Abstract
Objective
This study explored whether adolescents with elevated symptoms of mania (ESM+) engage in more HIV risk behaviors than those with other psychiatric disorders and examined factors associated with HIV risk behavior among ESM+ adolescents.
Method
Eight hundred and forty adolescents (56% female, 58% African American, mean age 14.9 years) who received mental health treatment completed private, computer-based assessments of psychiatric disorders, sexual and substance use behaviors, and provided urine to screen for sexually transmitted infections (STI).
Results
Eighty-seven percent met criteria for a psychiatric disorder and among these youth 21% were considered ESM+. Compared to those with other psychiatric disorders, ESM+ were more likely to be sexually active (61.6% vs. 53.6%), have multiple sexual partners (58.6% vs. 37.5%), have unprotected sex (38.4% vs. 28.0%), exchange sex for money (4.7% vs. 1.2%) and to test positive for an STI (14.0% vs. 6.3%). Among ESM+ youth, sexual risk behaviors were primarily associated with individual factors (e.g., self-efficacy, impulsivity, and substance use) and varied depending on the type of sexual behavior (e.g., onset of sex, number of partners, and condom use).
Conclusions
Adolescents with ESM should be regularly screened for sexual risk behaviors and receive HIV prevention skills. Efforts to increase self-efficacy for safer sex, reduce impulsivity, and decrease substance use may be effective targets for sexual risk reduction among adolescents with ESM.
Keywords: Bipolar Disorder, Mania, Adolescents, Sexual Risk, HIV Prevention
In the United States, youth under age 25 account for nearly half of newly diagnosed sexually transmitted infections (STIs) annually, including HIV (Eaton, et al., 2006). Adolescents with psychiatric disorders initiate sex earlier, are less likely to use condoms, have higher rates of STIs, more unintended pregnancies, and more sexual partners than adolescents without a history of mental illness (e.g., DiClemente & Ponton, 1993).
Although adolescents with psychiatric illness are at increased risk for HIV, those with elevated symptoms of mania (ESM) might be at even greater risk. A manic episode is defined by the DSM-IV (APA, 1994) as a distinct period of an abnormal and persistent elevated, expansive, or irritable mood with at least one week duration or requiring hospitalization accompanied by three (four if the mood is only irritable) of the following symptoms being present to a significant degree: inflated self-esteem or grandiosity, decreased need for sleep, abnormally talkative or pressured speech, flight of ideas or racing thoughts, distractibility, increased goal-directed activity or psychomotor agitation, and excessive involvement in pleasurable activities that have a high potential for unpleasant consequences. The disturbance in mood must impair functioning, require hospitalization, or be accompanied by psychotic features.
Data from the National Comorbidity Survey (Merikangas et al., 2007) suggests that although bipolar I disorder is relatively rare among adolescents (1%) impairing symptoms of bipolar spectrum disorders are more common (6.2%). Sub-threshold rates for bipolar disorders among adolescent populations vary widely from 1.2% to 13.3%, due to differences in how these cases are defined (Axelson et al., 2011). Among children and adolescents, symptoms of mania are more common than bipolar spectrum disorders and are associated with marked psychosocial dysfunction and psychopathology (Merikangas et al., 2007)
Among adults, symptoms of mania are associated with higher rates of sexual risk behaviors and STIs (Ramrakha, Caspi, Dickson, Moffitt, & Paul 2000). However, little is known about the relationship between mania symptoms and sexual risk behaviors among adolescents. Brown and colleagues (2010) found that adolescents with mania symptoms were nearly twice as likely to have had vaginal or anal sexual intercourse, three times as likely to have multiple sexual partners, and five times as likely to test positive for an STI compared to adolescents who did not meet criteria for any psychiatric disorder. Less is known about differences in HIV risk behaviors among those with ESM relative to those with other psychiatric presentations and, more importantly, how mania symptoms function to increase sexual risk behavior.
Consistent with theories of the Behavioral Activation System (BAS), activation and inhibition (i.e., movement toward goals that appear rewarding and movement away from behaviors that may lead to negative outcomes) appear to play important roles in sexual risk taking among adolescents (Hoyle, Fejfar, & Miller, 2000). Adolescents with more sensitive behavioral approach systems are more vulnerable to developing bipolar spectrum disorders (Alloy et al., 2011). Together these data suggest adolescents with ESM might be especially vulnerable because the BAS is associated with both bipolar disorder and sexual risk behaviors.
The Social Personal Framework (SPF; Donenberg & Pao, 2005) is a model that may prove useful for understanding sexual risk behavior among adolescents with ESM. This broad contextual model posits that personal attributes, family influences, peer/partner factors and community characteristics contribute uniquely to adolescent sexual risk behavior. The SPF accounts for the increased sexual risk among youth with psychiatric disorders by emphasizing how psychopathology is associated with impulsivity, lack of judgment, cognitive misperception, sensitivity to partner rejection, sexual trauma and low self-esteem.
The current paper examines differences in sexual risk behaviors among adolescents with ESM relative to teens with other psychiatric disorders and explores factors associated with sexual risk behavior among those with ESM. Analyses were guided by the SPF; we hypothesized more impulsivity, substance use, and less self-efficacy (individual factors), more parental permissiveness and less parental monitoring (family factors), and poorer neighborhood environment (community factor) would be associated with sexual risk behaviors (i.e., having vaginal or anal sex, having two or more sexual partners, and not using a condom during their last sexual intercourse) and consequences (i.e., sexually transmitted infections) among adolescents presenting with ESM. Findings are expected to guide HIV interventions by identifying modifiable factors that are associated with sexual risk behavior for this vulnerable group.
Method
Participants
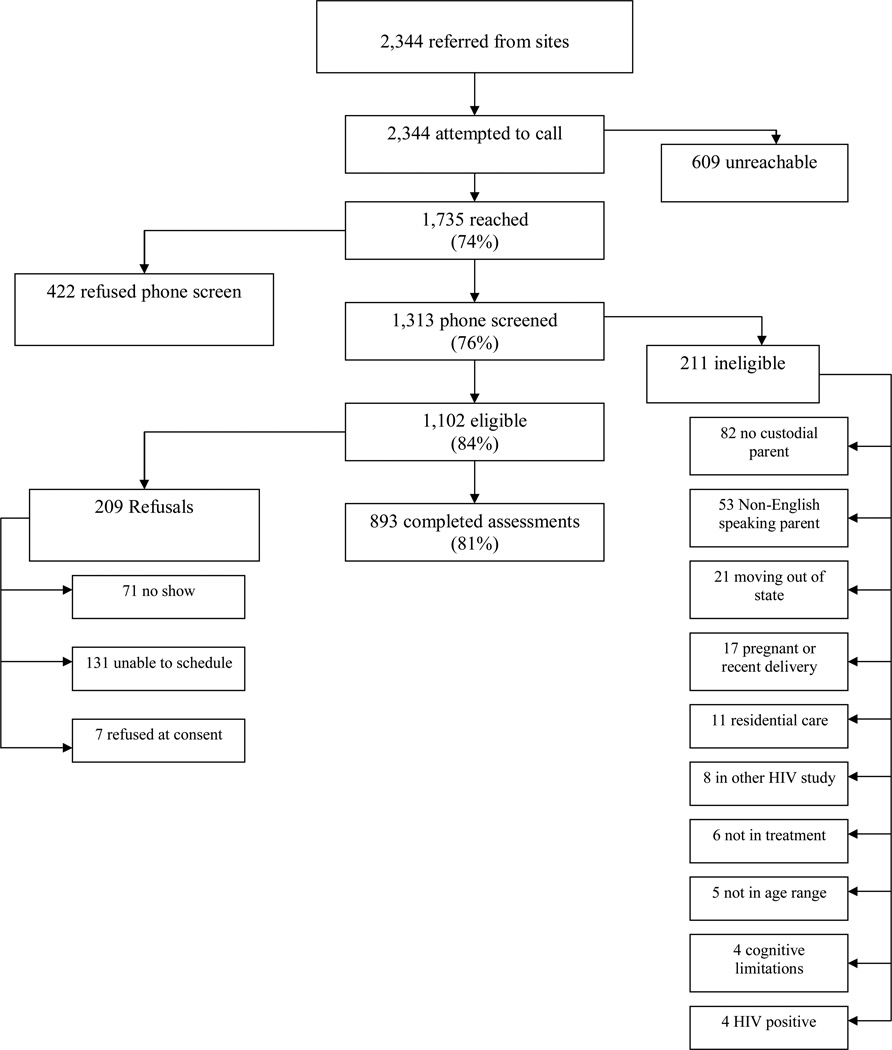
Data for this study are from baseline assessments for Project STYLE, a multi-site study testing the comparative efficacy of a family HIV prevention program relative to two adolescent only control interventions among adolescents recruited from outpatient and inpatient psychiatric settings (see Brown et al., 2010 for study details; see Figure 1 for recruitment and retention data).
Figure 1.
Project STYLE Consort.
All procedures were approved by the respective Institutional Review Boards for each study site. Adolescents under 18 years of age gave assent; parents gave informed consent for their child’s participation and their own participation. Adolescents over 18 years of age gave informed consent.
Measures
Personal factors
Personal or individual level factors guided by the SPF included substance use, impulsivity, and self-efficacy. Substance use (alcohol and marijuana) was collected via the Adolescent Risk Behavior Assessment (ARBA) (Donenberg, Emerson, Bryant, Wilson, & Weber-Shifrin, 2001), a computer-assisted structured interview designed for adolescents. Impulsivity was measured with the Impulsive Decision Making Questionnaire (Donohew et al., 2000) which measures how well a person can distinguish cognitive cues used in rational decision making from affective and physiological cues used in impulsive decision making (alpha = .78). Self-efficacy was measured with the HIV Self-Efficacy scale (Lawrence, Levy, & Rubinson, 1990) which assesses beliefs about engaging in HIV preventive behaviors (alpha = .85) and the Condom Use Self-Efficacy scale (Prochaska, Redding, Harlow, & Rossi, 1994) which measures beliefs about efficacy to use condoms in affect-laden situations (alpha = .93).
Family factors
The Parenting Style Questionnaire (PSQ; Oregon Social Learning Center, 1990) yields two subscales: Parental Monitoring (alpha = .62) and Parent Permissiveness (alpha = .75).
Community factors
The Neighborhood Environment Scale (Crum, Lillie-Blanton and Anthony, 1996) measures the perceived quality of the neighborhood (alpha = .88).
Sexual behaviors
The Adolescent Risk Behavior Assessment (ARBA) measured sexual behaviors that are associated with HIV infection among adolescents (e.g., number of sexual partners condom use).
Sexually transmitted infections (STI)
Data was obtained by urine screen for three prevalent sexually transmitted pathogens: N. gonorrhoeae, C. trachomatis, and T. vaginalis. Polymerase chain reaction assays tested for chlamydia, gonorrhea and trichomonas; positive STIs were treated by a study nurse.
Psychiatric disorders
The Computerized Diagnostic Interview Schedule for Children (C-DISC-IV) is an audio assisted measure used to screen for a full range of psychiatric symptoms, based on the DSM-IV (APA, 1994); reliability and validity are acceptable (Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). Caregivers and adolescents responded separately and both reported on adolescent symptoms. The Present State Youth version was used with variable timelines for specific symptoms.
The C-DISC scoring program assigns subjects as threshold/positive, sub-threshold/intermediate, or negative for a range of psychiatric diagnoses. Threshold/positive is assigned to those who have endorsed the full symptom criteria (including number of symptoms, duration and frequency) specified by the DSM-IV (APA 1994). Sub-threshold/intermediate diagnosis is assigned when at least half of the symptom criteria have been met (similar to a Not Otherwise Specified (NOS) diagnosis). Finally, a negative diagnosis when less than half of the symptom criteria are endorsed. Functional impairment is not included in the C-DISC algorithm.
Adolescents who reported a significantly elevated, expansive or irritable mood (that represented a notable departure from their typical mood state and occurred outside of a positive event) lasting for at least one week or requiring hospitalization were queried for mania symptoms corresponding with DSM-IV Criteria B. (e.g., grandiosity, decreased need for sleep, increased goal-directed activity) that occurred during either an elevated or irritable mood state in the past four weeks. Sub-threshold and threshold cases were assigned based on C-DISC scoring described above.
Data Analyses
Ninety-four percent (n = 840) of the adolescents enrolled in the study had complete C-DISC-IV diagnostic data. Adolescent and caregiver data were combined because this method is similar to clinical practice and because other studies have demonstrated this method is reasonable (Garland et al., 2001). Kappa values for youth and caregiver reports ranged from (.12 – .21), similar to a previous study examining parent-child C-DISC agreement (Jensen et al., 1999).
Adolescents were considered positive for ESM (ESM+) if they met sub-threshold or threshold criteria for mania. These were combined because sub-threshold cases of mania are more common, yet still highly impaired (Merikangas et al., 2007). Moreover, only one significant difference was found among all study variables between the sub-threshold and threshold levels (i.e., higher reported rates of substance use before sex in the sub-threshold group), further supporting the sensibility of combing these groups.
Based on the combination of parent and adolescent report of symptoms, 87% of adolescents (n = 734) met C-DISC sub-threshold or threshold criteria for one or more psychiatric diagnosis. Among those with a psychiatric diagnosis, 21% were classified ESM+. Many in the ESM+ group also met criteria for another diagnosis (e.g., 70% met C-DISC criteria for MDD), but we analyzed this group separately because the data on the sexual risk among adolescents with ESM is extremely limited. The ESM– group consisted of adolescents who met C-DISC criteria for another psychiatric disorder (i.e., Generalized Anxiety Disorder, Major Depressive Disorder, Post-Traumatic Stress Disorder, Attention Deficit Hyperactivity Disorder, Oppositional Defiant Disorder, Conduct Disorder), but did not meet threshold or sub-threshold criteria for mania. Thus, the final sample for this paper is comprised of adolescents in mental health treatment meeting criteria for one or more psychiatric diagnosis. Those who did not report psychiatric symptoms indicative of a current psychiatric diagnosis were excluded from the analyses.
First, chi-square and t-tests were conducted to examine differences between the ESM+ and ESM− groups on sexual behaviors and substance use. Based on these results, regression analyses were conducted to explore relationships between SPF factors and sexual risk behaviors among those with in the ESM+ group (n= 152). Demographic factors were entered in the first step and social-personal factors in the second step. The model predicting vaginal or anal sex included all participants in the ESM+ group; the remaining regressions were limited to those who were sexually active (n = 94). For the regression models examining condom use at last intercourse and two or more sexual partners, only one of the two self-efficacy measures (i.e., either HIV self-efficacy or condom use self-efficacy) was included in each model because these two measures were highly correlated (r = .54, p < .01). Adjusted odds ratios were calculated for each sexual risk behavior. For the regression model examining substance use before sex, models for sub-threshold and threshold mania symptoms were conducted separately based on a previous finding that this risk behavior was more frequent among those in the sub-threshold group (51.6% vs. 7.1%; χ2 = 8.29, df = 1, p < .01); however, the model was not tested for the threshold group because only one participant reported substance use before sex.
Results
Of the 152 adolescents classified as ESM+, 68% were female and 53% were African American with a mean age of 14.89 (SD = 1.31) years. Median annual household income was $20,000–$30,000 and over half had been psychiatrically hospitalized in the last three months. The ESM+ group was not significantly different from the ESM− group in terms of age, race, or household income; however, more females (68% vs. 54%) and more adolescents with a history of psychiatric hospitalization (47% vs. 30%) were ESM+ relative to ESM− (see Table 1).
Table 1.
Demographics for ESM+ and EMS− Groups
| ESM+ n=152 |
ESM− n=582 |
|
|---|---|---|
| Gender | ||
| Male | 48 (31.8%) | 265 (45.8%) |
| Female | 103 (68.2%)* | 314 (54.2%) |
| Ethnicity | ||
| African American | 80 (56.3%) | 293 (53.3%) |
| Other | 62 (43.7%) | 257 (46.7%) |
| Mean Age | 14.89 (sd=1.31) | 14.93(sd=1.35) |
| Household Income | ||
| < 30,000 | 77 (55.4%) | 341 (61.7%) |
| > 30,000 | 62 (44.6%) | 212 (38.3%) |
| Hospitalization in last 3 months | 71 (46.7%)* | 173 (29.9%) |
Note: * indicate p < .05
Differences in Sexual Risk Behaviors: ESM+ vs. ESM−
As shown in Table 2, those classified in the ESM+ group were significantly more likely than the ESM− group to ever have vaginal or anal sex, have two or more partners in the last ninety days, test positive for an STI, have unprotected sex at last vaginal or anal sexual intercourse, and exchange sex for money, drugs, or shelter.
Table 2.
Prevalence (%) of Sexual Risk Behaviors by ESM Group
| Risk Behavior | ESM+ (n=152) |
EMS− (n=582) |
χ2 (1) |
|---|---|---|---|
| Ever had vaginal or anal sex | 61.6 | 53.6 | 3.07* |
| Two or more partners in last 90 days | 58.6 | 37.5 | 7.95* |
| Positive STI urine screen | 14.0 | 6.3 | 8.07* |
| Unprotected at last sexual intercourse | 38.4 | 28.0 | 3.35* |
| Ever used marijuana | 43.5 | 41.5 | .20 |
| Partner used drugs before sex | 39.0 | 33.6 | .62 |
| Sex with someone met the same day | 26.7 | 16.4 | 2.33 |
| Had sex in exchange for money, drugs, or shelter | 4.7 | 1.2 | 7.39* |
| Bought sex with money, drugs, or shelter | 0.7 | 0.7 | .02 |
| Used drug/alcohol at last sexual intercourse | 37.8 | 35.2 | .10 |
Note: * indicate p < .05
Bivariate Associations with Sexual Risk Factors Among ESM+
For those classified as ESM+, a history of vaginal or anal sex was significantly associated with marijuana use (χ2 = 20.67, df = 1, p < .01), alcohol use (χ2 = 15.49, df = 1, p <. 01), gender (χ2 = 5.61, df = 1, p < .02), and age [t(149) = −3.43, p < .01]. Among those who were sexually active (n = 93), multiple sexual partners was significantly associated with greater impulsivity [t(38.54) = −2.30, p < .05], lower HIV prevention self-efficacy [t(56) = 2.66, p = .01], and lower condom use self-efficacy [t(55) = −2.62, p < .05]. Failure to use a condom during last sexual episode was significantly associated with lower condom use self-efficacy [t(41.67) = −4.31, p < .01], lower HIV self-efficacy [t(83) = 2.86, p < .01], a poorer neighborhood environment [t(83) = 2.62, p < .01], and race(χ2 = 11.20, df = 1, p < .01). Finally, testing positive for a STI was significantly associated with lower HIV self-efficacy [t(47.32) = 1.98, p < .01], gender (χ2 = 3.97, df = 1, p < .05), and race (χ2 = 4.99, df = 1, p < .04).
Multivariate Associations with Sexual Risk Behaviors Among ESM+
Logistic regressions results for those in the ESM+ group are presented in Table 3. A history of sex (model χ2 = 42.10, p < .01) was associated with being female (OR = 2.87), being 15 years of age or older (OR = 2.30), having used alcohol in the past thirty days (OR = 4.86), and having ever used marijuana (OR = 3.69). Two or more partners in the last ninety days (model χ2 = 11.97, p < .01) was associated with more impulsivity (OR = 1.13) and less HIV prevention self-efficacy (OR = 0.87). Not using a condom at last sexual intercourse (model χ2 = 25.24, p < .01) was associated with less self-efficacy for condom use (OR = .89). Only demographic factors were significantly associated with testing positive for an STI, such that being female (OR = 9.06) and African-American (OR = 4.45) were significant predictors for a positive STI test (model χ2 = 11.73, p < .01). None of the predictors were significant in the model predicting alcohol or drug use at last sexual intercourse (model χ2 = .35, p = .95) among those with sub-threshold symptoms of mania.
Table 3.
Logistic Regressions Predicting Sexual Risk Behavior in ESM+ Group
| Ever had Vaginal/ Anal Sex |
Two or More Partners1 |
Unprotected Last Sex1 |
Sexually Transmitted Infection1 |
|||||
|---|---|---|---|---|---|---|---|---|
| Variable | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Individual Factors | ||||||||
| Age (15 or older) |
2.3* | [1.04, 5.08] | --- | --- | --- | --- | --- | --- |
| Gender (Female) |
2.87* | [1.22, 6.73] | --- | --- | --- | --- | 9.06* | [1.03, 79.66] |
| Race (African American) |
--- | --- | --- | --- | 3.06 | [0.9, 9.61] | 4.45* | [1.07, 18.57] |
| Drank Alcohol in Last 30 Days | 4.86* | [1.62, 14.59] | --- | --- | --- | --- | --- | --- |
| Ever Used Marijuana |
3.69* | [1.59, 8.59] | --- | --- | --- | --- | --- | --- |
| Impulsive Decision Making Scale |
--- | --- | 1.13* | [1.00, 1.27] | --- | --- | --- | --- |
| HIV Self-Efficacy |
--- | --- | 0.87* | [0.80, 0.99] | --- | --- | 1.05 | [0.95, 1.16] |
| Condom Use Self-Efficacy |
--- | --- | --- | --- | .88* | [0.82, 0.96] | --- | --- |
| Community Factors | ||||||||
| Neighborhood Environment Scale |
--- | --- | --- | --- | 0.89 | [0.68, 1.16] | --- | --- |
| Family Factors | ||||||||
| Parental Monitoring |
--- | --- | --- | --- | --- | --- | --- | --- |
| Parental Permissiveness |
--- | --- | --- | --- | --- | --- | --- | --- |
Among sexually active only
Note: * indicate p < .05
Discussion
Results of the study suggest that those with ESM are among those at greatest risk for HIV, other STIs, teen pregnancy, and cervical cancer because they are more likely to engage in sexual risk behaviors than teens with other psychiatric disorders. Alarmingly, 14% of those with ESM tested positive with an untreated STI at their baseline assessment compared to only 6% of those with other psychiatric disorders. Moreover, the data suggests that sexual risk behaviors were equally high or higher among those with sub-clinical versus threshold mania symptoms. These data emphasize the importance of assessing and reducing sexual risk behaviors among adolescents presenting with ESM in medical and mental health settings.
Data from the current study further our understanding of risk and protective factors among this vulnerable sub-group of adolescents with ESM. Although no single factor within the SPF was consistently associated with all sexual risk behaviors, each of the individual factors (i.e., impulsivity, self-efficacy, and substance use) and the community factor (i.e., neighborhood environment) were each related to at least one type of sexual risk behavior at the bivariate level, suggesting that sexual risk behavior is significantly influenced by both individual characteristics and the surrounding environment. The nature of these relationships are in the expected directions and are clinically sensible.
More impulsivity was associated with having multiple sexual partners for adolescents with ESM. During manic or hypomanic episodes, poor discrimination in sexual partners may occur in the context of increased opportunities for risk behaviors (e.g., decreased need for sleep provides more opportunities for risk behaviors).
Less reported self-efficacy was associated with having multiple sexual partners and failure to use condoms among adolescents with ESM. During manic and hypomanic episodes thoughts of grandiosity might lead teens who feel invincible to ignore signs of risk or become less concerned about STIs or pregnancy, leading to decreased condom use. Adolescents with ESM who believe they are ineffective at using condoms are the least likely to use them consistently, and thus are at greater risk.
Alcohol and marijuana use were associated with a five- and four-fold increase, respectively, of ever having vaginal or anal sex among adolescents with ESM. This is consistent with previous studies among adults (Meade, Graff, Griffin, & Weiss, 2008) and indicates that manic episodes might lead directly to substance seeking behaviors, which in turn reduce inhibitions and increase sexual behavior. Alternatively, in the aftermath of a manic or hypomanic episode, adolescents might seek substances to re-experience euphoria or boost low moods; substance use in this context might also lower inhibitions and lead to sexual risk behavior.
Limitations
Despite the strengths of this study, some limitations should be noted. Data are self-report and the sample is not nationally representative. The C-DISC does not use all DSM-IV criteria (e.g., functional impairment is not required for positive diagnosis). Although the sample was ethnically diverse, data might not generalize to all mental health populations. No information about mania symptoms or mood disorders among parents/caregivers was collected and so we were not able to discern the effects of how parenting an adolescent with ESM may be influenced by a parent’s own history of mental health problems. Finally, the temporal relationships between sexual risk and individual factors cannot be determined from these data. It is impossible to know whether substance use, impulsivity, and poor self-efficacy are risk factors for sexual risk behavior specifically during a manic episode or whether these are risk factors for those with ESM more generally.
Implications for Research, Policy, and Practice
Addressing sexual risk behaviors in adolescents presenting with ESM is important because these youth engage in more sexual risk behaviors and present with higher rates of STIs compared to those with other psychiatric disorders. These data suggest that policies geared toward encouraging routine screening for sexual risk behaviors and STIs for adolescents with psychiatric disorders and to maintain more ongoing monitoring for youth with manic symptoms are sensible and might prevent adolescents from sexual risk behaviors. The Adolescent Risk Inventory is a brief measure that clinicians can use to assess sexual and other risk behaviors (Lescano et al., 2007). This practice is consistent with policies geared toward regular assessment for other risk behaviors, such as suicidal ideation. Adolescents with ESM should receive information about common STIs, symptoms, and treatment. There is strong evidence that STIs facilitate HIV transmission directly through biological methods (Fleming & Wasserheit, 1999) and therefore routine STI testing and treatment is important for decreasing risk for HIV. Moreover, testing positive for an STI is associated with a subsequent reduction in the number of sexual partners and unprotected sex behavior among adolescents (Sznitman et al., 2010). Therefore, connecting youth to STI testing and treatment is important for lowering risk for HIV infection and sexual risk behavior. Furthermore, early identification of HIV is important for engaging in treatment, decreasing the spread of the virus (especially during the period of new infection when transmission likelihood is great, due to high viral load), and prolonging the duration and quality of their lives (Rotheram-Borus & Futterman, 2000).
Increasing self-efficacy and condom use skills among adolescents with ESM is an important clinical goal to improve condom use and reduce risk for HIV and other health consequences. Medical and mental health providers can provide sexual risk prevention within the context of routine care and treatment. The current study suggests that among adolescents with ESM those with more condom use self-efficacy had less unprotected sex. This finding is consistent with research suggesting that adolescents with more self-efficacy to use condoms, especially during distress, are more likely to use condoms consistently in sexual situations (Lescano, Brown, Miller, & Puster, 2007).
Adolescents with ESM presenting for mental health treatment can be taught to identify triggers for risk behaviors and learn problem-solving, communication, and affect management skills that will increase condom use during periods of elevated, expansive or irritable moods. Teaching condom negotiation skills is an important component of effective HIV preventive interventions (Crepaz et al., 2009) and even more important with emotionally compromised youth, such as those experiencing a manic episode. Adolescents can improve their skills and self-efficacy through role playing a variety of situations, such as asking a partner to use and condom, responding to a partner who refuses to use a condom, and negotiating condom use during a manic episode.
This study provides strong evidence that adolescents presenting with ESM are at increased risk for STIs. Factors associated with increased sexual risk behavior were also identified, such as impulsivity, self-efficacy, and substance use. These might represent important targets of treatment to reduce sexual risk behaviors. More research is needed to understand the temporal relationships between manic episodes and sexual risk behavior, to understand if sexual risk assessment and STI testing referrals are useful in reducing risk, and which types of intervention or prevention modalities are effective at reducing sexual risk behaviors among adolescents presenting with ESM. However, until these data are available, professionals interfacing with adolescents with psychiatric diagnoses, and especially those with ESM, should routinely screen for sexual risk behavior and refer adolescents to STI testing and treatment.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (R01 MH63008) to Rhode Island Hospital (P.I. Larry K. Brown, M.D.) and the Lifespan/Tufts/Brown Center for AIDS Research.
Project STYLE Study Group
Principal Investigators
Larry K. Brown, M.D.-Rhode Island Hospital, Providence, RI
Ralph DiClemente, Ph.D.-Emory University, Atlanta, GA
Geri Donenberg, Ph.D., University of Illinois at Chicago, Chicago, IL
Site Investigators
Chinmayee Barve, Ph.D.- University of Illinois at Chicago, Chicago, IL
Richard Crosby, Ph.D.-Emory University, Atlanta, GA
Wendy Hadley, Ph.D.-Rhode Island Hospital, Providence, RI
Delia Lang, Ph.D.-Emory University, Atlanta, GA
Celia Lescano, Ph.D.-Rhode Island Hospital, Providence, RI
Cami McBride, Ph.D.- Rosalind Franklin University of Medicine and Science, Chicago, IL
Consultants
Nancy Beausoleil, M.S.- Rhode Island Hospital, Providence, RI
Angela Caliendo, M.D., Ph.D.- Emory University, Atlanta, GA
David Pugatch, M.D.- Rhode Island Hospital, Providence, RI
Ron Seifer, Ph.D.- Rhode Island Hospital, Providence, RI
Project Coordinators
| Rhode Island Hospital: | Katelyn Affleck, B.A. |
| Catherine Barber, B.S. | |
| Renee Johnson, MPH | |
| Harrison Kell, B.A. | |
| Erika Litvin, B.S. | |
| Jonathon Thompson, B.S. | |
| University of Illinois at Chicago: | Gloria Coleman, M.A. |
| Emily Hasselquist, B.A. | |
| Chisina Kapungu, Ph.D. | |
| Charu Thakral, Ph.D. | |
| Emory University : | Cara Averhart, M.A. |
| Wayne Baudy, MPH | |
| Emily Higgins, MPH | |
| Ana Massey, MPH |
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Alloy LB, Bender RE, Whitehouse WG, Wagner CA, Liu RT, Grant DA, Abramson LY. High Behavioral Approach System (BAS) sensitivity, reward responsiveness, and goal-striving predict first onset of bipolar spectrum disorders: A prospective behavioral high-risk design. Journal of Abnormal Psychology. 2011 doi: 10.1037/a0025877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelson DA, Birmaher B, Strober MA, Goldstein BI, Ha W, Gill M, Keller MB. Course of subthreshold bipolar disorder in youth: Diagnostic progression from bipolar disorder not otherwise specified. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(10):e1–e3. doi: 10.1016/j.jaac.2011.07.005. 1001–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LK, Hadley W, Stewart A, Lescano C, Whiteley L, Donenberg G, DiClemente R. Psychiatric disorders and sexual risk among adolescents in mental health treatment. Journal of Consulting and Clinical Psychology. 2010;78(4):590–597. doi: 10.1037/a0019632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crepaz N, Marshall KJ, Aupont LW, Jacobs ED, Mizuno Y, Kay LS, O’Leary A. The efficacy of HIV/STI behavioral interventions for African American females in the United States: A meta-analysis. American Journal of Public Health. 2009;99(11):2069–2078. doi: 10.2105/AJPH.2008.139519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crum RM, Lillie-Blanton M, Anthony JC. Neighborhood environment and opportunity to use cocaine and other drugs in late childhood and early adolescence. Drug and Alcohol Dependence. 1996;43(3):155–161. doi: 10.1016/s0376-8716(96)01298-7. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Ponton LE. HIV-related risk behaviors among psychiatrically hospitalized adolescents and school-based adolescents. The American Journal of Psychiatry. 1993;150(2):324–325. doi: 10.1176/ajp.150.2.324. http://ajp.psychiatryonline.org. [DOI] [PubMed] [Google Scholar]
- Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber-Shifrin E. Understanding AIDS-risk behavior among adolescents in psychiatric care: Links to psychopathology and peer relationships. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(6):642–653. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donenberg GR, Pao M. Youths and HIV/AIDS: Psychiatry's Role in a Changing Epidemic. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44(8):728–747. doi: 10.1097/01.chi.0000166381.68392.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohew L, Zimmerman R, Cupp PS, Novak S, Colon S, Abell R. Sensation seeking, impulsive decision-making, and risky sex: Implications for risk-taking and design of interventions. Personality and Individual Differences. 2000;28(6):1079–1091. [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Ross J, Hawkins J, Harris WA, Wechsler H. Youth risk behavior surveillance - United States 2005. Morbidity and Mortality Weekly Report. 2006;55(SS05):1–108. http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5505a1.htm. [PubMed] [Google Scholar]
- Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: The contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sexually Transmitted Infections. 1999;75(1):3–17. doi: 10.1136/sti.75.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland AF, Hough RL, McCabe KM, Yeh M, Wood PA, Aarons GA. Prevalence of psychiatric disorders in youths across five sectors of care. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(4):409–418. doi: 10.1097/00004583-200104000-00009. [DOI] [PubMed] [Google Scholar]
- Hoyle RH, Fejfar MC, Miller JD. Personality and sexual risk taking: A quantitative review. Journal of Personality. 2000;68(6):1203–1231. doi: 10.1111/1467-6494.00132. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Rubio-Stipec M, Canino G, Bird HR, Dulcan MK, Schwab-Stone ME, Lahey BB. Parent and child contributions to diagnosis of mental disorder: Are both informants always necessary? Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(12):1569–1579. doi: 10.1097/00004583-199912000-00019. [DOI] [PubMed] [Google Scholar]
- Lawrence L, Levy SR, Rubinson L. Self-efficacy and AIDS prevention for pregnant teens. Journal of School Health. 1990;60:19–24. doi: 10.1111/j.1746-1561.1990.tb04771.x. [DOI] [PubMed] [Google Scholar]
- Lescano CM, Hadley WS, Beausoleil NI, Brown LK, D'eramo D, Zimskind A. A brief screening measure of adolescent risk behavior. Child Psychiatry and Human Development. 2007;37(4):325–336. doi: 10.1007/s10578-006-0037-2. [DOI] [PubMed] [Google Scholar]
- Lescano CM, Brown LK, Miller PM, Puster KL. Unsafe Sex: Do Feelings Matter? Journal of Prevention & Intervention in the Community. 2007;33(1–2):51–62. doi: 10.1300/J005v33n01_05. [DOI] [PubMed] [Google Scholar]
- Meade CS, Graff FS, Griffin ML, Weiss RD. HIV risk behavior among patients with co-occurring bipolar and substance use disorders: Associations with mania and drug abuse. Drug and Alcohol Dependence. 2008;92(1–3):296–300. doi: 10.1016/j.drugalcdep.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RA, Petukhova M, Kessler RC. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2007;64(5):543–552. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oregon Science Learning Center. Parental monitoring and supervision constructs (Technical reports) Eugene, OR: Oregon Social Learning Center; 1990. [Google Scholar]
- Prochaska JO, Redding CA, Harlow LL, Rossi JS. The transtheoretical model of change and HIV prevention: A review. Health Education Quarterly. 1994;21(4):471–486. doi: 10.1177/109019819402100410. [DOI] [PubMed] [Google Scholar]
- Ramrakha S, Caspi A, Dickson N, Moffitt TE, Paul C. Psychiatric disorders and risky sexual behaviour in young adulthood: Cross sectional study in birth cohort. British Medical Journal. 2000;321(7256):263–266. doi: 10.1136/bmj.321.7256.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Futterman D. Promoting early detection of human immunodeficiency virus infection among adolescents. Archives of Pediatric Adolescent Medicine. 2000;154(5):435–439. doi: 10.1001/archpedi.154.5.435. http://archpedi.ama-assn.org/ [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Sznitman SR, Carey MP, Vanable PA, DiClemente RJ, Brown LK, Valois RF, Romer D. The impact of community-based sexually transmitted infection screening results on sexual risk behaviors of African American adolescents. Journal of Adolescent Health. 2010;47(1):12–19. doi: 10.1016/j.jadohealth.2009.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]