Abstract
Background
Walking speed is an indirect marker of overall mobility performance. Data regarding its association with diet is lacking.
Objectives
To determine the association between the Mediterranean Diet (MedDiet) score with 20m walking-speed over 8 years.
Design
Health-ABC cohort study beginning in 1997–1998.
Setting and participants
We analyzed data of 2,225 well-functioning participants aged ≥70y.
Measurements
Walking-speed was assessed in relation to low, medium, and high adherence to the MedDiet (0–2, 3–5, 6–9 points, respectively).
Results
Individuals in the highest vs. the lowest MedDiet adherence groups were more likely to be men, less likely to be smokers, with lower BMI, higher energy intake and physical activity (p<0.05). Usual and rapid 20m walking speed were highest in the high MedDiet adherence group compared with the other groups, 1.19±0.19, 1.16±0.21, and 1.15±0.19m/s, respectively, (p=0.02) for usual speed and 1.65±0.30, 1.59±0.32, and 1.55±0.30m/s, respectively (p=0.001) for rapid speed. Over 8y, both usual and rapid 20m walking speed declined in all MedDiet adherence groups. Higher MedDiet adherence was an independent predictor of less decline in usual 20m walking speed (p=0.049) in Generalized Estimating Equations adjusted for age, race, gender, site, education, smoking, physical activity, energy intake, health status, depression, and cognitive score. The effect decreased after adding total body-fat-percent to the model (p=0.134). Similar results were observed for MedDiet adherence and rapid 20m walking speed; the association remained significant after adjustment for total body-fat-percent (p=0.012). In all models the interaction between time and MedDiet adherence was not significant.
Conclusion
Walking speed over 8 years was faster among those with higher MedDiet adherence at baseline. The differences remained significant over 8y, suggesting a long-term effect of diet on mobility performance with aging.
Keywords: walking speed, elderly, Mediterranean diet, dietary assessment, function
INTRODUCTION
The Mediterranean diet (MedDiet) is a model of healthy diet that represents the dietary pattern among populations from Mediterranean areas (1). It refers to a diet with consumption of large quantities of olives, fruits, vegetables as salads, cooked legumes, nuts, and cereals. Adherence to the MedDiet has been shown to be associated with decreased rates of cardiovascular disease (2), cancer (3), diabetes (4), hypertension (1, 5), inflammation, Alzheimer’s disease, depression (6), and all cause mortality (7–11).
The MedDiet was shown to have protective effects against cognitive functional decline or dementia in older individuals due to the combination of several potentially protective foods and nutrients, such as fish, monounsaturated fatty acids, vitamin B12 and folate, antioxidants (vitamin E, carotenoids, flavonoids) and moderate amounts of alcohol (12–17). Recently an analysis of the InChianti study indicates a protective effect of the MedDiet on decline in mobility over time (18). To our knowledge, the relationship of MedDiet pattern with physical functioning and age-related disability in non-Mediterranean countries has yet to be examined. Walking speed declines with age and is a well-accepted marker of overall mobility performance (19, 20) and a major predictor for morbidity and mortality (19–21). Walking slower may also be thought of as a compensatory strategy aimed at increasing stability, avoiding falls or reducing the energetic cost of mobility (21, 22).
Observational studies from the last few years have shown associations between frailty and low circulating levels of vitamin E and carotenoids (23–26). Carotenoids were shown to be protective against sarcopenia, a condition characterized by loss of skeletal muscle mass and strength with aging (25). These data suggest that a diet rich in antioxidants may be protective against physical decline and disability. The MedDiet is one example of such a diet due to the high content of carotenoids from fruits and vegetables.
We hypothesized that adherence to the MedDiet will be associated with slower decline in 20 m walking speed and that the association will be similar among long-term survivors.
SUBJECTS AND METHODS
Study Sample
The Health, Aging, and Body Composition (Health ABC) study is a prospective cohort study initiated by the Laboratory of Epidemiology, Demography and Biometry of the National Institute on Aging, U.S.A. and carried out by investigators from the University of Pittsburgh (Pittsburgh, PA) and the University of Tennessee (Memphis). The study investigates the relations among health conditions, body composition, behavioral and social factors, and physical function in older adults. Participants (n=3075) aged 70–79 years were recruited from a random sample of White Medicare beneficiaries and all age-eligible Black community residents to participate in the Health ABC study in 1997–1998. Eligibility criteria included self-reporting no difficulty in walking a distance of ¼ mile (0.4 km) or climbing 10 stairs, independently performing mobility related activities of daily living, having plans to live in the area for the next 3 years, and having no evidence of life-threatening illnesses.
All participants having dietary assessment at year 2 (when dietary intake was measured) and 20m usual walking speed data were included in the analysis, leaving 2,225 participants for the analyses. We repeated the analyses in participants who survived 10 years in the study (survivors; n=1207) to see if effects in long term survivors were similar. The study was approved by the Institutional Review Boards of the University of Pittsburgh, University of Tennessee and UCSF, and participants provided written informed consent.
Walking speed
Performance-based evaluations included usual and rapid walking speed assessed over a 20 m course. Participants were asked first to walk at their “usual walking pace” and then “as fast as [they] can” for the return trip; time recorded to the hundredth of a second was divided by 20 to obtain usual and rapid speed in meters per second. Walking speed in general and specifically 20m walking speed are widely used in geriatric studies. In a recent meta-analysis by Studensky et al. (21) including data of 34,485 participants from 9 studies, gait speed was shown as a strong predictor of mortality. In the Health ABC, 20 m walking speed was the most consistent measurement of walking speed; therefore it was used in the current analysis.
Dietary assessment
A modified 108 item Block Food Frequency Questionnaire (FFQ) (27) was administered by trained dietary interviewers at the year 2 follow-up visit. Nutrients intake was assessed for each of the 108 items in the FFQ. The nutrient content including macronutrients, vitamins, and minerals including carotenoids and vitamin E was determined for one serving of each food and that was multiplied by the daily frequency of consumption of the food. The calculation of glycemic index (GI) was described in detail by Sahyoun et al. (28). Briefly, the amount of available carbohydrate in one serving of each food was determined. Each food’s GI was multiplied by the daily frequency of consumption of the food, and these products were summed over all foods.
Adherence to the MedDiet was appraised according to the score created by Trichopoulou et al (8, 9): high ratio of monounsaturated:saturated fatty acids, moderate intake of alcohol, high intake of legumes, high intake of grains, high intake of fruit and nuts, high intake of vegetables, low intake of meat and meat products, moderate intake of milk and dairy products and high intake of fish. The index assigns a score of 0 or 1 according to the daily intake of each of the nine components. With the exception of alcohol, the sex specific medians of the sample were used as cut-points and the unit of measurement was servings per day. For each of the six protective components (fatty acid ratio, legumes, grains, fruits, vegetables, and fish) participants received one point if their intake was over the sample median. Participants received one point if their intake was below the median for the two non-protective components (dairy products or meat).
For alcohol, one point was scored if mean consumption was 10–50 g/day for men or 5–25 g/day for women. Participants meeting all the characteristics of the MedDiet received a score of nine points, reflecting maximum adherence.
Using sensitivity analysis of our data and based on data from other studies (12), we divided the score into three levels: 0–2 indicating low adherence, 3–5 indicating medium adherence, and 6–9 indicating high adherence.
Other measurements
Sociodemographic measurements included age, sex, race (Black or White), study site (Memphis or Pittsburgh), education (<high school, high school graduate, and >high school), and marital status (married, not currently married). Smoking was assessed at the baseline Health ABC clinic visit. Self-reported health status was reclassified into 2 categories. “Fair” and “Poor” were grouped together as “1”. “Good”, “Very good”, and “Excellent” were classified as “0”. Body fat, body weight, and height were measured at the year 2 visit. Body fat percent was assessed using dual-energy x-ray absorptiometry (QDR-4500, version 8.21, Hologic Inc., Bedford, MA) and calculated as the ratio of body fat mass to total mass (percentage of body fat). Body weight was measured on a calibrated balance beam scale with the individual wearing a clinic gown and with shoes removed. Height was measured with a stadiometer. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared.
Physical activity over the past 7 days was assessed by questionnaire during an interview (29). Time spent climbing stairs, walking for exercise, walking for other purposes, aerobics, weight or circuit training, high-intensity exercise activities, and moderate-intensity exercise activities were obtained and information on the intensity level at which each activity was performed. A metabolic equivalent value was assigned to each activity and intensity combination and was used to calculate the number of kilocalories per week spent on those activities (30).
The following self-reported medical conditions were confirmed by treatment and/or medication: cerebrovascular disease, heart disease, diabetes, and hypertension. Participants were instructed to bring all prescription and over-the-counter medications used in the past 2 weeks with them to the clinic visit and the total number of medications was calculated.
Depressed mood was assessed using the Center for Epidemiologic Studies Depression scale (31) and cognitive status was assessed using the Modified Mini-Mental State Examination (3MS) score (32).
Measures of interleukin-6 (IL-6) and C-reactive protein (CRP) were obtained from frozen stored plasma or serum. Specimens were obtained by venipuncture in the morning after an overnight fast, processed, aliquoted into cryovials, frozen at −70°C, and subsequently shipped to the Health ABC Core Laboratory at the University of Vermont. Cytokine levels were measured in duplicate using ELISA kits (R&D Systems, Minneapolis, MN, USA). The HS600 Quantikine kit was used to measure IL-6 with a detectable limit of 0.10 pg/ml. Serum levels of high-sensitivity CRP were measured in duplicate by ELISA based on purified protein and polyclonal anti-CRP antibodies (Calbiochem, San Diego, CA, USA). The CRP assay was standardized according to the World Health Organization’s First International Reference Standard, with a sensitivity of 0.08 μg/ml. Reliability, as determined by blind duplicate analyses of IL-6 and CRP, revealed average interassay coefficients of variation of 10.3% and 8.0%, respectively (33, 34).
Statistical analyses
Participant characteristics by MedDiet score were compared using chi-square analysis or ANOVA as appropriate. Differences in dietary intake, usual and rapid walking speed, and walking ability across the three MedDiet categories at baseline were evaluated using ANOVA. Generalized Estimating Equations (GEE) model was used to test the main effect of MedDiet score on usual and rapid 20 meter walk over an 8 year period using 4 models with hierarchical adjustments. The models estimated the change in walking speed over time, allowing person-specific differences in walking speed at baseline and rate of walking speed decline. The first model was adjusted for demographic characteristics. The second model was adjusted for the variables in model 1 plus life style indicator levels of physical activity and energy intake. The third model was adjusted for the variables in models 1 and 2 plus health status, cognitive function, and depression. The fourth model was adjusted for the variables above plus total body fat percent. The analysis was run using the GENMOD procedure of SPSS. This procedure uses all available observations per case. We studied the effect of missing walking speed data by comparison of baseline profile of the cases that have and do not have walking speed in each year.
RESULTS
The analyses were performed on 2225 people for whom data on 20 m walking speed and dietary intake were available. For the 2225 subjects, we used all available observations. This gave us for the analysis 2225 cases with a total of 8358 (70%) available observations. During the 5 time points, the cohort had shrunk and the percentage of cases contributing a measurement at each point is 100%, 85%, 77%, 61%, and 54%. We compared the profile of cases missing walking speed information at later follow-up times and found that they had somewhat different demographic characteristics (older, more White females, more smokers, and less educated) and on average, they had more depressive symptoms with lower cognitive score.
Descriptive and health characteristics of our participants across MedDiet adherence categories are presented in Table 1. Significant differences were shown in gender, marital status, smoking prevalence, BMI, energy intake, body fat percent, and weekly physical activity. Participants in the highest vs. the lowest MedDiet adherence groups were more likely to be men and non-smokers, with lower BMI, higher energy-intake, and physical activity, and a lower use of medications. No difference was shown in the distribution of age, race, education, subjective health status, cognitive function, and depression score. The prevalence of chronic diseases did not differ by MedDiet score, except for a higher prevalence of heart disease among the higher MedDiet score group. Levels of CRP were significantly lower among the highest MedDiet adherence group. The same trend was shown in the IL6 levels.
Table 1.
Baseline demographic, clinical, and dietary characteristics and functional performance by categories of MedDiet score (N =2225).
| Characteristic | Mediterranean diet score, No. (%)
|
P-value | ||
|---|---|---|---|---|
| Low (0–2) N=809 |
Middle (3–5) N=1303 |
High (6–9) N=113 |
||
| Age, mean (SD) | 74.5 (2.8) | 74.6 (2.9) | 74.6 (2.7) | 0.92 |
|
| ||||
| Men, n (%) | 371(45.9) | 677 (52) | 66 (58.4) | 0.005 |
|
| ||||
| Black, n (%) | 262 (39.2) | 707 (39.2) | 85 (35.6) | 0.5 |
|
| ||||
| Pittsburgh site, n (%) | 426 (52.7) | 635 (48.7) | 59 (52.2) | 0.20 |
|
| ||||
| Married, n (%) | 385 (48.0) | 742 (56.9) | 64 (56.6) | <0.01 |
|
| ||||
| Over 12 years of school, n (%) | 624 (78.1) | 1027 (78.94) | 93 (82.3) | 0.59 |
|
| ||||
| Smoking | 0.012 | |||
| Never | 353 (43.6) | 597 (45.8) | 51 (45.1) | |
| Former | 363 (44.9) | 614 (47.2) | 54 (47.8) | |
| Current | 93 (11.5) | 92 (7.1) | 8 (7.1) | |
|
| ||||
| BMI, mean (SD) | 27.4 (4.6) | 26.9 (4.6) | 26.1 (4.2) | 0.008 |
|
| ||||
| Energy intake (Kcal/day), mean (SD) | 1566.1 (593.2) | 2040.6 (774.0) | 2500 (936.1) | <0.001 |
|
| ||||
| Weekly physical activity | 0.02 | |||
| Low, n (%) | 207 (26.0) | 269 (20.7) | 17 (15.0) | |
| Medium, n (%) | 401 (50.0) | 682 (52.4) | 63 (55.8) | |
| High, n (%) | 194 (24.2) | 350 (26.9) | 33 (29.2) | |
|
| ||||
| Total body fat %, mean (SD) | 35.8 (7.6) | 34.3 (7.6) | 32.4 (7.6) | <0.001 |
|
| ||||
| Depression CESD score, mean (SD) | 4.7 (5.6) | 4.2 (4.7) | 4.3 (5.0) | 0.17 |
|
| ||||
| Teng-Minimental score, mean (SD) | 90.9 (7.7) | 91.1 (7.4) | 90.2 (9.9) | 0.42 |
|
| ||||
| Fair-Poor health status, n (%) | 95 (11.8) | 146 (11.2) | 8 (7.1) | 0.34 |
|
| ||||
| Number of medications, mean (SD) | 2.8 (2.3) | 3.1 (2.6) | 2.6 (2.5) | 0.05 |
|
| ||||
| IL-6 (pg/ml), median (Q1, Q3)a | 1.8 (1.2, 2.7) | 1.7 (1.2, 2.6) | 1.5 (1.0, 2.5) | 0.02 |
|
| ||||
| CRP (mg/ml), median (Q1, Q3) a | 1.7 (1.0, 3.1) | 1.5 (1.0, 2.8) | 1.3 (0.9, 2.2) | 0.004 |
|
| ||||
| Cerebrovascular disease, n (%) | 26 (3.3) | 27 (2.1) | 5 (4.6) | 0.09 |
|
| ||||
| Heart disease, n (%) | 32 (4.1) | 32 (2.5) | 8 (7.3) | 0.023 |
|
| ||||
| Diabetes, n (%) | 92 (11.4) | 191 (14.7) | 12 (10.6) | 0.066 |
|
| ||||
| Hypertension, n (%) | 298 (36.8) | 493 (37.8) | 33 (29.2) | 0.12 |
Kruskal-Wallis non-parametric test was used
Table 2 presents the daily dietary intake of antioxidants, servings of MedDiet components, and glycemic index by MedDiet score. As expected, the dietary intake of the MedDiet components was significantly higher among the highest MedDiet group except for milk and dairy. The dietary intake of antioxidants (vitamin E and carotenoids) was significantly higher among the highest MedDiet score group, whereas the daily glycemic index of the diet was slightly higher.
Table 2.
Daily dietary intake of selected nutrients and servings by MedDiet score.
| Characteristic | Mediterranean diet score, mean (SD) | P-value | ||
|---|---|---|---|---|
| Low (0–2) N=809 |
Middle (3–5) N=1303 |
High (6–9) N=113 |
||
| Antioxidants and glycemic index | ||||
| Vitamin E (mg) | 8.7 (5.0) | 12.3 (7.2) | 16.1 (7.8) | <0.001 |
| Beta-Carotene (mcg) | 2360.5 (1553.7) | 3909.1 (2850.3) | 5956.4 (3816.3) | <0.001 |
| Cryptoxanthin (mcg) | 157.0 (129.9) | 186.3 (153.6) | 233.5 (159.8) | <0.001 |
| Lutein (mcg) | 1262.6 (1078.8) | 2039.4 (1768.0) | 2920.1 (2379.4) | <0.001 |
| Lycopene (mcg) | 3103.2 (5080.7) | 4574.1 (5479.2) | 7167.0 (8034.8) | <0.001 |
| Daily Glycemic Index (glucose scale) | 55. 8 (4.5) | 56.7 (4.1) | 56.1 (3.8) | <0.001 |
| Servings of MedDiet components | ||||
| Legumes (0.25 cup equivalents) | 0.1 (0.3) | 0.7 (1.1) | 1.3 (1.1) | <0.001 |
| Alcohol (gr/day)* | 3.6 (11.8) | 4.8 (10.4) | 7.9 (10.4) | <0.001 |
| Meat (1 ounce equivalent) | 2.1 (1.8) | 2.8 (2.4) | 3.5 (3.0) | <0.001 |
| Fish (1 ounce equivalent) | 0.02 (0.2) | 0.2 (0.9) | 0.9 (1.3) | <0.001 |
| Fruits and nuts (1 cup equivalents of fruits and 0.5 ounce of nuts) | 0.8 (0.6) | 1.3 (0.8) | 2.0 (1.0) | <0.001 |
| Milk and dairy products (1 cup equivalent) | 1.5 (1.2) | 1.4 (1.2) | 1.2 (1.3) | <0.001 |
| Vegetables (1 cup equivalents) | 1.1 (0.7) | 1.7 (0.9) | 2.3 (1.1) | <0.001 |
| Grains (ounce equivalents) | 5.1 (2.4) | 7.3 (3.2) | 8.9 (3.3) | <0.001 |
| Monounsaturated fat/Saturated fat ratio | 1.2 (0.2) | 1.4 (0.25) | 1.5 (0.25) | <0.001 |
Alcohol in grams was calculated from the different alcoholic beverages per ounce – beer 1.1, wine 2.6, and 9 for other drinks.
Table 3 depicts baseline differences in walking ability measured by different methods across the MedDiet score. Both usual and rapid 20 m walking speed were significantly higher among the highest MedDiet score participants. People in the highest MedDiet score group tended to be more physically active, with a significantly higher percent walking over 150 minutes per week and fewer reporting difficulty walking a quarter of a mile.
Table 3.
Gait speed and walking ability at baseline by MedDiet score.
| Characteristic | Mediterranean diet score, No. (%) | P-value* | ||
|---|---|---|---|---|
| Low (0–2) N=809 |
Middle (3–5) N=1303 |
High (6–9) N=113 |
||
| Usual gait speed (20m walk) m/sec | 1.15 (0.19) | 1.16 (0.21) | 1.19 (0.19) | 0.02 |
| Rapid gait speed (20m walk) m/sec | 1.55 (0.31) | 1.59 (0.32) | 1.65 (0.30) | 0.001 |
| Walking > 150 minutes per week, n (%) | 225 (27.9) | 429 (33.0) | 46 (40.7) | 0.014 |
| Reports difficulty walking a quarter of a mile, n (%) | 208 (21.4%) | 247 (16.0%) | 11 (8.5%) | <0.001 |
| Reports difficulty walking 1 mile, n (%) | 115 (11.8%) | 204 (13.2%) | 18 (14.0%) | 0.53 |
P-value for linear trend
Table 4 presents the results of GEE models to predict decline in usual and rapid walking speed over time by MedDiet score. Both usual and rapid 20 m walking speed declined over time in all models (p<0.01). The first model was adjusted for age, race, gender, education, site, smoking status, and a time by MedDiet score interaction term; in the second and third models we showed a significant difference in the usual walking speed across MedDiet scores (p=0.013, p=0.012, and p=0.049, respectively). However, in model 4 when total body fat percent was added, the difference in walking speed was attenuated (p=0.134). Similar results were observed for the association between MedDiet adherence score and rapid 20 m walking speed (p=0.01, p=0.003, and p<0.001, respectively); however, the association remained significant after adjustment for total body fat percent (p<0.012). In all models, the MedDiet by time interaction term was not significant. The best fitting models were chosen to be presented.
Table 4.
Usual and rapid 20m walking speed by 3 levels of adherence to the MedDiet over 8 years (N=2225) using 4 mixed models
| Test | Model 1a | Model 2b | Model 3c | Model 4d | ||||
|---|---|---|---|---|---|---|---|---|
| β (SE) | P-value | β (SE) | P-value | β (SE) | P-value | β (SE) | P-value | |
|
Usual 20m walking speed (m/sec)
| ||||||||
| Year 2 | Reference | Reference | Reference | Reference | ||||
| Year 4 | 0.03 (0.02) | 0.06 (0.02) | 0.036 (0.20) | 0.027 (0.018) | ||||
| Year 6 | −0.05 (0.02) | <0.001 | −0.02 (0.02) | <0.001 | −0.05 (0.018) | <0.001 | −0.05 (0.018) | <0.001 |
| Year 8 | −0.14 (0.022) | −0.11 (0.022) | −0.14 (0.022) | −0.142 (0.022) | ||||
| Year 10 | −0.17 (0.024) | −0.15 (0.024) | −0.18 (0.024) | −0.175 (0.024) | ||||
|
Mediterranean diet score
| ||||||||
| Score 0–2 | −0.03 (0.02) | 0.013 | −0.03 (0.02) | 0.012 | −0.014 (0.02) | 0.049 | −0.01 (0.02) | 0.134 |
| Score 3–5 | −0.014 (0.02) | −0.01 (0.02) | −0.008 (0.02) | −0.006 (0.08) | ||||
| Score 6–9 | Reference | Reference | Reference | Reference | ||||
| MedDiet score*time | 0.173 | 0.081 | 0.202 | 0.372 | ||||
|
Rapid 20m walking speed (m/sec)
| ||||||||
| Year 2 | Reference | Reference | Reference | Reference | ||||
| Year 4 | −0.009 (0.2) | −0.04 (0.02) | −0.008 (0.02) | −0.008 (0.02) | ||||
| Year 6 | −0.066 (0.03) | <0.001 | −0.12 (0.03) | <0.001 | −0.085 (0.02) | <0.001 | −0.084 (0.02) | <0.001 |
| Year 8 | −0.144 (0.03) | −0.19 (0.028) | −0.16 (0.029) | −0.15 (0.03) | ||||
| Year 10 | −0.144 (0.028) | −0.20 (0.03) | −0.17 (0.03) | −0.16 (0.03) | ||||
|
Mediterranean diet score
| ||||||||
| Score 0–2 | −0.02 (0.03) | <0.001 | −0.06 (0.03) | 0.003 | −0.03 (0.03) | <0.001 | −0.02 (0.03) | 0.012 |
| Score 3–5 | −0.003 (0.03) | −0.04 (0.03) | −0.02 (0.03) | −0.01 (0.03) | ||||
| Score 6–9 | Reference | Reference | Reference | Reference | ||||
| MedDiet score*time | 0.492 | 0.488 | 0.458 | 0.557 | ||||
Model is adjusted for age, race, gender, education, site, smoking status, time*MedDiet score
Model is adjusted for covariates in model 1 plus physical activity, and energy intake
Model is adjusted for covariates in model 2 plus health status, depression and cognition
Model is adjusted for covariates in model 3 plus total body fat percent
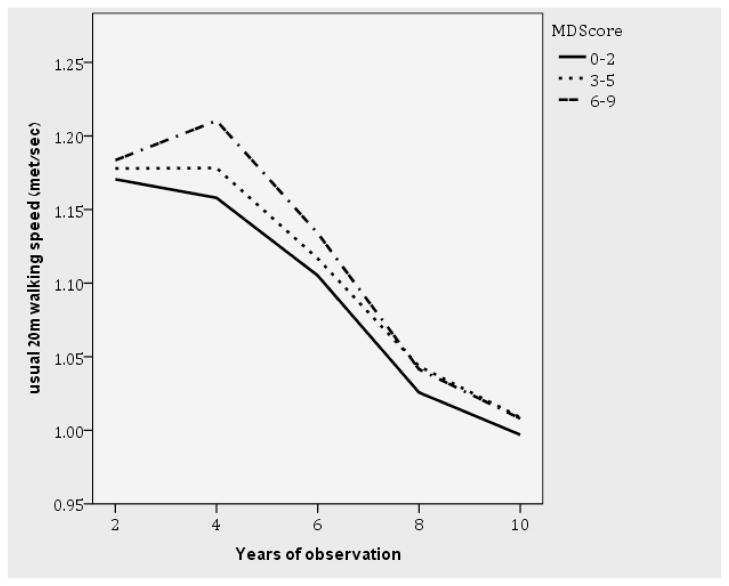
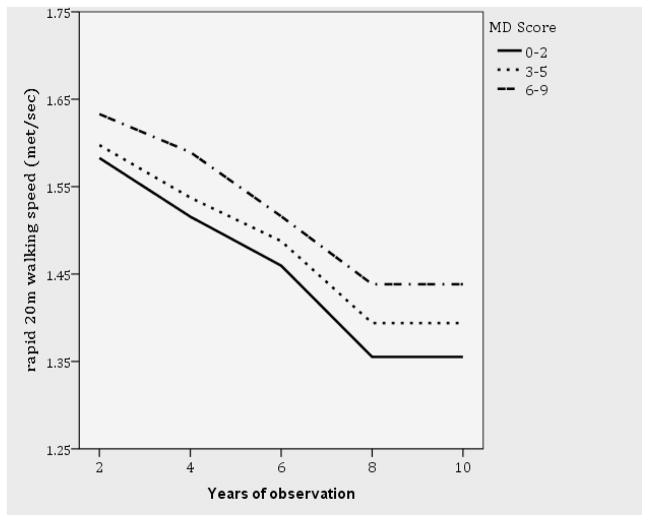
Figure 1a and b depict the final mixed-models of the decline in usual (Figure 1a) and rapid (Figure 1b) 20 m walking speed across MedDiet score adjusted for age, race, gender, education, site, smoking status, time by MedDiet score interaction term, physical activity, energy intake, health status, depression, cognition, and total body fat percent (p=0.134 for the difference in usual 20 m walking speed and p=0.012 for rapid 20 m walking speed). We repeated the analyses for participants for whom data were available on their 20m usual and rapid walking speed at year 10 (survivors). Among this group (n=1207), no association was found between usual walking speed and the MedDiet adherence category, while a strong relationship was detected between rapid walking speed and MedDiet in all models (p=0.005, 0.002, 0.004, and 0.016 for models 1–4, respectively).
Figure 1. Usual and rapid 20m walking speed by 3 levels of adherence to the MedDiet over 8 years (N=2225).
Figure 1a. Usual 20m walking speed by 3 levels of adherence to the MedDiet over 8 years- final model-adjusted for age, race, gender, education, site, smoking status, time*MedDiet score, physical activity, energy intake, health status, depression, cognition and total body fat percent (MD P=0.134)
Figure 1b. Rapid 20m walking speed by 3 levels of adherence to the MedDiet over 8 years-final model-adjusted for age, race, gender, education, site, smoking status, time*MedDiet score, physical activity, energy intake, health status, depression, cognition and total body fat percent (MD P=0.012)
DISCUSSION
In this long-term cohort study we addressed the association between physical performance captured by 20 m walking speed over 8 years and MedDiet. Over 8 years of follow-up, both usual and rapid 20 m walking speed declined in the three MedDiet adherence groups; however, the group with the highest adherence to the MedDiet performed better at all time points. Among those who survived to perform the test in year 10 of the study (survivors), higher MedDiet adherence score was related only to rapid 20 m walking speed.
In a recent publication from the InChianti study, a population-based study of older adults in the Chianti region of Tuscany, Italy, (18) the MedDiet was shown to be associated with a slower decline of mobility over time in community-dwelling older persons. Mobility was assessed using the Short Physical Performance Battery (SPPB) that includes gait speed as one of 3 indicators of mobility. Our findings in a non-Mediterranean country are in accord with these findings. Thus a combination of MedDiet components is a strong element of dietary exposure even in a non-Mediterranean country, namely the U.S.
Walking speed is an indirect measure of lower extremity function (35, 20) that is highly predictive of subsequent disability in various older populations (20, 35, 36). In a study by Shinkai et al., (35) out of several measurements to assess physical performance, usual walking speed was the most sensitive in predicting the onset of functional dependence for older people. To date several reports have shown that walking speed is highly predictive of future disability and mortality in non-disabled older people (20, 21, 36–38). Thus in the current study, usual and rapid 20m walking speed were chosen as ancillary indicators for physical performance over time.
Muscle strength and muscle mass are important predictors of walking speed. In advanced age both may be decreased due to cumulative oxidative stresses. The latter in turn may be related to several nutritional factors (25, 26). There is some evidence that excessive oxidative stress is involved in the pathogenesis of age-related muscle mass loss and subsequent decrease of strength and mobility (39, 40). In a study performed by Semba et al. among older women with high oxidative stress, as indicated by oxidative damage to proteins, oxidative stress was shown as an independent predictor of decrease in walking speed and progression to severe walking disability (25, 41). A group of nutrients that has a potential impact on oxidative stress is the carotenoids. Our nutritional analyses (Table 2) show significantly higher intake of carotenoids such as β-carotene, crytoxanthin, lutein, and lycopene among the highest MedDiet adherence group. Dietary carotenoids comprise an important component of the antioxidant defense system in humans. Low serum/plasma carotenoids are independently associated with poor skeletal muscle strength and impaired physical performance (25). In the InChianti study, beta-carotene intake was positively associated with physical performance (42). Another finding that stands out in our results is the intake of fish. The intake of fish in our study in the highest MedDiet score group was 40-fold higher than in the lowest score group. Fish intake was shown to be related to higher grip strength (43). These findings imply that a diet based on high consumption of fruits and vegetables, and supposedly fish, may affect physical performance. The exposure to the above dietary compounds is gathered in the Mediterranean composite score, which includes a higher consumption of fruits, vegetables, fish, and olive or canola oils.
In older adults, studies demonstrate an inverse relationship between physical function and individual inflammatory biomarkers. The MedDiet was shown in several studies to be negatively related to inflammatory markers (25). Results in the same direction were shown in two clinical trials. Esposito et al. showed a significant reduction of inflammatory markers in an intervention group with MedDiet compared with a control group (44). These findings were repeated in the PREDIMED study in Spain. The consumption of some typical Mediterranean foods (fruits, cereals, virgin olive oil, and nuts) was associated with lower serum concentrations of inflammatory markers, especially those related to endothelial function, in subjects with high cardiovascular risk living in a Mediterranean country (45). In our findings, the intake of monounsaturated fatty acids, from olive and canola oil, was higher among the highest MedDiet score. CRP was significantly lower with a trend for lower IL6 levels among participants in the highest MedDiet adherence score, suggesting that the association between MedDiet and lower level of inflammation may affect physical performance measured by walking speed.
Our study merits discussion of some limitations. The main limitation is the lack of continuous evaluation of the diet. The FFQ was administered only once at the year 2 visit and thus we cannot rule out changes in the diet prior to the baseline assessment. For example, the higher prevalence of cardiovascular disease among the higher adherence MedDiet score may indicate changes in dietary exposure due to health reasons prior to assessment. However, the FFQ captures long-term dietary intake and, thus, has been used in wide range of cohort studies. The assumption that underlies the development and use of the FFQ method is that the diet of adults is stable, particularly in old age (46). Therefore, we can assume that the diet of our participants did not change significantly prior to baseline assessment and over the course of the study, and that the participants’ diets were indeed represented in the FFQ. The second limitation of our study is that we chose walking speed as a singular composite parameter rather than dissecting it to its components, namely SPPB (Short Physical Performance Battery), muscle strength, reaction time, and integrity of the neurological motor system. Our choice was to determine the association between MedDiet and a physiological functional score. Since some of these measurements are available in Health ABC, future research can further dissect these functional parameters and provide further mechanistic insights on how MedDiet affects locomotion. The study was performed among relatively healthy elderly population. Thus our results cannot be generalized to the entire elderly population. Nonetheless, our population reflects a fairly wide segment of elderly, higher functioning individuals.
CONCLUSIONS
MedDiet was previously shown to be associated with longevity (9, 10, 47), cognitive function and Alzheimer diseases, physical function and other chronic diseases (1, 2, 12, 14). Our study provides data that relate the MedDiet to aging-associated declines in mobility performance. Walking speed over 8 years was greater among those with higher MedDiet adherence at baseline. The differences remained significant over 8 years suggesting a long-term effect of diet on mobility performance with aging.
Acknowledgments
This research was supported by National Institute on Aging (NIA) contracts N01-AG-6-2101, N01-AG-6-2103, and N01-AG-6-2106; NIA grant RO1-AG028050 and NINR grant RO1-NR012459. This research was supported in part by the Intramural Research Program of the NIH, National Institute on Aging.
Sponsor’s Role: The sponsor was not involved in the design, methods, subject recruitment, data collections, analysis, or preparation of the paper.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Danit Shahar, Denise Houston, Trisha Hue, Jung-Sun Lee, Nadine Sahyoun, Frances Tylavsky, Diklah Geva, Hillel Vardi, Tamara Harris
Author Contributions:
Danit Shahar conceptualized the idea, analyzed the data, and wrote the first draft of the manuscript. Denise Houston contributed to the conceptualization of the idea, interpreted the data, and contributed to drafts of the manuscript. Diklah Geva and Hillel Vardi were responsible for the statistical analyses and interpretation of the results and reviewed drafts of the manuscript. Tamara Harris, Jung-Sun Lee and Nadine Sahyoun were in charge of the nutritional part of the manuscript and reviewed drafts of the manuscript. Frances Tylavsky is a co-investigator of the Health ABC study, contributed to the data collection, interpreted the results, and reviewed drafts of the paper. Trisha Hue (project officer at NIA) contributed to the conceptualization of the idea, interpreted the data, and contributed to drafts of the manuscript. All authors approved the last version of the manuscript.
References
- 1.Psaltopoulou T, Naska A, Orfanos P, et al. Olive oil, the Mediterranean diet, and arterial blood pressure: The Greek European Prospective Investigation into Cancer and Nutrition (EPIC) study. Am J Clin Nutr. 2004;80:1012–1018. doi: 10.1093/ajcn/80.4.1012. [DOI] [PubMed] [Google Scholar]
- 2.Panagiotakos DB, Pitsavos C, Polychronopoulos E, et al. Can a Mediterranean diet moderate the development and clinical progression of coronary heart disease? A systematic review. Med Sci Monit. 2004;10:RA193–198. [PubMed] [Google Scholar]
- 3.de Lorgeril M, Salen P, Martin JL, et al. Mediterranean dietary pattern in a randomized trial: Prolonged survival and possible reduced cancer rate. Arch Intern Med. 1998;158:1181–1187. doi: 10.1001/archinte.158.11.1181. [DOI] [PubMed] [Google Scholar]
- 4.Biesalski HK. Diabetes preventive components in the Mediterranean diet. Eur J Nutr. 2004;43:26–30. doi: 10.1007/s00394-004-1106-6. [DOI] [PubMed] [Google Scholar]
- 5.Bondia-Pons I, Schroder H, Covas MI, et al. Moderate consumption of olive oil by healthy European men reduces systolic blood pressure in non-Mediterranean participants. J Nutr. 2007;137:84–87. doi: 10.1093/jn/137.1.84. [DOI] [PubMed] [Google Scholar]
- 6.Sanchez-Villegas A, Delgado-Rodriguez M, Alonso A, et al. Association of the Mediterranean dietary pattern with the incidence of depression: The Seguimiento Universidad de Navarra/University of Navarra follow-up (SUN) cohort. Arch Gen Psychiatry. 2009;66:1090–1098. doi: 10.1001/archgenpsychiatry.2009.129. [DOI] [PubMed] [Google Scholar]
- 7.Mitrou PN, Kipnis V, Thiebaut AC, et al. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: Results from the NIH-AARP diet and health study. Arch Intern Med. 2007;167:2461–2468. doi: 10.1001/archinte.167.22.2461. [DOI] [PubMed] [Google Scholar]
- 8.Trichopoulou A, Vasilopoulou E. Mediterranean diet and longevity. Br J Nutr. 2007;84:S205–S209. doi: 10.1079/096582197388554. [DOI] [PubMed] [Google Scholar]
- 9.Trichopoulou A, Costacou T, Bamia C, et al. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348:2599–2608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- 10.Knoops KTB, de Groot LC, Kromhout D, et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: The HALE project. JAMA. 2004;292:1433–1439. doi: 10.1001/jama.292.12.1433. [DOI] [PubMed] [Google Scholar]
- 11.Keys A, Menotti A, Karvonen MJ, et al. The diet and 15-year death rate in the seven countries study. Am J Epidemiol. 1986;124:903–912. doi: 10.1093/oxfordjournals.aje.a114480. [DOI] [PubMed] [Google Scholar]
- 12.Feart C, Samieri C, Rondeau V, et al. Adherence to a Mediterranean diet, cognitive decline, and risk of dementia. JAMA. 2009;302:638. doi: 10.1001/jama.2009.1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reynolds E. Vitamin B12, folic acid, and the nervous system. Lancet Neurol. 2006;5:949–960. doi: 10.1016/S1474-4422(06)70598-1. [DOI] [PubMed] [Google Scholar]
- 14.Solfrizzi V, Colacicco AM, D’Introno A, et al. Dietary intake of unsaturated fatty acids and age-related cognitive decline: A 8. 5-year follow-up of the Italian longitudinal study on aging. Neurobiol Aging. 2006;27:1694–1704. doi: 10.1016/j.neurobiolaging.2005.09.026. [DOI] [PubMed] [Google Scholar]
- 15.Stampfer MJ, Kang JH, Chen J, et al. Effects of moderate alcohol consumption on cognitive function in women. N Engl J Med. 2005;352:245–253. doi: 10.1056/NEJMoa041152. [DOI] [PubMed] [Google Scholar]
- 16.Engelhart MJ, Geerlings MI, Ruitenberg A, et al. Dietary intake of antioxidants and risk of Alzheimer disease. JAMA. 2002;287:3223–3229. doi: 10.1001/jama.287.24.3223. [DOI] [PubMed] [Google Scholar]
- 17.Letenneur L, Proust-Lima C, Le Gouge A, et al. Flavonoid intake and cognitive decline over a 10-year period. Am J Epidemiol. 2007;165:1364–1371. doi: 10.1093/aje/kwm036. [DOI] [PubMed] [Google Scholar]
- 18.Milaneschi Y, Bandinelli S, Corsi AM, et al. Mediterranean diet and mobility decline in older persons. Exp Gerontol. 2011;46:303–308. doi: 10.1016/j.exger.2010.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dumurgier J, Elbaz A, Ducimetiere P, et al. Slow walking speed and cardiovascular death in well functioning older adults: Prospective cohort study. Br Med J. 2009;339:b4460. doi: 10.1136/bmj.b4460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guralnik JM, Ferrucci L, Simonsick EM, et al. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duff-Raffaele M, Kerrigan DC, Corcoran PJ, et al. The proportional work of lifting the center of mass during walking. Am J Phys Med Rehabil. 1996;75:375–379. doi: 10.1097/00002060-199609000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Semba RD, Bartali B, Zhou J, et al. Low serum micronutrient concentrations predict frailty among older women living in the community. J Gerontol A Biol Sci Med Sci. 2006;61:594–599. doi: 10.1093/gerona/61.6.594. [DOI] [PubMed] [Google Scholar]
- 24.Ble A, Cherubini A, Volpato S, et al. Lower plasma vitamin E levels are associated with the frailty syndrome: The InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2006;61:278–283. doi: 10.1093/gerona/61.3.278. [DOI] [PubMed] [Google Scholar]
- 25.Semba RD, Ferrucci L, Sun K, et al. Oxidative stress and severe walking disability among older women. Am J Med. 2007;120:1084–1089. doi: 10.1016/j.amjmed.2007.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Semba RD, Blaum C, Guralnik JM, et al. Carotenoid and vitamin E status are associated with indicators of sarcopenia among older women living in the community. Aging Clin Exp Res. 2003;15:482–487. doi: 10.1007/BF03327377. [DOI] [PubMed] [Google Scholar]
- 27.Block G, Hartman AM, Dresser CM, et al. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 28.Sahyoun NR, Anderson AL, Kanaya AM, et al. Dietary glycemic index and load, measures of glucose metabolism, and body fat distribution in older adults. Am J Clin Nutr. 2005;82:547–552. doi: 10.1093/ajcn.82.3.547. [DOI] [PubMed] [Google Scholar]
- 29.Brach JS, Simonsick EM, Kritchevsky S, et al. The association between physical function and lifestyle activity and exercise in the health, aging and body composition study. J Am Geriatr Soc. 2004;52:502–509. doi: 10.1111/j.1532-5415.2004.52154.x. [DOI] [PubMed] [Google Scholar]
- 30.Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: Classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Beekman ATF, Deeg D, Van Limbeek J, et al. Criterion validity of the center for epidemiologic studies depression scale (CES-D): Results from a community-based sample of older subjects in the Netherlands. Psychol Med. 1997;27:231–235. doi: 10.1017/s0033291796003510. [DOI] [PubMed] [Google Scholar]
- 32.McDowell I, Kristjansson B, Hill G, et al. Community screening for dementia: The mini mental state exam (MMSE) and modified mini-mental state exam (3MS) J Clin Epidemiol. 1997;50:377–383. doi: 10.1016/s0895-4356(97)00060-7. [DOI] [PubMed] [Google Scholar]
- 33.Rao KM, Pieper CS, Currie MS, et al. Variability of plasma IL-6 and crosslinked fibrin dimers over time in community dwelling elderly subjects. Am J Clin Pathol. 1994;102:802–805. doi: 10.1093/ajcp/102.6.802. [DOI] [PubMed] [Google Scholar]
- 34.Macy EM, Hayes TE, Tracy RP. Variability in the measurement of C-reactive protein in healthy subjects: Implications for reference intervals and epidemiological applications. Clin Chem. 1997;43:52–58. [PubMed] [Google Scholar]
- 35.Shinkai S, Watanabe S, Kumagai S, et al. Walking speed as a good predictor for the onset of functional dependence in a Japanese rural community population. Age Ageing. 2000;29:441–446. doi: 10.1093/ageing/29.5.441. [DOI] [PubMed] [Google Scholar]
- 36.Ostir GV, Markides KS, Black SA, et al. Lower body functioning as a predictor of subsequent disability among older Mexican Americans. J Gerontol A Biol Sci Med Sci. 1998;53:M491–495. doi: 10.1093/gerona/53a.6.m491. [DOI] [PubMed] [Google Scholar]
- 37.Sonn U. Longitudinal studies of dependence in daily life activities among elderly persons. Scand J Rehabil Med. 1996;34:S1–35. [PubMed] [Google Scholar]
- 38.Cesari M, Kritchevsky SB, Penninx B, et al. Prognostic value of usual gait speed in well-functioning older people-results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53:1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 39.Pansarasa O, Bertorelli L, Vecchiet J, et al. Age-dependent changes of antioxidant activities and markers of free radical damage in human skeletal muscle. Free Radic Biol Med. 1999;27:617–622. doi: 10.1016/s0891-5849(99)00108-2. [DOI] [PubMed] [Google Scholar]
- 40.Mecocci P, Fano G, Fulle S, et al. Age-dependent increases in oxidative damage to DNA, lipids, and proteins in human skeletal muscle. Free Radic Biol Med. 1999;26:303–308. doi: 10.1016/s0891-5849(98)00208-1. [DOI] [PubMed] [Google Scholar]
- 41.Semba R, Ricks M, Ferrucci L, et al. Low serum selenium is associated with anemia among older adults in the United States. Eur J Clin Nutr. 2007;63:93–99. doi: 10.1038/sj.ejcn.1602889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cesari M, Pahor M, Bartali B, et al. Antioxidants and physical performance in elderly persons: The Invecchiare in Chianti (InCHIANTI) study. Am J Clin Nutr. 2004;79:289–294. doi: 10.1093/ajcn/79.2.289. [DOI] [PubMed] [Google Scholar]
- 43.Robinson SM, Jameson KA, Batelaan SF, et al. Diet and its relationship with grip strength in community-dwelling older men and women: The Hertfordshire cohort study. J Am Geriatr Soc. 2008;56:84–90. doi: 10.1111/j.1532-5415.2007.01478.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Esposito K, Marfella R, Ciotola M, et al. Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: A randomized trial. JAMA. 2004;292:1440–1446. doi: 10.1001/jama.292.12.1440. [DOI] [PubMed] [Google Scholar]
- 45.Salas-Salvado J, Garcia-Arellano A, Estruch R, et al. PREDIMED Investigators. Components of the Mediterranean-type food pattern and serum inflammatory markers among patients at high risk for cardiovascular disease. Eur J Clin Nutr. 2008;62:651–659. doi: 10.1038/sj.ejcn.1602762. [DOI] [PubMed] [Google Scholar]
- 46.Shahar D, Fraser D, Shai I, et al. Development of a food frequency questionnaire (FFQ) for an elderly population based on a population survey. J Nutr. 2003;133:3625–3629. doi: 10.1093/jn/133.11.3625. [DOI] [PubMed] [Google Scholar]
- 47.Lasheras C, Fernandez S, Patterson AM. Mediterranean diet and age with respect to overall survival in institutionalized, nonsmoking elderly people. Am J Clin Nutr. 2000;71:987–992. doi: 10.1093/ajcn/71.4.987. [DOI] [PubMed] [Google Scholar]