to their home settings and participated in either community-based outpatient therapies or in a day-rehabilitation treatment program. To further characterize the rehabilitation course and follow-up functioning of this subgroup of 16 children, we conducted chart reviews to locate additional relevant clinical information (see Tables, Supplemental Digital Content 1 and 2, which present demographic and rehabilitation information for this subgroup).
Figure 3.
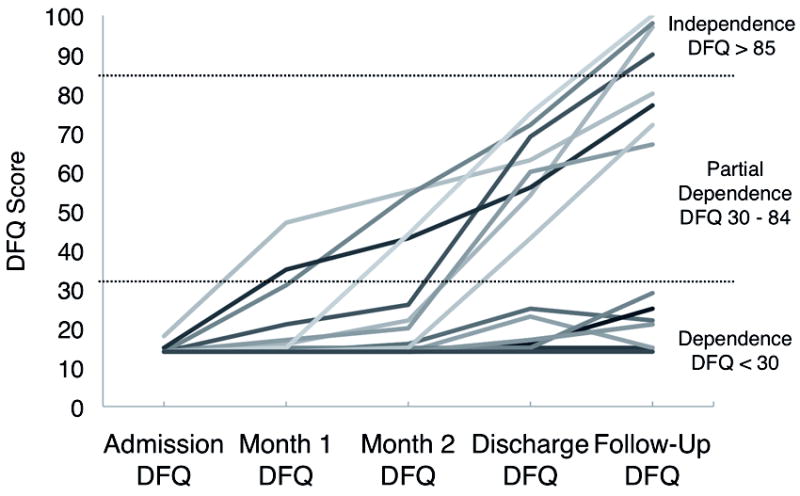
Change in functional status for the subgroup of 16 children with three-month follow-up data. Each line represents an individual child.
Of the children with three-month follow-up data, eight were discharged with functional skills in the Partial Dependence range. All made at least minimal improvements in functional status by Month 2 of admission and had emerged from a MCS by discharge. All children in this group continued to make gains after discharge, and four obtained follow-up total WeeFIM DFQ scores above 85, within the range of age-expected independent functioning. Review of rehabilitation and injury-related information suggests that children in this group tended to have short acute care stays and remained medically stable throughout rehabilitation. The depth of deepest lesion on imaging was quite variable within this group, and those with deeper lesions demonstrated motor impairments (e.g., hemiparesis) and comparatively lower overall functioning. Most children in this group were referred to an intensive day rehabilitation program upon discharge from the inpatient unit.
Of the children with follow-up data, eight remained at the Dependence level of functioning at discharge. None were following commands at admission, and three were in a VS. Seven children achieved command following by discharge, and the remaining child did so between discharge and three-month follow-up. At discharge, seven of eight children were in a MCS, indicating that they had not yet developed a means of functional communication or purposeful object use. During the three-month follow-up period, three children emerged from a MCS, and although a few made modest gains in functional status during this time period, all eight remained at the Dependence level of functioning at follow-up. Two children’s WeeFIM DFQ scores decreased slightly over the follow-up period. While known medical issues likely contributed to decreased functional independence in one child, it is also possible that differences in informants and/or environmental demands contributed to these declines following discharge. Review of rehabilitation and injury-related information suggests that children in this group tended to be medically complicated as evidenced by long TTA and interruptions to rehabilitation due to medical instability, resulting in lengthy inpatient rehabilitation stays. The children in this group had multiple deep lesions on imaging, with lesions extending to the brainstem in seven of eight children. These children all had severe motor impairments. Only one child in this group received therapy through the intensive day rehabilitation program upon discharge from the inpatient unit.
DISCUSSION
This study sought to identify predictors of functional outcome at discharge from inpatient rehabilitation in children with severe TBI who entered rehabilitation with total dependence for functional skills based on the WeeFIM. As expected, higher initial GCS and shorter TFC were correlated with higher WeeFIM DFQ scores at discharge, consistent with previous research2,3. In the smaller sample of children with three-month follow-up data, TFC but not GCS was significantly correlated with functional status. These findings confirm that these measures of severity remain useful in predicting outcome, even among the most severely injured children, and are consistent with prior work suggesting that TFC is more strongly associated with outcome following pediatric TBI than GCS3.
We also predicted that greater length of time from injury to admission to rehabilitation (TTA) would be correlated with worse functional status at discharge and follow-up. In our sample, TTA was significantly correlated with worse functional status at discharge and three-month follow-up. These results are consistent with the existing literature linking TTA to functional status in children with a range of injury severity1 and in adults with disorders of consciousness5,11 and suggest that TTA may also be useful for predicting functional status after discharge. Several authors have described TTA as a marker for injury severity, but it can also be considered a proxy for medical stability, and thus may capture slightly different information than other measures of injury severity. For example, in our small sample, TTA was more strongly correlated than initial GCS score with functional status at three-month follow-up.
Our second hypothesis was that functional status during the early course of a child’s rehabilitation admission would be correlated with functional status at discharge and three-month follow up. The results supported this hypothesis and suggested that early improvements (i.e., by the first month of admission) in WeeFIM DFQ scores were associated with higher discharge WeeFIM DFQ scores. These findings are consistent with the existing literature demonstrating that individuals with TBI who make early progress also make better ultimate recoveries6,11, but to our knowledge this is the first study to demonstrate this association in children with severe TBI who all entered rehabilitation with total functional dependence.
Exploratory analyses suggested that the absence or presence of any change in WeeFIM DFQ scores by Month 1 and Month 2 provides clinically meaningful information about likely functional status at discharge. Any improvement in functional status during the first month of inpatient rehabilitation was associated with further recovery and achievement of Partial Dependence status by discharge. Lack of improvement in WeeFIM DFQ scores by the second month of inpatient rehabilitation was associated with Dependence status at discharge. While analyses of this type have the potential to provide information that can be directly applied at the level of the individual and are an important step towards the development of evidence-based practice, these data should be considered preliminary given the small sample size. Clinically, these data pose the risk that some children who do not show functional change on the WeeFIM would be excluded from aggressive rehabilitation after two months. It is therefore important to emphasize the preliminary nature of these findings and the false negative rates (36% for Month 1 data and 13% for Month 2 data) in our exploratory test factor analyses. It is also critical to highlight that the WeeFIM provides a broad measure of function but does not capture important but lower-level changes in function. For example, improvements in tolerance to positioning, ease of care, arousal and responding, and isolated muscle movements may be important milestones resulting from aggressive rehabilitation but would not be captured by the WeeFIM. This highlights the need for continued investigation of measures best suited to track functional progress in children at the lowest level of function.
The CALS was developed with the goal of being sensitive to functional gains in children with disorders of consciousness and throughout the spectrum of recovery after TBI. Its utility within a cohort of children at the floor of the WeeFIM has not previously been studied; preliminary analyses were therefore conducted in the current study for the small subset of children with CALS data. Within that group, Month 1 and 2 CALS scores were strongly associated with discharge and follow-up WeeFIM DFQ scores. This is consistent with an investigation of the psychometric properties of the CALS20, which identified significant correlations between WeeFIM total raw scores and CALS scores at both admission and at discharge among a heterogeneous sample of children with acquired brain injury. In addition, the range of admission CALS scores observed in our narrowly defined sample suggests that CALS scores may provide unique information about the cognitive functioning of children with the lowest levels of functioning and may contribute to the prediction of functional status at discharge. Certainly, the small size of this subgroup necessitates that the conclusions be considered preliminary, and further study is needed to explore the current results which suggest that the CALS is a useful complement to the WeeFIM in this population. Additional measures designed to capture lower level motor changes which occur during inpatient rehabilitation may also be useful in this population.
The descriptive information about children with follow-up WeeFIM DFQ scores provided additional detail about the recovery trajectories of children who enter rehabilitation completely dependent for all daily activities. Most children (including those in the Dependence group at discharge) made functional gains during inpatient rehabilitation, including the emergence of command following in all but one child who was not following commands at admission. Consistent with the existing literature, children in the Dependent group at discharge tended to have longer TFC3, lower GCS2, longer TTA1,5,11, and deeper brain lesions25 compared to children in the Partial Dependence group at discharge. Consistent with research in adults with DOC suggesting that better functional outcomes are associated with earlier returns of consciousness5,10, seven of eight children in the Dependence group at discharge had not yet emerged from MCS by discharge.
In our sample of children with follow-up data, recovery continued along the same trajectory in the first few months following discharge. Children who were in the Partial Dependence group at discharge continued to make functional gains, with some children even achieving age-appropriate functional status at follow-up. Children who remained in the Dependent group at discharge tended to continue to make slow and small changes in WeeFIM DFQ scores following discharge but remained dependent for all activities, at least as measured by the WeeFIM. The children in the Partial Dependence group at discharge commonly received intensive outpatient therapy in a day rehabilitation setting between discharge and three-month follow-up, while the children in the Dependent group at discharge tended to receive less intensive outpatient therapy. This pattern likely represents a difference in perceived likelihood of benefit from ongoing intensive therapy at the time of discharge from inpatient rehabilitation; however, the effect of intensity of therapy on functional changes observed in these children over the three months following inpatient rehabilitation is unknown. Further study is needed to elucidate the pattern of long-term recovery in this population, particularly for children who remain in a state of total functional dependence at discharge and three-month follow-up.
The current findings need to be considered in the context of methodological limitations. This pilot study is a retrospective review of a select sample of children with severe TBI who were admitted to one rehabilitation center. It could be argued that center-specific policies and procedures as well as patient admission biases result in local differences in treatment delivery and the population served which may also influence functional outcomes. The practice in our institution is to admit children with even the lowest levels of functioning, with the goal of discharging all children to home. As such, replication of our findings across different sites and treatment models will be important. In addition, we did not directly explore the effect of age at injury on functional outcome, given that age-corrected DFQ scores were used in analyses. Future studies with larger samples of defined age groups are needed to explore age effects. Imaging and family psychosocial data were not available for the cohort studied but would be important additional variables to explore in future work. Finally, as noted above, the most important limitation of this study is small sample size, particularly in the correlations involving follow-up data and CALS data. Larger studies that track functional status for longer periods of time following discharge will be important to try to replicate and extend these findings.
CONCLUSIONS
In this sample of children with severe TBI who entered inpatient rehabilitation with total functional dependence, the majority made significant gains in functional status during admission and achieved a level of partial functional dependence by discharge. WeeFIM DFQ scores obtained early in admission were significantly correlated with functional status at discharge and at three months post-discharge. Moreover, any change in functional status on the WeeFIM during the first month of rehabilitation was associated with an increased likelihood of achieving partial dependence at discharge. This study demonstrates the utility of early and ongoing assessment of functional status during inpatient rehabilitation and suggests the potential of such information to inform clinical treatment planning. These findings support the argument that discharge planning for children with severe TBI should begin as early as the first month of rehabilitation admission. Particularly for children who have not made gains in functional status by two months and thus have a high likelihood of remaining in the Dependence group at discharge, discussions with families about planning for training, equipment, and home modifications should begin as early as possible, given that these activities require significant time and resources. In addition, continued efforts are needed to evaluate measures sensitive to functional goals achieved during TBI rehabilitation which are not captured by the WeeFIM.
Supplementary Material
Acknowledgments
Funding: National Institutes of Health: This project was supported by Award Number K23HD061611 (Dr. Suskauer) from the Eunice Kennedy Shriver National Institute of Child Health & Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the National Institutes of Health.
Footnotes
Acknowledgments/credits/disclaimers: N/A
References
- 1.Rice SA, Blackman JA, Braun S, Linn RT, Granger CV, Wagner DP. Rehabilitation of children with traumatic brain injury: descriptive analysis of a nationwide sample using the WeeFIM. Arch Phys Med Rehabil. 2005;86(4):834–836. doi: 10.1016/j.apmr.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Niedzwecki CM, Marwitz JH, Ketchum JM, Cifu DX, Dillard CM, Monasterio EA. Traumatic brain injury: a comparison of inpatient functional outcomes between children and adults. J Head Trauma Rehabil. 2008;23(4):209–219. doi: 10.1097/01.HTR.0000327253.61751.29. [DOI] [PubMed] [Google Scholar]
- 3.Suskauer SJ, Slomine BS, Inscore AB, Lewelt AJ, Kirk JW, Salorio CF. Injury severity variables as predictors of WeeFIM scores in pediatric TBI: Time to follow commands is best. J Pediatr Rehabil Med. 2009;2(4):297–307. [PMC free article] [PubMed] [Google Scholar]
- 4.Ryser DK, Egger MJ, Horn SD, Handrahan D, Gandhi P, Bigler ED. Measuring medical complexity during inpatient rehabilitation after traumatic brain injury. Arch Phys Med Rehabil. 2005;86(6):1108–1117. doi: 10.1016/j.apmr.2004.11.041. [DOI] [PubMed] [Google Scholar]
- 5.Whyte J, Katz D, Long D, et al. Predictors of outcome in prolonged posttraumatic disorders of consciousness and assessment of medication effects: A multicenter study. Arch Phys Med Rehabil. 2005;86(3):453–462. doi: 10.1016/j.apmr.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 6.Forsyth RJ, Salorio CF, Christensen JR. Modeling early recovery patterns after paediatric traumatic brain injury. Arch Dis Child. 2010;95(4):266–270. doi: 10.1136/adc.2008.147926. [DOI] [PubMed] [Google Scholar]
- 7.Dumas HM, Haley SM, Ludlow LH, Rabin JP. Functional recovery in pediatric traumatic brain injury during inpatient rehabilitation. Am J Phys Med Rehabil. 2002;81(9):661–669. doi: 10.1097/00002060-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Taylor HG, Alden J. Age-related differences in outcomes following childhood brain insults: an introduction and overview. J Int Neuropsychol Soc. 1997;3(6):555–567. [PubMed] [Google Scholar]
- 9.Ashwal S, Cranford R. The minimally conscious state in children. Semin Pediatr Neurol. 2002;9(1):19–34. doi: 10.1053/spen.2002.30334. [DOI] [PubMed] [Google Scholar]
- 10.Giacino J, Whyte J. The vegetative and minimally conscious states: current knowledge and remaining questions. J Head Trauma Rehabil. 2005;20(1):30–50. doi: 10.1097/00001199-200501000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Whyte J, Gosseries O, Chervoneva I, et al. Predictors of short-term outcome in brain-injured patients with disorders of consciousness. Prog Brain Res. 2009;177:63–72. doi: 10.1016/S0079-6123(09)17706-3. [DOI] [PubMed] [Google Scholar]
- 12.Msall ME, DiGaudio K, Duffy LC, LaForest S, Braun S, Granger CV. WeeFIM. Normative sample of an instrument for tracking functional independence in children. Clin Pediatr (Phila) 1994;33(7):431–438. doi: 10.1177/000992289403300709. [DOI] [PubMed] [Google Scholar]
- 13.Msall ME, DiGaudio K, Rogers BT, et al. The Functional Independence Measure for Children (WeeFIM). Conceptual basis and pilot use in children with developmental disabilities. Clin Pediatr (Phila) 1994;33(7):421–430. doi: 10.1177/000992289403300708. [DOI] [PubMed] [Google Scholar]
- 14.Ottenbacher KJ, Msall ME, Lyon NR, Duffy LC, Granger CV, Braun S. Interrater agreement and stability of the Functional Independence Measure for Children (WeeFIM): use in children with developmental disabilities. Arch Phys Med Rehabil. 1997;78(12):1309–1315. doi: 10.1016/s0003-9993(97)90302-6. [DOI] [PubMed] [Google Scholar]
- 15.Ziviani J, Ottenbacher KJ, Shephard K, Foreman S, Astbury W, Ireland P. Concurrent validity of the Functional Independence Measure for Children (WeeFIM) and the Pediatric Evaluation of Disabilities Inventory in children with developmental disabilities and acquired brain injuries. Phys Occup Ther Pediatr. 2001;21(2-3):91–101. [PubMed] [Google Scholar]
- 16.Azaula M, Msall ME, Buck G, Tremont MR, Wilczenski F, Rogers BT. Measuring functional status and family support in older school-aged children with cerebral palsy: comparison of three instruments. Arch Phys Med Rehabil. 2000;81(3):307–311. doi: 10.1016/s0003-9993(00)90076-5. [DOI] [PubMed] [Google Scholar]
- 17.Blackman JA, Rice SA, Matsumoto JA, et al. Brain imaging as a predictor of early functional outcome following traumatic brain injury in children, adolescents, and young adults. J Head Trauma Rehabil. 2003;18(6):493–503. doi: 10.1097/00001199-200311000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Massagli TL, Michaud LJ, Rivara FP. Association between injury indices and outcome after severe traumatic brain injury in children. Arch Phys Med Rehabil. 1996;77(2):125–132. doi: 10.1016/s0003-9993(96)90156-2. [DOI] [PubMed] [Google Scholar]
- 19.Msall ME, Tremont MR. Measuring functional status in children with genetic impairments. Am J Med Genet. 1999;89(2):62–74. doi: 10.1002/(sici)1096-8628(19990625)89:2<62::aid-ajmg3>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 20.Slomine B, Eikenberg J, Salorio C, Suskauer S, Trovato M, Christensen J. Preliminary evaluation of the Cognitive and Linguistic Scale: a measure to assess recovery in inpatient rehabilitation following pediatric brain injury. J Head Trauma Rehabil. 2008;23(5):286–293. doi: 10.1097/01.HTR.0000336841.53338.2f. [DOI] [PubMed] [Google Scholar]
- 21.Teasdale G, Jennett B. Assessment and prognosis of coma after head injury. Acta Neurochir (Wien) 1976;34(1-4):45–55. doi: 10.1007/BF01405862. [DOI] [PubMed] [Google Scholar]
- 22.Giacino JT, Ashwal S, Childs N, et al. The minimally conscious state: Definition and diagnostic criteria. Neurology. 2002;58(3):349–353. doi: 10.1212/wnl.58.3.349. [DOI] [PubMed] [Google Scholar]
- 23.Giacino JT, Kalmar K, Whyte J. The JFK coma recovery scale-revised: Measurement characteristics and diagnostic utility. Arch Phys Med Rehabil. 2004;85(12):2020–2029. doi: 10.1016/j.apmr.2004.02.033. [DOI] [PubMed] [Google Scholar]
- 24.Chelune GJ. Evidence-based research and practice in clinical neuropsychology. Clin Neuropsychol. 2010;24(3):454–467. doi: 10.1080/13854040802360574. [DOI] [PubMed] [Google Scholar]
- 25.Grados MA, Slomine BS, Gerring JP, Vasa R, Bryan N, Denckla MB. Depth of lesion model in children and adolescents with moderate to severe traumatic brain injury: use of SPGR MRI to predict severity and outcome. J Neurol Neurosurg Psychiatry. 2001;70(3):350–358. doi: 10.1136/jnnp.70.3.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


