Abstract
Enough solid evidence now exists to offer women several fundamental strategies for healthy eating. They include emphasizing healthful unsaturated fats, whole grains, good protein “packages,” and fruits and vegetables; limiting consumption of trans and saturated fats, highly refined grains, and sugary beverages; and taking a multivitamin with folic acid and extra vitamin D as a nutritional safety net. A diet based on these principles is healthy through virtually all life stages, from young adulthood through planning for pregnancy, pregnancy, and on into old age.
Keywords: diet, health, cardiovascular disease, cancer, pregnancy, fertility
INTRODUCTION
“What is a healthy diet?” Many clinicians find themselves at a loss to answer this common question from patients. The difficulty of offering a simple answer is understandable. The overwhelming volume of data generated by food and nutrition researchers coupled with sometimes contradictory findings, the seeming flip-flops in recommendations, and the flood of misinformation in diet books and the media can make it seem as though explaining the essentials of healthy eating is akin to describing the intricacies of particle physics. That is unfortunate, because there are now enough solid strands of evidence from reliable sources to weave simple but compelling recommendations about diet.
In the United States and other developed countries, the average woman can expect to live 80 years or more.1 With such longevity, it isn’t enough merely to consume the calories needed to sustain the body, build it, and repair it. The foods that supply these calories can influence the risk of developing chronic conditions, which range from heart disease and cancer to osteoporosis and age-related vision loss.
Although much remains to be learned about the role of specific nutrients in decreasing the risk of chronic disease, a large body of evidence supports the utility of healthy dietary patterns that emphasize whole-grain foods, legumes, vegetables, and fruits, and that limit refined starches, red meat, full-fat dairy products, and foods and beverages high in added sugars. Such diets have been associated with decreased risk of a variety of chronic diseases.2
Diet, of course, is just one approach to preventing illness. Limiting caloric intake to maintain a healthy weight, exercising regularly, and not smoking are three other essential strategies. Compelling data from the Nurses’ Health Study show that women who followed a healthy lifestyle pattern that includes these four strategies were 80% less likely to develop cardiovascular disease over a 14-year period compared to all other women in the study.3 A companion study, the Health Professionals Follow-up Study, showed that similar healthy choices were beneficial in men, even among those who were taking medications to lower blood pressure or cholesterol.4
In this article, we present evidence-based elements of healthful nutrition and an overview of healthy dietary patterns. We also touch on three special situations: diet and fertility, diet and pregnancy, and diet and weight loss.
DIETARY FAT
Dietary fat is a terribly misunderstood and mistakenly maligned nutrient. Myths and messages that have persisted since the 1960s warn that “fat is bad.” That dangerous oversimplification has helped launch dozens of largely ineffective diets and the development of thousands of fat-free but calorie-laden foods. It has also helped fuel the twin epidemics of obesity and type 2 diabetes. The message “fat is bad” is problematic because there are four main types of dietary fat with dramatically different effects on health.
Trans fats from partially hydrogenated oils are undeniably bad for the cardiovascular system and the rest of the body. These largely man-made fats elevate harmful low-density lipoprotein (LDL) cholesterol, reduce protective high-density lipoprotein (HDL) cholesterol, stimulate inflammation, and cause a variety of other changes that damage arteries and impair cardiovascular health.5 Higher intake of trans fat has been associated with an increased risk for developing cardiovascular disease, type 2 diabetes, gall stones, dementia, and weight gain.5 Saturated fats from red meat and dairy products increase harmful LDL, but also increase HDL. A moderate intake of saturated fat (under 8% of daily calories) is compatible with a healthy diet, whereas consumption of greater amounts has been associated with cardiovascular disease. Monounsaturated and polyunsaturated fats from vegetable oils, seeds, nuts, whole grains, and fish—especially the polyunsaturated omega-3 fatty acids—are important components of a healthy diet and are also essential for cardiac health. Eating polyunsaturated fats in place of saturated and trans fats lowers harmful LDL, elevates protective HDL, improves sensitivity to insulin, and stabilizes heart rhythms.6
Dietary fat per se is not associated with risk of chronic disease. In fact, diets that include up to 40% of calories from fat can be quite healthy if they are low in trans and saturated fat and emphasize polyunsaturated and monounsaturated fat.7 Although definitive data are not available on the optimal proportions of dietary fats, a low intake of trans and saturated fat and a higher intake of unsaturated fats reduce the risk of cardiovascular disease and diabetes.
CARBOHYDRATES
In the United States, the reduction in the intake of dietary fat from 45% of calories in 1965 to approximately 34% today was accompanied by an increase in the intake of carbohydrates.8 These extra carbohydrates were largely in the form of highly processed grains. Processing removes fiber, healthful fats, and an array of vitamins, minerals, and phytonutrients, making processed grains such as white flour or white rice nutritionally impoverished compared with whole-grain versions. Consumption of a diet rich in highly processed grains is associated with an increase in triglycerides and a reduction in protective HDL.9 These adverse responses may be aggravated in the context of insulin resistance, which often develops during pregnancy. The prevalence of insulin resistance and type 2 diabetes are both increasing in the United States and around the world.
The Glycemic Index
The glycemic response refers to the measurable increase in blood sugar after consuming carbohydrates. The greater the postprandial spike in glucose a food generates, the greater that food’s glycemic index. Highly refined grains cause a more rapid and a greater overall increase in blood sugar than less-refined whole grains.10 Greater glycemic responses are accompanied by increased plasma insulin levels, which are thought to be at the root of metabolic syndrome11 and have also been implicated in ovulatory infertility.12 Diets with a high glycemic index or glycemic load (the product of dietary glycemic index and total carbohydrate intake) appear to increase the risks of type 2 diabetes and coronary artery disease, particularly among women who have some insulin resistance.13 The dramatic loss of fiber and micronutrients during the milling process may also contribute to these adverse effects of highly processed grains.
In contrast, whole grains and foods made from whole grains, along with fruits, vegetables, and beans, provide slowly digested carbohydrates that are rich in fiber, vitamins, minerals, and phytonutrients. A substantial body of evidence indicates that eating whole grains or cereals high in fiber, rather than highly refined grains, reduces the risk of cardiovascular disease14 and type 2 diabetes.15 Although reductions in the risk of colon cancer by diets rich in whole-grain fiber have been difficult to document, such a dietary pattern has been clearly associated with reductions in constipation and diverticular disease.
PROTEIN
To the metabolic systems engaged in protein production and repair, it is immaterial whether amino acids come from animal or plant protein. However, protein is not consumed in isolation. Instead, it is packaged with a host of other nutrients. The quality and amount of fats, carbohydrates, sodium, and other nutrients in the “protein package” may influence long-term health. For example, results from the Nurses’ Health Study suggest that eating more protein from beans, nuts, seeds, and the like, while cutting back on easily digested carbohydrates reduces the risk of heart disease.16 In that study, eating more animal protein while cutting back on carbohydrates did not reduce heart disease risk, possibly because of the fats and other nutrients that come along (or don’t come along) with protein from animals.
VEGETABLES AND FRUITS
“Eat more fruits and vegetables” is timeless advice that has the backing of a large body of evidence.17 Vegetables and fruits provide fiber, slowly digested carbohydrates, vitamins and minerals, and numerous phytonutrients that have been associated with protection against cardiovascular disease, aging-related vision loss due to cataract and macular degeneration, and maintenance of bowel function. The connection between vegetables and fruits and cancer is less well established. Although they do not have a blanket anticancer effect, fruits and vegetables may work against specific cancers, including esophageal, stomach, lung, and colorectal cancer.18
Fruits and vegetables should be consumed in abundance, which means a minimum of five servings a day—and more is better. As few as 1 in 4 persons in the United States meet this guideline.19
BEVERAGES
The ideal beverage provides 100% of what the body needs—H2O—without any calories or additives. Water has all of those qualifications. From the tap, it costs a fraction of a penny per glass. After water, the two most commonly consumed beverages are tea and coffee. Both are remarkably safe beverages, and have been associated with reduced risks of type 2 diabetes,20 kidney stones and gallstones, and possibly heart disease and some types of cancer.
Two problematic beverages are sugar-sweetened drinks (sodas, fruit drinks, juices, sports drinks, etc.) and alcoholic drinks. One 12-ounce can of sugar-sweetened cola delivers 8–10 teaspoons of sugar, approximately 120–150 “empty” calories.21 Not surprisingly, daily consumption of sugary beverages has been associated with weight gain and increased risk of type 2 diabetes,22 heart disease,23 and gout.24 Alcohol in moderation (no more than one drink a day for women, 1–2 drinks a day for men) has been associated with reduced risks of cardiovascular disease and type 2 diabetes. On the other hand, even moderate drinking may increase the risk of breast cancer.
However, it is possible that a diet rich in folate may attenuate this risk. In the Nurses’ Health Study, the risk of breast cancer associated with alcohol intake was strongest among women with total folate intake less than 300 μg/d for alcohol intake ≥15 grams (g)/d vs <15 g/d which is the alcohol content of one “standard” drink. The multivariate relative risk (RR) was 1.32; 95% confidence interval (CI), 1.15–1.50. For women who consumed at least 300 μg/d of total folate, there was no increased risk of breast cancer associated with alcohol intake.25 Drinking alcohol during pregnancy is not recommended due to possible health hazards to the developing child.
VITAMINS AND MINERALS
An optimal diet generally provides all the vitamins, minerals, and other micronutrients needed for good health. However, many women in the U.S., and a very large percentage of poor women, do not follow optimal diets.3 Thus, for most women a daily multivitamin-multimineral supplement provides good insurance against nutritional deficiencies. Such supplements usually include extra iron, which is needed by the 9% to 11% of premenopausal women with iron deficiency.26
The most firmly established benefit of vitamin supplements is that additional folic acid can reduce the risk of neural tube defects by approximately 70%.27 Current guidelines call for all women of childbearing age to take a daily supplement containing 400 to 800 micrograms (μg) of folic acid, or 4 milligrams (mg) for women with a child with a neural tube defect.
Calcium is important for the maintenance of bone strength. Precisely how much calcium is needed is a controversial question. World Health Organization guidelines recommend an intake of 400 mg/day. In the United Kingdom, 700 mg/day is considered adequate for women aged 19 years and older. In the United States, dietary guidelines recommend that adult women receive 1,500 mg of calcium daily,28 in large part by consuming 3 servings of low-fat or fat-free dairy products a day.29 A lower-calorie, no-fat option is to get calcium from supplements.
For maintaining bone strength, other factors—including physical activity and vitamin D—are as important, or more important, than calcium. There is mounting evidence that current recommendations for vitamin D (200–600 IU/day, depending on age) are too low, and that 1,000 IU/day provides better protection against fractures and possibly heart disease and some cancers30 (see Focus on Vitamin D). Excess intake of preformed vitamin A (retinol) has been associated with an increased risk of hip fracture, possibly by competing with vitamin D.31 However, elevated risk is seen at intakes slightly higher than the current Dietary Reference Intake of 700 μg per day. Given this concern, a multivitamin that delivers much of its vitamin A as beta-carotene is preferred.
WEIGHT CONTROL, EXERCISE
Body weight sits like a spider at the center of a web of health and disease. Excess weight predisposes an individual to the development of a host of chronic conditions. The higher the body mass index (BMI) > 25 kg/m2, the greater the prevalence of abnormal blood glucose, lipids and blood pressure; hypertension and cardiovascular disease; diabetes; many cancers; gallstones; sleep apnea; complications of pregnancy; infertility; and premature mortality. Under the current national guidelines, a BMI between 18 and 25 kg/m2 is considered optimal, and the best health experience is achieved by avoiding increases in weight during adulthood.
Maintaining a healthy body weight, or losing weight, is a direct function of calories consumed and expended. Portion control is essential for weight maintenance. The percentage of calories from dietary fat has little relationship with weight maintenance, while low consumption of sugary beverages and trans fats and higher intake of dietary fiber appear to be helpful. Regular exercise and the avoidance of extreme inactivity, such as excessive television watching, are also integral strategies for weight control. A supportive social and physical environment are also important.
DIETARY PATTERNS
Although research on nutrients such as fats, carbohydrates, and specific vitamins and minerals has been revealing, it has also generated some dead ends, along with myths and confusion about what constitutes healthy eating. A key reason is because people eat food, not nutrients. Furthermore, humans tend to follow relatively repeatable dietary patterns. Although it is harder to study dietary patterns than it is to study nutrients, new research has shown how some dietary patterns are good for long-term health.
One dietary pattern that may harm long-term health is the typical Western diet—rich in red meat, highly processed grains, and sugar, and lacking in fruits, vegetables, whole grains, and fiber. A host of studies have emphasized that this type of dietary pattern promotes atherosclerosis and a variety of cardiovascular conditions, including heart attack and stroke, peripheral vascular disease, and heart failure.32, 33
One alternative is provided by the Dietary Guidelines for Americans.29 These guidelines are revised every five years by a panel that was once appointed by the U.S. Department of Agriculture (USDA). The Department of Health and Human Services is now also involved in the process. According to the USDA, the guidelines “provide authoritative advice for people two years and older about how good dietary habits can promote health and reduce risk for major chronic diseases.”
In an effort to make the guidelines more accessible to the public, they were initially distilled into the Food Guide Pyramid. Unfortunately, this ubiquitous symbol illustrated the goals of U.S. agriculture as much as it represented the principles of healthful eating. The Food Guide Pyramid offered no guidance on grains; it lumped together red meat, poultry, fish, and beans, and it asked us to judge these protein sources by their total fat content. The Food Guide Pyramid promoted drinking three glasses of low-fat milk or eating three servings of other dairy products per day; and made no distinction between types of fat, recommending that fat be consumed “sparingly.” The Food Guide Pyramid was retired in 2005 and replaced with the abstract MyPyramid (Figure 1), which cannot be deciphered without access to the accompanying Web site. The replacement of food groups with vertical stripes (orange for grains, green for vegetables, red for fruits, yellow for oils, blue for dairy and purple for meat and beans) was a win for the food industry, which took issue with the original Food Guide Pyramid because it represented foods near the bottom as “good” and those near the top as “bad.” The left-to-right design presents all foods as being nutritionally equal.
Figure 1. MyPyramid, designed by the USDA in 2006.

The vertical stripes in MyPyramid.gov represent different food groups and their relative contributions to a healthy diet. The figure is meaningless without information from its corresponding Web site.
NOTE: High-resolution file available for free download at: http://www.mypyramid.gov/global_nav/media_resources.html
Permission to Reprint:
All of the informational materials produced by the USDA Center for Nutrition Policy and Promotion, whether printed or maintained electronically on this website, are in the public domain and as such are not restricted by copyright law unless otherwise stated.
We ask only that informational materials, both graphic and text, provided by CNPP be reproduced as originally designed and/or written and that they not be altered or edited in any way. For accuracy and continuity of the message, we encourage all users to reproduce the information as original designed and/or written. [note: The MyPyramid image has not been altered in any way.]
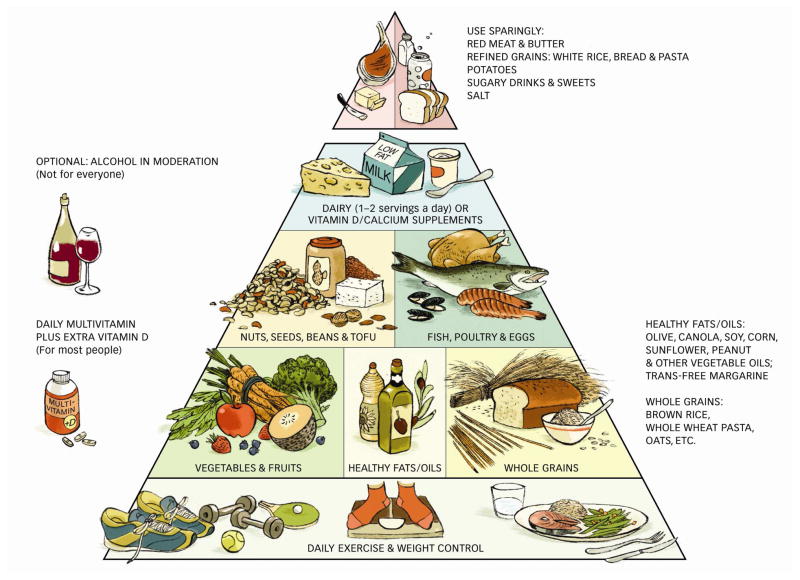
A better dietary pattern is embodied in the Healthy Eating Pyramid (Figure 2), which was developed by faculty members in the Department of Nutrition at Harvard School of Public Health based on the best available evidence. The dietary strategies embodied in this pyramid are summarized in Table 1.
Figure 2. The Healthy Eating Pyramid.
The Healthy Eating Pyramid provides evidence-based information on the elements of a diet that is good for long-term health.
[NOTE: High-resolution image available for free download at: http://www.hsph.harvard.edu/nutritionsource/what-should-you-eat/pyramid/index.html]
Permission to reprint:
The Healthy Eating Pyramid image is owned by the President and Fellows of Harvard College. It may be used without permission for educational and other non-commercial uses with proper attribution, including the following copyright notification and credit line:
Copyright © 2008. For more information about The Healthy Eating Pyramid, please see The Nutrition Source, Department of Nutrition, Harvard School of Public Health, http://www.thenutritionsource.org, and Eat, Drink, and Be Healthy, by Walter C. Willett, M.D. and Patrick J. Skerrett (2005), Free Press/Simon & Schuster Inc.
(http://www.hsph.harvard.edu/nutritionsource/what-should-you-eat/pyramid/index.html)
Table 1.
Elements of healthy eating
| Choose healthy fats over unhealthy fats. |
|
| Choose slowly digested carbohydrates over highly refined ones. | Limit intake of sources of rapidly digested carbohydrates such as white flour, white rice, pastries, sugary drinks, and French fries. In their place, emphasize whole grains (such as brown rice, barley, bulgur, quinoa, and wheat berries), whole fruits and vegetables, beans, and nuts. Aim for at least 6 servings of whole grains a day. Choosing a whole-grain breakfast cereal and whole grain bread are excellent starts. |
| Pick the best protein packages by emphasizing plant sources of protein rather than animal sources. | Adopting a “flexitarian” approach to protein has long-term health payoffs. Aim for at least half of protein from plants—beans, nuts, seeds, whole grains, fruits, and vegetables. Choose fish, eggs, poultry for most of the rest, with small amounts of red meat and dairy making up the balance. Aim for two servings of fish per week.** |
| Accentuate fruits and vegetables. | Consider 5 servings of fruit and vegetables a daily minimum; 9 a day is even better. Eat for variety and color. Each day try to get at least one serving of a dark green leafy vegetable, a yellow or orange fruit or vegetable, a red fruit or vegetable, and a citrus fruit. Fresh is usually best, especially if it is local; frozen fruits and vegetables are nearly as good. |
| Opt for low-calorie hydration. | Water is the best choice for hydration. Coffee and tea in moderation (with only a small amount of milk or sugar) are generally safe and healthful beverages. If milk is part of the diet, skim or low-fat milk is best. Avoid sugar-laden drinks such as sodas, fruits drinks, and sports drinks. Limit fresh juice to one small glass a day. Alcohol in moderation (no more than one drink a day for women) if at all. |
| Meet the daily recommendations for vitamins and minerals. | Taking an RDA-level multivitamin-multimineral supplement each day that contains folic acid and 1,000 IU of vitamin D provides an inexpensive nutritional safety net. Many premenopausal women need extra iron, and some women need additional calcium. |
| Daily exercise | Calories expended are as important for good health as the quality and quantity of calories consumed. Current recommendations call for 30 minutes of physical activity such as brisk walking on most, if not all, days of the week. |
for a diet of 2,000 calories a day
low-mercury choices are best, especially for women who are pregnant or breastfeeding
Adapted from Willett WC, Skerrett PJ. Eat, Drink, and Be Healthy: the Harvard Medical School Guide to Healthy Eating. New York: Free Press; 2005
For individuals who would rather follow a set dietary pattern instead of building their own based on the Healthy Eating Pyramid, a Mediterranean-type diet or the DASH diet can have profoundly positive effects on health (Table 2).
Table 2.
Elements of two healthy dietary patterns
| Mediterranean- type diet55 |
|
| DASH diet38, 39* |
|
In the DASH diet, servings listed are based on a diet of 2,000 calories per day.
Mediterranean Diet
Traditional diets developed in countries surrounding the Mediterranean Sea have been linked with lower rates of heart disease and other chronic conditions. Such diets also appear to transplant well to foreign soil. Among the 166,012 women participating in the National Institutes of Health AARP Diet and Health Study, those whose diets most closely matched a traditional Mediterranean diet had reduced risks of all-cause mortality (multivariate hazard ratio [HR], 0.80; 95% CI, 0.75–0.85), cardiovascular mortality (HR, 0.81; 95% CI, 0.68–0.97) and cancer mortality (HR, 0.88; 95% CI, 0.78–1.00) compared with those following a Western diet.34 A similar trend was observed for men. The impact was even greater among smokers. The Mediterranean diet has other health benefits as well, such as reduced risk of cancer, Parkinson’s disease, and Alzheimer’s disease.35 It has also been associated with control of asthma36 and improvement in rheumatoid arthritis.37
Although there is no single diet that can be called “the” Mediterranean diet, those worthy of the name are high in extra virgin olive oil; high in whole grain foods and fiber; and rich in fruits, vegetables, legumes, and nuts. Small portions of cheese and yogurt are eaten daily; fish is consumed in varying amounts; red meat, poultry, eggs, and sweets are consumed sparingly. Modest amounts of red wine complement meals, and regular physical activity is a part of daily life. An example of a Mediterranean-type diet is listed in the Table 2.
A DASH of Prevention
In the 1990s, the National Heart, Lung, and Blood Institute sponsored a randomized, controlled trial called Dietary Approaches to Stop Hypertension (DASH) to see if certain changes in diet could lower blood pressure. The DASH diet emphasized fruits, vegetables, and low-fat dairy foods and limited red meat, saturated fats, and sweets. Compared with an average American diet, the DASH diet lowered participants’ systolic blood pressure by an average of 5.5 mm Hg and diastolic pressure by 3 mm Hg.38 A low-sodium DASH approach was even more effective; the results were comparable to those from trials of antihypertensive medications.39 The impact of the DASH diet goes beyond lowering blood pressure. It has since been shown to reduce weight,40 the risk of coronary heart disease and stroke,41 and the development of kidney stones.42 Details of the DASH diet can be downloaded for free from the National Heart, Lung, and Blood Web site (see Box 1, More information).
BOX 1. MORE INFORMATION.
Women (and clinicians) seeking more information on healthful eating can be directed to the following resources:
General nutrition
Willett WC, Skerrett PJ. Eat, Drink, and Be Healthy: The Harvard Medical School Guide to Healthy Eating. New York: Free Press; 2005
U.S. Department of Health and Human Services and U.S. Department of Agriculture. Dietary guidelines for Americans 2005. Washington, DC: U.S. Department of Agriculture, 2005; www.healthierus.gov/dietaryguidelines
The Nutrition Source, a free online publication of the Department of Nutrition, Harvard School of Public Health, www.hsph.harvard.edu/nutritionsource.
Healthful diet patterns
Keys A and Keys M. How to Eat Well and Stay Well the Mediterranean Way. Garden City, NY: Doubleday; 1975
National Heart, Lung, and Blood Institute. Your Guide to Lowering Your Blood Pressure with DASH. Available for free at www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf
Diet and fertility
Chavarro JE, Willett WC, and Skerrett PJ. The Fertility Diet. New York: McGraw-Hill; 2008
Mediterranean-type and DASH-type diets aren’t the only dietary patterns under investigation. Data from the Optimal Macronutrient Intake Trial to Prevent Heart Disease (OmniHeart,) suggest that substituting protein or unsaturated fat for some of the carbohydrates in an already healthy diet can further lower blood pressure, improve lipid levels, and reduce estimated cardiovascular risk.43 University of Toronto investigators created what has been dubbed the portfolio dietary pattern. This mostly vegetarian diet targeted cholesterol by adding specific foods known to lower LDL: oats, barley, psyllium, okra, and eggplant, all of which are rich in soluble fiber; soy protein; whole almonds, and margarine enriched with plant sterols. This portfolio of cholesterol-lowering foods reduced the mean LDL values by 29% and did not harm HDL.44
DIET AND FERTILITY
An estimated 2 million American women cope with infertility each year.45 Some turn to assisted reproduction, others struggle in silence. Although farmers and ranchers have long recognized a connection between diet and fertility in farm animals, surprisingly little research has been done into connections between the two in humans. The largest, longest, and most systematic investigation of associations between diet and fertility was recently conducted as part of the Nurses’ Health Study. The participants of the diet and fertility substudy included 18,555 women who said on one of the Nurses’ Health Study biennial surveys that they were trying to become pregnant, none of women had previously reported problems with infertility. Over an 8-year follow-up period, these women reported more than 25,217 pregnancies and/or pregnancy attempts that lasted from a few weeks to more than twelve months. A total of 3,209 of the women (13%) had difficulty becoming pregnant, including 438 diagnosed with ovulatory infertility, the leading cause of female-factor infertility. Data from this nested case-control study revealed ten diet and lifestyle strategies that were associated with decreased risk for ovulatory infertility (Box 2). The results were published in a series of articles examining individual factors.12, 46–53 After creating a “fertility diet” score based on these factors, women in the highest quintile of this score had significantly lower risks for ovulatory infertility (RR, 0.34; 95% CI, 0.23–0.48) and other causes of infertility (RR, 0.73; 95% CI, 0.57–0.95) than those in the lowest quintile. A combination of five or more low-risk lifestyle factors, including diet, weight control, and physical activity, was associated with a 69% lower risk of ovulatory disorder infertility and an estimated population attributable risk of 66% (95% confidence interval 29%–86%).49
Box 2. DIETARY STRATEGIES OBSERVED IN THE NURSES’ HEALTH STUDY THAT REDUCED THE RISK OF OVULATORY INFERTILITY49.
| Avoid trans fats. |
| Include more unsaturated vegetable oils in the diet, such as olive oil or canola oil, and cut back on saturated fat from red meat and other sources. |
| Eat more vegetable protein, like beans and nuts, and less animal protein. |
| Choose whole grains and other sources of carbohydrate that have lower, slower effects on blood sugar and insulin rather than highly refined carbohydrates. |
| Temporarily trade in skim milk and low- or no-fat dairy products like cottage cheese and frozen yogurt for their full-fat counterparts. |
| Take a multivitamin that contains folic acid and other B vitamins. |
| Get plenty of iron from fruits, vegetables, beans, and supplements, but not from red meat. |
| Limit the intake of sugared sodas. |
| Aim for a healthy weight. If needed, losing between 5 and 10 percent of starting weight may improve ovulation. |
| Women who are sedentary or overweight should begin regular exercise. Lean women who exercise strenuously should cut back to moderate exercise. |
DIET AND PREGNANCY
Good nutrition can optimize maternal health throughout pregnancy, reduce the risk of birth defects, promote optimal fetal growth and development, and prevent chronic health problems in the developing child. The American College of Obstetrics and Gynecology and the American Dietetic Association recommend that women generally follow the Dietary Guidelines for Americans before becoming pregnant and during pregnancy. Other key strategies include appropriate weight gain; appropriate physical activity; vitamin (folic acid) and mineral (iron) supplementation as needed; and avoiding alcohol, tobacco, and other harmful substances.
Recent advisories about mercury in fish have prompted some women to avoid eating fish during pregnancy. However, the omega-3 fatty acids in many types of fish promote healthy fetal development. Eating average amounts of seafood containing low levels of mercury during pregnancy has not been shown to cause problems. The Food and Drug Administration and Environmental Protection Agency advise women who are pregnant or breastfeeding that it is safe to eat up to 12 ounces (2 average meals) a week of a variety of fish and shellfish that are lower in mercury.54 Types of seafood low in mercury include anchovies, catfish, flounder, mackerel, pollock, salmon, sardines, shrimp, and tilapia.
Other articles in this issue discuss the importance of omega-3 fatty acids and Vitamin D during pregnancy. Jordan stresses that pregnant women should consume between 200–300 mg daily from safe food sources, such as purified fish and algal oil supplements and DHA enriched egg, which are alternative sources for pregnant women who do not eat fish.55 Kendall-Tackett reviews recent research on omega-3s and women’s mental health, where the majority of studies indicate that EPA has efficacy in treating depression, and in moderate doses, EPA and DHA, appear safe for pregnant and postpartum women.56 The Kaludjerovic and Vieth article illustrates that inadequate vitamin D nutrition during perinatal development is a threat to human health and due to the risks of exposure to sunlight, provides current recommendations for vitamin D supplementation.57
DIET AND WEIGHT CONTROL
Almost any diet will result in weight loss, at least for a short time, if it helps the dieter take in fewer calories than she burns. Few dieters, however, are able to sustain weight-loss diets for long periods. Different palates, food preferences, family situations, and even genes mean that no single diet is right for everyone. What is needed is a dietary pattern that can be sustained for years, and that is as good for the heart, bones, brain, psyche, and taste buds as it is for the waistline. This diet should include plenty of choices and few restrictions or “special” foods. Data from randomized trials suggest that the nutrient makeup of a dietary pattern for weight loss matters far less than the number of calories it delivers.
In a head-to-head trial of four diets loosely based on the Atkins, Ornish, and Mediterranean diets (low fat, average protein; low fat, high protein; high fat, average protein; and high fat, high protein respectively), participants lost an average of 13.2 pounds (6 kg) at 6 months, and had a 2-inch reduction in waist size, regardless of the diets they were following. At 12 months, most began to regain some weight. Among those who completed the trial, the amount of weight loss after 2 years was similar in participants assigned to a diet with 25% protein and those assigned to a diet with 15% protein (average of 4.5 and 3.6 kg, respectively; P=0.11), and was also the same in those assigned to a diet with 40% fat and those assigned to a diet with 20% fat (average of 3.9 and 4.1 kg, respectively; P=0.76).58 There was no effect of carbohydrate level on weight loss within the target range of 35% to 65% of calories from carbohydrate. The change in waist circumference was also similar across the diet groups. Feelings of hunger, satiety, and satisfaction with the diet were the same across the board, as were cholesterol levels and other markers of cardiovascular risk. It is important to note that these averages hide huge variations in weight loss, with some participants losing 30 pounds or more while others actually gained weight during the trial. This supports the idea that weight-loss strategies must be individualized. Group counseling was an aid to weight loss, suggesting that behavioral, psychological, and social factors are probably more important for weight loss than the mix of nutrients in a diet.
CONCLUSIONS
Although much solid information on optimal diets has emerged, the full picture of the relationships between diet and health will take years of further research to fill in. Yet several fundamentals have been established and are unlikely to change significantly. These include the seven general strategies listed in Table 1.
It is impossible to cover all this ground in a 5-minute office visit. However, it is possible to make several general points, offer a handout, and direct a patient to more information. If a patient is overweight, the most important general points should be about portion control, avoiding sugary beverages, and exercise. Weight is probably at least as important for long-term health as are dietary components. For a patient whose weight is in the healthy range, reinforce that it is prudent to avoid trans and saturated fats and emphasize unsaturated fats, replace highly refined grains with whole grains, and choose healthful sources of protein. The Healthy Eating Pyramid (see Figure 2) offers a good visual reminder of these points and other essentials of healthful eating.
The seven strategies listed in Table 1 aren’t quite as pithy as food writer Michael Pollan’s extraordinary seven-word summary of healthy eating: Eat food. Not too much. Mostly plants.43 But they are more concrete, and provide a satisfactory answer to the question, “What is a healthy diet?”
Biography
Patrick J. Skerrett is editor of the Harvard Heart Letter. Walter C. Willett is the Fredrick John Stare Professor of Epidemiology and Nutrition and chair of the Department of Nutrition at Harvard School of Public Health. They are co-authors of Eat, Drink, and Be Healthy: The Harvard Medical School Guide to Healthy Eating and (with Jorge E. Chavarro, MD) The Fertility Diet.
Footnotes
Disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Heron MP, Hoyert DL, Murphy SL, Xu JQ, Kochanek KD, Tejada-Vera B. National vital statistics reports. Hyattsville, MD: National Center for Health Statistics; 2009. [Accessed 16 November 2009]. Deaths: Final data for 2006. Available from: http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_14.pdf. [PubMed] [Google Scholar]
- 2.Eyre H, Kahn R, Robertson RM. Preventing cancer, cardiovascular disease, and diabetes: a common agenda for the American Cancer Society, the American Diabetes Association, and the American Heart Association. Diabetes Care. 2004;27(7):1812–24. doi: 10.2337/diacare.27.7.1812. [DOI] [PubMed] [Google Scholar]
- 3.Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med. 2000;343(1):16–22. doi: 10.1056/NEJM200007063430103. [DOI] [PubMed] [Google Scholar]
- 4.Chiuve SE, McCullough ML, Sacks FM, Rimm EB. Healthy lifestyle factors in the primary prevention of coronary heart disease among men: benefits among users and nonusers of lipid-lowering and antihypertensive medications. Circulation. 2006;114(2):160–7. doi: 10.1161/CIRCULATIONAHA.106.621417. [DOI] [PubMed] [Google Scholar]
- 5.Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC. Trans fatty acids and cardiovascular disease. N Engl J Med. 2006;354(15):1601–13. doi: 10.1056/NEJMra054035. [DOI] [PubMed] [Google Scholar]
- 6.Riediger ND, Othman RA, Suh M, Moghadasian MH. A systemic review of the roles of n-3 fatty acids in health and disease. J Am Diet Assoc. 2009;109(4):668–79. doi: 10.1016/j.jada.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 7.de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99(6):779–85. doi: 10.1161/01.cir.99.6.779. [DOI] [PubMed] [Google Scholar]
- 8.USDA Center for Nutrition Policy and Promotion. Nutrition Insights: Is total fat consumption really decreasing? Beltsville, MD: USDA Center for Nutrition Policy and Promotion; 1998. [Accessed 16 November 2009]. Available from: http://www.cnpp.usda.gov/Publications/NutritionInsights/insight5.pdf. [Google Scholar]
- 9.Mensink RP, Katan MB. Effect of dietary fatty acids on serum lipids and lipoproteins: a meta-analysis of 27 trials. Arteriosclerosis and Thrombosis. 1992;12:911–9. doi: 10.1161/01.atv.12.8.911. [DOI] [PubMed] [Google Scholar]
- 10.Ludwig DS. Clinical update: the low-glycaemic-index diet. Lancet. 2007;369(9565):890–2. doi: 10.1016/S0140-6736(07)60427-9. [DOI] [PubMed] [Google Scholar]
- 11.Lann D, LeRoith D. Insulin resistance as the underlying cause for the metabolic syndrome. Med Clin North Am. 2007;91(6):1063–77. viii. doi: 10.1016/j.mcna.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 12.Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. A prospective study of dietary carbohydrate quantity and quality in relation to risk of ovulatory infertility. Eur J Clin Nutr. 2009;63(1):78–86. doi: 10.1038/sj.ejcn.1602904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schulze MB, Liu S, Rimm EB, Manson JE, Willett WC, Hu FB. Glycemic index, glycemic load, and dietary fiber intake and incidence of type 2 diabetes in younger and middle-aged women. Am J Clin Nutr. 2004;80(2):348–56. doi: 10.1093/ajcn/80.2.348. [DOI] [PubMed] [Google Scholar]
- 14.Mellen PB, Walsh TF, Herrington DM. Whole grain intake and cardiovascular disease: a meta-analysis. Nutr Metab Cardiovasc Dis. 2008;18(4):283–90. doi: 10.1016/j.numecd.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 15.Kastorini CM, Panagiotakos DB. Dietary patterns and prevention of type 2 diabetes: from research to clinical practice; a systematic review. Curr Diabetes Rev. 2009 doi: 10.2174/157339909789804341. [DOI] [PubMed] [Google Scholar]
- 16.Halton TL, Willett WC, Liu S, Manson JE, Albert CM, Rexrode K, et al. Low-carbohydrate-diet score and the risk of coronary heart disease in women. N Engl J Med. 2006;355(19):1991–2002. doi: 10.1056/NEJMoa055317. [DOI] [PubMed] [Google Scholar]
- 17.National Research Council (U.S.) Committee on Diet and Health. Diet and health : implications for reducing chronic disease risk. Washington, D.C: National Academy Press; 1989. [Accessed 16 November 2009]. Available from: http://www.nap.edu/catalog.php?record_id=1222#toc. [PubMed] [Google Scholar]
- 18.Vainio H, Bianchini F. Fruit and Vegetables - IARC Handbooks of Cancer Prevention. Vol. 8. Lyon, France: International Agency for Research on Cancer; 2005. [Google Scholar]
- 19.King DE, Mainous AG, 3rd, Carnemolla M, Everett CJ. Adherence to healthy lifestyle habits in US adults, 1988–2006. Am J Med. 2009;122(6):528–34. doi: 10.1016/j.amjmed.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 20.van Dieren S, Uiterwaal CS, van der Schouw YT, van der AD, Boer JM, Spijkerman A, et al. Coffee and tea consumption and risk of type 2 diabetes. Diabetologia. 2009 doi: 10.1007/s00125-009-1516-3. [DOI] [PubMed] [Google Scholar]
- 21.Boston, MA: Harvard School of Public Health Nutrition Source; 2009. [Accessed 10 September 2009]. How sweet is it? Available from: http://www.hsph.harvard.edu/nutritionsource/healthy-drinks/how-sweet-is-it/index.html. [Google Scholar]
- 22.Schulze MB, Manson JE, Ludwig DS, Colditz GA, Stampfer MJ, Willett WC, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA. 2004;292(8):927–34. doi: 10.1001/jama.292.8.927. [DOI] [PubMed] [Google Scholar]
- 23.Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2009;120(11):1011–20. doi: 10.1161/CIRCULATIONAHA.109.192627. [DOI] [PubMed] [Google Scholar]
- 24.Choi HK, Curhan G. Soft drinks, fructose consumption, and the risk of gout in men: prospective cohort study. BMJ. 2008;336(7639):309–12. doi: 10.1136/bmj.39449.819271.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang S, Hunter DJ, Hankinson SE, Giovannucci EL, Rosner BA, Colditz GA, et al. A prospective study of folate intake and the risk of breast cancer. JAMA. 1999;281:1632–7. doi: 10.1001/jama.281.17.1632. [DOI] [PubMed] [Google Scholar]
- 26.Looker AC, Dallman PR, Carroll MD, Gunter EW, Johnson CL. Prevalence of iron deficiency in the United States. JAMA. 1997;277(12):973–6. doi: 10.1001/jama.1997.03540360041028. [DOI] [PubMed] [Google Scholar]
- 27.MRC Vitamin Study Research Group. Prevention of neural tube defects: results of the Medical Research Council Vitamin Study. Lancet. 1991;338(8760):131–7. [PubMed] [Google Scholar]
- 28.Institute of Medicine. Dietary reference intakes: calcium, phosphorous, magnesium, vitamin D, and fluoride. National Academy Press; 1997. [Accessed 16 November 2009]. Available from: http://books.nap.edu/books/0309063507/html/index.html. [Google Scholar]
- 29.U.S. Department of Health and Human Services and U.S. Department of Agriculture. Dietary guidelines for Americans 2005. Washington, DC: U.S. Department of Agriculture; 2005. [Accessed 15 September]. Available from: http://www.healthierus.gov/dietaryguidelines/ [Google Scholar]
- 30.Stechschulte SA, Kirsner RS, Federman DG. Vitamin D: bone and beyond, rationale and recommendations for supplementation. Am J Med. 2009;122(9):793–802. doi: 10.1016/j.amjmed.2009.02.029. [DOI] [PubMed] [Google Scholar]
- 31.Feskanich D, Singh V, Willett WC, Colditz GA. Vitamin A intake and hip fractures among postmenopausal women. JAMA. 2002;287(1):47–54. doi: 10.1001/jama.287.1.47. [DOI] [PubMed] [Google Scholar]
- 32.Iqbal R, Anand S, Ounpuu S, Islam S, Zhang X, Rangarajan S, et al. Dietary patterns and the risk of acute myocardial infarction in 52 countries: results of the INTERHEART study. Circulation. 2008;118(19):1929–37. doi: 10.1161/CIRCULATIONAHA.107.738716. [DOI] [PubMed] [Google Scholar]
- 33.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169(7):659–69. doi: 10.1001/archinternmed.2009.38. [DOI] [PubMed] [Google Scholar]
- 34.Mitrou PN, Kipnis V, Thiebaut AC, Reedy J, Subar AF, Wirfalt E, et al. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: results from the NIH-AARP Diet and Health Study. Arch Intern Med. 2007;167(22):2461–8. doi: 10.1001/archinte.167.22.2461. [DOI] [PubMed] [Google Scholar]
- 35.Sofi F, Cesari F, Abbate R, Gensini GF, Casini A. Adherence to Mediterranean diet and health status: meta-analysis. BMJ. 2008;337:a1344. doi: 10.1136/bmj.a1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barros R, Moreira A, Fonseca J, de Oliveira JF, Delgado L, Castel-Branco MG, et al. Adherence to the Mediterranean diet and fresh fruit intake are associated with improved asthma control. Allergy. 2008;63(7):917–23. doi: 10.1111/j.1398-9995.2008.01665.x. [DOI] [PubMed] [Google Scholar]
- 37.Skoldstam L, Hagfors L, Johansson G. An experimental study of a Mediterranean diet intervention for patients with rheumatoid arthritis. Ann Rheum Dis. 2003;62(3):208–14. doi: 10.1136/ard.62.3.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–24. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 39.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344(1):3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 40.Moore TJ, Alsabeeh N, Apovian CM, Murphy MC, Coffman GA, Cullum-Dugan D, et al. Weight, blood pressure, and dietary benefits after 12 months of a Web-based Nutrition Education Program (DASH for health): longitudinal observational study. J Med Internet Res. 2008;10(4):e52. doi: 10.2196/jmir.1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168(7):713–20. doi: 10.1001/archinte.168.7.713. [DOI] [PubMed] [Google Scholar]
- 42.Taylor EN, Fung TT, Curhan GC. DASH-Style Diet Associates with Reduced Risk for Kidney Stones. J Am Soc Nephrol. 2009 doi: 10.1681/ASN.2009030276. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER, 3rd, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA. 2005;294(19):2455–64. doi: 10.1001/jama.294.19.2455. [DOI] [PubMed] [Google Scholar]
- 44.Jenkins DJ, Kendall CW, Faulkner D, Vidgen E, Trautwein EA, Parker TL, et al. A dietary portfolio approach to cholesterol reduction: combined effects of plant sterols, vegetable proteins, and viscous fibers in hypercholesterolemia. Metabolism. 2002;51(12):1596–604. doi: 10.1053/meta.2002.35578. [DOI] [PubMed] [Google Scholar]
- 45.Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of US women: data from the 2002 National Survey of Family Growth. Bethesda, MD: National Center for Health Statistics; 2005. [Accessed 10 September 2009]. Available from: http://www.cdc.gov/nchs/data/series/sr_23/sr23_025.pdf. [PubMed] [Google Scholar]
- 46.Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Iron intake and risk of ovulatory infertility. Obstet Gynecol. 2006;108(5):1145–52. doi: 10.1097/01.AOG.0000238333.37423.ab. [DOI] [PubMed] [Google Scholar]
- 47.Chavarro JE, Rich-Edwards JW, Rosner B, Willett WC. A prospective study of dairy foods intake and anovulatory infertility. Hum Reprod. 2007;22(5):1340–7. doi: 10.1093/humrep/dem019. [DOI] [PubMed] [Google Scholar]
- 48.Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Dietary fatty acid intakes and the risk of ovulatory infertility. Am J Clin Nutr. 2007;85(1):231–7. doi: 10.1093/ajcn/85.1.231. [DOI] [PubMed] [Google Scholar]
- 49.Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Diet and lifestyle in the prevention of ovulatory disorder infertility. Obstet Gynecol. 2007;110(5):1050–8. doi: 10.1097/01.AOG.0000287293.25465.e1. [DOI] [PubMed] [Google Scholar]
- 50.Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Protein intake and ovulatory infertility. Am J Obstet Gynecol. 2008;198(2):210 e1–7. doi: 10.1016/j.ajog.2007.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Use of multivitamins, intake of B vitamins, and risk of ovulatory infertility. Fertil Steril. 2008;89(3):668–76. doi: 10.1016/j.fertnstert.2007.03.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Caffeinated and alcoholic beverage intake in relation to ovulatory disorder infertility. Epidemiology. 2009;20(3):374–81. doi: 10.1097/EDE.0b013e31819d68cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chavarro JE, Willett WC, Skerrett PJ. The Fertility Diet: groundbreaking research reveals natural ways to boost ovulation & improve your chances of getting pregnant. New York: McGraw-Hill; 2008. [Google Scholar]
- 54.What You Need to Know About Mercury in Fish and Shellfish. Washington, DC: Food and Drug Administration, Environmental Protection Agency; 2004. [Accessed 14 September]. Available from: http://www.epa.gov/fishadvisories/advice/ [Google Scholar]
- 55.Robin Jordan article (in this issue 55.6)
- 56.Kendall-Tackett (in this issue 55.6)
- 57.Kaludjerovic article
- 58.Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360(9):859–73. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]