Abstract
Objective
To estimate the number of rotavirus-associated deaths among Indian children younger than five years.
Methods
We surveyed more than 23 000 child deaths from a nationally representative survey of 1.1 million Indian households during 2001–2003. Diarrhoeal deaths were characterized by region, age and sex and were combined with the proportion of deaths attributable to rotavirus, as determined by hospital microbiologic data collected by the Indian Rotavirus Strain Surveillance Network from December 2005 to November 2007. Rotavirus vaccine efficacy data from clinical trials in developing countries were used to estimate the number of deaths preventable by a national vaccination programme. Data were analysed using Stata SE version 10.
Findings
Rotavirus caused an estimated 113 000 deaths (99% confidence interval, CI: 86 000–155 000); 50% (54 700) and 75% (85 400) occurred before one and two years of age, respectively. One child in 242 died from rotavirus infection before five years of age. Rotavirus-associated mortality rates overall, among girls and among boys were 4.14 (99% CI: 3.14–5.68), 4.89 (99% CI: 3.75–6.79) and 3.45 (99% CI: 2.58–4.66) deaths per 1000 live births, respectively. Rates were highest in Bihar, Uttar Pradesh and Madhya Pradesh, which together accounted for > 50% of deaths (64 400) nationally. Rotavirus vaccine could prevent 41 000–48 000 deaths among children aged 3–59 months.
Conclusion
The burden of rotavirus-associated mortality is high among Indian children, highlighting the potential benefits of rotavirus vaccination.
Résumé
Objectif
Estimer le nombre de décès associés au rotavirus chez les enfants indiens de moins de cinq ans.
Méthodes
Nous avons examiné plus de 23 000 décès d'enfants sur la base d'une enquête représentative au niveau national de 1,1 million de foyers indiens durant la période 2001-2003. Les décès par diarrhée étaient classés par région, âge et sexe, ainsi que corrélés à la proportion de décès attribuables au rotavirus, tels que déterminés par les données microbiologiques hospitalières collectées par le réseau de surveillance indien de la souche du rotavirus de décembre 2005 à novembre 2007. Les données d'efficacité du vaccin contre le rotavirus provenant d'essais cliniques réalisés dans les pays en développement ont été utilisées pour estimer le nombre de décès évitables par un programme national de vaccination. Les données ont été analysées à l'aide de Stata SE version 10.
Résultats
Le rotavirus a causé environ 113 000 décès (intervalle de confiance, IC de 99%: 86 000 à 155 000), 50% (54 700) et 75% (85 400) d'entre eux survenaient respectivement avant l’âge d’un an et de deux ans. Un enfant sur 242 est mort d'une infection par le rotavirus avant l'âge de cinq ans. Les taux de mortalité associés au rotavirus étaient, dans l'ensemble, parmi les filles et les garçons, de 4,14 décès (IC de 99%: 3,14-5,68), 4,89 (IC de 99%: 3,75-6,79) et 3,45 (IC de 99%: 2,58-4,66) pour 1 000 naissances vivantes, respectivement. Les taux étaient les plus élevés dans le Bihar, l'Uttar Pradesh et le Madhya Pradesh, représentant au total, à l'échelle nationale, plus de 50% des décès (64 400). Le vaccin contre le rotavirus pourrait éviter 41 000 à 48 000 décès chez les enfants âgés de 3 à 59 mois.
Conclusion
L'impact de la mortalité associée au rotavirus est élevé chez les enfants indiens, soulignant les avantages potentiels d'une vaccination contre le rotavirus.
Resumen
Objetivo
Calcular el número de muertes asociadas al rotavirus entre niños indios menores de cinco años.
Métodos
Estudiamos más de 23 000 muertes de niños procedentes de una encuesta representativa a nivel nacional sobre 1,1 millón de hogares indios durante 2001–2003. Las muertes por diarrea se caracterizaron por región, edad y sexo y se combinaron con la proporción de muertes atribuibles al rotavirus, como determinaron los datos microbiológicos hospitalarios recogidos por la Red india de vigilancia de la cepa del rotavirus (Indian Rotavirus Strain Surveillance Network) desde diciembre de 2005 hasta noviembre de 2007. Los datos acerca de la eficacia de la vacuna contra el rotavirus de ensayos clínicos en países en vías de desarrollo se emplearon para calcular el número de muertes prevenibles por medio de un programa de vacunación nacional. Los datos se analizaron mediante Stata SE versión 10.
Resultados
El rotavirus causó aproximadamente 113 000 muertes (99% intervalo de confianza, IC: 86 000–155 000); el 50% (54 700) y el 75% (85 400) sucedió antes del primer y segundo año de edad, respectivamente. Un niño de cada 242 falleció debido a una infección por rotavirus antes de llegar a los cinco años de edad. Las tasas generales de mortalidad asociadas con el rotavirus entre niños y entre niñas fueron de 4,14 (99% IC: 3,14–5,68), 4,89 (99% IC: 3,75–6,79) y 3,45 (99% IC: 2,58–4,66) muertes por 1 000 nacidos vivos, respectivamente. Las tasas más altas se dieron en Bihar, Uttar Pradesh y Madhya Pradesh, que en conjunto integraron más del 50% de las muertes (64 400) a nivel nacional. La vacuna contra el rotavirus podría prevenir 41 000–48 000 muertes entre niños de entre 3 y 59 meses.
Conclusión
La carga de la mortalidad asociada con el rotavirus es mayor entre los niños indios, y resalta los beneficios potenciales de la vacuna contra el rotavirus.
ملخص
الغرض
تقدير عدد الوفيات المرتبطة بالفيروس العجلي (الروتا) بين الأطفال الهنود الذين تقل أعمارهم عن خمس سنوات.
الطريقة
أجرينا مسحاً لوفيات أكثر من 23000 طفل من خلال مسح تمثيلي على الصعيد الوطني لعدد 1.1 مليون أسرة هندية في الفترة ما بين 2001 إلى 2003. وتم تصنيف وفيات الإسهال حسب المنطقة والعمر والجنس وتم دمجها مع نسبة الوفيات التي تعزى إلى الفيروس العجلي (الروتا)، على النحو المحدد عن طريق البيانات الأحيائية المجهرية الخاصة بالمستشفيات التي جمعتها الشبكة الهندية لترصد سلالة الفيروس العجلي (الروتا) من ديسمبر 2005 وحتى نوفمبر 2007. وجرى استخدام بيانات نجاعة لقاح الفيروس العجلي من التجارب السريرية في البلدان النامية لتقدير عدد الوفيات التي يمكن تجنبها باستخدام برنامج تطعيم وطني. وتم تحليل البيانات باستخدام Stata SE الإصدار 10.
النتائج
تسبب الفيروس العجلي (الروتا) في حوالي 113000 حالة وفاة (فاصل الثقة 99 %، فاصل الثقة:86000 - 155000)؛ و50 % (54700)؛ و75 % (85400) وقعت قبل بلوغ سنة وسنتين من العمر، على التوالي. وتوفي طفل واحد من بين 242 من جراء عدوى الفيروس العجلي قبل بلوغ خمس سنوات من العمر. وكانت معدلات الوفيات المرتبطة بالفيروس العجلي بشكل عام، بين الفتيات والفتيان 4.14 حالة وفاة (99 % فاصل الثقة: 3.14 -5.68 )، و4.89 (99 % فاصل الثقة: 3.75 – 6.79)، و3.45 (99 % فاصل الثقة: 2.58 – 4.66) لكل 1000 ولادة حية، على التوالي. وكانت أعلى المعدلات في بيهار وأوتار براديش وماديا براديش، التي مثلت معاً >50 % من الوفيات (64400) على الصعيد الوطني. ويستطيع لقاح الفيروس العجلي منع ما بين 41000 إلى 48000 حالة وفاة بين الأطفال الذين تتراوح أعمارهم بين 3 إلى 59 شهراً.
الاستنتاج
عبء الوفيات المرتبطة بالفيروس العجلي مرتفعة بين الأطفال الهنود مما يسلط الضوء على الفوائد المحتملة للتطعيم ضد الفيروس العجلي.
摘要
目的
估计印度五岁以下儿童与轮状病毒相关的死亡数。
方法
我们调查了2001 年至2003 年期间110 万印度家庭的全国性典型调查中超过2.3 万例的儿童死亡。按地区、年龄、性别区分腹泻死亡特征,并与2005 年12 月至2007 年11 月由印度轮状病毒监测网络收集的医院微生物数据所确定因轮状病毒所致死亡的比例相结合。使用来自发展中国家临床试验的轮状病毒疫苗有效性数据估计可由国家疫苗接种计划预防的死亡人数。使用Stata SE 10 对数据进行分析。
结果
因轮状病毒引起的死亡人数估计为11.3 万人(99% 置信区间,CI:8.6 万-15.5 万);分别有50%(5.47 万)和75%(8.54 万)出现在一岁和两岁前。对于五岁以下的儿童,242 名儿童中有1 名死于轮状病毒感染。总体而言,与轮状病毒相关的死亡率在女童和男童中分别为4.14(99% CI:3.14-5.68)和4.89(99% CI:3.75-6.79),每1000 名活产婴儿中有3.45 例(99% CI:2.58-4.66)死亡。比哈尔邦、北方邦和中央邦的死亡率最高,这三个邦的死亡数合计超过全国(6.44 万)的50%。在3-59 个月大的儿童中,轮状病毒疫苗可预防4.1-4.8 万例死亡。
结论
印度儿童的轮状病毒相关死亡率负担偏高,凸显了轮状病毒接种疫苗的潜在益处。
Резюме
Цель
Оценить количество смертельных исходов, связанных с ротаривирусом, среди индийских детей в возрасте до пяти лет.
Методы
Было изучено 23 000 случаев детских смертей из национального репрезентативного исследования 1,1 миллиона индийских домохозяйств в течение 2001–2003 гг. Смертельные исходы от диареи были охарактеризованы по региону, возрасту и полу, и были объединены с количеством смертей, связанных с ротавирусом, согласно госпитальным микробиологическим данным, собранным Индийской сетью по эпиднадзору за ретровирусными штаммами в период с декабря 2005 года по ноябрь 2007 года. Данные клинических испытаний по эффективности ротавирусной вакцины в развивающихся странах использовались для оценки числа смертей, которые возможно предотвратить программой национальной вакцинации. Данные анализировались с помощью программного обеспечения Stata SE 10-й версии.
Результаты
По нашим оценкам, ротавирус послужил причиной 113 000 смертей (99% доверительный интервал, ДИ: 86 000–155 000); 50% (54 700) и 75% (85 400) смертей наступило в возрасте от 1 до 2 лет соответственно. Из 242 детей один ребенок скончался от ротавирусной инфекции, не достигнув пятилетнего возраста. Общий уровень смертности от ротаривируса среди девочек и мальчиков составил 4,14 (99% ДИ: 3,14–5,68), 4,89 (99% ДИ: 3,75–6,79) и 3,45 (99% ДИ: 2,58–4,66) смертельных исходов на 1000 живорожденных соответственно. Наивысший уровень отмечен в Бихаре, Уттар-Прадеше и Мадья-Прадеше, на которые приходится > 50% смертельных исходов (64 400) в масштабе всей страны. Ротавирусная вакцина могла бы предотвратить 41 000–48 000 смертей среди детей в возрасте 3–59 месяцев.
Вывод
Основное бремя смертности, связанной с ротавирусом, несут индийские дети, что подчеркивает потенциальные выгоды ротавирусной вакцинации.
Introduction
Diarrhoeal diseases are a major cause of hospitalizations and child deaths globally. Together they account for approximately one in six deaths among children younger than five years.1 Of India’s more than 2.3 million annual deaths among children, about 334 000 are attributable to diarrhoeal diseases.1–3 Rotavirus is the leading cause of severe diarrhoea in children in developed and developing countries.3,4 Two rotavirus vaccines have been shown to be effective against rotavirus and have been licensed in more than 100 countries, including India.5–7 Introduction of these vaccines is expected to reduce child mortality by decreasing the incidence of severe diarrhoea and the frequency of death from diarrhoeal disease.
There is considerable controversy in India regarding the introduction of rotavirus vaccines, especially because of uncertainty surrounding the estimates of deaths and hospitalizations caused by rotavirus and because of the current cost of the vaccines.8 Studies estimate that 90 000–153 000 children die from rotavirus infection in India each year but these numbers are not based on nationally representative samples.3,9,10 Here, we present new estimates of the frequency and number of diarrhoeal deaths attributable to rotavirus among Indian children younger than 5 years by combining direct estimates of diarrhoea-related mortality from a nationally representative study of deaths2 with the fraction of diarrhoeal hospitalizations in selected Indian urban centres that were caused by rotavirus.11 We also calculate the number of deaths preventable in India by a national rotavirus vaccination programme by using the estimated annual number of rotavirus-associated deaths in India and rotavirus vaccine efficacy data from clinical trials in two developing countries.
Methods
We ascertained the number of deaths from diarrhoea among children during 2001–2003 on the basis of findings from the Million Death Study.2,12,13 The Million Death Study is an ongoing project conducted with the Registrar General of India and collaborators to determine causes of death in India. The study derives its data from a nationally representative sample of 6.3 million people in 1.1 million households within the Sample Registration System, a large, routine demographic survey performed by the Registrar General of India in all 28 Indian states and seven union territories that has been the primary system for the collection of Indian fertility and mortality data since 1971. Sample units are randomly selected to ensure that they are representative of the population at the state level. Enrolment in the system is voluntary and its confidentiality and consent procedures are defined as part of the Registration of Births and Deaths Act of 1969. Additional details about the Sample Registration System are available elsewhere.12
A dual-recording system was used in which births and deaths were continuously enumerated by a resident part-time enumerator and a retrospective survey was conducted independently every six months by a full-time supervisor. When a death occurred, the cause was assessed using the Routine, Reliable, Representative and Re-sampled Household Investigation of Mortality with Medical Evaluation, a standard verbal autopsy questionnaire.13,14 Two independent physicians reviewed the field reports and assigned a single cause of death by use of International classification of diseases, 10th revision codes.15 Deaths were defined as due to diarrhoea if they received a final code of A00–A09. Differences in coding were resolved by anonymous reconciliation of initial codes and, if needed, a third, senior physician adjudicated the final cause of death. We characterized diarrhoeal deaths by sex, age (< 1 month, 1–2 months, 3–11 months, 12–23 months and 24–59 months) and region (central, east, north, north-east, south and west). Sex-, age- and region-specific live births and deaths were corrected proportionally by use of methods described elsewhere2 to reflect the United Nations estimates of live births and deaths in India in 2005.
To estimate the number of deaths attributable to rotavirus infection, the annual number of diarrhoeal deaths by region was multiplied by the regional age-specific proportion of confirmed rotavirus infections among children hospitalized with diarrhoea. For example, the percentage of diarrhoea-associated hospitalizations due to rotavirus infection among boys aged 12–23 months in the state of Punjab was multiplied by the estimated number of diarrhoeal deaths among boys aged 12–23 months in the north region. Rotavirus data were obtained from the Indian Rotavirus Strain Surveillance Network (IRSSN) and covered admissions to 10 hospitals in 7 cities from December 2005 to November 2007.16 Overall, faecal samples from 1405 (39%) of 3580 children hospitalized with diarrhoea during this period tested positive for rotavirus by means of a commercial enzyme immunoassay.16 No data were available from the IRSSN for the central region, so we used an age-specific average of proportions from the other regions. In sensitivity analyses, we also applied the IRSSN age-specific rotavirus proportions from the regions with the highest and lowest rotavirus proportions (the north-east and west regions, respectively) to the central region.
Most diarrhoeal deaths in the Million Death Study occurred outside hospital (90%; 2734 of 3053) and in rural areas (92%; 2798 of 3053).2 Because no laboratory-confirmed data on the etiology of diarrhoea were available for children who died outside hospital, we assumed that, of these deaths, the proportion due to rotavirus infection reflected the proportion of deaths due to laboratory-confirmed rotavirus infection among children hospitalized with diarrhoeal disease. The proportion of diarrhoea cases attributable to rotavirus infection increases with the severity diarrhoea, so we also assumed that diarrhoea resulting in death in rural settings with limited access to health care is similar in severity to the diarrhoea that would be treated in hospitals in settings with more accessible health care.
To estimate the number of deaths preventable by a national rotavirus vaccination programme, we multiplied the estimated annual number of rotavirus-associated deaths in India by the values of vaccine efficacy from field studies of the monovalent rotavirus vaccine (Rotarix; GlaxoSmithKline, London, United Kingdom of Great Britain and Northern Ireland) in Malawi (efficacy, 49%) and the pentavalent bovine reassortant vaccine (Rotateq; Merck, Whitehouse Station, United States of America) in Bangladesh (efficacy, 43%).17,18 On-time vaccination and 100% coverage were assumed. Because infants aged < 3 months are too young to be fully vaccinated, we applied vaccine efficacy data only to children aged 3–59 months. We also calculated the number of children who would need to be vaccinated to save one life on the basis of the following method described by Kelly et al.: number needed to vaccinate = 1/([annual event rate attributed to disease among unvaccinated individuals] × [vaccine efficacy for prevention of the event]).19 All statistical analysis was performed using Stata SE version 10 (StataCorp. LP, College Station, United States of America).
This study was approved by the institutional review board of the Postgraduate Institute of Medical Education and Research (Chandigarh, India), the Indian Council of Medical Research, the Indian Health Ministry’s Screening Committee and the institutional review board of St Michael’s Hospital (Toronto, Canada).
Results
In the Million Death Study, 3053 (13.2%) of 23 152 deaths among children younger than 5 years were due to diarrhoea (Table 1).2 This corresponds to approximately 334 000 diarrhoeal deaths nationally during 2005, or 1 in 82 Indian children dying from diarrhoea before the age of 5 years. On the basis of IRSSN data, rotavirus was estimated to cause approximately 34% (113 000; 99% confidence interval, CI: 86 000–155 000) of all diarrhoeal deaths in this age group. Together, these findings yielded an estimated mortality rate of 4.14 (99% CI: 3.14–5.68) deaths per 1000 live births during 2005 and suggest that approximately 1 in 242 children will die from rotavirus infection before their fifth birthday.
Table 1. Deaths from diarrhoea – all-cause and rotavirus-attributable – detected during the study and estimated nationally, among Indian children younger than 5 years, by age, during 2005a.
| Age (months) | Study findings |
National estimates, 2005a |
||||
|---|---|---|---|---|---|---|
| All-cause diarrhoea deaths (No.)b | Deaths attributable to RV (%)c | All-cause diarrhoea deaths (No.) | Deaths attributable to RV (No.)d | Mortality ratee (99% CI) | ||
| < 1 | 241 | 26.0 | 31 800 | 8 300 | 0.30 (0.22–0.67) | |
| 1–2 | 368 | 26.1 | 30 600 | 8 000 | 0.29 (0.18–0.47) | |
| 3–11 | 811 | 42.8 | 89 700 | 38 400 | 1.41(1.08–1.82) | |
| 12–23 | 634 | 44.2 | 69 500 | 30 700 | 1.12 (0.85–1.47) | |
| 24–59 | 996 | 24.9 | 111 300 | 27 700 | 1.01 (0.81–1.27) | |
| Overall | 3053 | 34.0 | 334 000 | 113 000 | 4.14 (3.14–5.68) | |
CI, confidence interval; MDS, Million Death Study; RV, rotavirus infection.
a Data are corrected on the basis of United Nations estimates of live births (n = 27 311 155) and deaths in India during 2005.
b Data are from Million Death Study, 2001–2003. Values do not sum to the overall value because the month of death was missing for three children.
c Data are from the Indian Rotavirus Strain Surveillance Network, 2005–2007. Overall value is weighted to the age distribution in the MDS.
d Cumulative proportion of all rotavirus-attributable deaths is as follows: < 1 month, 8%; < 2 months, 14%; < 12 months, 47%; < 24 months, 75%; < 60 months, 100%. The overall value is rounded to the nearest 1000.
e Deaths from rotavirus diarrhoea per 1000 live births.
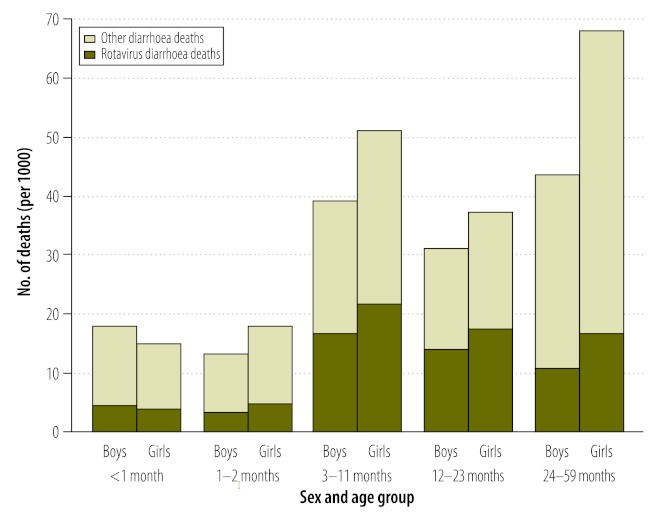
The estimated rotavirus-associated mortality rate varied by region, age and sex during 2005 (Appendix A, available at: http://www.cghr.org/wordpress/wp-content/uploads/Rotavirus-BWHO_Web-Table-1_20120103.doc). The rate among girls (4.89 deaths per 1000 live births; 99% CI: 3.75–6.79) was 42% higher than among boys (3.45 deaths per 1000 live births; 99% CI: 2.58–4.66) (Table 2). Overall, about 64 000 girls (99% CI: 49 000–89 000) and 49 000 boys (99% CI: 37 000–66 000) died from rotavirus infection. At every age group beyond the neonatal period, the ratio of the rotavirus-associated mortality rate among girls to the rate among boys exceeded 1.30 deaths per 1000 live births and peaked at 1.70 deaths per 1000 live births between ages 24 and 59 months. Approximately 50% of rotavirus-associated deaths (54 700 of 113 000) occurred in the first year of life and about 75% (85 400 of 113 000) occurred in the first two years of life (Fig. 1).
Table 2. Estimated rotavirus-attributable diarrhoeal deaths and mortality rates among Indian children younger than 5 years, by age and sex, during 2005.
| Age (months) | Boys |
Girls |
Mortality rate ratio, girls vs boys | |||
|---|---|---|---|---|---|---|
| Deaths (No.) | Mortality ratea (99% CI) | Deaths (No.) | Mortality ratea (99% CI) | |||
| < 1 | 4 400 | 0.31 (0.24–0.46) | 3 900 | 0.30 (0.20–0.90) | 0.97 | |
| 1–2 | 3 300 | 0.23 (0.14–0.38) | 4 700 | 0.36 (0.23–0.56) | 1.57 | |
| 3–11 | 16 700 | 1.18 (0.90–1.52) | 21 700 | 1.66 (1.27–2.14) | 1.41 | |
| 12–23 | 13 800 | 0.97 (0.71–1.31) | 16 900 | 1.29 (1.00–1.63) | 1.33 | |
| 24–59 | 10 800 | 0.76 (0.59–0.99) | 16 900 | 1.29 (1.06–1.57) | 1.70 | |
| Overall | 49 000b | 3.45 (2.58–4.66)b | 64 000b | 4.89 (3.75–6.79)c | 1.41 | |
CI, confidence interval.
a Deaths per 1000 live births.
b The value is rounded to the nearest 1000.
c The value denotes the cumulative mortality rate, calculated as the no. of rotavirus deaths in first five years of life divided by the no. of children born in one year.
Note: Values were calculated using data from the Million Death Study (collected during 2001–2003) and the Indian Rotavirus Strain Surveillance Network (collected during 2005–2007) that were corrected on the basis of United Nations estimates of live births (14 180 792 boys and 13 130 363 girls) and deaths in India during 2005.
Fig. 1.
Estimated overall number of diarrhoeal deaths and rotavirus-attributable diarrhoeal deaths among Indian children younger than 5 years, by age and sex, during 2005
Note: The mean percentage of deaths attributable to rotavirus among boys and girls from the Indian Rotavirus Strain Surveillance Network was 26% for ages 0–2 months, 43% for ages 3–11 months, 44% for ages 12–23 months and 25% for ages 24–59 months. Values were calculated using data from the Million Death Study (collected during 2001–2003) and the Indian Rotavirus Strain Surveillance Network (collected during 2005–2007) that were corrected on the basis of United Nations estimates of live births (14 180 792 boys and 13 130 363 girls) and deaths in India during 2005.
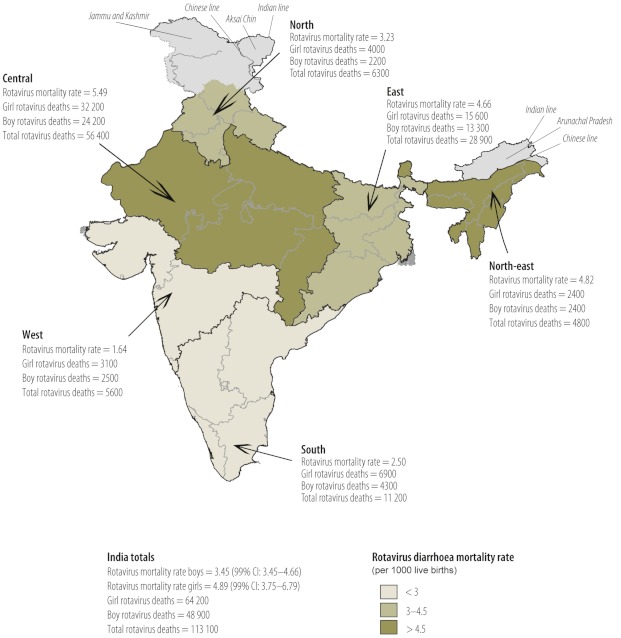
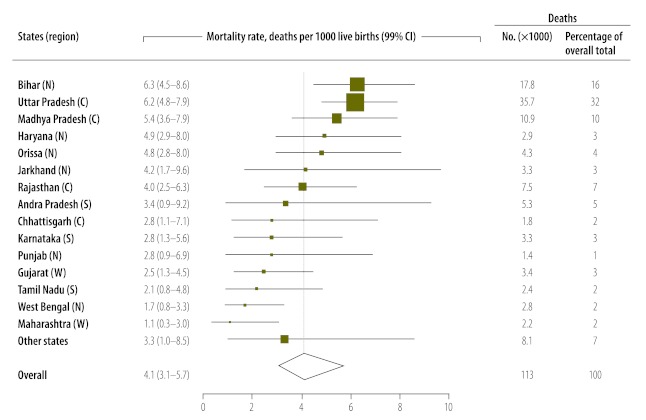
Most rotavirus-associated deaths during 2005 occurred in the central region (56 400) and east region (28 900) (Fig. 2). The mortality rate from rotavirus-associated gastroenteritis among children younger than five years ranged from a low of 1.64 deaths per 1000 live births in the west region to a high of 5.49 deaths per 1000 live births in the central region. The age distribution of deaths from rotavirus infection was similar for boys across regions but girls in the north and south regions died at somewhat earlier ages than those in other regions (data not shown). Rotavirus-associated deaths were not distributed evenly across the country (Fig. 3). More than half (64 400) of deaths were estimated to occur in three states: Uttar Pradesh (35 700 deaths), Bihar (17 800) and Madhya Pradesh (10 900). The sensitivity analysis involving use of varying proportions of rotavirus-associated deaths for the central region did not markedly change the national totals.
Fig. 2.
Estimated rotavirus-attributable diarrhoeal deaths and mortality rates among Indian children younger than 5 years, by age and sex, during 2005
CI, confidence interval.
Note: Values were calculated using data from the Million Death Study (collected during 2001–2003) and the Indian Rotavirus Strain Surveillance Network (collected during 2005–2007) that were corrected on the basis of United Nations estimates of live births (14 180 792 boys and 13 130 363 girls) and deaths in India during 2005.
Source of shapefile: GfK Geomarketing, Bruchsal, Germany.
Fig. 3.
Estimated mortality rates and diarrhoeal deaths due to rotavirus infection among Indian children younger than 5 years, by state, during 2005
CI, confidence interval; C, central region; N, north region; NE, north-east region; E, east region, S, south region; W, west region.
Note: Data for the 15 states with the greatest number of estimated rotavirus deaths is shown and are arranged by estimated rotavirus mortality rates, with data for the remaining states grouped together under “Other states”. The size of the boxes denoting mortality rates is proportionate to the state’s total estimated rotavirus deaths.
Values were calculated using data from the Million Death Study (collected during 2001–2003) and the Indian Rotavirus Strain Surveillance Network (collected during 2005–2007) that were corrected on the basis of United Nations estimates of live births (14 180 792 boys and 13 130 363 girls) and deaths in India during 2005.
Between 41 000 and 48 000 deaths among children aged 3–59 months (18 000–20 000 boys and 24 000–27 000 girls) could be avoided every year by administering one of the currently available rotavirus vaccines. These figures correspond to 3.6–4.2% of the 1 135 000 deaths in this group, with a greater benefit for girls (3.6–4.0% of 505 000 deaths among boys, compared with 3.8–4.3% of 630 000 deaths among girls) if vaccination coverage and timing for both sexes were equal. On the basis of our estimated rotavirus-associated mortality rates for boys and girls 3–59 months old (2.91 and 4.23 deaths per 1000 live births, respectively), 570 girls and 660 boys would need to be vaccinated against rotavirus to prevent 1 girl and 1 boy, respectively, from dying due to rotavirus infection.
Discussion
Approximately 113 000 children (99% CI: 86 000–155 000) younger than five years died from rotavirus infection in India in 2005, for a mortality rate of 4.14 (99% CI: 3.14–5.68) deaths per 1000 live births. This suggests that roughly 1 child in 242 will die from rotavirus infection by the age of 5 years. The first year of life was the period of highest risk for death due to rotavirus infection, a finding that underscores the need for on-time vaccination.20 At every age beyond the neonatal period, a marked sex-related disparity was apparent and more girls than boys died from rotavirus infection. The greatest discrepancy by sex and region existed between girls in the central region (mortality rate, 6.55 deaths per 1000 live births) and boys in the south region (mortality rate, 1.88 deaths per 1000 live births), with a mortality rate ratio of 3.5 for girls relative to boys.
Our mortality estimates, which are based on directly measured data on diarrhoea-associated deaths, are similar to previously published estimates of 122 0003 and 122 000–153 00010 rotavirus-associated deaths that were based on indirect national estimates of deaths attributable to diarrhoea among children younger than five years. Our estimate is higher than that of Jain et al.9 who multiplied the fraction of diarrhoeal deaths due to rotavirus infection by the total number of diarrhoeal deaths in India and concluded that rotavirus caused approximately 98 000 deaths during 1998. Unlike these earlier estimates, our results provide age-, sex- and region-specific patterns of rotavirus-associated mortality in India, which can be used to optimize the influence of rotavirus vaccination programmes.
Rotavirus vaccine is available in India through the private sector, although on a small scale. Therefore, the number of vaccinated children is likely to be exceedingly small, although no data on who is being vaccinated are available. Our data indicate that if rotavirus vaccine were delivered as part of a national programme, about 4% of all deaths among Indian children younger than five years could be prevented. This would make rotavirus vaccine a valuable component of India’s strategy to reduce childhood mortality.
One of the most important findings in this study is the sex-based difference in mortality. Increased overall and disease-specific mortality rates among Indian girls have previously been shown for children of different ages.2,21 Various factors associated with increased mortality rates have been documented to be more common among girls, including poor nutritional status, delayed or incomplete vaccination or none, limited access to health care and failure to seek medical attention, and decreased likelihood of receiving appropriate antibiotic therapy.20,22–25 The study of these factors, especially about what is needed to minimize sex-based differences, must be a key component of interventions to reduce overall childhood mortality in India.
This study has several limitations. First, the main potential source of uncertainty in our estimates involves possible misclassification bias attributable to the use of verbal autopsy to ascertain causes of death. However, for infants older than one month, the accuracy of diagnosis by verbal autopsy has been shown to be reasonably similar to that of hospital-reference diagnosis when diarrhoea is defined as frequent liquid, watery, loose or soft stools or dysentery: sensitivities for verbal autopsy ranged from 72% to 91% and specificities ranged from 57% to 78% in studies in Bangladesh, Nicaragua and Uganda.26 However, we caution that hospital-based studies are not an appropriate comparison for the large number of rural, unattended deaths.2 Second, because most diarrhoeal deaths recorded in the Million Death Study occurred outside hospital and/or in rural areas, it was not feasible to obtain samples from these individuals for microbiologic analysis. Consequently, our estimates are based on the assumption that, of the children who died from diarrhoeal disease outside hospital, the proportion of deaths due to rotavirus infection reflects the proportion of deaths due to laboratory-confirmed rotavirus infection among hospitalized children with severe diarrhoeal disease. Third, the largest absolute number of diarrhoeal deaths occurred in the central region, an area where the IRSSN does not collect rotavirus data. However, the use of various proportions from the national rotavirus surveillance study did not greatly alter our national totals (range, 106 000–114 000 deaths; data not shown), primarily because the large number of estimated rotavirus-attributable deaths in the central region is mainly a result of the underlying high diarrhoeal mortality rate in the region.2,27 Fourth, the Million Death Study data are from 2001–2003, the IRSSN data are from 2005–2007 and the rotavirus-associated mortality burden we estimated is projected onto India’s 2005 population. Because it is possible that the diarrhoeal mortality rate and the proportion of severe diarrhoea cases due to rotavirus infection have changed over the past 5–10 years, our estimates may not be accurate. However, although use of more recent data would have been ideal, no other more recent nationally representative source of comparable data exists. Some data suggest that there has not been any substantial change in at least some of the key factors driving diarrhoeal mortality; a review of India’s District Level Household Survey 3 showed that between 2002–2004 and 2007–2008, the percentage of children with diarrhoea who received oral rehydration solution (30.3% versus 34.2%) and sought medical treatment (73.2% versus 70.6%) changed only minimally.24 The survey also shows that less than one quarter of India’s population has access to piped water and that well under one half has access to relatively improved means of sanitation and human waste disposal.24 Data collection in the Million Death Study continues to the present date and we hope to analyse more recent data, including for time trends, in the future. Fifth, our calculation of avoidable deaths from rotavirus infection assumes on-time vaccination of the complete cohort of vaccine-eligible children. Unfortunately, overall vaccination coverage among children in India remains low and significant discrepancies in vaccination rates between boys and girls persist.20 In addition, it is likely that many of the children who received delayed vaccination or who are unvaccinated have other characteristics that increase their risk of dying from a diarrhoeal episode and thus we may have overestimated the benefits of the vaccine. Finally, our calculations relied on vaccine efficacy findings from Bangladesh and Malawi, rather than from India. Although it is reasonable to apply vaccine efficacy data from settings similar to India, assessment of the effectiveness of rotavirus vaccine after it is introduced will help refine our estimates of vaccine-preventable rotavirus deaths.
Findings from this study support the introduction of rotavirus vaccine in India, particularly in states such as Bihar and Uttar Pradesh, where rotavirus-associated mortality rates are high. Although a national rotavirus vaccination programme can play a key role in achieving the United Nations Millennium Development Goal of reducing child mortality,28 ongoing evaluation must be conducted to address major gaps in knowledge. The cost-effectiveness of a national rotavirus vaccination programme is among the most prominent gaps29 and the data presented here can serve as a basis for future analysis of this and other factors that can prepare policy-makers for decisions about how to optimally target health-care interventions and policies to reduce rotavirus infection and diarrhoeal deaths in India.
Acknowledgements
The Registrar General of India established the Sample Registration System in 1971, has continued it ever since and is collaborating with several of the authors on the ongoing Million Death Study. The opinions expressed in this paper are those of the authors and do not necessarily represent those of the Government of India, the United States National Institutes of Health or the United States Centers for Disease Control and Prevention. We thank Brendon Pezzack, Chinthanie Ramasundarahettige, Peter Rodriguez, Vicky Hsiao and Wilson Suraweera for data support. Much of this work was conducted when one of the authors (SKM) was a research fellow at the Centre for Global Health Research, Li Ka Shing Knowledge Institute, St Michael’s Hospital.
Funding:
This work was supported by the Fogarty International Centre of the United States National Institutes of Health (grant R01 TW05991–01), the Canadian Institute of Health Research (grant IEG-53506), the International Development Research Centre (grant 102172), the Li Ka Shing Knowledge Institute and Keenan Research Centre at St Michael's Hospital, University of Toronto, and the United States Fund for the United Nations Children’s Fund (subgrant 50140, via a grant from the Bill & Melinda Gates Foundation for the Child Health Epidemiology Reference Group). Authors received support from the Canada Research Chair programme (PJ) and from the Paediatric Scientist Development Program, the Sick Kids Foundation, the Paediatric Chairs of Canada and the March of Dimes (SKM). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Competing interests:
None declared.
References
- 1.Black RE, Cousins S, Johnson HL, Johnson HL, Lawn JE, Rudan I, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 2.Million Death Study Collaborators. Bassani DG, Kumar R, Awasthi S, Morris SK, Paul VK, et al. Causes of neonatal and child mortality in India: a nationally representative mortality survey. Lancet. 2010;376:1853–60. doi: 10.1016/S0140-6736(10)61461-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parashar UD, Burton A, Lanata C, Boschi-Pinto C, Shibuya K, Steele D, et al. Global mortality associated with rotavirus disease among children in 2004. J Infect Dis. 2009;200(Suppl 1):S9–15. doi: 10.1086/605025. [DOI] [PubMed] [Google Scholar]
- 4.Parashar UD, Hummelman EG, Bresee JS, Miller MA, Glass RI. Global illness and deaths caused by rotavirus disease in children. Emerg Infect Dis. 2003;9:565–72. doi: 10.3201/eid0905.020562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vesikari T, Matson DO, Dennehy P, Van Damme P, Santosham M, Rodriguez Z, et al. Safety and efficacy of a pentavalent human-bovine (WC3) reassortant rotavirus vaccine. N Engl J Med. 2006;354:23–33. doi: 10.1056/NEJMoa052664. [DOI] [PubMed] [Google Scholar]
- 6.Linhares AC, Velazquez FR, Perez-Schael I, Saez-Llorens X, Abate H, Espinoza F, et al. Efficacy and safety of an oral live attenuated human rotavirus vaccine against rotavirus gastroenteritis during the first 2 years of life in Latin American infants: a randomised, double-blind, placebo-controlled phase III study. Lancet. 2008;371:1181–9. doi: 10.1016/S0140-6736(08)60524-3. [DOI] [PubMed] [Google Scholar]
- 7.Ruiz-Palacios GM, Perez-Schael I, Velazquez FR, Abate H, Breuer T, Clemens SC, et al. Safety and efficacy of an attenuated vaccine against severe rotavirus gastroenteritis. N Engl J Med. 2006;354:11–22. doi: 10.1056/NEJMoa052434. [DOI] [PubMed] [Google Scholar]
- 8.Lone Z, Puliyel JM. Introducing pentavalent vaccine in the EPI in India: a counsel for caution. Indian J Med Res. 2010;132:1–3. [PubMed] [Google Scholar]
- 9.Jain V, Parashar UD, Glass RI, Bhan MK. Epidemiology of rotavirus in India. Indian J Pediatr. 2001;68:855–62. doi: 10.1007/BF02762113. [DOI] [PubMed] [Google Scholar]
- 10.Tate JE, Chitambar S, Esposito DH, Sarkar R, Gladstone B, Ramani S, et al. Disease and economic burden of rotavirus diarrhoea in India. Vaccine. 2009;27(Suppl 5):F18–24. doi: 10.1016/j.vaccine.2009.08.098. [DOI] [PubMed] [Google Scholar]
- 11.Kang G, Kelkar SD, Chitambar SD, Ray P, Naik T. Epidemiological profile of rotaviral infection in India: challenges for the 21st century. J Infect Dis. 2005;192(Suppl 1):S120–6. doi: 10.1086/431496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jha P, Gajalakshmi V, Gupta PC, Kumar R, Mony P, Dhingra N, et al. Prospective study of one million deaths in India: rationale, design, and validation results. PLoS Med. 2006;3:e18. doi: 10.1371/journal.pmed.0030018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morris SK, Bassani DG, Kumar R, Awasthi S, Paul VK, Jha P. Factors associated with physician agreement on verbal autopsy of over 27000 childhood deaths in India. PLoS ONE. 2010;5:e9583. doi: 10.1371/journal.pone.0009583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centre for Global Health Research [Internet]. Million Death Study. Toronto: CGHR; Available from: http://www.cghr.org/index.php/publications/million-death-study/ [accessed 22 May 2012].
- 15.International statistical classification of diseases and related health problems, 10th revision Geneva: World Health Organization; 2007. [Google Scholar]
- 16.Kang G, Arora R, Chitambar SD, Deshpande J, Gupte MD, Kulkarni M, et al. Multicenter, hospital-based surveillance of rotavirus disease and strains among Indian children aged <5 years. J Infect Dis. 2009;200(Suppl 1):S147–53. doi: 10.1086/605031. [DOI] [PubMed] [Google Scholar]
- 17.Madhi SA, Cunliffe NA, Steele D, Witte D, Kirsten M, Louw C, et al. Effect of human rotavirus vaccine on severe diarrhea in African infants. N Engl J Med. 2010;362:289–98. doi: 10.1056/NEJMoa0904797. [DOI] [PubMed] [Google Scholar]
- 18.Zaman K, Dang DA, Victor JC, Shin S, Yunus M, Dallas MJ, et al. Efficacy of pentavalent rotavirus vaccine against severe rotavirus gastroenteritis in infants in developing countries in Asia: a randomised, double-blind, placebo-controlled trial. Lancet. 2010;376:615–23. doi: 10.1016/S0140-6736(10)60755-6. [DOI] [PubMed] [Google Scholar]
- 19.Kelly H, Attia J, Andrews R, Heller RF. The number needed to vaccinate (NNV) and population extensions of the NNV: comparison of influenza and pneumococcal vaccine programmes for people aged 65 years and over. Vaccine. 2004;22:2192–8. doi: 10.1016/j.vaccine.2003.11.052. [DOI] [PubMed] [Google Scholar]
- 20.Corsi DJ, Bassani DG, Kumar R, Awasthi S, Jotkar R, Kaur N, et al. Gender inequity and age-appropriate immunization coverage in India from 1992 to 2006. BMC Int Health Hum Rights. 2009;9(Suppl 1):S3. doi: 10.1186/1472-698X-9-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morris SK, Bassani DG, Awasthi S, Kumar R, Shet A, Suraweera W, et al. Diarrhea, pneumonia, and infectious disease mortality in children aged 5 to 14 years in India. PLoS ONE. 2011;6:e20119. doi: 10.1371/journal.pone.0020119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mathew JL. Inequity in childhood immunization in India: a systematic review. Indian Pediatr. 2012;49:203–23. doi: 10.1007/s13312-012-0063-z. [DOI] [PubMed] [Google Scholar]
- 23.Registrar General of India, Centre for Global Health Research. Causes of death in India in 2001–2003. Sample Registration System New Delhi: Government of India; 2009. [Google Scholar]
- 24.International Institute for Population Sciences. District Level Household and Facility Survey (DLHS-3), 2007-08 Mumbai: IIPS; 2010. [Google Scholar]
- 25.International Institute for Population Sciences & Macro International. National Family Health Survey (NFHS-3), 2005-06 Mumbai: IIPS; 2008. [Google Scholar]
- 26.Anker M, Black RE, Coldham C, Kalter HD, Quigley MA. A standard verbal autopsy method for investigating causes of death in infants and children Geneva: World Health Organization; 1999.
- 27.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 28.United Nations Development Programme [Internet]. Millennium Development Goals. New York: UNDP; 2012. Available from: http://web.undp.org/mdg/index.shtml [accessed 22 May 2012].
- 29.Jha P, Laxminarayan R. Choosing health: an entitlement for all Indians. Available from: http://cghrindia.org/images/choosing-health.pdf [accessed 22 May 2012].