Abstract
Objective. To investigate acute recoil of bioabsorbable poly-L-lactic acid (PLLA) stent. Background. As newly developed coronary stent, bioabsorbable PLLA stent still encountered concern of acute stent recoil. Methods. Sixteen minipigs were enrolled in our study. Eight PLLA XINSORB stents (Weite Biotechnology Co., Ltd., China) and eight metallic stents (EXCEL, Jiwei Co., Ltd. China) were implanted into coronary arteries. Upon quantitative coronary angiography analysis, acute absolute recoil was defined as the difference between mean diameter of inflated balloon (X) and mean lumen diameter of stent immediately after deployment (Y), while acute percent recoil was defined as (X−Y)/X and expressed as a percentage. Intravascular ultrasound (IVUS) was performed immediately after implantation and 24 hours later to compare cross-sectional area (CSA) between two groups and detect stent malapposition or collapse. Results. Acute absolute recoil in XINSORB and EXCEL was 0.02 ± 0.13 mm and −0.08 ± 0.08 mm respectively (P = 0.19). Acute percent recoil in XINSORB and EXCEL was 0.66 ± 4.32% and −1.40 ± 3.83%, respectively (P = 0.45). CSA of XINSORB was similar to that of EXCEL immediately after implantation, so was CSA of XINSORB at 24-hours followup. Within XINSORB group, no difference existed between CSA after implantation and CSA at 24-hours followup. No sign of acute stent malapposition was detected by IVUS. Conclusions. The acute stent recoil of XINSORB is similar to that of EXCEL. No acute stent malapposition or collapse appeared in both kinds of stent. This preclinical study was designed to provide preliminary data for future studies of long-term efficacy and safety of XINSORB stent.
1. Introduction
Coronary stenting has been considered to be a great achievement in the history of percutaneous coronary interventions (PCIs) since 1986 for its utility of diminishing early elastic recoil of vessel wall, which once was one of disadvantages of balloon dilation. Furthermore, drug-eluting stent (DES) successfully inhibits neointima hyperplasia with antiproliferative agents in its polymeric coating. Therefore DES decreases the risk of in-stent restenosis and improves prognosis in comparison to bare metal stent (BMS). However, concerning of late or very late stent thrombosis (ST), which in turn may be associated with nonfatal myocardial infarction or cardiac death, arise after BASKET-LATE study was published in 2006 [1]. Delayed reendothelialization caused by antiproliferative drug plays an important role in ST [2, 3]. Long-term endothelial dysfunction [4, 5], chronic artery inflammation, allergic reaction [6], and possibly jailing side branches are the limitations of current DES.
As a newly developed vessel scaffold, bioabsorbable poly-L-lactic acid (PLLA) stent resists vessel recoil at the early stage after implantation and fully biodegrades into water and carbon dioxide within a period ranging from 10 months to 4 years after the process of vessel wall negative remodeling completes [7], leading to a healed natural vessel without inflammation and restoring normal vasomotor function. However, there is still the concern about acute stent recoil and radial strength of bioabsorbable stent because of the different structure between this polymeric PLLA stent and metallic stent. The Igaki-Tamai stent (Igaki Medical, Kyoto, Japan) was made of PLLA monofilament. Tamai et al. [8] treated 19 lesions with this kind of bioabsorbable stent in human coronary arteries. Quantitative coronary angiography (QCA) and intravascular ultrasound (IVUS) were performed immediately and 1 day after stenting. No acute stent recoil within 1 day was detected. Tanimoto et al. [9] demonstrated that in vivo acute stent recoil of the bioabsorbable everolimus-eluting coronary scaffold (BVS, Abbott Vascular, USA) was 6.85 ± 6.96%, which was slightly higher than that for the metallic everolimus-eluting stent (4.27 ± 7.08%, XIENCE V, Abbott Vascular, USA) from the ABSORB and SPIRIT trials. The improved BVS revision 1.1 has a similar acute recoil property to BVS revision 1.0 [10].
In this study, we designed a balloon-expandable bioabsorbable stent system (XINSORB stent, Shanghai Weite Biotechnology CO., Ltd., China) composed of PLLA as its backbone with sirolimus eluted from the matrix. EXCEL stent (Shandong JIWEI CO., Ltd. China), which was made of 316L stainless steel as its platform with sirolimus released from bioabsorbable polymer, was used as control stent in our study. Acute clinical outcomes of EXCEL stent showed 15% of postprocedure in-lesion percent diameter stenosis and 3.0% of postprocedure in-stent percent diameter stenosis [11]. Long-term clinical outcomes of this commercialized metallic stent have been verified [12, 13]. These two kinds of stents were randomly implanted into porcine coronary arteries. Acute stent recoil, stent malapposition and collapse were tested and compared by QCA and IVUS. We hope to confirm that acute stent recoil of XINSORB stent might be similar to metallic EXCEL stent. This study was designed to provide preclinical observations and generate preliminary data for future studies of long-term efficacy and safety of XINSORB stent.
2. Materials and Methods
2.1. Stent Description
Bioabsorbable XINSORB stent was designed and fabricated by Shanghai Weite Biotechnology Co., Ltd. This stent was composed of bioabsorbable PLLA as its backbone. The molecular weight of PLLA used for XINSORB stent was 300 kDa. Bioabsorbable polymer, poly-D-L-lactic acid (PDLLA) mixed with PLLA, carrying sirolimus, was coated on the stent struts and controlled the release of antiproliferative drug. The stent was carefully mounted on a prewrapped balloon automatically by mounting equipments. Finally, this kind of balloon expandable stent could then be squeezed down and constrained on the delivery system, able to return to that set shape when expanding the balloon in the coronary artery. Then the device was sterilized by γ-ray. The radial strength of XINSORB was more than 1 N. Thickness of strut was 150 μm. The dose of sirolimus on the XINSORB stent was 8 μg/mm. Drug release profile of XINSORB stent was evaluated by immersing stent in a 20 mL of phosphate buffer solution (PBS) containing 4% FBS (Hyclone, pH 7.4) at 37°C in a shaking incubator. At each time point (12 h, 24 h, 48 h, 3 days, 7 days, 14 days, and 28 days), the syringes were quickly removed from the incubator and the concentration of sirolimus in PBS was measured with High-Performance Liquid Chromatography (HPLC, Agilent 1100). About 80% of sirolimus eluted from the polymer in 28 days ex vivo [14]. There were two dots of markers on both ends of the stent, as well as two longitudinal markers on both ends of the balloon. These markers were radiopaque so that they could be detected under fluoroscope although the stent body was radiolucent. These markers showed the position and length of stent in the coronary artery. Optical coherence tomography (OCT, M2x, Light Lab, USA) could clearly demonstrate stent struts as a unique box appearance (Figure 1). The device can be stored at room temperature.
Figure 1.
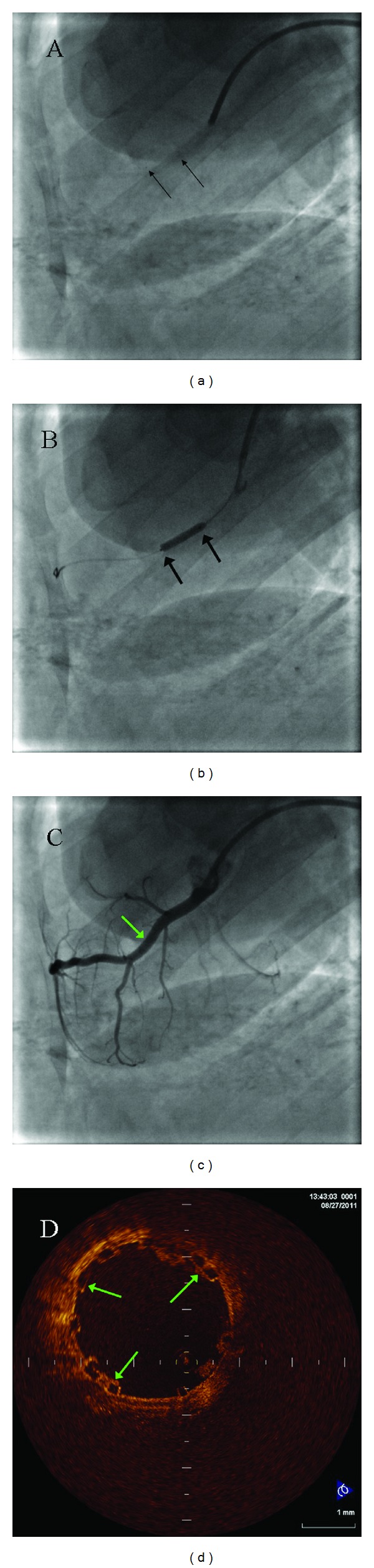
Under fluoroscopy, two dots of markers (slender arrows) can be seen on the both ends of stent, indicating the position and length of stent in the coronary artery, although the body of stent is radiolucent (a). There are also two radiopaque balloon markers (gross arrows), which are used for analysis of balloon diameter by quantitative coronary angiography software (b). After implantation, the stent itself can not be detected by angiography, but with optical coherence tomography (M2x, Light Lab, USA), the stent struts are clarified as a unique box appearance (c and d, green arrows).
EXCEL stents were purchased form Shandong JIWEI CO., Ltd. This sirolimus-eluting stent was made of 316L stainless steel as its platform. Bioabsorbable PLLA polymer carrying sirolimus was coated on its struts.
Size of the stents used in our study was 3.0 mm in diameter and 18 mm in length (3.0 × 18 mm) for both XINSORB and EXCEL.
2.2. Animal Procedure
Minipigs (obtained from Shanghai Miaodi Bio-Sci-Tech Co., Ltd.) weighing 20–25 kg, aging 6–8 months, were used for our study. The study protocol was reviewed and approved by the Animal Care and Use Committee of Zhongshan Hospital Fudan University. Pigs utilized in our study were cared for according to the policies and principles established by the Animal Welfare Act and the NIH Guide for Care and Use of Laboratory Animals. Before procedure started, the animals had been pretreated with aspirin 100 mg and clopidogrel 75 mg daily for 3 days. Animals were injected with 0.3 mg/kg ketamine subcutaneously as basal anesthesia and then 30–40 mg/kg pentobarbital intravenously for continuous sedation. Limb-lead electrocardiography and blood pressure were monitored throughout the procedure. After placement of a sheath in the right femoral artery surgically, unfractured heparin bolus of 200 U/kg was given intravenously to avoid thrombosis. Under fluoroscopic guidance (GE Medical, Innova 2000), a guiding catheter (6F EBU3.5 for left coronary artery and 6F JR3.5 for right coronary artery) was positioned in left and right coronary ostium successively. After infusing 200 μg of nitroglycerin into vessel, coronary angiography was performed in at least two orthogonal views and recorded on cine film. Tortuous arteries were excluded. Arteries whose diameters were larger than 3.0 mm and smaller than 2.5 mm were excluded. Before implantation, XINSORB stents were immersed into normal saline at room temperature for 1 minute. Basing on QCA analysis of the target vessel, the stents of experimental group (XINSORB) or control group (EXCEL) were delivered randomly to the vessel segment in left anterior descending artery (LAD) or right coronary artery (RCA) with a diameter about 2.8 mm and no obvious tapering. One artery accommodated only one stent. Stent deployment was performed using a 1.1 : 1 stent-to-artery ratio which was 8 atm (nominal pressure of balloon) for 20 seconds. The diameter of inflated balloon was recorded. Angiography was repeated after stent implantation for affirmation of complete dilation of stent and no artery dissection. Then IVUS (iLab, Boston Scientific, USA) was performed immediately after implantation to detect whether there was acute stent malapposition or collapse. Both XINSORB and EXCEL underwent IVUS examination. After infusing 200 μg of nitroglycerin into stented vessel through a guiding catheter to relieve possible artery spasm, imaging catheter (40 MHz rotating transducer within a 2.6 Fr imaging sheath) was advanced approximately 10 mm beyond the stent into the distal vessel through a guidewire. The transducer was withdrawn at a speed of 0.5 mm/s back to the guiding catheter. All cines were recorded for further analysis. The cross-sectional area (CSA) at distal, middle, and proximal parts of stent was calculated and analyzed both for XINSORB and EXCEL. At 24-hour followup, angiography and IVUS were performed again following the previous protocol. After the intervention, all catheters were removed. Animals were recovered and housed. Aspirin 100 mg and clopidogrel 75 mg daily were given for 4 weeks.
2.3. Quantitative Coronary Angiography Analysis
All angiograms were analyzed by an independent observer. Measurements were made based on calibration of a contrast-filled catheter and automatic contour detection of treated segment using QCA software package (Sanders Data Systems, CA, USA). Acute absolute recoil was defined as the difference between mean diameter of the inflated balloon (X) and mean lumen diameter of the stent immediately after the balloon deflation (Y). Acute absolute recoil was calculated by X−Y. Acute percent recoil was defined as (X−Y)/X and expressed as a percentage. Analysis of X was performed between two balloon markers, and analysis of Y was performed between two dotted stent markers. The angiogram of X and Y was the same projection so that these two images were perfectly matched.
2.4. Intravascular Ultrasound Analysis
CSA at distal, middle, and proximal parts of stent was recorded both for XINSORB and EXCEL immediately and 24 hours later after implantation. Acute stent malapposition was defined as one or more stent struts clearly separated from the vessel wall with evidence of blood speckles behind the strut in a vessel segment not associated with any side branches immediately after implantation. CSA of stent was defined as the area surrounded by the stent struts. The IVUS images were interpreted by an independent observer blinded to the study protocols.
2.5. Statistical Analysis
All quantitative measurements and histological parameters were obtained by blinded observations. All numerical data are summarized as mean ± standard deviation. Analyses were carried out using PASW Statistics 18.0 software. Independent two-sample t-test was performed to detect the difference between groups. Significance was established by a value of P < 0.05.
3. Results
Eight minipigs were enrolled in this study. Total 16 stents were implanted into porcine coronary arteries (XINSORB = 8 and EXCEL = 8). QCA analysis of angiographic parameters was listed in Table 1. Before implantation, diameter of segment chosen for performing deployment was almost the same (2.78 ± 0.03 mm for XINSORB versus 2.80 ± 0.03 mm for EXCEL, P = 0.18). The stent to artery ratio of XINSORB and EXCEL was comparable (1.09 ± 0.06 versus 1.11 ± 0.02, P = 0.47). No significant difference was detected about mean diameter of the inflated balloon between XINSORB group and EXCEL group (3.02 ± 0.13 mm versus 3.06 ± 0.11 mm, respectively, P = 0.62), as well as mean lumen diameter of the stent (3.00 ± 0.20 mm versus 3.14 ± 0.05 mm, respectively, P = 0.17). The acute absolute recoil in EXCEL was −0.08 ± 0.08 mm, indicating slight enlargement of the lumen after implantation. However, XINSORB represented a similar acute absolute recoil which was 0.02 ± 0.13 mm without apparent difference in comparison to EXCEL (P = 0.19). Obviously, no difference existed between XINSORB and EXCEL in acute percent recoil (0.66 ± 4.32% versus −1.40 ± 3.83%, P = 0.45). At 24-hour followup, the lumen diameter of XINSORB stent was 3.00 ± 0.19 mm, while that of EXCEL was 3.12 ± 0.08 mm, without difference between two groups (P = 0.23).
Table 1.
Angiographic parameters related with acute stent recoil assessment.
| Parameters | XINSORB (N = 8) | EXCEL (N = 8) | P value |
|---|---|---|---|
| Diameter of vessel segment chosen for deployment (mm) | 2.78 ± 0.03 | 2.80 ± 0.03 | 0.18 |
| Stent to artery ratio | 1.09 ± 0.06 | 1.11 ± 0.02 | 0.47 |
| Mean diameter of the inflated balloon (X, mm) | 3.02 ± 0.13 | 3.06 ± 0.11 | 0.62 |
| Mean lumen diameter of stent (Y, mm) | 3.00 ± 0.20 | 3.14 ± 0.05 | 0.17 |
| Mean lumen diameter of stent at 24 hours follow-up (mm) | 3.00 ± 0.19 | 3.12 ± 0.08 | 0.23 |
| Acute absolute recoil (X−Y, mm) | 0.02 ± 0.13 | −0.08 ± 0.08 | 0.19 |
| Acute percent recoil ((X−Y)/X, %) | 0.66 ± 4.32 | −1.40 ± 3.83 | 0.45 |
Every stent was tested by IVUS instantly after implantation. Each stent was adequately expanded and wellpositioned, while there was no sign of acute stent malapposition. IVUS showed a fully expanded XINSORB stent with the polymer struts represented by parallel layers of echoes and without the acoustic shadowing characteristic of metallic stents. IVUS images of distal, middle, and proximal parts of XINSORB immediately after implantation were illustrated in Figure 2. After the stent deployment instantly, distal, CSA of middle and proximal part of XINSORB and EXCEL was calculated and summarized in Table 2. It was clear that CSA of distal, middle, and proximal part of XINSORB was similar to that of EXCEL without significant difference. Within the group of XINSORB, CSA of distal, middle and proximal part of stent was 6.96 ± 0.46 mm2, 6.95 ± 0.50 mm2, and 7.05 ± 0.62 mm2 respectively. No difference existed among these three data (P = 0.87). CSA from distal to proximal of XINSORB seemed to be the same. The similar phenomenon was also detected in EXCEL group (P = 0.56).
Figure 2.
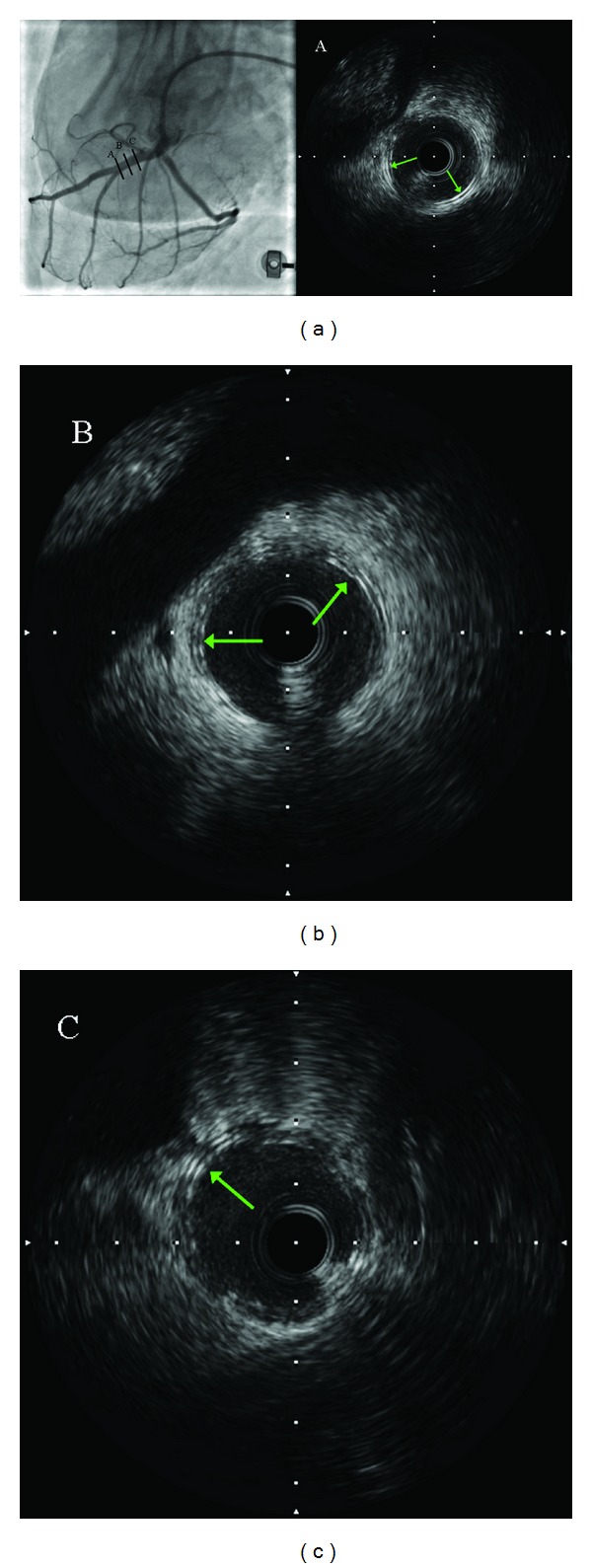
After implantation of XINSORB stent, angiography showed no residual stenosis. There were no acute stent malapposition and the stents were welldeployed by intravascular ultrasound (IVUS). Green arrows show the stent struts. The polymer struts were represented by parallel layers of echoes (a, distal part of XINSORB stent; b, middle part of XINSORB stent; and c, proximal part of XINSORB stent).
Table 2.
IVUS analysis of cross-sectional area of stent to assess acute stent recoil.
| XINSORB (N = 8) | EXCEL (N = 8) | P value | |
|---|---|---|---|
| CAS of immediately after stenting | |||
| Distal part of stent (mm2) | 6.96 ± 0.46 | 7.04 ± 0.24 | 0.67 |
| Middle part of stent (mm2) | 6.95 ± 0.50 | 7.07 ± 0.31 | 0.60 |
| Proximal part of stent (mm2) | 7.05 ± 0.62 | 7.18 ± 0.36 | 0.65 |
| CSA of 24 hours later after stenting | |||
| Distal part of stent (mm2) | 6.99 ± 0.06 | 7.02 ± 0.05 | 0.15 |
| Middle part of stent (mm2) | 6.97 ± 0.06 | 7.02 ± 0.07 | 0.21 |
| Proximal part of stent (mm2) | 7.01 ± 0.08 | 7.07 ± 0.07 | 0.12 |
IVUS: intravascular ultrasound; CSA: cross-sectional area.
At 24 hours after implantation, CSA of distal, middle, and proximal part of XINSORB was 6.99 ± 0.06 mm2, 6.97 ± 0.06 mm2 and 7.01 ± 0.08 mm2 respectively. No difference existed among these three data (P = 0.28). As to EXCEL, CSA of distal, middle and proximal part of stent was 7.02 ± 0.05 mm2, 7.02 ± 0.07 mm2 and 7.07 ± 0.07 mm2, respectively, without difference (P = 0.37) (Figure 3).
Figure 3.
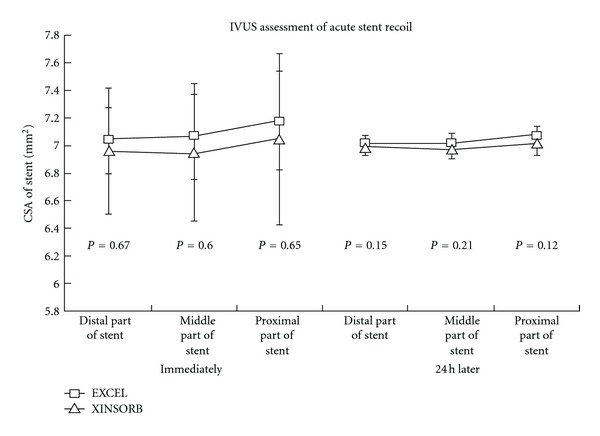
IVUS assessment of acute stent recoil. CSA of distal, middle and proximal parts of XINSORB stent was similar to that for EXCEL immediately after implantation, so was that at 24-hour followup, suggesting no acute stent recoil or collapse during 24-hours followup for both two kinds of stent. IVUS: intravascular ultrasound; CSA: cross-sectional area.
Within XINSORB group, CSA of distal, middle, and proximal parts of stent between immediately after implantation and 24 hours later was compared with paired t-test. The P value was 0.93, 0.92, and 0.86, respectively. CSA of XINSORB stent did not decrease during 24 hours after deployment. As to EXCEL group, P value were also calculated for CSA of distal, middle, and proximal parts of stent between immediately after implantation and 24 hours later. They were 0.78, 0.63, and 0.47, respectively, suggesting no acute recoil after stent implantation.
4. Discussion
The principal findings of this study are as follow: (1) bioabsorbable PLLA XINSORB stent and EXCEL stent were both well expanded, with no sign of acute stent malapposition by IVUS; (2) the acute absolute/percent recoil of XINSORB stent was similar to that of commercialized stainless steel based EXCEL stent; (3) no acute elastic recoil or stent collapse occurred immediately and 24 hours later after XINSORB stent implantation in comparison to EXCEL stent.
In the early era of PCI, the main limitation of percutaneous coronary angioplasty (PTCA) was acute vessel closure caused by elastic recoil after balloon dilation. Metallic stent was developed to scaffold vessel wall after PTCA and successfully prevented this critical complication. Bioabsorbable vessel scaffold is a newly developed coronary stent which has the ability of biodegradation after negative artery remodeling completes. The first polymeric material proposed for a bioabsorbable stent was PLLA [15]. PLLA was chosen for materials of this bioabsorbable stent because of its biocompatibility [16, 17], adequate mechanical properties, and the ability to be processed into scaffolds of different shapes [18]. Polymeric PLLA stent possesses a lot of superiority to metallic stent. In contrast to a permanent metal stent, a completely biodegradable stent may allow the vessel to react to positively remodel and to respond to factors released by endothelium normally. A polymer stent is potentially compatible with imaging by magnetic resonance that will play an increasing role in the future. The stented segment may be suitable for future surgical revascularization, unlike vessels that have undergone extensive metal stent deployment. Up to now, PLLA stents have completed their long-term followup which is 2 to 10 years. Cardiovascular imaging (OCT and IVUS) demonstrated that neither Igaki-Tamai stent nor BVS existed 2 years after initial implantation [19–21], which confirmed that PLLA stents completely biodegraded 2 years after being implanted into human coronary artery. Considering the vascular negative remodel after stent implantation will be terminated within 6 to 9 months as well as the mechanical property of PLLA stent, duration of 2 years may be an optimal choice. However, the strength of PLLA material and its ability to expand with sufficient radial force are essential for successful stent deployment and avoidance of immediate recoil.
Many reasons relate to acute stent recoil. Radial strength and compression pressure are the most essential mechanical capabilities for a stent to scaffold lesions as well as vessel wall elastic recoil. Weak radial strength may lead to residual stenosis after PCI and separation of the stent struts from the intimal surface of the arterial wall. As a result, the stent might shift in the vessel, what is worse, in-stent thrombosis might occur. However, there is no ready answer for the question of how much compression resistance is sufficient. Stack et al. [15] designed the first bioabsorbable PLLA stent in 1988. This kind of stent could bear a crush pressure of 1000 mmHg (1330 kPa) without collapsing. Rieu et al. [22] tested the mechanical performance of 17 coronary stents in vitro. None of these expanded stents deformed noticeably at radial compression pressures up to 30 kPa. Beyond that pressure, stent compression performance differed. Because all 17 metal stents were already clinically proven to be capable of maintaining coronary artery patency, 30 kPa may be considered to be minimum required compression resistance for coronary applications. The current polymeric expandable stent design passes this minimum requirement, and its initial radial compression strength is higher than 200 kPa. Thus, this stent fulfilled the minimum requirement to resist vessel wall elastic recoil [23, 24]. On the other hand, more radial strength or compression pressure does not associate with better outcomes. Exaggerated radial resistance will hinder the natural elasticity of the artery. Additionally, overrigidity will hinder deliverability of the device [25].
Second, coronary stents are affected by a number of external compressive forces during deployment. These include the elastic recoil of the atheromatous lesion and nondiseased sections of the arterial wall. Stents are designed with a high radial force to prevent recoil after deployment. However, there is a relationship between stent delivery balloon underexpansion and metallic stent elastic recoil [26]. Failure of the delivery balloon to reach its target size during stent deployment and subsequent elastic recoil are the mechanism that contributes to stent underdeployment, especially in small vessel. Coil stent suffers greater elastic recoil than slotted tube stent. In normal porcine coronary arteries, acute stent recoil measured by IVUS core wire positioned in the guide wire lumen of the delivery balloon was found to be the predominant mechanism by which metallic stents failed to achieve the nominal CSA [27]. Modification of stent geometry and use of new chromium cobalt alloy with greater radial force may allow maximisation of radial strength. However, there results are acquired from metallic stent. There are no such data about bioabsorbable PLLA stent up to now. Postdilation of the stent with high pressure might be a resolvent.
The thickness of stent plays an essential role in stent recoil. The polymer alone has a limited mechanical performance and a greater recoil rate. Therefore, polymeric PLLA stent requires thicker struts to achieve similar radial strength in comparison to those relative thinner metallic stents. This kind of PLLA stent might not provide enough radial strength with thinner struts less than 150 μm. On the contrary, thicker struts might lead to increased incidence of in-stent restenosis [28, 29]. Balance between radial strength and in-stent restenosis must be carefully considered. Thickness of BVS used in ABSORB study was 150 μm, so was XINSORB stent. Two-year outcomes from ABSORB study demonstrated that in-stent late loss and diameter stenosis of BVS were 0.48 ± 0.28 mm and 27 ± 11%, respectively, without difference from the findings at 6 months [21]. The results showed thickness of currently used bioabsorbable PLLA stent might be the optimal consideration.
In our study, QCA analysis showed no difference in acute absolute/percent recoil between XINSORB and EXCEL. Although XINSORB stents were composed of polymer, they supported the vessel wall just like the metallic stents did, suggesting excellent radial strength. Surprisingly, percent recoil of EXCEL was −1.4%, suggesting the diameter of stent after implantation was slightly larger than that of balloon. We blamed this discrepancy to negligible variety of balloon nominal pressure. Angiography could display diameter of lumen, but it could not descript the detail of stent strut against vessel wall. IVUS can clarify the relationship between stent struts and artery wall. Acute stent malapposition appears as a separation of the stent struts from the intimal surface of the arterial wall. It can easily be detected by IVUS. IVUS also reveals whether stents are welldeployed. In our study, both XINSORB and EXCEL were sufficiently expanded. No sign of acute stent malapposition was found in both groups. After implantation, CSA of distal, middle, and proximal parts of stent was almost the same, suggesting welldeployment of two kinds of stent. At 24 hour later, CSA of XINSORB stent remained steady without significant difference compared to that of EXCEL. Within XINSORB group, CSA of stent did not decrease during 24 hours observation. No stent collapse occurred in the early stage after PCI. XINSORB stent had almost the same acute stent recoil as EXCEL stent.
There are some limitations in this study. The vessel segments selected for stent deployment were relatively straight. Those extremely small, large, or tortuous were excluded. XINSORB stent did not encounter a challenge about flexibility, pushability, and trackability. More importantly, there is no animal model of human vascular disease; there are only animal models of how devices will behave in well-characterized animal models. There is no atherosclerosis in porcine coronary arteries as well as stenosis, calcification. Artery injury is due to overstretching during balloon dilation or stent deployment rather than plaque rupture or lumen obstructive. Pathology and pathophysiology of coronary heart diseases are more complex in human race than porcine model. However, the coronary arteries of pigs respond similarly to human coronary because the stages of neointimal growth described in the porcine model follow those now known in humans [30]. Though the statistics got from the porcine model cannot be regarding as equal to human being, there is no other or better animal model available that closely resembles the human scenario. It should be extensive and careful to apply these data to human. Finally, only one size of XINSORB stent (3.0 × 18 mm) was tested in this study. Whether other stents of different size share the same results remains a question.
Currently, BVS is the unique bioabsorbable PLLA stent which has been commercialized and used in clinical field. Bioabsorbable PLLA XINSORB stent showed excellent early outcomes without acute stent recoil in this preclinical study. Middle- to long-term assessment of this stent will be carried out as soon as possible. When safety and efficacy are proved, XINSORB stent will become an alternative treating coronary heart disease in human being.
5. Conclusion
The acute stent recoil of bioabsorbable PLLA XINSORB stent is similar to that of stainless-steel-based EXCEL stent. No acute stent malapposition or collapse appeared in both kinds of stent. This preclinical study was designed to provide preliminary data for future studies of long-term efficacy and safety of XINSORB stent.
Authors' Contribution
Y. Wu, L. Shen, and Q. Wang contributed equally to this study.
Acknowledgments
The authors thank An Shen, Jianguo Jia, and Ruiming Yao for their excellent technical assistance. This work was supported by the National Basic Research Program (“973” Program) of China (no. 2011CB503905), Shanghai Committee of Science and Technology (no. 11441900300 and 11441900900), and the Specialized Research Fund for the Doctoral Program of Higher Education of China (no. 20110071110053).
References
- 1.Pfisterer M, Brunner-La Rocca HP, Buser PT, et al. Late clinical events after clopidogrel discontinuation may limit the benefit of drug-eluting stents: an observational study of drug-eluting versus bare-metal stents. Journal of the American College of Cardiology. 2006;48(12):2584–2591. doi: 10.1016/j.jacc.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 2.Lang NN, Newby DE. Emerging thrombotic effects of drug eluting stents. Arteriosclerosis, Thrombosis, and Vascular Biology. 2007;27(2):261–262. doi: 10.1161/01.ATV.0000255308.41576.ae. [DOI] [PubMed] [Google Scholar]
- 3.Joner M, Finn AV, Farb A, et al. Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. Journal of the American College of Cardiology. 2006;48(1):193–202. doi: 10.1016/j.jacc.2006.03.042. [DOI] [PubMed] [Google Scholar]
- 4.Hofma SH, Van Der Giessen WJ, Van Dalen BM, et al. Indication of long-term endothelial dysfunction after sirolimus-eluting stent implantation. European Heart Journal. 2006;27(2):166–170. doi: 10.1093/eurheartj/ehi571. [DOI] [PubMed] [Google Scholar]
- 5.Togni M, Windecker S, Cocchia R, et al. Sirolimus-eluting stents associated with paradoxic coronary vasoconstriction. Journal of the American College of Cardiology. 2005;46(2):231–236. doi: 10.1016/j.jacc.2005.01.062. [DOI] [PubMed] [Google Scholar]
- 6.Kim JW, Suh SY, Choi CU, et al. Six month comparison of coronary endothelial dysfunction associated with sirolimus-eluting stent versus Paclitaxel-eluting stent. JACC. 2008;1(1):65–71. doi: 10.1016/j.jcin.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Chen CC, Chueh JY, Tseng H, Huang HM, Lee SY. Preparation and characterization of biodegradable PLA polymeric blends. Biomaterials. 2003;24(7):1167–1173. doi: 10.1016/s0142-9612(02)00466-0. [DOI] [PubMed] [Google Scholar]
- 8.Tamai H, Igaki K, Kyo E, et al. Initial and 6-month results of biodegradable poly-l-lactic acid coronary stents in humans. Circulation. 2000;102(4):399–404. doi: 10.1161/01.cir.102.4.399. [DOI] [PubMed] [Google Scholar]
- 9.Tanimoto S, Serruys PW, Thuesen L, et al. Comparison of in vivo acute stent recoil between the bioabsorbable everolimus-eluting coronary stent and the everolimus-eluting cobalt chromium coronary stent: insights from the ABSORB and SPIRIT trials. Catheterization and Cardiovascular Interventions. 2007;70(4):515–523. doi: 10.1002/ccd.21136. [DOI] [PubMed] [Google Scholar]
- 10.Onuma Y, Serruys PW, Gomez J, et al. Comparison of in vivo acute stent recoil between the bioresorbable everolimus-eluting coronary scaffolds (revision 1.0 and 1.1) and the metallic everolimus-eluting stent. Catheterization and Cardiovascular Interventions. 2011;78(1):3–12. doi: 10.1002/ccd.22864. [DOI] [PubMed] [Google Scholar]
- 11.Sketch MH, Ball M, Rutherford B, Popma JJ, Russell C, Kereiakes DJ. Evaluation of the Medtronic (Driver) cobalt-chromium alloy coronary stent system. American Journal of Cardiology. 2005;95(1):8–12. doi: 10.1016/j.amjcard.2004.08.055. [DOI] [PubMed] [Google Scholar]
- 12.Ge J, Qian J, Wang X, et al. Effectiveness and safety of the sirolimus-eluting stents coated with bioabsorbable polymer coating in human coronary arteries. Catheterization and Cardiovascular Interventions. 2007;69(2):198–202. doi: 10.1002/ccd.20926. [DOI] [PubMed] [Google Scholar]
- 13.Liu HB, Xu B, Yang YJ, et al. Long-term clinical outcomes after bioabsorbable polymer- and durable polymer-based sirolimus-eluting stents implantation: two-year follow-up results from a large single-center database. Chinese Medical Journal. 2009;122(6):681–686. [PubMed] [Google Scholar]
- 14.Shen L, Wang Q, Wu Y, Hu X, Xie J, Ge J. Short-term effects of fully bioabsorbable PLLA coronary stents in a porcine model. Polymer Bulletin. 2012;68(4):1171–1181. [Google Scholar]
- 15.Stack RS, Califf RM, Phillips HR, et al. Interventional cardiac catheterization at Duke Medical Center. American Journal of Cardiology. 1988;62(10, part 2):3F–24F. [PubMed] [Google Scholar]
- 16.Lincoff AM, Furst JG, Ellis SG, Tuch RJ, Topol EJ. Sustained local delivery of dexamethasone by a novel intravascular eluting stent to prevent restenosis in the porcine coronary injury model. Journal of the American College of Cardiology. 1997;29(4):808–816. doi: 10.1016/s0735-1097(96)00584-0. [DOI] [PubMed] [Google Scholar]
- 17.Yamawaki T, Shimokawa H, Kozai T, et al. Intramural delivery of a specific tyrosine kinase inhibitor with biodegradable stent suppresses the restenotic changes of the coronary artery in pigs in vivo. Journal of the American College of Cardiology. 1998;32(3):780–786. doi: 10.1016/s0735-1097(98)00312-x. [DOI] [PubMed] [Google Scholar]
- 18.Yang F, Murugan R, Wang S, Ramakrishna S. Electrospinning of nano/micro scale poly(l-lactic acid) aligned fibers and their potential in neural tissue engineering. Biomaterials. 2005;26(15):2603–2610. doi: 10.1016/j.biomaterials.2004.06.051. [DOI] [PubMed] [Google Scholar]
- 19.Tsuji T, Tamai H, Igaki K, et al. Four-year follow-up of the biodegradable stent (Igaki-Tamai Stent) Circulation Journal . 2004;68, article 135 [Google Scholar]
- 20.Onuma Y, Garg S, Okamura T, et al. Ten-year follow-up of the IGAKI-TAMAI stent. A posthumous tribute to the scientific work of Dr. Hideo Tamai. EuroIntervention. 2009;5(supplement):F109–F111. doi: 10.4244/EIJV5IFA19. [DOI] [PubMed] [Google Scholar]
- 21.Serruys PW, Ormiston JA, Onuma Y, et al. A bioabsorbable everolimus-eluting coronary stent system (ABSORB): 2-year outcomes and results from multiple imaging methods. The Lancet. 2009;373(9667):897–910. doi: 10.1016/S0140-6736(09)60325-1. [DOI] [PubMed] [Google Scholar]
- 22.Rieu R, Barragan P, Masson C, et al. Radial force of coronary stents: a comparative analysis. Catheterization and Cardiovascular Interventions. 1999;46(3):380–391. doi: 10.1002/(SICI)1522-726X(199903)46:3<380::AID-CCD27>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 23.Zilberman M, Nelson KD, Eberhart RC. Mechanical properties and in vitro degradation of bioresorbable fibers and expandable fiber-based stents. Journal of Biomedical Materials Research—Part B Applied Biomaterials. 2005;74(2):792–799. doi: 10.1002/jbm.b.30319. [DOI] [PubMed] [Google Scholar]
- 24.Onuma Y, Serruys PW. Bioresorbable scaffold: the advent of a new era in percutaneous coronary and peripheral revascularization? Circulation. 2011;123(7):779–797. doi: 10.1161/CIRCULATIONAHA.110.971606. [DOI] [PubMed] [Google Scholar]
- 25.Sharkawi T, Cornhill F, Lafont A, Sabaria P, Vert M. Intravascular bioresorbable polymeric stents: a potential alternative to current drug eluting metal stents. Journal of Pharmaceutical Sciences. 2007;96(11):2829–2837. doi: 10.1002/jps.20957. [DOI] [PubMed] [Google Scholar]
- 26.Aziz S, Morris JL, Perry RA, Stables RH. Stent expansion: a combination of delivery balloon underexpansion and acute stent recoil reduces predicted stent diameter irrespective of reference vessel size. Heart. 2007;93(12):1562–1566. doi: 10.1136/hrt.2006.107052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carrozza JP, Hermiller JB, Linnemeier TJ, et al. Quantitative coronary angiographic and intravascular ultrasound assessment of a new nonarticulated stent: report from the Advanced Cardiovascular Systems MultiLink stent pilot study. Journal of the American College of Cardiology. 1998;31(1):50–56. doi: 10.1016/s0735-1097(97)00426-9. [DOI] [PubMed] [Google Scholar]
- 28.Briguori C, Sarais C, Pagnotta P, et al. In-stent restenosis in small coronary arteries: impact of strut thickness. Journal of the American College of Cardiology. 2002;40(3):403–409. doi: 10.1016/s0735-1097(02)01989-7. [DOI] [PubMed] [Google Scholar]
- 29.Pache J, Kastrati A, Mehilli J, et al. Intracoronary stenting and angiographic results: strut thickness effect on restenosis outcome (ISAR-STEREO-2) trial. Journal of the American College of Cardiology. 2003;41(8):1283–1288. doi: 10.1016/s0735-1097(03)00119-0. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz RS, Huber KC, Murphy JG, et al. Restenosis and the proportional neointimal response to coronary artery injury: results in a porcine model. Journal of the American College of Cardiology. 1992;19(2):267–274. doi: 10.1016/0735-1097(92)90476-4. [DOI] [PubMed] [Google Scholar]


