Abstract
Objectives: Limited human resources are widely recognised as a barrier to achieve health-related Millennium Development Goals. Availability of medical supplies and suitably trained health personnel are crucial to ensuring a well-functioning medical supply system. The objective of this paper is to identify the factors which influence the availability of medical supplies within the health facilities of Vanuatu.
Methods: A qualitative triangulated strategy using semi-structured interviews, observational workplace surveys and semi-structured focus groups was developed. This research was approved by the Human Ethics Committee of the University of Canberra and was funded through a direct grant from the United Nations Population Fund Suva, Pacific sub regional office.
Results: During two weeks of data collection, 21 interviews were conducted, observational workplace surveys were completed in 19 facilities and 22 personnel participated in three focus groups across three provinces. The interviewees had a wide range of primary professional groupings and were representative of the Vanuatu health workforce. A complex array of medical supply issues are described from within the three tiered structure of the medical supply system.
Conclusion: The results of this research have further informed our understanding of the competencies required by healthcare personnel to conduct medical supply management activities effectively in Pacific Island countries. As a result of this research, a platform is provided for the government of Vanuatu to engage development partners to work toward a sustainable medical supply system.
Keywords: Essential medicines supply, medical supply, interview, pharmacy, surveys, Vanuatu
Introduction
The Pacific regional context
Limited human resources are widely recognised as an impediment to achieving the health-related Millennium Development Goals (MDGs). Many maternal and child deaths may be prevented by having ready access to essential medical supplies provided by appropriately trained health personnel (where medical supplies include medicines and medical sundries e.g. syringes and dressings) [1]. Millennium Development Goals 4, 5, 6 and 8 explicitly involve the availability of medical supplies at the primary care level - the absence of these supplies is a significant barrier [2] to meeting these goals (Table 1).
The availability of medical supplies and suitable personnel in adequate numbers with appropriate competency is crucial to ensure a well-functioning medical supply system [3]. In many countries pharmacists perform this role; however on average across Pacific Island countries (PICs) there is less than 1 pharmacist per 10,000 population [4]. This ratio is similar to sub-Saharan African countries [3]. Some PICs have no pharmacists at all. In this environment the medical supply system is often operated by pharmacy support staff such as assistants, technicians and dispensers with a wide variance in the formal training they receive for this role [3, 4].
The majority of the population in PICs resides in rural areas which are serviced by primary healthcare facilities such as clinics and aid posts [1,4]. These facilities commonly do not employ pharmacy staff and medical supply activities are conducted by healthcare personnel such as nurses or midwives who may have little or no formal training in this medical supply role.
The International Pharmaceutical Federation (FIP) acknowledge that insufficient numbers and inadequate competency of pharmacy personnel is a contributor to continued problems in maintaining reliable medical supplies systems; an observation supported by the World Health Organisation (WHO), Australian Agency for International Development (AusAID) and other agencies active in PICs [1,5,6].
Strengthening the pharmaceutical sector has been a long-term political priority for PICs. This priority has arisen from recommendations from the meetings of Ministers and Directors of Health for PICs held since 1995 [7]. The United Nations Population Fund (UNFPA) and the University of Canberra (UC) are contributing to this process by investigating the competencies required by personnel to operate medical supply systems, and by developing appropriate and sustainable approaches to health personnel competency development. Aligned with the UNFPA mandate, reproductive health commodities (RHCs) are employed as tracer items in the investigation of country medical supply systems and the competencies required by personnel who work in them.
Table 1. The explicit relationship between the Millennium Development Goals (MDGs) and the medical supply system.
| MDG 4. Reduce child mortality | Pneumonia, diarrhea, malaria and AIDS account for 43 per cent of all deaths in under-fives with most of these lives saved through low-cost prevention and treatment measures including antibiotics for acute respiratory infections, oral rehydration for diarrhea, and immunization [2]. |
| MDG 5. Improve maternal health | More than 80 per cent of maternal deaths are caused by conditions such as hemorrhage, sepsis, and hypertensive diseases of pregnancy, each requiring medication and the use of medical sundries. It is estimated that meeting the unmet needs for contraception alone could cut, by almost a third, the number of maternal deaths [2]. |
| MDG 6. Combat HIV/AIDS, malaria, and other diseases | Each disease has medication as part of the treatment protocol. |
| MDG 8. Develop a global partnership for development | In cooperation with pharmaceutical companies, provide access to affordable essential medicines in developing countries. |
United Nations (UN).The Millennium Development Goals Report United Nations. 2010. URL: http://www.un.org/millenniumgoals/pdf/MDG_20Report_202010_20En_20r15_20-low_20res_2020100615_20-.pdf Accessed 4th February 2012.
Vanuatu country context and the Vanuatu medical supply system
Vanuatu is a Y-shaped archipelago in the South West Pacific Ocean consisting of about eighty islands, extending approximately 1176 kilometers from north to south and covering a land area of 12,336 square kilometers. The country is divided into six provinces, namely Shefa, Sanma, Malampa, Tafea, Penama and Torba. The vast majority of the 240,000 population are Melanesians (ni-Vanuatu), with Europeans being the other major ethnic group [8].
The leading causes of morbidity include; acute respiratory infection, cutaneous abscess, malaria, asthma, diarrhoea, injuries, food poisoning, diabetes, chronic obstructive pulmonary disease and hypertension, while the leading causes of mortality include; heart disease, cancer, asthma, stroke, pneumonia, liver diseases, neonatal death, diabetes mellitus, septicaemia, and hypertension [9].
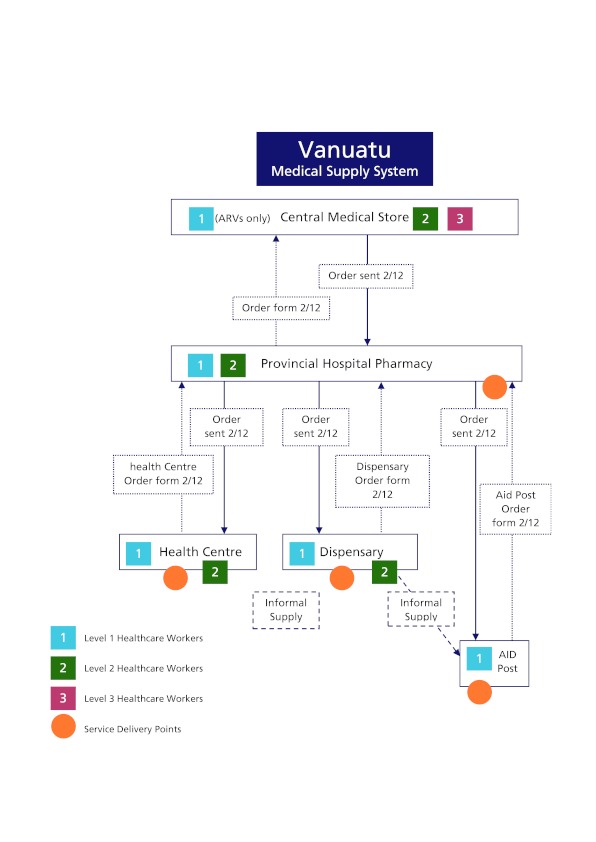
Vanuatu is geographically widespread creating challenges for medical supply distribution and communication, especially to remote areas. The Ministry of Health (MoH) is responsible for the national distribution of medical supplies to the four levels of health facilities (hospital, health centre, dispensary, and aid post) throughout Vanuatu using a national distribution system involving the Central Medical Store (CMS) in Port Vila and the Division of Pharmacy [10] (Figure 1).
The MoH is responsible for all aspects of the operation of hospitals, health centers and dispensaries, while the community, local government or faith based organisations are responsible for the provision and support of personnel for aid posts. The MoH provides training, medicines and basic medical supplies for aid posts [10].
There are currently five hospitals in Vanuatu, with a sixth hospital proposed for Torba. Two of these hospitals, Vila Central Hospital and Northern District Hospital, are major referral centres while the other three hospitals (Lenakel (Tafea), Norsup (Malampar) and Lolowai (Penama) are classified as provincial hospitals and provide referral services from local health centres and dispensaries [10]. Hospital pharmacies receive medical supplies from CMS and distribute them to dependent health centres, dispensaries and aid posts. They also provide inpatient ward services by imprest systems and outpatient dispensing services.
In 2004 there were 27 active health centres providing outpatient and inpatient services, including acute care such as care during labour and delivery, health promotion and preventive health services such as immunization. Health centres are usually staffed by a nurse practitioner who also acts as manager, a midwife and general nurse [10]. Health centres act as referral centres for dispensaries and aid posts, although urgent referrals may go directly from dispensary or aid post to hospital. In 2004 there were 74 active dispensaries, with at least one dispensary on most inhabited islands. Dispensaries provide outpatient services with a focus on basic essential health care including health promotion and preventive services [10]. Dispensaries refer complicated cases, or those requiring admission to a health centre or hospital. Dispensaries are usually staffed by a general nurse. Dispensary staff are responsible for supervising aid posts in their area. In 2004 there were about 180 aid posts, with an aid post in most villages. Aid posts are established and funded by the community in which they are based, the local or provincial government, or faith based organizations [10]. Aid posts are staffed by Village Health Volunteers (VHVs) providing first aid and community education.
Figure 1.
Objectives
The aim of this study was to determine the factors which influence the availability of medical supplies within the health facilities of Vanuatu. A further objective was to document the medical supply activities undertaken within the various levels of the Vanuatu medical supply system.
Methods
To answer the research question a qualitative triangulated strategy using semi-structured interviews, observational workplace surveys and semi-structured focus groups was developed. This research was approved by the Human Ethics Committee of the University of Canberra (project number 10-85), and was funded through a direct grant from the United Nations Population Fund Suva, Pacific sub regional office.
The interview tool used was developed using existing World Health Organisation (WHO) medicines supply indicator survey concepts and informed by the Medication Safety Self Assessment for Australian Hospitals; applied to the context of Vanuatu [11, 12]. A separate observational workplace survey tool was developed using the same process and designed to complement the interview tool through the use of direct workplace observation. Both tools were validated in a preliminary trial involving Vanuatu pharmacy staff, with a focus on appropriate format, language and cultural considerations.To complete the triangulation of data, a semi-structured focus group format was developed using key elements of the‘World Café’ methodology [13].This approach to ‘focus group’ facilitation had previously been used by the authors (in unpublished consultancy activities),to reduce hierarchical sensitivities in mixed cadre environments,and is seen to be successful in empowering individuals to contribute as well as encouraging them to consider the opinions of others in a relaxed environment [13].
The interviews were designed to reveal the thoughts and practices of individuals while the workplace survey allowed the investigators to cross-check the interview findings with the practice situation observed in the health facilities.Site visits were undertaken in conjunction with Ministry of Health and local UNFPA counterparts to provide a vertical picture of the various levels of the medical supply system through a cluster based approach. Three provinces were visited to represent both urban and rural environments, due consideration was given to varied geography, and to be accessible by the research team over a two week data collection period.Within each province clusters of service delivery points were selected to include examples of hospitals, health centers, dispensaries and aid posts. Data was collected anonymously, then pooled and organised using the web based survey application ‘Survey Monkey’. Thematic analysis was conducted using a team based consultative approach where recurring issues were prioritised and cross referenced for validity across the three data collection methods.
Results
During two weeks of data collection (18-31st July 2010) 21 interviews were conducted, observational workplace surveys were completed in 19 facilities and 22 health personnel participated in three focus groups across the three provinces. The main themes identified in this research are presented under headings of the three tiered structure of the medical supply system.
Participant and clinic demographics
The interviewees represented a wide range of primary professional groupings, with nursing being the most common (62%). This included registered nurses (RNs) and nurse practitioners. Those who classified themselves as pharmacy staff included storemen, dispensers, assistant pharmacists and intern pharmacists. Six of the 21 interviewees worked in urban locations, with the remaining 15 working in rural locations. Interviewees had worked at their current facility an average of 8 years (range 1-20yrs). The average time that interviewees had worked in their current health professional capacity was 13 years (range 1-35 years). This wide range of experiences and work histories provides a robust representative view of the issues around medical supply in Vanuatu.
Healthcare personnel retention was cited regularly as a challenge to maintain best practices around medical supply management, with staff who receive training then moving to other facilities thus losing medical supply management capacity in that facility. The healthcare personnel interviewed represented the three tiers of the medical supply system, representing service delivery to 100% of the Vanuatu population at the national level through the Central Medical Store (CMS), 68-100% at the provincial level through the three main hospitals and approximately 20% of the population through other primary care service delivery points. This provides a representative picture of the issues around medical supply in Vanuatu, in particular at the main distribution points. The 21 interviewees worked at 19 different health facilities: 1 x CMS, 3 x hospitals, 11 x health centers, 2 x dispensaries and 2 x aid posts.
Central Medical Store (CMS) – Main thematic issues
The absence of a principal pharmacist and staff to fill two other currently vacant supporting posts in CMS (at the time of the study), was placing considerable strain on existing staff, reducing their capacity to undertake regular stock management activities such as: regular stocktaking, future planning, quality assurance and yearly activity plans. The routine completion of standard operating procedures (SOPs) is also affected e.g. absence of packing slips when stock is sent to provincial hospitals. Current space in CMS was observed to be limited and is cited by staff as an impediment to efficient stock layout and movement, including inventory control activities.The recent loss of electronic order history data will impair the ability of CMS to plan for future requirements based on past ordering. Medical supplies data was previously collected using the computer based ‘Mind Your Own Business’ (MYOB) accounting package, but is now in the process of being replaced by the ‘mSupply’ computer based, medical supply management system.
The National Drugs and Therapeutics Committee was not active, removing the ability of inclusive country level decision making, which has resulted in country wide issues relating to medication selection and wastage.Default quantities ordered using the existing order forms have been observed to lead to wastage, as they are not responsive to the differing scales of service delivery points. The majority of oral medications are currently supplied in bulk containers of 1000 doses. National order forms for aid posts, dispensaries and health centres were highlighted for review by key interviewees during the survey, as they were considered to be outdated and could be better designed to encourage best practice by personnel throughout the supply chain.
Provincial hospital pharmacies – Main thematic issues
There is strong evidence of a good theoretical knowledge of medical supply management procedures amongst hospital pharmacy staff; however there is evidence that this knowledge is not routinely applied. This causes the problems with under and over supply of medical supplies. Notable examples include the absence of routine stock management activities such as unpacking and shelving of supplies received in bulk cartons. Also, many foreign medical staff travel to Vanuatu hospitals to provide clinical services for short term appointments. Interviewees gave several examples where these workers did not follow local procedures concerning medical supply or the Essential Medicines List (EML), leading to uncertainty or conflict with pharmacy staff.
Hospital pharmacies keep copies of all prescriptions dispensed and collate daily statistics around patient numbers. They also keep computerised records of stock received and distributed to dependent facilities along with hard copies of order forms received from all dependent facilities. This data was not routinely used by interviewees to inform the ordering process.
Supervisory visits are identified by pharmacy and provincial health personnel as a key activity to support pharmacy’s role but the absence of a specific budget line for this purpose has limited their completion. The majority of supervisory visits occur on an ad-hoc basis when specific project funds for transport are available.
Interviewees indicated that patient counseling is considered an area with potential for greater input by pharmacy staff with the areas of dosage instructions (how much, how often, how long), relationship to food and any important expected adverse effects being identified as core areas that needed improvement. Non communicable diseases (NCDs) are seen to contribute significantly and increasingly to the burden of disease in Vanuatu; however they do not form a large part of the conditions managed by rural facilities. Most health centres and dispensaries visited had only a small number of patients receiving medication regularly for NCDs despite health statistics indicating that their prevalence is significant.
Health centres, dispensaries, aid posts - Main thematic issues
Provincial governments are responsible for the cost of the distribution of medical supplies from the provincial centre to primary health care facilities;however it was observed that this is not regularly funded by provincial governments, with individual facilities paying these costs.
Many facilities require four wheel drive vehicles to deliver medical supplies which can quickly become inaccessible after rain, which is frequent. Large rivers and the absence of roads also reduce access with many facilities only accessible via boat. Delivery of medical supplies to some villages in the interior requires personnel to walk for several days return, carrying large cartons of medical supplies. These journeys are often assisted by villagers but provide challenges to efficient and reliable supply, especially for temperature sensitive medications or large/heavy items. These issues are amplified in the outer islands by infrequent transport and limited communication access.
Some interviewees reported attending up to nine or more work related week-long refresher workshops in provincial centres over a twelve month period. This heavy training schedule has significant consequences for service delivery; some facilities with a solo worker are closed during these training activities which can account for approximately 20% of the time they are expected to be open.All facilities visited kept an outpatient register detailing the name, diagnosis and treatment for each patient. These registers provide a detailed chronological record of the activities of the facility. The use of outpatient register was observed to be rigorous and considered important by personnel. This contrasts with other record keeping activities which were not observed to be completed, especially around medical supply management, and provides a useful model for instituting good record keeping practices.
There is evidence of good theoretical knowledge of supply management procedures amongst staff in these facilities however many of these procedures are not routinely completed or able to be applied in practice, leading to medical supply problems. Common issues include irregular making of orders and inaccurate estimates of requirements based on instinct. Records of previous orders are not routinely kept (despite procedures requiring a copy to be made and kept) hence there is no capacity for analysis of previous usage to inform ordering.Many interviewees agreed that they did not always complete required supply management activities because there was no one directly supervising them to do so. Infrequent visits from Central medical store staff or provincial hospital pharmacy staff did not provide the incentive to regularly do these activities, even though their value was recognised. A similar issue is the hesitance of personnel to make improvements to medical supply procedures even though they “...know it’s not the best but it’s always been done this way...”. This appears to be due to personnel requiring, or feeling the need for permission to undertake changes or simply being overwhelmed by the task. Several examples were observed where personnel were unable to organise the cleaning of facilities and organisation of stock as the situation had become ‘overwhelming’ with no apparent starting point.
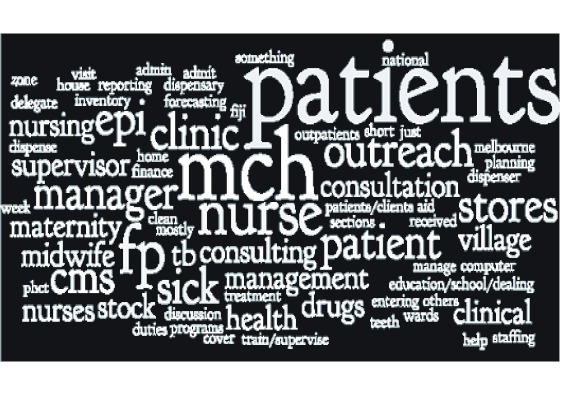
The regular order cycle for these facilities is bimonthly, with the capacity for emergency top-up orders in exceptional circumstances. A commonly observed contributor to excess stock is the reliance on emergency orders, sometimes to the exclusion of regular orders. This was especially true for those facilities within a day’s drive from provincial hospitals. The issue of the lack of importance of medical supplies was brought forward by personnel. Emphasising this point is the ‘word cloud’ created using responses regarding the day to day responsibilities of healthcare personnel, with the most commonly reported responsibilities appearing in the largest font size [Figure 2].
A conditions checklist was completed for each of the facilities to determine if there were adequate conservation conditions and handling of medicines in the storeroom and dispensing area. Generally storerooms have adequate conservation and handling conditions, with the exception of recording of refrigerator temperatures and use of stock rotation. It was found that the dispensing areas were more problematic, with many instances of inadequate conditions. Temperature and light control, stock layout and pest control are all areas where many facilities require improvement. Unique environmental circumstances such as large amounts of volcanic dust (the island of Tanna provides the best example), are challenges that healthcare personnel face in maintaining suitable environments for medicines storage.
Figure 2. Day to day responsibilities of healthcare personnel.
Discussion
Sustainable health systems strengthening
Potter and Brough provide a systematic approach to achieving sustainable health systems including medicines supply, describing the interrelationship between tools, skills, staff and infrastructure, and structures systems and roles in the wider health system [14].Our results can be categorized using the Potter and Brough model [14] (Table 2).
The documented results of our research show some interrelationship between the four categories. ‘Tools’ require ‘Skills’ which require ‘Staff and Infrastructure’, which in turn require ‘Structures Systems and Roles’. Conversely ‘Structures Systems and Roles’ enable an effective use of ‘Staff and Infrastructure’ which enable the use of ‘Skills’ which in turn enable an effective use of ‘Tools’. This is supported by the observations of Potter and Brough [14].
The results of our research provide the start of a systematic approach to strengthening the medical supply system in Vanuatu. A systematic method for improvement is support by recent WHO approaches and involves consideration of the impact of observations before improvements can be made effectively [15,16]. Part of applying this approach is to understand the implication of our findings at the three levels of the health system, and how these may affect each other.
Table 2. Vanuatu medicines supply issues mapped against the Potter and Brough health system categories.
| Potter and Brough health systems category | Specific Medicine supply issues revealed from the Vanuatu research |
| Tools |
|
| Skills |
|
| Staff and Infrastructure |
|
| Structures Systems and Roles |
|
Brough R, Potter C. Systemic capacity building: a hierarchy of needs. Health Policy Plan 2004: 19 (5): 336-345. http://heapol.oxfordjournals.org/content/19/5/336.full.pdf+html
Central Medical Store (CMS)
As the national agency for medical supplies, CMS takes the leading role in forecasting, procuring, receiving, storing and distributing medical supplies for Vanuatu. CMS establishes the procedures to be followed in medical supply management for the country and any improvement in accessibility of essential medicines needs to be based upon the capacity of the facilities, staff and procedures of CMS.With this central role in mind, the absence of a principal pharmacist and senior staff means that the overseeing and leadership role required for national organisation of medical supply is missing. This is a contributing factor to all the other medical supply issues described.The absence of an active National Drugs and Therapeutics Committee impairs the ability of CMS to respond to changing prescribing patterns at a national level and reduces the possibility of multi-stakeholder engagement. The collective engagement of medical, nursing, finance and administrative staff on issues of medication selection, distribution and use may encourage greater ownership of the medical supply system, in turn providing greater support for the system across the country [18].
Provincial hospital pharmacies
These provincial hubs are the gateway for the effective supply of the primary health care facilities. The ‘know do’ gap between a working knowledge of the systems and procedures of the medicines supply system and the enacting of them is a significant issue disrupting effective supply to the primary health care facilities of the provinces. Of these procedures the ability to effectively and appropriately ‘screen’ orders submitted by primary health care facilities is the most significant. Arbitrary reductions in stock issues and a lack of understanding of what is happening on the ground at the facility level have direct implications for patients.
The lack of funds which could enable the regular transport of orders from the provincial centre to primary health care facilities and an absence of funds for regular supervisory visits are issues across PICs. With 80% of the population residing in rural areas these two issues are perhaps the greatest impediment to the effective delivery of medications to primary care facilities [1,4].The disparity between the reported national non communicable disease burden (which is increasing) and the low amounts of medicines being used at the primary health care level is of specific concern [9]. This may be because of a significant misalignment with the process for the supply of NCD medications requiring patients to return to hospitals for ongoing supply, or the process may create such an impediment to their supply that patients discontinue treatment (NCD medication in Vanuatu may only be initially prescribed by a doctor but ongoing supply can be arranged through health centres and dispensaries by nursing staff).
Health centres, dispensaries, aid posts
A lack of stock cards and adequate storage appear to be two of the most significant resource based issues at this level of the system, while the absence of regular supervisory visits reduces the likelihood of systems being followed. This may leave some heathcare personnel feeling isolated [19]. One interviewee replied candidly that they “don’t count stock regularly” even though they know they should. Another interviewee was concerned that they themselves were “too lazy” to undertake these activities regularly.
The health personnel who staff these facilities are the backbone of health service delivery. With usually only one or two staff members at each facility the workload and responsibilities around the implementation of health programs (e.g. extended program on immunisation, malaria, maternal and child health, tuberculosis, family planning) is such that medical supply management is considered one of the lowest priorities.
Appreciation of the appropriate care and respect for medical supplies is not widespread and potentially reflects a lack of understanding of its importance to the successful delivery of healthcare services.
The ‘know do’ gap was also evident in these facilities with participants showing a good working knowledge of many of the procedures required for medical supply management but choosing not to follow those procedures day to day. The exception in our observations was the two step ‘ordering calculation’ where we were unable to see any evidence of appropriate understanding or its use. This had been replaced by estimating or ‘guessing’ as the preferred method of determining orders.
Next Steps in the Pacific
Sustainable health systems’ strengthening is difficult, especially in resource constrained environments. The WHO points to six interrelated ‘building blocks’ that form the foundation of a framework for sustainable health systems: service delivery, health workforce, information, medical products, vaccines and technologies, financing, and leadership and governance which could be useful to streamline this agenda[15,16].These ‘building blocks’ clearly identify what is essential within the health system. The blocks cannot be considered in isolation, as the six ‘building blocks’ are interrelated and require a systematic governmental response for sustainable whole of health systems strengthening to occur [16].
Our research findings reveal issues in each of the WHO building block areas which points to the need of a “whole of system approach” if the medical supply system of Vanuatu is to be improved.The UNFPA - UC research team is using this research to engage governments, pharmacists, doctors, nurses, pharmacy assistants and other pharmacy support workforce cadres to seek a combined solution to identified medical supply competency deficiencies in PICs.
The results of this research have further informed our understanding of the competencies required by healthcare personnel to conduct medical supply management activities effectively in PICs. It is our endeavor to further explore these competencies and to develop training approaches that will meet local requirements for competency development so that further progress toward reaching the MDGs can be maintained.
Study limitations
Both time and funding influenced the final number and location of health facilities visited as described in our methodology. The authors did not experience ‘first hand’ the supply issues facing more remote facilities and declare that this may be a limitation to the results revealed in this research. However, there was significant discussion of remote supply issues during the research from a wide range of interviewees and within the focus groups which partly addresses this gap.
Conclusions
It is clear from this research that the factors influencing the availability of medical supplies, within the health facilities of Vanuatu, consist of a range of interrelating issues that can be classified under: ‘tools’; ‘skills’; ‘workers and infrastructure’; and ‘structures, systems and roles’. These issues consist of both simple and complex problems involving the three levels of the medical supply chain operating within Vanuatu. Health systems sustainability theory suggests that a coordinated approach lead by the government of Vanuatu with invited development partners will be required for sustainable health systems change to occur.
Authors’ contributions
AB was responsible for the original concept and design of the manuscript. AB and BG were involved in the data collection and analysis. AB and BG were involved in the drafting, revising and final approval of the manuscript.
Conflict of interest
The authors report no conflict of interest.
Acknowledgments
The authors would also like to thank the Ministry of Health officials and health personnel from within the Republic of Vanuatu who gave of their time to participate in the site visits, focus groupsand surveys used to validate our work.
Funding Statement
The authors would like to acknowledge the funding provided by the United Nations Population Fund (UNFPA) Suva, Pacific sub regional office, for the data collection required in this research.
References
- 1.Regional Strategy on Human Resources for Health 2006-2015. Manila: World Health Organization (WHO); http://www.wpro.who.int/publications/PUB_978+92+9061+2445.htm. [Google Scholar]
- 2.The Millennium Development Goals Report United Nations. http://www.un.org/millenniumgoals/pdf/MDG_20Report_202010_20En_20r15_20-low_20 res_2020100615_20-.pdf.
- 3.FIP Global Pharmacy Workforce Report. International Pharmaceutical Federation (FIP); 2009. http://www.hrhresourcecenter.org/node/2801. [Google Scholar]
- 4.Brown A. A Systematic Review of the Literature Addressing Competencies, Training and Workforce Requirements for any Health Care Worker in Pacific Island Countries Involved in Essential Medicines Supply Management. Report to the Pharmaceuticals Programme, Western Pacific Regional Office, World Health Organization. 2009.
- 5.Hawthorne N, Anderson C. The Global Pharmacy Workforce: a systematic review of the literature. Human Resources for Health. 2009;7:48–7. doi: 10.1186/1478-4491-7-48. http://www.human-resources-health.com/content/7/1/48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Annual Thematic Performance Report: Health 2008-09. AusAID; 2009. http://www.ausaid.gov.au/publications/pubout.cfm?ID=2895_6386_5758_723_290&Type= [Google Scholar]
- 7.WHO-WIPRO Meeting of Ministers of Health of the Pacific Island Countries, Overview . http://www2.wpro.who.int/southpacific/sites/pi/pic/
- 8.Vanuatu MDG Assessment Summary. UNDP; 2010. http://www.undp.org.fj/pdf/VANUATU_20MDG_20ASSSESSMENT_20SUMMARY.pdf. [Google Scholar]
- 9.CHIPS for Vanuatu. WHO; 2012. http://www.wpro.who.int/countries/2010/van/ [Google Scholar]
- 10.Ministry of Health Master Health Services Plan 2004-2009. Vanuatu MoH; 2004. http://www.wpro.who.int/NR/rdonlyres/F762FF40-F2D9-49FD-B4F7-7B4E2B1CD27A/0/VanuatuHealthMasterPlan_LIGHTVERSION.pdf. [Google Scholar]
- 11.WHO Operational Packages for Assessing, Monitoring and Evaluating Country Pharmaceutical situations, Guide for Coordinators and Data Collectors. WHO; 2007. http://www.who.int/medicines/publications/WHO_TCM_2007.2/en/index.html. [Google Scholar]
- 12.Medication Safety Self Assessment for Australian Hospitals . https://mssa.cec.health.nsw.gov.au/download_MSSA.html.
- 13.World Café. http://www.theworldcafe.com/
- 14.Potter Christopher, Brough Richard. Systemic capacity building: a hierarchy of needs. Health Policy Plan. 2004;19(5):336–45. doi: 10.1093/heapol/czh038. http://heapol.oxfordjournals.org/content/19/5/336.full.pdf+html. [DOI] [PubMed] [Google Scholar]
- 15.Systems Thinking for Health Systems Strengthening. Geneva: WHO; 2009. http://www.who.int/alliance-hpsr/systemsthinking/en/index.html. [Google Scholar]
- 16.Strengthening Health Systems to Improve Health Outcomes, Everybody’s Business. Geneva: 2007. http://www.who.int/healthsystems/strategy/everybodys_business.pdf. [Google Scholar]
- 17.Drugs and Therapeutic Committees. Practical Guide. WHO; 2003. http://apps.who.int/medicinedocs/pdf/s4882e/s4882e.pdf. [Google Scholar]
- 18.Increasing accessto health workers inremote and rural areasthrough improved Retention. Global Policy Recommendations. WHO; 2010. http://whqlibdoc.who.int/publications/2010/9789241564014_eng.pdf. [PubMed] [Google Scholar]