Introduction
Overweight and obesity have emerged as a major public health concern in the US over the past 20 years, as their prevalence increased substantially in all age groups. More than 70 percent of people 70 years and older are overweight with more than 30 percent obese (Ogden et al., 2006). In older ages, obesity has been associated with increased mortality (e.g., Thorpe & Ferraro, 2004), cognitive impairment and dementia (e.g., Profenno, Porsteinsson, & Faraone, 2010), cardiovascular morbidity (e.g., Harris et al., 1997) and functional impairment (e.g., Ferraro, Su, Gretebeck, Black, & Badylak, 2002; Peeters, Bonneux, Nusselder, De Laet, & Barendregt, 2004).
Empirical observations on how body-weight changes over time are mixed (Hedley et al., 2004; Ogden, Carroll, McDowell, & Flegal, 2007). Some cross-sectional studies suggest that body-weight increases up to about age 65 years and declines afterwards (Flegal, Carroll, Kuczmarski, & Johnson, 1998; McDowell, Fryar, Ogden, & Flegal, 2008; Seidell & Visscher, 2000). However, weight loss in old age may be an artifact of selective survival of leaner healthier individuals (Barone et al, 2006; Losonczy et al., 1995; Thorpe & Ferraro, 2004). Longitudinal studies of change in body-weight in older ages are few and limited to relatively short periods of follow-up, ranging from three to six years (Kahng, Dunkle, & Jackson, 2004; Newman et al., 2001; Woo, Ho, & Sham, 2001). The results of such studies are rather inconsistent: while some report that body-weight declines after age 65 (e.g., Kahng, Dunkle, & Jackson, 2004), others find either no reduction (e.g., Villareal, Apovian, Kushner, & Klein, 2005) or increases in body-weight into older ages (e.g., Barone et al., 2006; He & Baker, 2004).
Charting and describing the trajectory (i.e., estimating the intercept and rate-of-change) of body-weight over time cannot be accomplished through cross-sectional studies or studies of change between two points in time. Cross-sectional studies confound intrapersonal and interpersonal differences, while studies of transitions between two points in time are inadequate in assessing the underlying growth curve or trajectory (Rogosa, 1988). Currently, there is little research on the level and rate-of-change in BMI from middle to older age.
Furthermore, there is limited knowledge concerning how the level and rate-of-change in body-weight in middle and old age vary with key dimensions of social stratification, such as race/ethnicity, gender, and socioeconomic status (SES). Himes (2004), in a special issue of Research in Aging dedicated to obesity in older ages, argues that despite the strong relationship between ethnicity and body-weight, race/ethnicity is seldom the main focus of investigation in obesity studies. Given the association of obesity with poor aging outcomes (e.g., Field et al, 2001) and the well-defined pattern of social inequalities in aging and health (Alwin & Wray, 2005; Kim & Durden, 2007), advancing our understanding of how social stratification dimensions affect the trajectory of body-weight in middle and later life should be viewed as a critical goal.
This study has two specific aims. First, we offer quantitative estimates depicting the trajectory of body-mass index (BMI) by analyzing 14 years (1992 – 2006) of longitudinal data from a national sample of Americans born between 1931 and 1941. Second, we examine how the level and rate-of-change in BMI vary with ascribed (race/ethnicity, gender, age-at-baseline) and achieved (education) social status.
Conceptual Framework
The prevalence of obesity varies significantly with gender, race/ethnicity, and socio-economic status (e.g., Baltrus, Lynch, Everson-Rose, Raghunathan, & Kaplan, 2005; Clarke, O’Malley, Johnston, & Schulenberg, 2009). This is consistent with the perspective of social stratification of aging and health (House, Lantz, & Herd, 2005; Seeman & Crimmins, 2001), which proposes that race (Williams & Jackson, 2005), age (Riley, 1987), and gender (Bird & Rieker, 1999) influence socio-economic status (SES) attainment (i.e., income, education, occupation) (Adler & Ostrove, 1999), marital status (Wyke & Ford, 1992), and exposure to health risks and protective factors (Link & Phelan, 1995), consequently leading to inequalities in health outcomes in later life (e.g., Adler, Marmot, McEwen, & Stewart, 1999; Lantz et al., 2001). This conceptual framework will guide our examination of relationships between social stratification dimensions and trajectories of BMI starting in middle age.
Hypotheses
To the best of our knowledge, there is currently no quantitative depiction of long-term body-weight trajectory after age 50.. Existing studies suggest that body-weight increases throughout adult life up to 60–65 years of age, where it levels off or declines (e.g., Ogden et al., 2007; Williamson, 1993). However, most of these results come from cross-sectional or longitudinal studies of short duration. We hypothesize that after age 50, body-mass index (BMI) increases over time following a curvilinear decelerating trajectory (Hypothesis 1).
Racial/ethnic minorities, especially women, are disproportionately represented among the overweight and obese (Center for Disease Control [CDC], 2009; Ogden et al., 2007; Wang & Beydoun, 2007). While some investigators have reported that minority groups also experience higher weight gain over time (Chor, Faerstein, Kaplan, Lynch, & Lopes, 2004; Clarke et al., 2009; Truong & Sturm, 2005), this has not been replicated by others (Lewis et al., 2005). In addition, racial/ethnic differences in weight gain are confounded with other socio-economic characteristics (Baltrus et al., 2005; Kahn & Williamson, 1991). Because of these inconsistencies and because many studies do not include Hispanics as a separate group in the analysis (e.g., Kahng et al., 2004; Lewis et al., 2005; Mujahid, Diez-Roux, Borrell, & Nieto, 2005), racial/ethnic similarities or differences in body-weight trajectories are not well understood. We hypothesize that, relative to non-Hispanic Whites, Non-Hispanic Blacks and Hispanics exhibit a higher level of BMI and a higher rate of increase over time (Hypothesis 2).
Findings on gender differences in the prevalence of overweight/obesity are mixed. Some studies find no differences (e.g., Ogden et al., 2007; Sobal & Rauschenbach, 2003), while others point to a higher prevalence of overweight in men (Clarke et al., 2009; He & Baker, 2004; Novak, Ahlgren, & Hammarström, 2005; Wang & Beydoun, 2007), and a higher prevalence of obesity in women (e.g., Jenkins, Fultz, Fonda, & Wray, 2003; Williamson, 1993). Over time, women show greater variability in body weight (Williamson, 1993) and tend to gain more weight compared to men (He & Baker, 2004; Truong & Sturm, 2005). Consequently, we hypothesize that, relative to men, women will have a lower BMI level, but a higher rate of increase over time (Hypothesis3).
The educational advantage in overweight/obesity is well documented in younger adults (review in Ball & Crawford, 2005). Both the risk of overweight/obesity (Molarius, Seidell, Sans, Tuomilehto, & Kuulasmaa, 2000; Mujahid et al., 2005; Novak et al., 2005) and the rate of weight gain over time (Baltrus, Everson-Rose, Lynch, Raghunathan, & Kaplan, 2007; Mujahid et al., 2005) are inversely associated with educational achievement. Further research is required to clarify the role of education in shaping the trajectory of body-weight in older adults. We hypothesize that, relative to individuals with less education, those with more education will have both a lower level of BMI and a lower rate of increase over time (Hypothesis 4).
Age differences in the trajectories of health may reflect cohort and aging effects. The prevalence of overweight/obesity has increased in recent cohorts (Reynolds & Himes, 2007). Further, in younger adults, a more rapid pace of weight gain has been identified (Clarke et al. 2009; Grinker, Tucker, Vokonas, & Rush, 1995; Jacobsen et al., 2001). Extrapolating from these findings, we hypothesize that relative to younger individuals, older individuals will have both a lower level of BMI and lower rates of increase over time (Hypothesis 5).
Consistent with the social stratification of health and aging framework, and because of their previously documented relationship with overweight/obesity, we control in our analyses for other socio-economic characteristics, such as income/assets (Chang & Lauderdale, 2005; Fonda, Fultz, Jenkins, Wheeler, & Wray, 2004) and marital status (Sobal & Rauchenbach, 2003), and for health status (Mehta & Chang, 2009).
Methods
Design and Data
Data came from the Health and Retirement Study (HRS). The study started in 1992 by surveying a nationally representative sample of over 12,800 respondents from the 1931–1941 birth cohort, and subsequently added participants from older and younger birth cohorts (HRS documentation at: http://hrsonline.isr.umich.edu/). Because our study’s goal is to depict the BMI trajectory starting in middle age, and to minimize the potential for cohort effects (Reynolds & Himes, 2007), we chose to focus on one cohort, namely respondents who were born between 1931 and 1941 (the original HRS birth cohort). A total of 13,565 individuals are in the HRS sample: 12,899 in the original sample (95.1%) and the remaining 666 added as new spouses and partners since the beginning of the study in 1992. Baseline data were obtained in 1992, and follow-up data were gathered every 2 years from 1994 to 2006 (for a total of up to 8 repeated observations over a 14-year follow-up period).
The response rates range from 81.7% (1992) to 89.1% (in 1994). As of 2006, cumulative mortality rate (validated through linkages to the National Death Index) was 19%. When a respondent was unable to be interviewed due to physical or cognitive limitations, a proxy interview was conducted. The rates of proxy interviews vary by wave and range from 4.8% (1992) to 9.0% (2002).
From the initial sample of 13,565 individuals, 3,116 were excluded for being age-ineligible spouses (i.e., born before 1931 or after 1941). Further, 135 individuals were excluded because they never responded to the survey health sections relevant to our analysis. This resulted in a final analytic sample of 10,314 individuals with a total of 82,512 observations (mean number of interviews completed = 6.4). More than half (55.7%) of the respondents in the final sample completed all 8 interviews.
Measures
The dependent variable Body Mass Index (BMI) was calculated using the following formula:
BMI = [Weight (lb)/Height (inches)2] × 703.
Self-reported weight was recorded at each wave; height was recorded for the first interview and verified in the second one. For BMI calculation at each wave we used current weight and initial height.
Several measures of social stratification were included. Indicator variables were created for gender (1=Female, 0=Male) and race/ethnicity (i.e., non-Hispanic White, non-Hispanic Black, and Hispanic). Race/ethnicity was ascertained through a series of questions designed to ensure mutually-exclusive racial/ethnic categories. The Hispanic sample consisted of Mexican-Americans (60.5%), Cubans (9.8%), Puerto Ricans (8.4%), Dominicans (2.2%) and “other” Hispanic origin (18.9%). Henceforth, non-Hispanic Whites will be referred to as “Whites”, non-Hispanic Blacks as “Blacks”, while the “Hispanic” category includes only those who at the outset defined themselves as “Hispanics or Latino”. Education was measured by the number of years of schooling completed (lowest =0, highest =17 years). Age-at-baseline was measured as the difference between the baseline (i.e., 1992) and the year of birth (range = 51–61; mean = 55.8, SD=3.17).
Income and assets were measured at each wave respectively by total household income (from respondent and spouse only) and total household assets. Because the distributions of both income and assets were highly skewed, the variables were categorized (quartiles) for all analyses. Marital status was measured by binary variable coded as 1= married or living with a partner, 0 = single, divorced, widowed, or separated.
Because health status may operate either as a confounder (Mehta & Chang, 2009) or as a mediator between socio-economic and demographic characteristics and other health outcomes of interest (Seeman et al., 2004), in this case BMI, physical and mental health measures were added as time-varying covariates. Index of Chronic Diseases was measured as a count of seven prevalent chronic conditions – heart disease, stroke, high-blood pressure, diabetes, arthritis, chronic lung disease, and cancer. Each disease was coded as 0 (no) and 1 (yes), and a count of 1 (yes) was created (range = 0–7). Self-rated health was assessed as a single-item rating of respondent’s health (1 = excellent; 2 = very good; 3 = good; 4 = fair; 5 = poor). Functional status was represented by the NAGI index (Nagi, 1979), calculated as a count of six items, assessing difficulties with the following activities: (1) stooping, crouching or kneeling; (2) lifting or carrying weights >10 pounds (>4.5 kg); (3) extending the arms above shoulders; (4) standing up after sitting; (5) pulling or pushing a large object; and (6) writing or handling small objects. Each item was scored as 0 (no difficulty reported) or 1 (at least some difficulty reported). NAGI index ranges from 0 (no difficulty) to 6 (difficulties reported in all activities). Depressive symptoms were assessed by a count of nine items from the CES-D Scale (Center for Epidemiological Studies Depression Scale) (Radloff, 1977). All nine items were concordant across waves and include: (1) felt depressed, (2) everything was an effort, (3) restless sleep, (4) felt happy, (5) felt lonely, (6) enjoy life, (7) felt sad, (8) couldn’t get going, (9) had a lot of energy. For consistency, all items were re-coded to indicate negative feelings, with a value of 0 = no or 1 = yes. CES-D count ranges from 0 (no depressive symptoms) to 9 (maximum depressive symptoms). Finally, proxy status was measured at each wave by a binary variable coded 0 (self-respondent) or 1 (proxy respondent).
Weighted sample descriptive statistics (Gelman, 2007) for all time-varying covariates (Table 1) and time-constant covariates (Table 2) are presented below.
Table 1.
| Baseline (1992) |
Wave2 (1994) |
Wave3 (1996) |
Wave4 (1998) |
Wave5 (2000) |
Wave6 (2002) |
Wave7 (2004) |
Wave8 (2006) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Socio-Demographic | ||||||||||||||||
| Marital Status | 0.77 | 0.42 | 0.76 | 0.43 | 0.73 | 0.44 | 0.71 | 0.46 | 0.69 | 0.46 | 0.68 | 0.47 | 0.67 | 0.47 | 0.66 | 0.47 |
| Proxy Status | 0.05 | 0.21 | 0.06 | 0.23 | 0.06 | 0.23 | 0.07 | 0.26 | 0.08 | 0.27 | 0.08 | 0.27 | 0.07 | 0.25 | 0.05 | 0.21 |
| Assets (category) | 2.47 | 1.19 | 2.51 | 1.19 | 2.50 | 1.20 | 2.54 | 1.21 | 2.57 | 1.21 | 2.57 | 1.21 | 2.61 | 1.18 | 2.64 | 1.19 |
| Income (category) | 2.57 | 1.10 | 2.62 | 1.10 | 2.59 | 1.10 | 2.61 | 1.11 | 2.62 | 1.11 | 2.63 | 1.10 | 2.63 | 1.11 | 2.65 | 1.10 |
| Health | ||||||||||||||||
| Self-Rated Health (1–5) | 2.55 | 1.18 | 2.72 | 1.20 | 2.69 | 1.19 | 2.83 | 1.16 | 2.80 | 1.16 | 2.81 | 1.15 | 2.86 | 1.14 | 2.87 | 1.13 |
| Index of Chronic Diseases (0–7) | 1.16 | 1.11 | 2.44 | 1.47 | 2.74 | 1.62 | 3.02 | 1.76 | 3.30 | 1.88 | 3.58 | 1.93 | 3.80 | 1.95 | 4.01 | 1.94 |
| CES-D count (0–9) | 3.77 | 1.56 | 3.21 | 1.61 | 3.51 | 1.28 | 3.64 | 1.33 | 3.61 | 1.35 | 3.61 | 1.33 | 3.54 | 1.31 | 3.52 | 1.34 |
| NAGI count (0–6) | 1.44 | 1.66 | 1.18 | 1.56 | 1.27 | 1.61 | 1.32 | 1.61 | 1.34 | 1.61 | 1.45 | 1.62 | 1.51 | 1.61 | 1.58 | 1.64 |
| Body-Mass Index | 26.98 | 4.96 | 27.10 | 4.94 | 27.23 | 5.05 | 27.36 | 5.12 | 27.53 | 5.23 | 27.66 | 5.30 | 27.73 | 5.39 | 28.07 | 5.48 |
Time-varying covariates (Level 1) are those associated with repeated observations within individuals.
Case weights for each wave are respondent-level weights (2006 HRS Cross-Tracker file).
Table 2.
| Covariates | Mean/% | SD |
|---|---|---|
| Age (1992) | 55.83 | 3.17 |
| Female | 52.3% | |
| Educationc | 12.34 | 3.05 |
| Non-Hispanic Black | 10.3% | |
| Hispanic | 6.5% | |
| Mortality (between baseline and 2006) | 18.7% | |
| Attrition (between baseline and 2006) | 7.1% |
Time-constant covariates (Level 2) are those associated with the individual at baseline (1992).
Case weights are respondent-level 1992 weights (2006 HRS Cross-Tracker File).
Education is measured as "number of school-years completed".
Data Analysis
Hierarchical linear models (Raudenbush & Bryk, 2002) were used to estimate the trajectory of BMI over a period of observation of 14 years (1992–2006).
We modeled the intra-personal changes in BMI with the following equation:
| (1) |
where YiT is the BMI of an individual i at time T. π0i is the intercept of BMI for an individual I, and π1i is the slope (intra-personal rate of change) in BMI for individual i over time. Time is the distance (in years) of assessment from the baseline. XkiT represents the time-varying covariates (e.g., marital status, income, assets) associated with individual i at time T, and πki represents the effect of Xk on individual i’s BMI. εiT is the random error in BMI for individual i at time T.
We employed a time-based analytic approach (Alwin, Hofer, & McCammon, 2006) and controlled for inter-personal age-at-baseline differences. We considered both linear and non-linear (quadratic and cubic) patterns of change in BMI. Time was centered at its mean to minimize the possibility of multicollinearity when evaluating quadratic and cubic time (T) functions. Consequently, the intercept for any given model should be interpreted as the BMI at the mean follow-up time (i.e., 7 years into the study).
Time-constant predictors, such as race/ethnicity, education, gender, and age-at-baseline, are included in the Level 2 equation (person-level or inter-personal variations model):
| (2) |
Here, Xqi is the qth time constant covariate associated with individual i, and βpq represents the effect of variable Xq on the pth growth parameter (πp). rpi is a random effect and has a mean of 0.
The HRS involved the over-sampling of Blacks, Hispanics and respondents from Florida. For the multivariate analyses, we decided against the inclusion of sample weights, because many of the attributes on which differential selection weights are calculated (e.g., race/ethnicity, gender, marital status) are explicitly controlled in the models. As such, unweighted ordinary least squares estimates are less biased than and preferable over weighted estimates (Winship & Radbill, 1994). In addition, we ran all models both with and without weights (respondent-level case weights from the 2006 HRS Cross-Tracker file) and obtained very similar results. Finally, we set the statistical significance p-level at less than 0.01, to avoid the over-abundance of significant results due to the very large HRS sample.
Mortality, Attrition and Proxy Status
To minimize the loss of participants due to item missing (Little & Rubin, 2002), multiple imputation was performed (Schafer & Olsen, 1998). Using the NORM software (Schafer, 1997), we imputed 5 data sets and ran HLM analyses using each data set. Parameter estimates and their standard errors were calculated by averaging across the 5 data sets and adjusting for their variance (Raudenbush & Bryk, 2002).
We also addressed the potential for selection bias due to non-ignorable missing data as a result of mortality and attrition. Prior studies document the complicated relation between body-weight and mortality in older age (e.g., Thorpe & Ferraro, 2004). In studies of older populations, the probability of missing data due to mortality and attrition is systematically related to the health outcomes of interest (Harel, Hofer, Hoffman, & Pedersen, 2007) and consequently the critical “missing-at-random” assumption is violated (Little & Rubin, 2002). The potential for confounding effects of selective mortality and attrition needs to be methodologically addressed (Liang et al., 2010; Mroczek & Spiro, 2005). We included binary variables in the Level 2 equation (Mortality: 0 = alive at the end of the study and 1 = died during study; Attrition: 0 = completed the study period and 1 = dropped out for reasons other than mortality and did not return in subsequent waves) to differentiate respondents who completed the study period from those who died or dropped-out before the study ended. This approach is similar to the pattern-mixture models, in which subjects are classified into different groups, based on their missing data patterns, and estimates are obtained by averaging over the identified patterns (Hedeker & Gibbons, 2006, pp. 302–312). Finally, proxy status was measured as a time-varying covariate (0=self, 1=proxy respondent).
Results
Trajectory of BMI
Using linear, quadratic, and cubic functions, we mapped the trajectory of BMI between 1992 and 2006. The unconditional model showed that BMI follows a quadratic trajectory, with an intercept of 27.38 (p<.001), linear slope of 0.047 (p<.001) and a quadratic slope of 0.002 (p<.01) (Table 3 - M0), apparently lending support for Hypothesis 1. However, adjustment for mortality/attrition and additional socio-demographic and health status measures (Table 3 – M1, M2, M3, and M4) rendered the quadratic coefficient non-significant and revealed a largely linear trajectory (intercept b=27.361, p<.001; linear slope b=0.067, p<.001 in M4). As the cubic slope coefficient was not significant in the unconditional model (M0) it was not included in subsequent analyses.
Table 3.
Within-persons and Between-persons Differences in Body-Mass Index: Hierarchical Linear Modeling Results.
| Parameter | Variable | M0 | M1 | M2 | M3 | M4 | M5 |
|---|---|---|---|---|---|---|---|
| Fixed Effect | |||||||
| Time-varying variables | |||||||
| Proxy | −0.606*** | −0.612*** | −0.612*** | −0.658*** | −0.568*** | ||
| Marital Status | 0.256*** | 0.285*** | 0.210*** | ||||
| Assets | −0.008 | 0.010 | 0.013 | ||||
| Income | −0.095*** | −0.078*** | −0.059*** | ||||
| Self-Rated Health | −0.006 | −0.003 | |||||
| Index Disease | 0.002 | 0.001 | |||||
| NAGI Index | 0.241*** | 0.167*** | |||||
| CES-D Index | −0.013 | −0.019 | |||||
| Intercept | π0 | ||||||
| Intercept | 27.383*** | 27.613*** | 27.370*** | 27.290*** | 27.361*** | 27.517*** | |
| Mortality | −0.436*** | −0.531** | −0.610*** | −0.713*** | −0.690*** | ||
| Attrition | −0.686*** | −0.790*** | −0.754*** | −0.708** | −0.197 | ||
| Black | 1.585*** | 1.446*** | 1.417*** | 0.145 | |||
| Hispanic | 0.687*** | 0.221 | 0.247 | −0.144 | |||
| Female | −0.146 | −0.159 | −0.259** | −0.083 | |||
| Age (1992) | −0.063*** | −0.072*** | −0.074*** | −0.051*** | |||
| Education | −0.099*** | −0.085*** | −0.009 | ||||
| BMI (1992) | 0.696*** | ||||||
| Linear Slope | π1 | ||||||
| Intercept | 0.047*** | 0.066*** | 0.073*** | 0.075*** | 0.067*** | 0.063*** | |
| Mortality | −0.079*** | −0.068*** | −0.069*** | −0.056*** | −0.062*** | ||
| Attrition | −0.002 | 0.000 | 0.001 | 0.002 | −0.018 | ||
| Black | −0.053*** | −0.054*** | −0.056*** | −0.008 | |||
| Hispanic | −0.047*** | −0.046*** | −0.047*** | −0.032* | |||
| Female | 0.010 | 0.011 | 0.014 | 0.007 | |||
| Age (1992) | −0.006*** | −0.005*** | −0.005*** | −0.006*** | |||
| Education | 0.000 | −0.000 | −0.002** | ||||
| BMI (1992) | −0.025*** | ||||||
| Quadratic Slopea | π2 | ||||||
| Intercept | 0.002** | 0.001 | −0.001 | −0.001 | −0.001 | −0.001 | |
| Random Effect | VARIANCE | VARIANCE | VARIANCE | VARIANCE | VARIANCE | VARIANCE | |
| Intercept1 | 20.054*** | 19.916*** | 19.510*** | 19.372*** | 18.191*** | 6.835*** | |
| Linear | 0.074*** | 0.072*** | 0.072*** | 0.071*** | 0.070*** | 0.060*** | |
| Quadratic | 0.001*** | 0.001*** | 0.001*** | 0.001*** | 0.001*** | 0.002*** | |
| Level1 R | 7.579 | 7.558 | 7.558 | 7.553 | 7.525 | 7.114 | |
| AIC | 445,993.33 | 445,607.26 | 445,411.33 | 445,326.31 | 444,765.75 | 424,447.38 | |
p< .05,
p< .01,
p< .001.
Regression coefficients associated with all covariates on quadratic slope are non-significant in models 1 through 5.
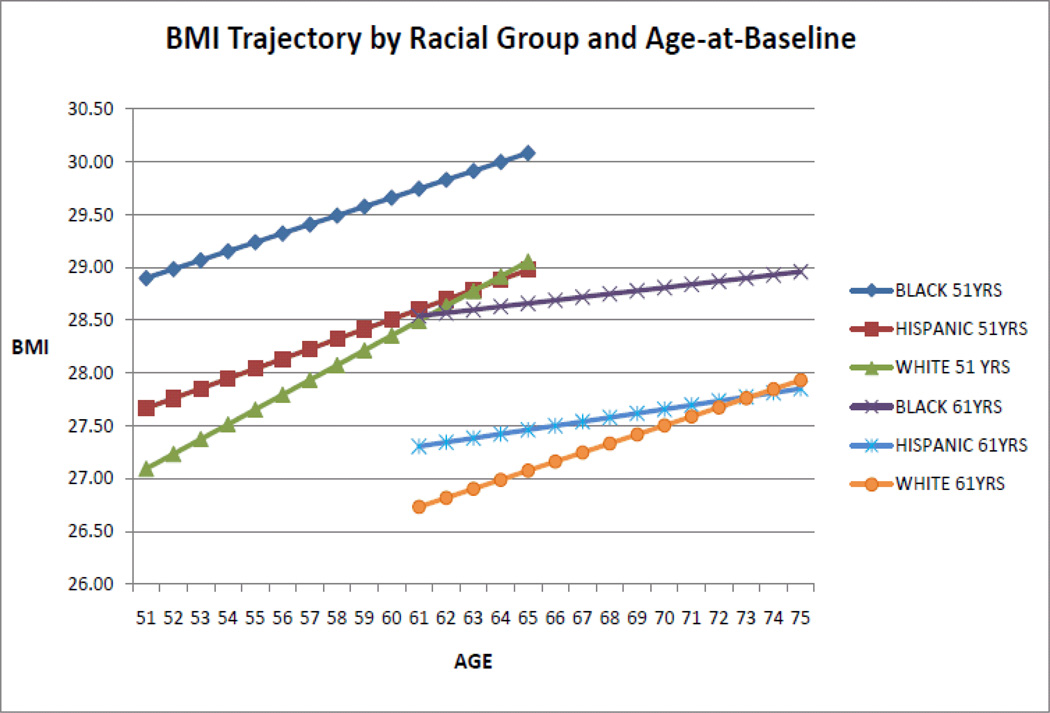
Racial/Ethnic Differences in BMI Trajectory
The results showed significant racial/ethnic differences in the intercept and linear slope (Hypothesis 2), but not in the quadratic slope (Table 3 - M2). As Figure 1 illustrates, compared with Whites, Blacks exhibited a higher BMI level (b=1.585, p<.001), but a lower rate-of-increase (b = −0.053, p<.001). Differences between Whites and Blacks remain robust after adjustment for socio-economic and health status factors. However, heterogeneity in SES and health status appears to account for the Hispanics – White differences in the level of BMI, but not in the rate-of-change (M3 and M4).
Figure 1.
BMI Trajectory by Racial/Ethnic Group and Age-at-Baselinea.
a Graph derived based on M4 (Table 3).
Gender Differences in BMI Trajectory
The hypothesized gender differences in BMI trajectory (Hypothesis 3) were not supported (M2). Men and women had similar BMI levels and linear rates-of-change, except in the model controlling for health status (M4), in which females showed a lower BMI level (b= −0.259, p<.01).
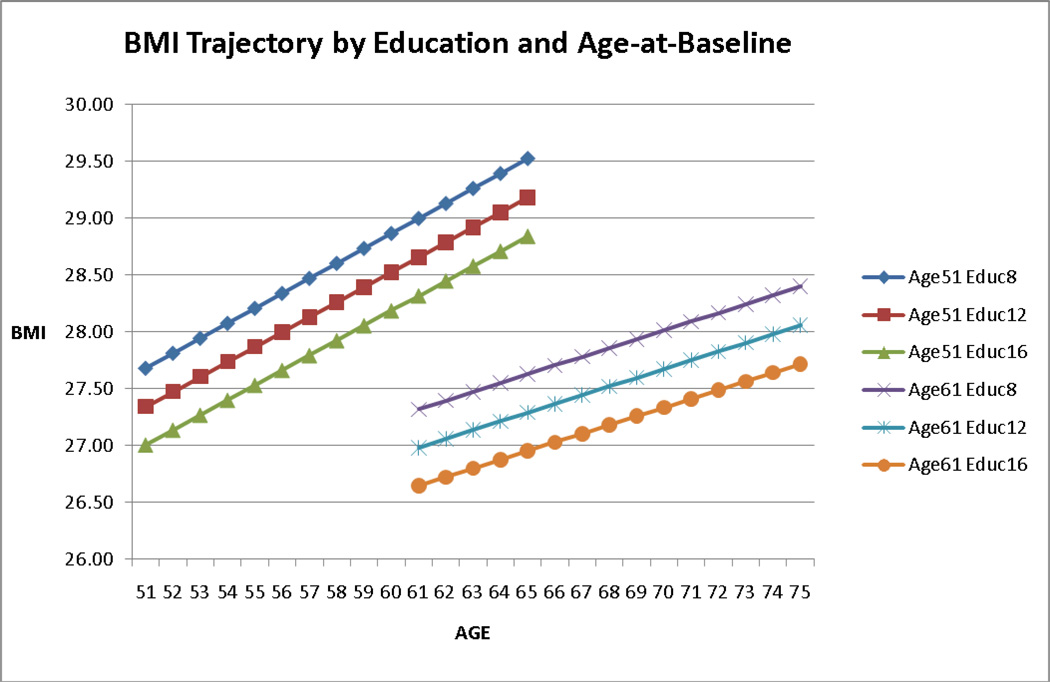
Educational Differences in BMI Trajectory
Hypothesis 4 was partially supported, as we found significant educational differences in BMI level, but not in the rate-of-change over time. Specifically, higher education was associated with a lower BMI intercept (b = −0.099, p<.001 in M3). The linear rate-of-change in BMI was similar at different levels of education, except when accounting for baseline BMI (b = −0.002, p<.01 in M5). These results remained robust when SES (M3) and health status (M4) were taken into account (Figure 2).
Figure 2.
BMI Trajectory by Years-of-Education Completed and Age-at-Baselinea.
a Graph derived based on M4 (Table 3).
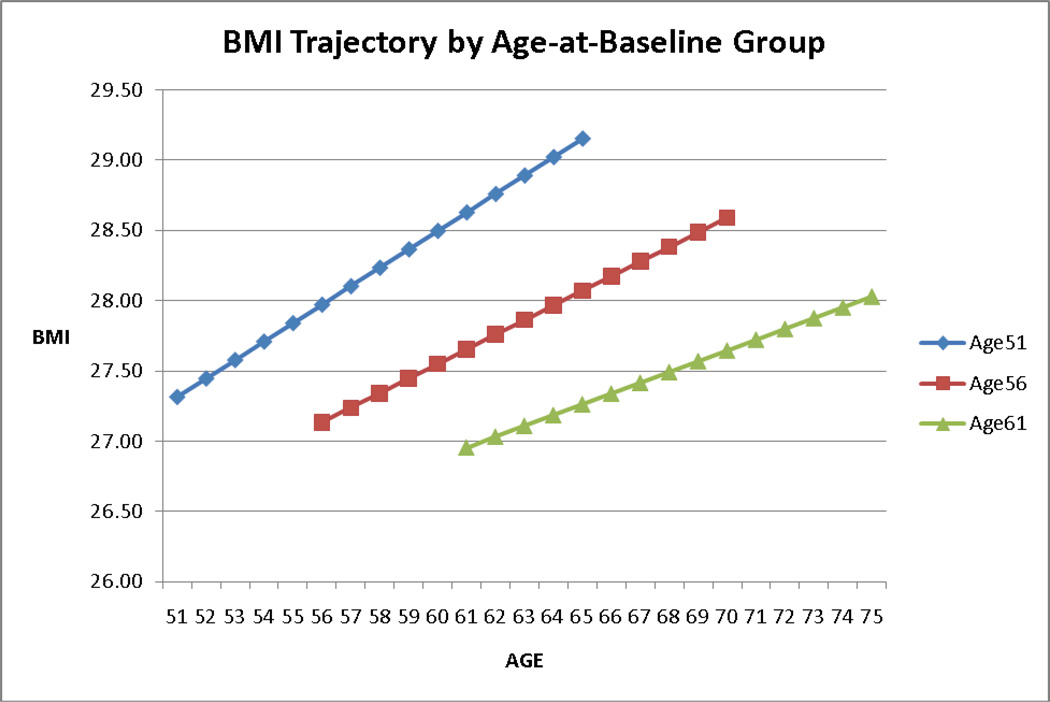
Age Differences in BMI Trajectory
Older age groups had lower levels of BMI (b = −0.063, p<.001 in M2) and smaller rates-of-change (b = −0.006, p<.001 in M2). Age differences persisted after adjustment for SES, health status and baseline BMI (M4 and M5). As depicted in Figure 3, participants who are older at baseline had a lower intercept and a lower linear rate of weight gain compared with their younger-at-baseline counterparts. Controlling for all covariates, a one-year increase in age-at-baseline is associated with a decrease of 0.051 in the level of BMI at the mean follow-up time (p<.001) and a lower linear rate of increase over time (b = −0.006, p<.001 in M5). These findings were consistent with the hypothesized age-at-baseline differences in BMI trajectory (Hypothesis 5).
Figure 3.
BMI Trajectory by Age-at-Baseline in 1992a.
a Graph derived based on M4 (Table 3).
Effects of Other Covariates
Socioeconomic factors, such as income/assets and marital status, as well as health status, may operate as confounding variables (Chang & Lauderdale, 2005; Mehta & Chang, 2009; Sobal & Rauchenbach, 2003) or as mediators (Baltrus et al., 2005; Seeman et al., 2004). In accordance with Baron and Kenny’s (1986) recommendation for mediation testing, models 4 and 5 (Table 3) account for these variables. While BMI levels were not significantly associated with assets, higher income predicted a lower BMI in all models (p<.001) (M3). Marital status was positively associated with BMI, such that in every model tested, married people had higher BMI (p<.001 for all models) than people who were single, widowed or divorced.
Finally, with the exception of NAGI index, health status measures (chronic diseases, self-rated health and CES-D) showed no association with BMI levels. In particular, those with more functional limitations exhibited higher BMI, even after adjusting for baseline age and BMI.
Mortality, Attrition and Proxy Interview
To control for potential selection bias, mortality, attrition and proxy status were included as confounding variables. Even though the analyses performed with these covariates amount to regression analyses, we recommend against interpreting mortality and attrition as classic “predictors”, because both are final events which do not precede any event to be eventually “predicted”. As such, they are viewed as confounding variables, although they may also serve as proxies for poor health (Harel, Hofer, Hoffman, & Pedersen, 2007).
Mortality was negatively associated with the trajectory of BMI in all models; those who died during the follow-up period had a lower BMI (b= −0.436, p<.001) and a lower rate of gain (b = −0.079, p <. 001 in M1) prior to death. Attrition was negatively associated with the level of BMI, such that people who dropped-out of the study had a lower mean BMI (b = −0.686, p <.001 in M1). The linear rate-of-change was not associated with attrition in any of the models tested. Proxy status predicted a lower level of BMI (b = −0.606, p<.001 in M1) in all models. These results suggest that selection bias is a threat in that parameter estimates for the trajectory of BMI would be biased should those measures not be included in the analysis.
Discussion and Conclusions
To the best of our knowledge, this is the first study which quantitatively depicts the long-term trajectory of BMI in a national sample of middle aged Americans. Whereas BMI increases in a largely linear fashion over time, this trajectory varies significantly across several dimensions of social stratification, including race/ethnicity, education, and age-at-baseline. However, we observe no gender differences in BMI trajectories.
There are significant racial/ethnic variations in the level and rate-of-change in BMI. Non-Hispanic Blacks enter middle age at a significantly higher BMI level, but they gain less weight over time compared with their White counterparts. After accounting for differences in SES and health status, Hispanics do not differ from Whites in BMI levels, but they tend to gain less weight over time. Our findings differ from those of studies of BMI changes in younger age groups, which show that Hispanics and Blacks exhibit similar trajectories, having higher BMI levels and more accelerated rates of BMI growth compared with Whites (Clarke et al., 2009). Differences in cohort composition (Roshania, Narayan, & Oza-Frank, 2008) and acculturation patterns (Abraido-Lanza, Chao, & Florez, 2005) may account for the discrepancy in findings. In younger cohorts (Clarke et al., 2009), the risk for overweight/obesity and the rate of change in BMI are similar among minority groups, perhaps due to similar life experiences and exposures (Palmore, 1978). In an older cohort, such as ours, a higher proportion of Hispanics may be foreign-born, first-generation immigrants (Card, 2005), exposed to different early-life environments (nutrition or physical activity patterns) and more likely to preserve cultural norms and values associated with “better” health behaviors (Abraido-Lanza, Chao, & Florez, 2005; Akresh, 2007). Another possible explanation is the underlying heterogeneity within the Hispanic population (Zsembik & Fennell, 2005). A majority (61%) of our sample consisted of Mexican-Americans. Because of the small number of respondents in other Hispanic groups (e.g., Cubans, Puerto Ricans, Dominicans) we were unable to analyze the trajectory of BMI in each of these sub-groups. The approach of combining various Hispanic sub-groups may obscure differences in socio-economic characteristics and in health behavior and further mute underlying differences in BMI trajectories. The same holds true for the underlying heterogeneity within the Non-Hispanic White and Non-Hispanic Black populations. The three commonly-recognized racial groups may fail to capture the considerable biological variability in human populations (Williams, 1999). Additional studies need to further define sub-group differences in BMI trajectories within the White, Black and Hispanic populations.
Contrary to findings from younger groups (e.g., Baltrus et al., 2005), our results show that in middle and old age socio-economic status does not substantially attenuate the relationship between race/ethnicity and BMI trajectory, with the exception of Hispanic/White differences in BMI intercept. This suggests that developmental patterns of body-weight are set much earlier in life (Barker, 2007). Disadvantaged prenatal and childhood environments have been associated with an increased risk of obesity in adulthood (e.g., Ferraro, Thorpe, & Wilkinson, 2003). Racial/ethnic differences in early-life determinants of obesity (Whitaker & Orzol, 2006) and the strong tracking of early-life obesity into adulthood and older ages (Eriksson, Forsen, Osmond, & Barker, 2003) may explain how childhood racial disparities in body-weight track into adulthood and older ages.
Our study reveals educational differences in the level of body-weight, but not in the rate-of-change. Further, the effect is diminished when baseline BMI is considered, illustrating again the importance of early life factors in setting the course for weight development into older ages (e.g., Baltrus et al., 2007). We also find that the effect of education is not attenuated when considering potentially intervening economic determinants, such as income or assets, or differences in health status. It has been argued that health status and behaviors partially explain socio-economic, including educational, disparities in health trajectories in old age (e.g., Dietz, 2007; Lynch, Kaplan, & Salonen, 1997). According to our findings, the effect of education persists even after adjusting for time-varying measures of health status. Health behaviors partially mediate the association between education (as a measure of SES) and other health outcomes (Lantz et al., 2001) and may mediate the observed educational differences in BMI trajectory. Future examination of health behaviors (smoking, alcohol consumption, physical activity) as potential mediators between education and BMI trajectory is warranted, and may explain the observed decline in the “advantage” of education in younger cohorts (Himes & Reynolds, 2005).
Older age-at-baseline is associated not only with a lower level of BMI, but also with a slower rate of increase over time. Shorter-term longitudinal studies of older respondents (e.g., Dziura, Mendes de Leon, Kasl, & DiPietro, 2004; Kahng et al, 2004) found a decline in body weight after age 65, but our results are consistent with at least one study (Barone et al., 2006), which suggested that cohort and selective survival explain the apparent decline in body weight in older ages. Because of previously documented cohort effects (Reynolds & Himes, 2007) and the potential inadequacy of BMI as a measure of body composition in old ages, we chose to limit our focus to a single cohort of 51 to 61 years old. Our respondents were followed up to age 75 (the age of the oldest respondents at the end of the follow-up period), revealing that, barring cohort and healthy survivor effects, BMI increases between the ages of 51 and 75.
We should emphasize that in our analysis we used time-based models (i.e., intrapersonal changes over the period of observation), and that interpersonal age differences were controlled in the prediction of both intercept and slope by the introduction of age-at-baseline as a time-constant covariate (Alwin, Hofer, & McCammon, 2006). We did not pursue an age-based analysis because HRS data are unsuitable for the correct estimation of the intrapersonal age effects on BMI (discussion in Liang et al, 2008). Briefly, because HRS yields only data collected from respondents from different cohorts at different ages, age and cohort effects are highly confounded, such that the observed age effects represent a combination of cohort- and “true” age effects. Therefore, we cannot infer on the effects of age on intrapersonal BMI development, but only on the effect of time in this specific age group.
Contrary to some prior observations, we find no gender differences in the trajectories of BMI. However, most previous findings come from younger groups (e.g., Baltrus et al., 2005; Clarke et al., 2009). Gender-related socio-economic profiles change across cohorts, and the effects of education (Clarke et al., 2009, Novak et al., 2006), race/ethnicity (Baltrus et al., 2005; Chor et al., 2004) and other measures of SES (Ball & Crawford, 2005; Mujahid et al., 2005) on BMI, vary by gender. In addition, prior studies often do not explicitly account for selective survival (e.g., He & Baker, 2004). Given the significant effect of mortality and attrition observed in our and other (e.g., Barone et al., 2006) studies, and the well-documented gender differences in mortality rates in older ages (with men dying younger), selective survival may explain previously observed gender differences in patterns of change in body-weight.
Several limitations of this research should be noted. Self-reported weight and height were used for BMI calculations across all waves. Individuals tend to over-report their height and under-estimate their weight (Gunnell et al., 2000; Nawaz, Chan, Abdulrahman, Larson, & Katz, 2001), therefore BMI calculations based on self-reported weight and height are likely to understate the “true” BMI. Three considerations mitigate the potential for bias related to self-reporting. First, if the under-reporting of weight and the over-reporting of height are consistent over time, and there is no indication in the literature to the contrary, the analysis should yield valid estimates of changes in BMI over time. Second, we undertook a comparison of self-reported and interviewer-measured weight and height (available for two distinct random sub-samples of respondents in 2004 and 2006) and found the differences to be rather small in absolute values (not shown; results available upon request). This is also consistent with another analysis of the quality of self-reports of weight and height in HRS (Weir, 2008). Third, within the very limited literature on socio-demographic correlates of bias in self-reporting of weight and height, a review of accuracy of self-reporting in women found no differences among various racial groups (Engstrom, Paterson, Doherty, Trabulsi, & Speer, 2003). Nonetheless, we cannot entirely rule out yet unidentified socio-demographic differences in self-reporting of weight and height; future studies employing measured rather than self-reported weight and height are needed to validate our results.
Conventional anthropometric measures, such as BMI, may be inadequate measures of overall and abdominal fatness in elderly subjects (Prentice & Jebb, 2001; Seidell & Visscher, 2000). Further, interpretations of BMI trajectories in older age should take into account to effect of age-related loss of height. Prior longitudinal studies show that height loss accelerates during the eighth decade of life, peaks after age 80 (Dey, Rothenberg, Sundh, Bosaeus, Steen, 1999; Sorkin, Muller and Andres, 1999) and may account for small artifactual increases in BMI between age 70 and 80 (Sorkin et al., 1999). As some of the respondents in our sample were followed up to age 75, the possibility of upward bias in BMI in later waves in some participants should be considered. We were unable to augment our results with a similar analysis of other body-composition indicators and to assess the potential for artifactual BMI changes due to loss of height because HRS does not collect data on these indicators or on self-reported height in later waves.
Finally, additional studies need to consider a more refined differentiation of racial/ethnic groups, by considering the underlying heterogeneity within the three traditionally studied groups. Race/ethnicity embody life experiences and socio-economic characteristics (Williams, 1999); identifying meaningful ethnic sub-groups representing diverse socio-economic and life course patterns may elucidate some of the complexity in BMI development in adult and older ages. Further, since obesity is linked to an increased risk of early mortality and chronic morbidities, the associations identified here between race/ethnicity, SES and weight trajectories are prone to reinforce and even exacerbate the existing health inequalities in older ages. Our findings highlight the need for long-term longitudinal studies starting in young and middle adulthood, assessing multiple potential mediators and investigating the cumulative effects of racial and socio-economic components (education, income, occupation) on BMI development into old ages.
This research contributes to our understanding of the social stratification of health and aging dynamics by focusing on intra-personal and inter-personal differences in BMI trajectory in a national sample of middle-age Americans over a 14-year period. Our findings complement existing studies of younger and older age groups, to elucidate the dynamics of body-weight development in mid-adult life.
Acknowledgments
FUNDING
This work was supported by grants T32-AG027708 (to A.B.) and R01-AG154124 and R01-AG028116 (to J.L) from the National Institute on Aging at the National Institutes of Health. The Japanese Ministry of Health, Labor and welfare Longevity Foundation, the Tokyo Metropolitan Institute of Gerontology, and the Michigan Claude D. Pepper Older Americans Independence Center (P60-AG08808) provided additional support (to J.L.). The authors wish to thank the funding agencies for their generous support.
Footnotes
Conflict of Interest: The authors have no financial or other kinds of personal conflicts of interest to declare.
Authors’ Contribution: All authors meet the criteria for authorship stated in the ‘Uniform Requirements for Manuscripts Submitted to Biomedical Journals’. Anda Botoseneanu planned the study, performed data management and statistical analysis, interpreted the results, and drafted and revised the manuscript. Jersey Liang helped in planning the study, supervised the data analysis and interpretation of results, and contributed to writing and revising the manuscript. Both authors gave their final approval for the version submitted for publication.
References
- Abraido-Lanza AF, Chao MT, Florez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Social Science & Medicine. 2005;61(6):1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler NE, Marmot M, McEwen BS, Stewart J, editors. Socioeconomic status and health in industrialized nations: Social, psychological, and biological pathways. 1. Vol. 896. New York, NY: The Annals of the New York Academy of Sciences; 1999. [PubMed] [Google Scholar]
- Adler NE, Ostrove JM. Socioeconomic status and health: What we know and what we don't. In: Adler NE, Marmot M, McEwen BS, Stewart J, editors. Socioeconomic status and health in industrialized nations: Social, psychological, and biological pathways. 1. Vol. 896. New York, NY: The Annals of the New York Academy of Sciences; 1999. pp. 3–15. [DOI] [PubMed] [Google Scholar]
- Akresh IR. Dietary assimilation and health among Hispanic immigrants to the United States. Journal of Health and Social Behavior. 2007;48(4):404–417. doi: 10.1177/002214650704800405. [DOI] [PubMed] [Google Scholar]
- Alwin DF, Wray LA. A life-span developmental perspective on social status and health. Journal of Gerontology: Social Sciences. 2005;60(2):7–14. doi: 10.1093/geronb/60.special_issue_2.s7. [DOI] [PubMed] [Google Scholar]
- Alwin DF, Hofer SM, McCammon RJ. Modeling the effects of time: Integrating demographic and developmental perspectives. In: Binstock RH, George LK, editors. Handbook of aging and the social sciences. 6th ed. San Diego, CA: Elsevier; 2006. pp. 20–38. [Google Scholar]
- Ball K, Crawford D. Socioeconomic status and weight change in adults: a review. Social Science & Medicine. 2005;60(9):1987–2010. doi: 10.1016/j.socscimed.2004.08.056. [DOI] [PubMed] [Google Scholar]
- Baltrus PT, Everson-Rose SA, Lynch JW, Raghunathan TE, Kaplan GA. Socioeconomic position in childhood and adulthood and weight gain over 34 years: The Alameda County Study. Annals of Epidemiology. 2007;17(8):608–614. doi: 10.1016/j.annepidem.2007.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baltrus PT, Lynch JW, Everson-Rose S, Raghunathan TE, Kaplan GA. Race/ethnicity, life-course socioeconomic position, and body weight trajectories over 34 years: The Alameda County Study. American Journal of Public Health. 2005;95(9):1595–1601. doi: 10.2105/AJPH.2004.046292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker DJ. Obesity and early life. Obesity Reviews. 2007;8(Supplement 1):45–49. doi: 10.1111/j.1467-789X.2007.00317.x. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barone BB, Clark JM, Wang NY, Meoni LA, Klag MJ, Brancati FL. Lifetime weight patterns in male physicians: The effects of cohort and selective survival. Obesity. 2006;14(5):902–908. doi: 10.1038/oby.2006.104. [DOI] [PubMed] [Google Scholar]
- Bird CE, Rieker PP. Gender matters: An integrated model for understanding men's and women's health. Social Science & Medicine. 1999;48(6):745–755. doi: 10.1016/s0277-9536(98)00402-x. [DOI] [PubMed] [Google Scholar]
- Card D. Is the new immigration really so bad? Economic Journal. 2005;115(507):F300–F323. [Google Scholar]
- Center for Disease Control and Prevention [CDC] Differences in prevalence of obesity among Black, White, and Hispanic adults — United States, 2006–2008. Morbidity and Mortality Weekly Report. 2009;58(27):740–744. [PubMed] [Google Scholar]
- Chang VW, Lauderdale DS. Income disparities in body mass index and obesity in the United States, 1971–2002. Archives of Internal Medicine. 2005;165(18):2122–2128. doi: 10.1001/archinte.165.18.2122. [DOI] [PubMed] [Google Scholar]
- Chor D, Faerstein E, Kaplan GA, Lynch JW, Lopes CS. Association of weight change with ethnicity and life course socioeconomic position among Brazilian civil servants. International Journal of Epidemiology. 2004;33(1):100–106. doi: 10.1093/ije/dyg277. [DOI] [PubMed] [Google Scholar]
- Clarke P, O'Malley PM, Johnston LD, Schulenberg JE. Social disparities in BMI trajectories across adulthood by gender, race/ethnicity and lifetime socio-economic position: 1986–2004. International Journal of Epidemiology. 2009;38(2):499–509. doi: 10.1093/ije/dyn214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dey D, Rothenberg E, Sundh V, Bosaeus I, Steen B. Height and body weight in the elderly. A 25-year longitudinal study of a population aged 70 to 95 years. European Journal of Clinical Nutrition. 1999;53(12):905–914. doi: 10.1038/sj.ejcn.1600852. [DOI] [PubMed] [Google Scholar]
- Dietz WH. The role of lifestyle in health: The epidemiology and consequences of inactivity. Proceedings of the Nutrition Society. 2007;55(03):829–840. doi: 10.1079/pns19960082. [DOI] [PubMed] [Google Scholar]
- Dziura J, Mendes de Leon C, Kasl S, DiPietro L. Can physical activity attenuate aging-related weight loss in older people? The Yale Health and Aging Study, 1982–1994. American Journal of Epidemiology. 2004;159(8):759–767. doi: 10.1093/aje/kwh105. [DOI] [PubMed] [Google Scholar]
- Engstrom JL, Paterson SA, Doherty A, Trabulsi M, Speer KL. Accuracy of self-reported height and weight in women: An integrative review of the literature. Journal of Midwifery & Women's Health. 2003;48(5):338–345. doi: 10.1016/s1526-9523(03)00281-2. [DOI] [PubMed] [Google Scholar]
- Eriksson J, Forsen T, Osmond C, Barker D. Obesity from cradle to grave. International Journal of Obesity. 2003;27(6):722–727. doi: 10.1038/sj.ijo.0802278. [DOI] [PubMed] [Google Scholar]
- Ferraro KF, Su Y, Gretebeck RJ, Black DR, Badylak SF. Body mass index and disability in adulthood: A 20-year panel study. American Journal of Public Health. 2002;92(5):834–840. doi: 10.2105/ajph.92.5.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro KF, Thorpe RJ, Wilkinson JA. The life course of severe obesity: Does childhood overweight matter? Journal of Gerontology: Social Sciences. 2003;58(2):S110–S119. doi: 10.1093/geronb/58.2.s110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Archives of Internal Medicine. 2001;161(13):1581–1586. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: Prevalence and trends, 1960–1994. International Journal of Obesity. 1998;22(1):39–47. doi: 10.1038/sj.ijo.0800541. [DOI] [PubMed] [Google Scholar]
- Fonda SJ, Fultz NH, Jenkins KR, Wheeler LM, Wray LA. Relationship of body mass and net worth for retirement-aged men and women. Research on Aging. 2004;26(1):153–176. [Google Scholar]
- Gelman A. Struggles with survey weighting and regression modeling. Statistical Science. 2007;22(2):153–164. [Google Scholar]
- Grinker JA, Tucker K, Vokonas PS, Rush D. Body habitus changes among adult males from the normative aging study: Relations to aging, smoking history and alcohol intake. Obesity Research. 1995;3(5):435–446. doi: 10.1002/j.1550-8528.1995.tb00173.x. [DOI] [PubMed] [Google Scholar]
- Gunnell D, Berney L, Holland P, Maynard M, Blane D, Frankel S, et al. How accurately are height, weight and leg length reported by the elderly, and how closely are they related to measurements recorded in childhood? International Journal of Epidemiology. 2000;29(3):456–464. [PubMed] [Google Scholar]
- Harel O, Hofer SM, Hoffman L, Pedersen NL. Population inference with mortality and attrition in longitudinal studies on aging: A two-stage multiple imputation method. Experimental Aging Research. 2007;33(2):187–203. doi: 10.1080/03610730701239004. [DOI] [PubMed] [Google Scholar]
- Harris TB, Savage PJ, Tell GS, Haan M, Kumanyika S, Lynch JC. Carrying the burden of cardiovascular risk in old age: Associations of weight and weight change with prevalent cardiovascular disease, risk factors, and health status in the Cardiovascular Health Study. American Journal of Clinical Nutrition. 1997;66(4):837–844. doi: 10.1093/ajcn/66.4.837. [DOI] [PubMed] [Google Scholar]
- He XZ, Baker DW. Changes in weight among a nationally representative cohort of adults aged 51 to 61, 1992 to 2000. American Journal of Preventive Medicine. 2004;27(1):8–15. doi: 10.1016/j.amepre.2004.03.016. [DOI] [PubMed] [Google Scholar]
- Hedeker DR, Gibbons RD. Longitudinal data analysis. Hoboken, NJ: John Wiley & Sons, Inc; 2006. pp. 279–313. [Google Scholar]
- Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. Journal of American Medical Association. 2004;291(23):2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- Himes CL. Obesity in later life. Research on Aging. 2004;26(1):3–12. [Google Scholar]
- Himes CL, Reynolds SL. The changing relationship between obesity and educational status. Gender Issues. 2005;22(2):45–57. [Google Scholar]
- House JS, Lantz PM, Herd P. Continuity and change in the social stratification of aging and health over the life course: Evidence from a nationally representative longitudinal study from 1986 to 2001/2002 (Americans' Changing Lives Study) Journal of Gerontology: Social Sciences. 2005;60(2):S15–S26. doi: 10.1093/geronb/60.special_issue_2.s15. [DOI] [PubMed] [Google Scholar]
- Jacobsen BK, Njolstad I, Thune I, Wilsgaard T, Lochen ML, Schirmer H. Increase in weight in all birth cohorts in a general population: The Tromso Study, 1974–1994. Archives of Internal Medicine. 2001;161(3):466–473. doi: 10.1001/archinte.161.3.466. [DOI] [PubMed] [Google Scholar]
- Jenkins KR, Fultz NH, Fonda SJ, Wray LA. Patterns of body weight in middle-aged and older Americans, by gender and race, 1993–2000. Sozial- Und Praventivmedizin. 2003;48(4):257–268. doi: 10.1007/s00038-003-2053-3. [DOI] [PubMed] [Google Scholar]
- Kahn HS, Williamson DF. Is race associated with weight change in US adults after adjustment for income, education, and marital factors? American Journal of Clinical Nutrition. 1991;53(6):1566–1570. doi: 10.1093/ajcn/53.6.1566S. [DOI] [PubMed] [Google Scholar]
- Kahng SK, Dunkle RE, Jackson JS. The relationship between the trajectory of body mass index and health trajectory among older adults: Multilevel modeling analyses. Research on Aging. 2004;26(1):31–61. [Google Scholar]
- Kim J, Durden E. Socioeconomic status and age trajectories of health. Social Science & Medicine. 2007;65(12):2489–2502. doi: 10.1016/j.socscimed.2007.07.022. [DOI] [PubMed] [Google Scholar]
- Lantz PM, Lynch JW, House JS, Lepkowski JM, Mero RP, Musick MA, Williams DR. Socioeconomic disparities in health change in a longitudinal study of US adults: The role of health-risk behaviors. Social Science & Medicine. 2001;53(1):29–40. doi: 10.1016/s0277-9536(00)00319-1. [DOI] [PubMed] [Google Scholar]
- Lewis TT, Everson-Rose SA, Sternfeld B, Karavolos K, Wesley D, Powell LH. Race, education, and weight change in a biracial sample of women at midlife. Archives of Internal Medicine. 2005;165(5):545–551. doi: 10.1001/archinte.165.5.545. [DOI] [PubMed] [Google Scholar]
- Liang J, Bennett JM, Shaw BA, Quinones AR, Ye W, Xu X, Ofstedal MB. Gender differences in functional status in middle and older age: Are there any age variations? Journal of Gerontology: Social Sciences. 2008;63(5):S282–S292. doi: 10.1093/geronb/63.5.s282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang J, Quinones AR, Bennett JM, Ye W, Xu X, Shaw BA, et al. Evolving self-rated health in middle and old age: How does it differ across Black, Hispanic, and White Americans? Journal of Aging and Health. 2010;22(1):3–26. doi: 10.1177/0898264309348877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;35:80–94. [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. 2nd ed. Hoboken, NJ: Wiley-Interscience; 2002. [Google Scholar]
- Losonczy KG, Harris TB, Cornoni-Huntley J, Simonsick EM, Wallace RB, Cook NR, et al. Does weight loss from middle age to old age explain the inverse weight mortality relation in old age? American Journal of Epidemiology. 1995;141(4):312. doi: 10.1093/aje/141.4.312. [DOI] [PubMed] [Google Scholar]
- Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Social Science & Medicine. 1997;44(6):809–819. doi: 10.1016/s0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- McDowell MA, Fryar CD, Ogden CL, Flegal KM. National Center for Health Statistics. Hyattsville, MD: National Health Statistics Reports (NHSR); 2008. Anthropometric reference data for children and adults: United States, 2003–2006. (No.10). [PubMed] [Google Scholar]
- Mehta NK, Chang VW. Mortality attributable to obesity among middle-aged adults in the United States. Demography. 2009;46(4):851–872. doi: 10.1353/dem.0.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molarius A, Seidell J, Sans S, Tuomilehto J, Kuulasmaa K. Educational level, relative body weight, and changes in their association over 10 years: An international perspective from the WHO MONICA project. American Journal of Public Health. 2000;90(8):1260–1268. doi: 10.2105/ajph.90.8.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mroczek DK, Spiro A. Change in life satisfaction during adulthood: Findings from the Veterans Affairs Normative Aging Study. Journal of Personality and Social Psychology. 2005;88(1):189–202. doi: 10.1037/0022-3514.88.1.189. [DOI] [PubMed] [Google Scholar]
- Mujahid MS, Diez Roux AV, Borrell LN, Nieto FJ. Cross-sectional and longitudinal associations of BMI with socioeconomic characteristics. Obesity Research. 2005;13(8):1412–1421. doi: 10.1038/oby.2005.171. [DOI] [PubMed] [Google Scholar]
- Nagi SZ. Disability Policies and Government Policies. New York, NY: Praeger; 1979. The concept and measurement of disability. [Google Scholar]
- Nawaz H, Chan W, Abdulrahman M, Larson D, Katz DL. Self-reported weight and height implications for obesity research. American Journal of Preventive Medicine. 2001;20(4):294–298. doi: 10.1016/s0749-3797(01)00293-8. [DOI] [PubMed] [Google Scholar]
- Newman AB, Yanez D, Harris T, Duxbury A, Enright PL, Fried LP, et al. Weight change in old age and its association with mortality. Journal of American Geriatrics Society. 2001;49(10):1309–1318. doi: 10.1046/j.1532-5415.2001.49258.x. [DOI] [PubMed] [Google Scholar]
- Novak M, Ahlgren C, Hammarström A. A life-course approach in explaining social inequity in obesity among young adult men and women. International Journal of Obesity. 2005;30(1):191–200. doi: 10.1038/sj.ijo.0803104. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, McDowell MA, Flegal KM. National Center for Health Statistics. Bethesda, MD: US Department of Health and Human Services, CDC; 2007. Obesity among adults in the United States: No change since 2003--2004. [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. Journal of American Medical Association. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Palmore E. When can age, period, and cohort be separated. Social Forces. 1978;57:282. [Google Scholar]
- Peeters A, Bonneux L, Nusselder WJ, De Laet C, Barendregt JJ. Adult obesity and the burden of disability throughout life. Obesity Research. 2004;12(7):1145–1151. doi: 10.1038/oby.2004.143. [DOI] [PubMed] [Google Scholar]
- Prentice AM, Jebb SA. Beyond body mass index. Obesity Reviews. 2001;2(3):141–147. doi: 10.1046/j.1467-789x.2001.00031.x. [DOI] [PubMed] [Google Scholar]
- Profenno LA, Porsteinsson AP, Faraone SV. Meta-analysis of Alzheimer’s disease risk with obesity, diabetes, and related disorders. Biological Psychiatry. 2010;67(6):505–512. doi: 10.1016/j.biopsych.2009.02.013. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Reynolds SL, Himes CL. Cohort differences in adult obesity in the United States: 1982–2002. Journal of Aging and Health. 2007;19(5):831–850. doi: 10.1177/0898264307305182. [DOI] [PubMed] [Google Scholar]
- Riley MW. On the significance of age in sociology. American Sociological Review. 1987;52(1):1–14. [Google Scholar]
- Rogosa DR. Myths about longitudinal research. In: Schaie KW, Campbell RT, Meredith WM, Rawlings SC, editors. Methodological issues in aging research. New York, NY: Springer; 1988. pp. 171–209. [Google Scholar]
- Roshania R, Narayan KMV, Oza-Frank R. Age at arrival and risk of obesity among US immigrants. Obesity. 2008;16(12):2669–2675. doi: 10.1038/oby.2008.425. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Olsen MK. Multiple imputation for multivariate missing-data problems: A data Analyst’s perspective. Multivariate Behavioral Research. 1998;33(4):545–571. doi: 10.1207/s15327906mbr3304_5. [DOI] [PubMed] [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. London: Chapman & Hall; 1997. [Google Scholar]
- Seeman TE, Crimmins E. Social environment effects on health and aging integrating epidemiologic and demographic approaches and perspectives. Annals of the New York Academy of Sciences. 2001;954(1):88–117. doi: 10.1111/j.1749-6632.2001.tb02749.x. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Crimmins E, Huang MH, Singer B, Bucur A, Gruenewald T, et al. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Social Science & Medicine. 2004;58(10):1985–1997. doi: 10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- Seidell JC, Visscher TL. Body weight and weight change and their health implications for the elderly. European Journal of Clinical Nutrition. 2000;54(3):33–39. doi: 10.1038/sj.ejcn.1601023. [DOI] [PubMed] [Google Scholar]
- Sobal J, Rauschenbach BS. Gender, marital status, and body weight in older US adults. Gender Issues. 2003;21(3):75–94. [Google Scholar]
- Sorkin JD, Muller DC, Andres R. Longitudinal change in height of men and women: Implications for interpretation of the body mass index: The Baltimore Longitudinal Study of Aging. American Journal of Epidemiology. 1999;150(9):969–977. doi: 10.1093/oxfordjournals.aje.a010106. [DOI] [PubMed] [Google Scholar]
- Thorpe RJ, Jr, Ferraro KF. Aging, obesity, and mortality: Misplaced concern about obese older people? Research on Aging. 2004;26(1):108–129. doi: 10.1177/0164027503258738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truong KD, Sturm R. Weight gain trends across sociodemographic groups in the United States. American Journal of Public Health. 2005;95(9):1602–1606. doi: 10.2105/AJPH.2004.043935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villareal DT, Apovian CM, Kushner RF, Klein S. Obesity in older adults: Technical review and position statement of the American Society for Nutrition and NAASO, the Obesity Society. American Journal of Clinical Nutrition. 2005;82(5):923–934. doi: 10.1093/ajcn/82.5.923. [DOI] [PubMed] [Google Scholar]
- Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: A systematic review and meta-regression analysis. Epidemiologic Reviews. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- Weir D. Elastic powers: The integration of biomarkers into the Health and Retirement Study. In: Weinstein M, Vaupel JW, Wachter KW, editors. Biosocial surveys. Committee on advances in collecting and utilizing biological indicators and genetic information in social science surveys. Washington, DC: National Academies Press; 2008. pp. 78–95. [Google Scholar]
- Whitaker RC, Orzol SM. Obesity among US urban preschool children: Relationships to race, ethnicity, and socioeconomic status. Archives of Pediatrics and Adolescent Medicine. 2006;160(6):578–584. doi: 10.1001/archpedi.160.6.578. [DOI] [PubMed] [Google Scholar]
- Williams DR. Race, socioeconomic status and health. Annals New York Academy of Sciences. 1999;896:173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- Williams DR, Jackson PB. Social sources of racial disparities in health. Health Affairs. 2005;24(2):325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- Williamson DF. Descriptive epidemiology of body weight and weight change in U.S. adults. Annals of Internal Medicine. 1993;119(7 Pt 2):646–649. doi: 10.7326/0003-4819-119-7_part_2-199310011-00004. [DOI] [PubMed] [Google Scholar]
- Winship C, Radbill L. Sampling weights and regression analysis. Sociological Methods & Research. 1994;23(2):230–257. [Google Scholar]
- Woo J, Ho SC, Sham A. Longitudinal changes in body mass index and body composition over 3 years and relationship to health outcomes in Hong Kong Chinese age 70 and older. Journal of the American Geriatrics Society. 2001;49(6):737–746. doi: 10.1046/j.1532-5415.2001.49150.x. [DOI] [PubMed] [Google Scholar]
- Wyke S, Ford G. Competing explanations for associations between marital status and health. Social Science & Medicine. 1992;34(5):523–532. doi: 10.1016/0277-9536(92)90208-8. [DOI] [PubMed] [Google Scholar]
- Zsembik BA, Fennell D. Ethnic variation in health and the determinants of health among Latinos. Social Science & Medicine. 2005;61(1):53–63. doi: 10.1016/j.socscimed.2004.11.040. [DOI] [PubMed] [Google Scholar]