Abstract
Background
Medication use among Medicare beneficiaries has increased and adherence has improved since the implementation of the Medicare Part D prescription drug benefit in 2006. However, the structure of the benefit, particularly, the coverage gap, is still problematic. It is critical to understand how beneficiaries with coexisting conditions respond to the coverage gap and whether their response differs by type of medications.
Aims of the Study
The paper aims to evaluate the effects of Medicare Part D’s coverage gap on drug regimens among beneficiaries with coexisting depression and heart failure (HF).
Methods
Drug utilization patterns of a 5% random sample of Medicare Part D beneficiaries with depression and HF in 2007 were observed. We compared drug use pattern pre and post coverage gap among three groups: no coverage, generic coverage, and full coverage due to low-income subsidies (LIS) and used propensity score weighting to adjust for difference across groups.
Results
Beneficiaries with some drug coverage in the gap were more likely to enter the gap: 82% for LIS, 79% for generic-only and 58% for no coverage. Beneficiaries without drug coverage reduced their use of antidepressants by 5.0% (95% CI 1.7%-8.2%), and HF drugs by 9.4% (95% CI 7.2%-11.5%) after they entered the coverage gap. Those with generic coverage cut their brand-name drugs more than generic drugs but did not shift to generic drugs. However, adherence to antidepressants did not change; adherence to HF drugs reduced slightly, 2.5% (95% CI 1.2%-3.7%) in the no-coverage group and 2.6% (95% CI 1.3%-3.9%) in the generic-coverage group.
Conclusions
The coverage gap was associated with a modest reduction in number of prescriptions filled for depression and HF but it was not associated with a significant effect on adherence.
Implications for Health Policy
We found that beneficiaries with coexisting depression and HF were less likely to reduce their drug use than beneficiaries in general. In addition, the gap was not associated with a large reduction in adherence. It suggests that concerns about the coverage gap’s harmful effects on medication adherence, or comorbidities might be overstated.
Implications for Further Research
Further studies on how people make medication use decisions in the face of changes in benefits and how the coverage affects non-drug medical outcomes are warranted.
Depression is a common and disabling mental disorder with the leading cause of disability.1 Approximately 10% of American adults, or about 19 million of people suffer from depression every year,2 and 50 to 85% of people with depression will experience recurrent episode during their life time.3 Although available pharmacotherapies are known to be effective to alleviate symptoms and decrease recurrent episodes of depression, less than half of people with depression maintain antidepressant pharmacotherapy.2, 3 Depression affects 13% of US Medicare beneficiaries aged 65 and older and depression often coexists with other chronic physical conditions among older adults. For example, depression affects up to 40% of patients with heart failure.4 Coexisting depression reduces adherence with recommended care, increases healthcare costs and morbidity and even mortality.5, 6–11
Heart failure (HF) affects over 5.7 million Americans with more than 660,000 newly diagnosed cases, 277,000 deaths, and $39 billion in direct and indirect costs yearly, and is also the leading cause for hospitalization among Medicare beneficiaries.12 Guideline-recommended pharmacotherapy for HF, if followed, decreases morbidity and mortality and may reduce healthcare costs.13, 14 It is important to maintain the pharmacotherapy for HF. Two potential contributors to medication non-adherence in HF patients are the presence of depression and high out-of-pocket medication costs.15, 16
Medication use among Medicare beneficiaries has increased and adherence has improved since the implementation of the Medicare Part D prescription drug benefit in 2006.16, 17 However, the structure of the benefit, particularly, the coverage gap, is still problematic. The standard Part D benefit in 2007 included an initial $265 deductible, an insured period in which beneficiaries paid 25 percent of drug cost between $265 and $2400 (“initial coverage phase”), and a coverage gap phase in which beneficiaries paid all medication costs out of pocket until their out-of-pocket spending reached $3850, and then 5% coinsurance above that threshold (“catastrophic coverage phase”). Seniors with multiple chronic conditions often enter the Part D coverage gap and once there the probability of adherence with their medication regimen typically decreases.18–23
Under the current provisions of the US Affordable Care Act, the coverage gap will be gradually reduced and eliminated by 2020. Still, it remains of interest to understand how beneficiaries with coexisting conditions respond to the coverage gap and whether their response differs by type of medications. For example, the coverage gap could have a disproportionate impact on seniors with co-occurring depression and HF as they are more likely to enter the coverage gap and to reduce their medication use than patients without these comorbidities,24–26 and pharmacotherapy for both conditions may save downstream medical costs by preventing hospitalizations and progression of these disorders.
To provide policymakers with evidence on how these medically complex patients respond to the coverage gap, we address the following questions: (a) What proportion of Part D beneficiaries with depression enter the coverage gap? What about among those with comorbid depression and HF? (b) Do beneficiaries reduce their drug use and spending after entering the coverage gap, and if so do their responses differ for use of brand-name vs. generic drugs? (c) Do beneficiaries with comorbid depression and HF make similar adjustment in their use of heart and antidepressant drugs? (d) How does these patients’ adherence with their medications respond to the gap? e) How do generic-and low-income subsidy (LIS) coverage benefits affect medication use patterns within the gap compared to no drug coverage?
Previous studies used pharmacy data either from one local Medicare-Advantage Part D (MA-PD) plan,19, 21 or for one specific condition – beneficiaries with diabetes.22, 23, 27, 28 This report is the first to use a nationally representative sample of claims data to evaluate how the Medicare Part D coverage gap affects medication use among Medicare beneficiaries with depression and HF any other coexisting physical and mental illnesses.
METHODS
Data source
We obtained national Medicare data including demographic and enrollment information, plan benefits, and prescription drug events for a 5% random sample of all beneficiaries who had a fee-for-service plan to cover inpatient (Medicare Part A) and physician services (Medicare Part B) and were continuously enrolled in a stand-alone Part D plan (PDP) in 2007. We then identified seniors with depression and HF using 2007 indicators in the Centers for Medicare & Medicaid Services Chronic Condition Warehouse (Appendix Table 1).29
Setting and study groups
Even though the standard Part D benefit design has a coverage gap, some beneficiaries were eligible for partial or full drug coverage for generic and/or brand-name medications while in the coverage gap,30 and some plans offered slightly modified thresholds for entering the coverage-gap or catastrophic coverage period.31 Moreover, some beneficiaries with low-incomes received federal assistances and subsidies from state governments and therefore were not exposed to the sudden change in price when their total pharmacy spending reached the coverage-gap threshold.32 This group of beneficiaries includes those dually eligible for Medicare and Medicaid as well as those who were eligible for Part D federal low income subsidies (LIS).
Based on the types of coverage before and after the coverage gap threshold, we classified beneficiaries into three groups: “no-coverage” and “generic-coverage group”, and those whose coverage did not change before or after the coverage-gap threshold due to LIS. Beneficiaries in the generic-coverage group were covered only for generic drugs in the gap. We used the LIS group to control for underlying trends in use because their drug coverage remained the same over the year while the other two groups had a sudden decrease in drug coverage. We acknowledge that LIS group has different socio-economic characteristics than non-LIS because LIS group is poor. However, as long as different groups have similar baseline trends, the difference-in-difference estimates can be unbiased.33 We tested the pre-gap baseline trends in both antidepressant use and overall medication use across three groups, and found no statistically-significant difference between each group comparison.34 We excluded beneficiaries with both generic and branded coverage (n=174) because there were too few to draw meaningful conclusions.
Outcomes
For beneficiaries who entered the coverage gap, we classified the index date as the first day that the beneficiary’s total drug spending reached the coverage gap threshold, and defined “pre-gap” period as 1/1/2007 to that index date and “within-gap” period as the first date after the index date until the last day of the coverage gap among those entering the catastrophic period or until 12/31/2007. We then analyzed each outcome for pre- and within-gap periods.
We defined four main outcomes in both pre-gap and within-gap periods: (a) probability of using any medication (1=used a medication; 0=did not use a medication); (b) average number of monthly prescriptions filled per month defined as the mean number of filled prescriptions standardized by 30 days’ supply (i.e., a prescription with 90 days’ supply counts as 3 monthly prescription fills); (c) average monthly pharmacy spending; and (d) medication adherence measured by the medication possession ratio (MPR) defined as the proportion of days during a given period (e.g., either pre-gap or within-gap period) that a subject had possession of any drug for chronic illnesses. To determine whether the coverage gap had a differential effect on type of medications, we constructed the above outcomes separately for HF and antidepressant medications (Appendix Table 1 provides the list of medications), and we evaluated first three outcomes separately for both brand-name and generic drugs.
Data analytical procedures
We used the propensity score approach to balance different groups on observed characteristics.35 To do so, we first conducted a multinomial logit model to calculate the probability (or propensity score) of being in one of the three groups: no-coverage, generic-only, and LIS groups, based on Zip Code level education level and median household income, as well as beneficiary-level age, sex, race, and prescription drug hierarchical condition (RxHCC), the beneficiary risk adjuster used by CMS to adjust payment to plans for expected pharmacy costs.35, 36 For those in the no-coverage group, the propensity score is the predicted probability of belonging to the no-coverage group (P_hat_nocoverage), for those with generic coverage, the propensity score is the predicted probability of belonging to the generic-coverage group (P_hat_genericonly), and for those with LIS, the propensity score is the predicted probability of belonging to LIS group.
In the second step, we then conducted a multiple linear regression analysis with the inverse of propensity score as a weight. For example, the weight for individuals in the no-coverage is 1/P_hat_nocoverage, the weight for individuals in the generic-only group is 1/P_hat_genericonly. This effectively assigned a higher weight to individuals with similar characteristics in groups. In this model, the dependent variable is the pre-gap and within-gap difference for each previously-defined outcome. The key independent variable is the indicator for being in a coverage group. In the model, we controlled for time in the coverage gap because the longer beneficiaries stayed in the gap, the more likely they might change medication usage. We conducted statistical analyses using SAS software, version 9.2 (SAS Institute Inc., Cary, NC) and R: A Language and Environment for Statistical Computing, version 2.12.
RESULTS
Comparisons of patient characteristics and proportion entering the coverage gap
Among the 552,956 senior Medicare beneficiaries in the overall sample, 12% had depression, 19% had HF and about 4% had coexisting depression and HF. Overall, those with depression, HF, or both conditions combined were more likely to enter the coverage gap than Medicare patients in general. For example, in the no-coverage group, 24.3% of overall population, 43.3% of those with depression, 43.7% of those with HF, and 58.3% of those with both depression and HF entered the coverage gap in 2007. Beneficiaries in the generic-coverage and LIS groups were more likely to enter the coverage gap and go through the gap than those with no-gap coverage (Table 1).
Table 1.
Proportions of Seniors Getting into and out of the Coverage Gap among All Elderly Beneficiaries, by Comorbidity
| No-coverage | Generic-only | LIS* | ||||
|---|---|---|---|---|---|---|
|
Proportion Getting in the Coverage Gap
| ||||||
| N | % | N | % | N | % | |
| Overall Population | 70616 | 24.3 | 24777 | 53.0 | 93196 | 49.3 |
| Those with Depression | 10370 | 43.3 | 4057 | 69.6 | 23439 | 73.1 |
| Those with Heart Failure | 17111 | 43.7 | 6525 | 69.1 | 35386 | 68.2 |
| Those with Heart Failure and Depression | 3036 | 58.3 | 1269 | 78.5 | 10389 | 82 |
|
| ||||||
|
Proportion Getting Out the Coverage Gap among Those in the Gap
| ||||||
| Overall Population | 9021 | 12.8 | 3306 | 13.3 | 34242 | 36.7 |
| Those with Depression | 2139 | 20.6 | 779 | 19.2 | 11394 | 48.6 |
| Those with Heart Failure | 3037 | 17.8 | 1080 | 16.6 | 15442 | 43.6 |
| Those with Heart Failure and Depression | 772 | 25.4 | 289 | 22.8 | 5554 | 53.5 |
Note:
Abbreviations: LIS = low-income-subsidies.
Table 2 compares characteristics between each study group and comparison group (Panel A and Panel B are for before and after propensity score adjustment, respectively). After propensity score weighting, all characteristics used to calculate propensity scores, including age, sex, race, education level, median household income, and RxHCC, were balanced across groups.
Table 2.
Characteristics of Beneficiaries with Depression and Heart Failure Who Entered the Coverage Gap in 2007
| A. Before Propensity Score Weighting
| |||||||
|---|---|---|---|---|---|---|---|
| Variables | No Coverage (n=2948) | Generic-only (n=1224) | LIS (n=9809) | ||||
|
| |||||||
| N | % | N | % | N | % | P-value | |
| Female sex | 2123 | 72 | 879 | 72 | 7696 | 78 | <.001 |
| Race | |||||||
| Non-Hispanic White | 2809 | 95 | 1185 | 97 | 7401 | 75 | <.001 |
| African American | 61 | 2 | 9 | 1 | 1037 | 11 | <.001 |
| Hispanic | 51 | 2 | 21 | 2 | 1059 | 11 | <.001 |
| Asian | 13 | 0 | 3 | 0 | 189 | 2 | <.001 |
| Age | |||||||
| 65–74 | 696 | 24 | 363 | 30 | 3148 | 32 | <.001 |
| 75–84 | 1186 | 40 | 497 | 41 | 3799 | 39 | 0.2 |
| ≥ 85 | 1066 | 36 | 364 | 30 | 2862 | 29 | <.001 |
|
| |||||||
| Mean | SD | Mean | SD | Mean | SD | ||
|
| |||||||
| Zip Code Completion of College | 0.26 | 0.16 | 0.26 | 0.16 | 0.21 | 0.13 | <.001 |
| Zip Code log of median household income | 10.69 | 0.35 | 10.68 | 0.34 | 10.5 | 0.34 | <.001 |
| Prescription drug risk score | 1.23 | 0.34 | 1.27 | 0.35 | 1.28 | 0.36 | <.001 |
| B. After Propensity Score Weighting†
| |||||||
|---|---|---|---|---|---|---|---|
| Variables | No Coverage (n=2948) | Generic-only (n=1224) | LIS (n=9809) | ||||
|
| |||||||
| N | % | N | % | N | % | P-value | |
| Female sex | 2123 | 76 | 879 | 77 | 7696 | 77 | 0.15 |
| Race | |||||||
| Non-Hispanic White | 2809 | 82 | 1185 | 82 | 7401 | 82 | 0.88 |
| African American | 61 | 8 | 9 | 7 | 1037 | 8 | 0.09 |
| Hispanic | 51 | 7 | 21 | 8 | 1059 | 8 | 0.06 |
| Asian | 13 | 2 | 3 | 2 | 189 | 1 | 0.25 |
| Age | |||||||
| 65–74 | 696 | 30 | 363 | 30 | 3148 | 30 | 0.96 |
| 75–84 | 1186 | 39 | 497 | 39 | 3799 | 39 | 0.84 |
| ≥ 85 | 1066 | 30 | 364 | 30 | 2862 | 31 | 0.68 |
|
| |||||||
| Mean | SD | Mean | SD | Mean | SD | ||
|
| |||||||
| Zip Code Completion of College | 0.22 | 0.30 | 0.22 | 0.48 | 0.22 | 0.17 | 0.61 |
| Zip Code log of median household income | 10.59 | 0.75 | 10.57 | 1.14 | 10.58 | 0.42 | 0.08 |
| Prescription drug risk score | 1.26 | 0.77 | 1.27 | 1.22 | 1.27 | 0.43 | 0.07 |
Abbreviations: LIS = low-income-subsidies
All numbers in panel B are adjusted using the inverse propensity score weights. Propensity scores were calculated using logistic regression models that predict the probability of being in a study group, controlling for beneficiary-level age, sex, race, and prescription drug hierarchical condition, and Zip Code level education and log of median household income.
To assess differences in baseline socio-demographic characteristics among beneficiaries in three different coverage groups, descriptive statistical analyses were performed using two-sided Chi-square test for categorical variables and Fisher’s two-sided F test for continuous variables.
We excluded those with end stage renal disease (n = 389) and outliers (n = 269) defined as data point more than 4 interquartile ranges (IQRs) below the 1st quartile or above the 3rd quartile.
Bold denotes statistically significant at α = 0.05.
Time spent in the gap
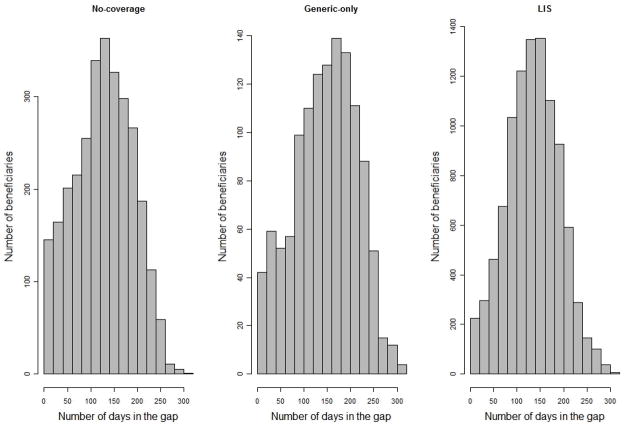
Figure 1 shows the histograms of the time spent in the gap for each group. On average, beneficiaries in the no-coverage group stayed 127 days in the gap, 7 days fewer than those in the LIS group (p <.05), while those in the generic-only group spent 146 days in the gap, 12 days more than those in the LIS group (p <.05).
Figure 1.
Histograms of the Time Spent in the Gap by Group
Abbreviations: LIS = low-income-subsidies; this is the comparison group.
Evaluating the effects of the coverage gap on medication use and adherence
Table 3 presents the effects of the coverage gap on four measures of medication use for all medications, antidepressants, and HF drugs using multiple regression models with propensity-score weighting.
Table 3.
The Impact of the Coverage Gap on Medication Use among Elderly Beneficiaries Diagnosed with Depression and Heart Failure Who Entered the Coverage Gap Period in 2007
| A. All Medications | |||||||
|---|---|---|---|---|---|---|---|
| Unadjusted Data* | Diff-in-Diff Coverage Gap Effects† | % Change, Diff-in-Diff Effects/Pre-Gap Values | |||||
|
| |||||||
| Pre-Gap | Within-Gap | Estimate | 95% CI | % | 95% CI | ||
|
Probability of Using any Drug
| |||||||
| All | No-coverage | 1.00 | 0.96 | −0.01 | (−0.02, −0.01) | −1.2 | (−2.0, −0.5) |
| Generic-only | 1.00 | 0.97 | −0.01 | (−0.02, −0.01) | −1.4 | (−2.2, −0.7) | |
| LIS | 1.00 | 0.99 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 1.00 | 0.91 | −0.02 | (−0.03, −0.01) | −2.0 | (−3.0, −1.0) |
| Generic-only | 1.00 | 0.92 | −0.03 | (−0.04, −0.02) | −2.9 | (−3.9, −1.9) | |
| LIS | 1.00 | 0.97 | reference | ||||
|
| |||||||
| Generics | No-coverage | 0.99 | 0.94 | −0.01 | (−0.02, 0.00) | −1.1 | (−1.9, −0.2) |
| Generic-only | 1.00 | 0.96 | −0.01 | (−0.02, 0.00) | −1.3 | (−2.2, −0.5) | |
| LIS | 0.99 | 0.98 | reference | ||||
|
| |||||||
|
No. of Monthly Prescriptions for any Drug
| |||||||
| All | No-coverage | 7.08 | 6.17 | −0.54 | (−0.65, −0.42) | −7.6 | (−9.2, −5.9) |
| Generic-only | 7.97 | 6.81 | −0.51 | (−0.63, −0.39) | −6.4 | (−7.9, −4.9) | |
| LIS | 8.61 | 8.19 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 3.29 | 2.57 | −0.36 | (−0.42, −0.30) | −10.8 | (−12.7, −9.0) |
| Generic-only | 3.49 | 2.57 | −0.33 | (−0.39, −0.26) | −9.3 | (−11.1, −7.6) | |
| LIS | 3.82 | 3.42 | reference | ||||
|
| |||||||
| Generics | No-coverage | 3.76 | 3.56 | −0.18 | (−0.26, −0.09) | −4.7 | (−7.0, −2.5) |
| Generic-only | 4.43 | 4.19 | −0.19 | (−0.28, −0.10) | −4.3 | (−6.2, −2.3) | |
| LIS | 4.75 | 4.72 | reference | ||||
|
| |||||||
|
Monthly Pharmacy Spending for any Drug
| |||||||
| All | No-coverage | 429 | 357 | −48.82 | (−57.3, −40.33) | −11.4 | (−13.4, −9.4) |
| Generic-only | 468 | 374 | −34.28 | (−42.84, −25.72) | −7.3 | (−9.2, −5.5) | |
| LIS | 589 | 558 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 342 | 277 | −40.82 | (−48.49, −33.15) | −11.9 | (−14.2, −9.7) |
| Generic-only | 364 | 274 | −32.38 | (−40.13, −24.64) | −8.9 | (−11.0, −6.8) | |
| LIS | 464 | 433 | reference | ||||
|
| |||||||
| Generics | No-coverage | 86 | 79 | −7.85 | (−10.9, −4.81) | −9.1 | (−12.6, −5.6) |
| Generic-only | 103 | 99 | −2.05 | (−5.12, 1.02) | −2.0 | (−5.0, 1.0) | |
| LIS | 124 | 123 | reference | ||||
| B. Antidepressants | |||||||
|---|---|---|---|---|---|---|---|
| Unadjusted Data | Diff-in-Diff Coverage Gap Effects† | % Change, Diff-in-Diff Effects/Pre-Gap Values | |||||
|
| |||||||
| Pre-Gap | Within-Gap | Estimate | 95% CI | % | 95% CI | ||
|
Probability of Using an Antidepressant
| |||||||
| All | No-coverage | 0.79 | 0.71 | −0.01 | (−0.03, 0.00) | −1.6 | (−3.7, 0.5) |
| Generic-only | 0.82 | 0.74 | −0.01 | (−0.03, 0.01) | −1.3 | (−3.4, 0.7) | |
| LIS | 0.80 | 0.77 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 0.38 | 0.32 | −0.01 | (−0.02, 0.00) | −2.6 | (−6.5, 1.3) |
| Generic-only | 0.36 | 0.31 | 0.00 | (−0.02, 0.01) | −1.3 | (−5.4, 2.8) | |
| LIS | 0.34 | 0.32 | reference | ||||
|
| |||||||
| Generics | No-coverage | 0.55 | 0.49 | 0.01 | (−0.01, 0.02) | 1.3 | (−1.8, 4.3) |
| Generic-only | 0.59 | 0.54 | 0.00 | (−0.01, 0.02) | 0.6 | (−2.2, 3.5) | |
| LIS | 0.59 | 0.56 | reference | ||||
|
| |||||||
|
No. of Monthly Prescription for Antidepressants
| |||||||
| All | No-coverage | 0.75 | 0.68 | −0.04 | (−0.06, −0.01) | −5.0 | (−8.2, −1.7) |
| Generic-only | 0.84 | 0.74 | −0.02 | (−0.04, 0.00) | −2.4 | (−5.3, 0.5) | |
| LIS | 0.88 | 0.83 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 0.29 | 0.25 | −0.03 | (−0.04, −0.02) | −10.5 | (−15.4, −5.5) |
| Generic-only | 0.30 | 0.24 | −0.04 | (−0.05, −0.02) | −12.7 | (−17.6, −7.8) | |
| LIS | 0.29 | 0.28 | reference | ||||
|
| |||||||
| Generics | No-coverage | 0.46 | 0.43 | −0.01 | (−0.03, 0.01) | −1.5 | (−6.0, 3.1) |
| Generic-only | 0.54 | 0.51 | 0.02 | (0.00, 0.04) | 3.3 | (−0.6, 7.2) | |
| LIS | 0.58 | 0.55 | reference | ||||
|
| |||||||
|
Monthly Pharmacy Spending for Antidepressants
| |||||||
| All | No-coverage | 40 | 33 | −3.05 | (−4.74, −1.37) | −7.7 | (−11.9, −3.4) |
| Generic-only | 44 | 35 | −3.18 | (−4.88, −1.48) | −7.2 | (−11.0, −3.3) | |
| LIS | 47 | 43 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 29 | 25 | −3.37 | (−4.96, −1.78) | −11.7 | (−17.3, −6.2) |
| Generic-only | 31 | 25 | −3.96 | (−5.57, −2.35) | −13.0 | (−18.2, −7.7) | |
| LIS | 30 | 30 | reference | ||||
|
| |||||||
| Generics | No-coverage | 11 | 8 | 0.31 | (−0.46, 1.09) | 2.8 | (−4.2, 9.8) |
| Generic-only | 14 | 11 | 0.78 | (0.00, 1.56) | 5.6 | (0, 11.2.0) | |
| LIS | 17 | 13 | reference | ||||
|
| |||||||
|
Medication Possession Ratio(MPR) for Antidepressants
| |||||||
| All | No-coverage | 0.56 | 0.49 | −0.01 | (−0.02, 0.01) | −1.3 | (−3.8, 1.1) |
| Generic-only | 0.60 | 0.53 | −0.01 | (−0.02, 0.01) | −0.9 | (−3.2, 1.4) | |
| LIS | 0.61 | 0.58 | reference | ||||
| C. Heart Failure Medications | |||||||
|---|---|---|---|---|---|---|---|
| Unadjusted Data | Diff-in-Diff Coverage Gap Effects† | % Change, Diff-in-Diff Effects/Pre-Gap Values | |||||
|
| |||||||
| Pre-Gap | Within-Gap | Estimate | 95% CI | % | 95% CI | ||
|
Probability of Using a Heart Failure Drugs
| |||||||
| All | No-coverage | 0.95 | 0.88 | −0.01 | (−0.02, 0.00) | −1.1 | (−2.3, 0.1) |
| Generic-only | 0.96 | 0.89 | −0.03 | (−0.04, −0.02) | −2.8 | (−3.9, −1.6) | |
| LIS | 0.95 | 0.92 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 0.74 | 0.55 | 0.00 | (−0.02, 0.02) | −0.2 | (−2.6, 2.2) |
| Generic-only | 0.74 | 0.56 | −0.02 | (−0.04, −0.01) | −3.2 | (−5.6, −0.8) | |
| LIS | 0.68 | 0.55 | reference | ||||
|
| |||||||
| Generics | No-coverage | 0.89 | 0.83 | −0.01 | (−0.03, 0.00) | −1.5 | (−3.1, 0.0) |
| Generic-only | 0.90 | 0.85 | −0.03 | (−0.04, −0.01) | −2.9 | (−4.4, −1.4) | |
| LIS | 0.89 | 0.88 | reference | ||||
|
| |||||||
|
No. of Monthly Prescriptions for Heart Failure Drugs
| |||||||
| All | No-coverage | 2.44 | 2.04 | −0.23 | (−0.28, −0.18) | −9.4 | (−11.5, −7.2) |
| Generic-only | 2.66 | 2.23 | −0.21 | (−0.26, −0.15) | −7.8 | (−9.8, −5.8) | |
| LIS | 2.59 | 2.40 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 0.92 | 0.57 | −0.12 | (−0.15, −0.09) | −12.8 | (−15.8, −9.8) |
| Generic-only | 0.98 | 0.58 | −0.09 | (−0.12, −0.06) | −9.2 | (−12.1, −6.4) | |
| LIS | 0.88 | 0.63 | reference | ||||
|
| |||||||
| Generics | No-coverage | 1.52 | 1.47 | −0.11 | (−0.15, −0.07) | −7.3 | (−10.1, −4.4) |
| Generic-only | 1.68 | 1.64 | −0.12 | (−0.16, −0.07) | −7.0 | (−9.6, −4.4) | |
| LIS | 1.71 | 1.77 | reference | ||||
|
| |||||||
|
Monthly Pharmacy Spending for Heart Failure Drugs
| |||||||
| All | No-coverage | 83 | 60 | −10.47 | (−12.66, −8.29) | −12.6 | (−15.2, −10.0) |
| Generic-only | 90 | 64 | −7.75 | (−9.96, −5.55) | −8.7 | (−11.1, −6.2) | |
| LIS | 88 | 76 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 62 | 37 | −8.05 | (−10.09, −6.00) | −13.0 | (−16.3, −9.7) |
| Generic-only | 66 | 39 | −5.18 | (−7.24, −3.12) | −7.9 | (−11.0, −4.7) | |
| LIS | 62 | 46 | reference | ||||
|
| |||||||
| Generics | No-coverage | 21 | 23 | −2.43 | (−3.43, −1.43) | −11.5 | (−16.2, −6.7) |
| Generic-only | 24 | 25 | −2.57 | (−3.59, −1.56) | −10.8 | (−15.1, −6.6) | |
| LIS | 26 | 30 | reference | ||||
|
| |||||||
|
Medication Possession Ratio(MPR) for Heart Failure Drugs
| |||||||
| All | No-coverage | 0.89 | 0.79 | −0.02 | (−0.03, −0.01) | −2.5 | (−3.7, −1.2) |
| Generic-only | 0.90 | 0.82 | −0.02 | (−0.04, −0.01) | −2.6 | (−3.9, −1.3) | |
| LIS | 0.89 | 0.86 | reference | ||||
“Gap Effects” are adjusted estimates from the difference model with the inverse of propensity score as a weight. The estimates measure changes in outcomes between within-gap and pre-gap periods in a study group, relative to the changes in outcomes in the other group.
Abbreviations: LIS = low-income-subsidies; this is the comparison group. HF=heart failure.
Bold denotes statistically significant at α = 0.05
The coverage gap was associated with less use of drugs, especially less use of brand-name drugs
Compared to the LIS group, the probability of using any drug in both no-coverage and generic-only group decreased slightly by 1.2% (95% CI 0.5% – 2.0%) and 1.4% (95% CI 0.7% – 2.2%). We also observed decreases in number of monthly prescriptions and monthly spending on prescription drugs associated with the coverage gap. With the exception of some measures of antidepressant usage, decreases were statistically significant.
After entering the coverage gap, beneficiaries reduced brand-name drugs more than generic drugs. For example, beneficiaries in the no-coverage group reduced their average number of monthly prescriptions for branded and generic drugs by 10.8% (95% CI 9.0%-12.7%) and 4.7% (95% CI 2.5%-7.0%), relative to the LIS group. Similarly, beneficiaries with generic-coverage reduced their average number of monthly prescriptions for branded and generic drugs by 9.3% (95% CI 7.6%-11.1%) and 4.3% (95% CI 2.3%-6.2%), respectively.
The coverage gap was associated with less reduction in antidepressants than HF drugs
While in the gap, beneficiaries decreased their use of antidepressants less than HF drugs. This pattern was more strongly observed in the generic-coverage group. For example, relative to the LIS group, the no-coverage group decreased their monthly prescriptions of antidepressants by 5.0% (95% CI 1.7%-8.2%), while they decreased their use of HF by 9.4% (95% CI 7.2%-11.5%). Those with generic-coverage reduced their monthly number of antidepressant drugs (2.4%) but this was not statistically significant, while they did reduce their use of HF drugs by 7.8% (95% CI 5.8%-9.8%).
The coverage gap was not associated with the reduction in medication adherence
While medication use such as average number of monthly prescriptions was dropped during the gap, medication adherence, as measured by the medication possession ratio, did not change much. Relative to the LIS group, medication adherence for antidepressants did not decrease, and HF adherence dropped slightly while in the coverage gap. Compared to the LIS group, neither the no-coverage group nor the generic-coverage group reduced their adherence for antidepressant medications. However, relative to the LIS group, those in the no-coverage group decreased their MPR for HF drugs, from 0.89 to 0.79, or 2.5% (95% CI 1.2%-3.7%), and those with generic-coverage reduced their MPR, from 0.90 to 0.82, or 2.6% (95% CI 1.3%-3.9%).
Partial drug coverage did not benefit medication use within the gap
Contrary to our expectations, the coverage gap did not have less of an impact on those with generic coverage relative to those with no coverage. Appendix Table 2 explores differences in medication use between those with no-coverage and generic-coverage. Compared to the generic-only group, decreases in medication use for those with no-coverage were insignificant or negligibly small. Moreover, those with generic coverage did not increase their use of generic drugs in the gap; i.e., they did not switch from brand-name drugs to generic drugs.
DISCUSSION
Medicare Part D beneficiaries with depression and HF frequently entered the coverage gap, and when they did they decreased their use of pharmacotherapy for these conditions, particularly use of brand-name medications. Beneficiaries with coverage for generic medications did not have much advantage in medication adherence over those without any prescription drug coverage.
Beneficiaries with generic coverage paid on average $23 per month for generic drugs in the pre-gap and their average monthly copayments for generic drugs increased to $27 in the gap. There is a small increase in copayments for generic drugs before and after getting into the gap. It is possible that this has an effect on the reduction in generic drugs in the gap and it is also possible to have spillover effect from having to spend more on branded drugs. This might explain why beneficiaries with generic coverage in the gap did not improve adherence much compared to those in the no-coverage group.
We acknowledge that beneficiaries with LIS have different socio-economic and demographic characteristics than those with non-LIS. Therefore, they would not be entirely comparable with the beneficiaries in the no-coverage or generic-coverage groups. We employed a propensity score model to minimize these differences in baseline characteristics. We acknowledge that propensity score method does not address the issue of unobservable, and in some situations may worsen the problem of unobserved confounders, relative to ordinary regression methods.37
After minimizing observed differences, we used those in the LIS group to control for secular trends in medication use (e.g., natural decline in medication adherence not related to medication costs) and to compare the differences in drug use before and after the coverage gap across groups (difference-in-difference). This difference-in-difference estimates do not require that groups be the same at the baseline but do require the assumption that baseline trend should be parallel. We conducted the baseline trend in drug use across groups and confirmed this assumption.34
We included the time of being in the gap in the model because the longer individuals stay in the gap, the more likely they will reduce their drug use. Individuals with higher utilization and costs may enter the gap earlier but they might get out of the gap earlier too, so they do not necessarily stay in the gap longer. We also included those exiting the gap in the analysis and included an indicator in the model to distinguish the results among those exiting the gap. Our difference-in-difference approach should mitigate the potential endogeneity of time in the gap and gap exit, but it cannot eliminate it.
We found no prior studies evaluating how beneficiaries with coexisting mental and medical conditions respond to drug coverage changes. Our prior hypothesis is that beneficiaries would drop their antidepressants first when having to make a decision to drop antidepressants or heart failure drugs, but this was not observed. One interpretation is that beneficiaries with depression and HF might care more about immediate symptom relief than control of a condition that constitutes a long-term health hazard but may be asymptomatic in the short run.
Although the coverage gap will be gradually reduced and eliminated by 2020 under the current provisions of ACA, it remains of interest to understand how beneficiaries with coexisting conditions respond to the coverage gap and whether their response differs by type of medications. We found that beneficiaries with coexisting depression and HF were less likely to reduce their drug use than beneficiaries in general. For example, the reduction in medication use due to the coverage gap was smaller among elderly beneficiaries with depression and HF (7.6%) compared to overall elderly beneficiaries (16.0%).19, 38 In addition, the gap was not associated with large reduction in adherence. This finding is encouraging because it suggests that concerns about the coverage gap’s harmful effects on medication adherence, or comorbidities might be overstated. Our findings also contribute to the general literature evaluating the effects of cost-sharing of prescription drugs on utilization among patients with coexisting chronic conditions. It is important to understand how patients make decisions to forgo one type of treatment first.
Acknowledgments
Source of Funding:
NIMH RC1 MH088510, AHRQ R01 HS018657, University of Pittsburgh CRDF (Dr. Zhang); P30 MH071944, P30 MH090333, the UPMC Endowment in Geriatric Psychiatry (Dr. Reynolds)
Role of the sponsor:
The National Institute of Mental Health, Agency for Healthcare Research and Quality, and University of Pittsburgh had no role in the design or conduct of our study, in the analysis and interpretation of our data, or in drafting of this manuscript.
Appendix
Appendix Table 1.
| Panel A. Definitions for Depression and Heart Failure | |||
|---|---|---|---|
| Chronic Conditions | Reference Time Period | Valid ICD-9 Codes | Number/Type of Claims to Qualify |
| Depression | 1/1/2007–12/31/2007 | DX: 296.2–296.6, 296.89, 298.0, 300.4, 309.1, and 311 (any DX on the claim) | At least 1 claim with DX codes during the 1-yr period (2007) |
| Heart Failure | 1/1/2006–12/31/2007 | DX: 398.91, 402.01, 402.11, 402.91, 404.01, 404.11, 404.91, 404.03, 404.13, 404.93, 428.0X-428.4X, 428.9X (any DX on the claim) | At least 1 inpatient, outpatient or physician claim with DX codes during the 2-yr period (2006–2007) |
| Panel B. Drug Classes Used to Treat Depression and Heart Failure | |
|---|---|
| Chronic Medical Illnesses | Major Drug Classes |
| Depression | Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin/Noradrenaline Reuptake Inhibitors (SNRIs), tricyclic antidepressants, Alpha-2 Receptor Antagonists (NaSSA), MAO Inhibitor Nonselective & irreversible, Norepinephrine & Dopamine Reuptake Inhibitors (NDRIs), Serotonin-2 Antagonist-Reuptake Inhibitors (SARIs) and the combination drugs |
| Heart failure | Angiotensin-Converting Enzyme inhibitors (ACEi), Angiotensin II Receptor Blockers (ARB), beta blockers, Calcium Channel Blockers, diuretics, vasodilators, digoxin |
Appendix Table 2.
The Impact of the Coverage Gap on Medication Use among Elderly Beneficiaries Diagnosed with Depression and Heart Failure Who Entered the Coverage Gap Period in 2007
| Panel A. All Medications | |||||||
|---|---|---|---|---|---|---|---|
| Unadjusted Data | Diff-in-Diff Coverage Gap Effects† | % Change, Diff-in-Diff Effects/Pre-Gap Values | |||||
|
| |||||||
| Pre-Gap | Within-Gap | Estimate | 95% CI | % | 95% CI | ||
|
Probability of Using any Drug
| |||||||
| All | No-coverage | 1.00 | 0.96 | 0.00 | (−0.005, 0.009) | 0.2 | (−0.49, 0.88) |
| Generic-only | 1.00 | 0.97 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 1.00 | 0.91 | 0.01 | (0.000, 0.019) | 0.9 | (−0.05, 1.88) |
| Generic-only | 1.00 | 0.92 | reference | ||||
|
| |||||||
| Generics | No-coverage | 0.99 | 0.94 | 0.00 | (−0.005, 0.011) | 0.3 | (−0.53, 1.10) |
| Generic-only | 1.00 | 0.96 | reference | ||||
|
| |||||||
|
No. of Monthly Prescriptions for any Drug
| |||||||
| All | No-coverage | 7.08 | 6.17 | −0.03 | (−0.141, 0.087) | −0.4 | (−1.99, 1.23) |
| Generic-only | 7.97 | 6.81 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 3.29 | 2.57 | −0.03 | (−0.089, 0.028) | −0.9 | (−2.71, 0.84) |
| Generic-only | 3.49 | 2.57 | reference | ||||
|
| |||||||
| Generics | No-coverage | 3.76 | 3.56 | 0.01 | (−0.070, 0.094) | 0.3 | (−1.86, 2.51) |
| Generic-only | 4.43 | 4.19 | reference | ||||
|
| |||||||
|
Monthly Pharmacy Spending for any Drug
| |||||||
| All | No-coverage | 429 | 357 | −14.54 | (−22.730, −6.347) | −3.4 | (−5.30, −1.48) |
| Generic-only | 468 | 374 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 342 | 277 | −8.44 | (−15.845, −1.028) | −2.5 | (−4.64, −0.30) |
| Generic-only | 364 | 274 | reference | ||||
|
| |||||||
| Generics | No-coverage | 86 | 79 | −5.80 | (−8.738, −2.864) | −6.7 | (−10.13, −3.32) |
| Generic-only | 103 | 99 | reference | ||||
| Panel B. Antidepressants | |||||||
|---|---|---|---|---|---|---|---|
| Unadjusted Data | Diff-in-Diff Coverage Gap Effects† | % Change, Diff-in-Diff Effects/Pre-Gap Values | |||||
|
| |||||||
| Pre-Gap | Within-Gap | Estimate | 95% CI | % | 95% CI | ||
|
Probability of Using an Antidepressant
| |||||||
| All | No-coverage | 0.79 | 0.71 | 0.00 | (−0.018, 0.014) | −0.2 | (−2.24, 1.78) |
| Generic-only | 0.82 | 0.74 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 0.38 | 0.32 | −0.01 | (−0.019, 0.009) | −1.4 | (−5.14, 2.39) |
| Generic-only | 0.36 | 0.31 | reference | ||||
|
| |||||||
| Generics | No-coverage | 0.55 | 0.49 | 0.00 | (−0.013, 0.020) | 0.6 | (−2.35, 3.56) |
| Generic-only | 0.59 | 0.54 | reference | ||||
|
| |||||||
|
No. of Monthly Prescription for Antidepressants
| |||||||
| All | No-coverage | 0.75 | 0.68 | −0.02 | (−0.041, 0.006) | −2.3 | (−5.43, 0.85) |
| Generic-only | 0.84 | 0.74 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 0.29 | 0.25 | 0.01 | (−0.006, 0.021) | 2.6 | (−2.21, 7.39) |
| Generic-only | 0.30 | 0.24 | reference | ||||
|
| |||||||
| Generics | No-coverage | 0.46 | 0.43 | −0.02 | (−0.045, −0.004) | −5.4 | (−9.77, −0.97) |
| Generic-only | 0.54 | 0.51 | reference | ||||
|
| |||||||
|
Monthly Pharmacy Spending for Antidepressants
| |||||||
| All | No-coverage | 40 | 33 | 0.13 | (−1.500, 1.754) | 0.3 | (−3.76, 4.40) |
| Generic-only | 44 | 35 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 29 | 25 | 0.59 | (−0.946, 2.128) | 2.1 | (−3.29, 7.40) |
| Generic-only | 31 | 25 | reference | ||||
|
| |||||||
| Generics | No-coverage | 11 | 8 | −0.46 | (−1.213, 0.285) | −4.2 | (−10.93, 2.56) |
| Generic-only | 14 | 11 | reference | ||||
|
| |||||||
|
Medication Possession Ratio(MPR) for Antidepressants
| |||||||
| All | No-coverage | 0.56 | 0.49 | 0.00 | (−0.015, 0.011) | −0.4 | (−2.78, 2.01) |
| Generic-only | 0.60 | 0.53 | reference | ||||
| Panel C. Heart Failure Medications | |||||||
|---|---|---|---|---|---|---|---|
| Unadjusted Data | Diff-in-Diff Coverage Gap Effects† | % Change, Diff-in-Diff Effects/Pre-Gap Values | |||||
|
| |||||||
| Pre-Gap | Within-Gap | Estimate | 95% CI | % | 95% CI | ||
|
Probability of Using a Heart Failure Drugs
| |||||||
| All | No-coverage | 0.95 | 0.88 | 0.02 | (0.005, 0.027) | 1.7 | (0.53, 2.81) |
| Generic-only | 0.96 | 0.89 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 0.74 | 0.55 | 0.02 | (0.005, 0.040) | 3.0 | (0.69, 5.38) |
| Generic-only | 0.74 | 0.56 | reference | ||||
|
| |||||||
| Generics | No-coverage | 0.89 | 0.83 | 0.01 | (−0.001, 0.026) | 1.4 | (−0.06, 2.89) |
| Generic-only | 0.90 | 0.85 | reference | ||||
|
| |||||||
|
No. of Monthly Prescriptions for Heart Failure Drugs
| |||||||
| All | No-coverage | 2.44 | 2.04 | −0.02 | (−0.072, 0.028) | −0.9 | (−2.95, 1.16) |
| Generic-only | 2.66 | 2.23 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 0.92 | 0.57 | −0.03 | (−0.054, −0.001) | −3.0 | (−5.87, −0.09) |
| Generic-only | 0.98 | 0.58 | reference | ||||
|
| |||||||
| Generics | No-coverage | 1.52 | 1.47 | 0.01 | (−0.036, 0.048) | 0.4 | (−2.36, 3.13) |
| Generic-only | 1.68 | 1.64 | reference | ||||
|
| |||||||
|
Monthly Pharmacy Spending for Heart Failure Drugs
| |||||||
| All | No-coverage | 83 | 60 | −2.72 | (−4.826, −0.615) | −3.3 | (−5.80, −0.74) |
| Generic-only | 90 | 64 | reference | ||||
|
| |||||||
| Brand-name | No-coverage | 29 | 25 | −2.87 | (−4.839, −0.894) | −4.6 | (−7.81, −1.44) |
| Generic-only | 31 | 25 | reference | ||||
|
| |||||||
| Generics | No-coverage | 21 | 23 | 0.14 | (−0.823, 1.113) | 0.7 | (−3.88, 5.25) |
| Generic-only | 24 | 25 | reference | ||||
|
| |||||||
|
Medication Possession Ratio(MPR) for Heart Failure Drugs
| |||||||
| All | No-coverage | 0.89 | 0.79 | 0.00 | (−0.009, 0.013) | 0.2 | (−1.04, 1.44) |
| Generic-only | 0.90 | 0.82 | reference | ||||
“Gap Effects” are adjusted estimates from the difference model with the inverse of propensity score as a weight. The estimates measure changes in outcomes between within-gap and pre-gap periods in a study group, relative to the changes in outcomes in the other group.
Abbreviations: LIS = low-income-subsidies; this is the comparison group. HF=heart failure.
Bold denotes statistically significant at α = 0.05.
Footnotes
Disclosures and acknowledgments:
Drs. Lave and Zhang recently completed a study to evaluating the effects of high deductible health plan that was partially funded by Highmark Inc. Highmark Inc. sells Part D products. Dr. Reynolds receives pharmaceutical supplies from BMS, Pfizer, Forest Laboratories, and Lilly in support of his NIH-sponsored research.
References
- 1.Centers for Medicare & Medicaid Services. Chronic Condition Data Warehouse User Guide: Version 1.8. 2011 [cited 2011 September 9]; Available from: http://www.ccwdata.org/cs/groups/public/documents/document/ccw_userguide.pdf.
- 2.Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Archives of General Psychiatry. 1993;50(2):85. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- 3.Melfi CA, Chawla AJ, Croghan TW, Hanna MP, Kennedy S, Sredl K. The effects of adherence to antidepressant treatment guidelines on relapse and recurrence of depression. Archives of General Psychiatry. 1998;55(12):1128. doi: 10.1001/archpsyc.55.12.1128. [DOI] [PubMed] [Google Scholar]
- 4.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 5.Sullivan M, Simon G, Spertus J, Russo J. Depression-related costs in heart failure care. Arch Intern Med. 2002;162:1860–1866. doi: 10.1001/archinte.162.16.1860. [DOI] [PubMed] [Google Scholar]
- 6.Pelle AJM, Gidron YY, Szabo BM, Denollet J. Psychological predictors of prognosis in chronic heart failure. Journal of Cardiac Failure. 2008;14:341–350. doi: 10.1016/j.cardfail.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 7.O’Connor CM, Abraham WT, Albert NM, Clare R, Gattis Stough W, Gheorghiade M, Greenberg BH, Yancy CW, Young JB, Fonarow GC. Predictors of mortality after discharge in patients hospitalized with heart failure: an analysis from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) Am Heart J. 2008;156:662–673. doi: 10.1016/j.ahj.2008.04.030. [DOI] [PubMed] [Google Scholar]
- 8.Rathore SS, Wang Y, Druss BG, Masoudi FA, Krumholz HM. Mental Disorders, Quality of Care, and Outcomes Among Older Patients Hospitalized With Heart Failure: An Analysis of the National Heart Failure Project. Archives of General Psychiatry. 2008;65:1402–1408. doi: 10.1001/archpsyc.65.12.1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jiang W, Kuchibhatla M, Clary GL, Cuffe MS, Christopher EJ, Alexander JD, Califf RM, Krishnan RR, O’Connor CM. Relationship between depressive symptoms and long-term mortality in patients with heart failure. Am Heart J. 2007;154:102–108. doi: 10.1016/j.ahj.2007.03.043. [DOI] [PubMed] [Google Scholar]
- 10.Vaccarino V, Kasl SV, Abramson J, Krumholz HM. Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol. 2001;38:199–205. doi: 10.1016/s0735-1097(01)01334-1. [DOI] [PubMed] [Google Scholar]
- 11.Koenig HG. Depression in hospitalized older patients with congestive heart failure. General Hospital Psychiatry. 1998;20:29–43. doi: 10.1016/s0163-8343(98)80001-7. [DOI] [PubMed] [Google Scholar]
- 12.Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES. Heart Disease and Stroke Statistics—2011 Update: a report from the American Heart Association. Circulation. 2011;123(4):e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu J-R, Moser DK, Chung ML, Lennie TA. Objectively Measured, but Not Self-Reported, Medication Adherence Independently Predicts Event-Free Survival in Patients With Heart Failure. Journal of Cardiac Failure. 2008;14(3):203–210. doi: 10.1016/j.cardfail.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wald NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80% BMJ. 2003;326(7404):1419. doi: 10.1136/bmj.326.7404.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newby LK, Allen LaPointe NM, Chen AY, Kramer JM, Hammill BG, DeLong ER, Muhlbaier LH, Califf RM. Long-term adherence to evidence-based secondary prevention therapies in coronary artery disease. Circulation. 2006;113(2):203–212. doi: 10.1161/CIRCULATIONAHA.105.505636. [DOI] [PubMed] [Google Scholar]
- 16.Zhang Y, Lave JR, Donohue JM, Fischer MA, Chernew ME, Newhouse JP. The impact of Medicare Part D on medication adherence among older adults enrolled in Medicare-Advantage products. Medical Care. 2010;48(5):409–417. doi: 10.1097/MLR.0b013e3181d68978. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Y, Donohue JM, Lave JR, O’Donnell G, Newhouse JP. The impact of the Medicare Part D drug benefits on pharmacy and medical care spending. New England Journal of Medicine. 2009;361(1):52–61. doi: 10.1056/NEJMsa0807998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li P, McElligott S, Bergquist H, Schwartz JS, Doshi JA. Effect of the Medicare Part D Coverage Gap on Medication Use Among Patients With Hypertension and Hyperlipidemia. Annals of Internal Medicine. 2012;156(11):776–784. doi: 10.7326/0003-4819-156-11-201206050-00004. [DOI] [PubMed] [Google Scholar]
- 19.Zhang Y, Donohue JM, Newhouse JP, Lave JR. The effects of the coverage gap on drug spending: a closer look at Medicare Part D. Health Affairs. 2009;28 (2):w317–w325. doi: 10.1377/hlthaff.28.2.w317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schneeweiss S, Patrick AR, Pedan A, Varasteh L, Levin R, Liu N, Shrank WH. The effect of Medicare Part D coverage on drug use and cost sharing among seniors without prior drug benefits. Health Affairs. 2009;28(2):w305–316. doi: 10.1377/hlthaff.28.2.w305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raebel MA, Delate T, Ellis JL, Bayliss EA. Effects of reaching the drug benefit threshold on Medicare members’ healthcare utilization during the first year of Medicare Part D. Medical Care. 2008;46(10):1116–1122. doi: 10.1097/MLR.0b013e318185cddd. [DOI] [PubMed] [Google Scholar]
- 22.Schmittdiel JA, Ettner SL, Fung V, Huang J, Turk N, Quiter ES, Swain BE, Hsu JT, Mangione CM. Medicare Part D coverage gap and diabetes beneficiaries. American Journal of Managed Care. 2009;15(3):189–193. [PMC free article] [PubMed] [Google Scholar]
- 23.Fung V, Mangione CM, Huang J, Turk N, Quiter ES, Schmittdiel JA, Hsu J. Falling into the coverage gap: Part D drug costs and adherence for Medicare Advantage prescription drug plan beneficiaries with diabetes. Health Services Research. 2010;45(2):355–375. doi: 10.1111/j.1475-6773.2009.01071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bush D, Ziegelstein R, Patel U, Thombs B, Ford D, Fauerbach J, McCann U, Stewart K, Tsilidis K, Patel A, Feuerstein C, Bass E. Post-Myocardial Infarction Depression Summary, Evidence Report/Technology Assessment No 123. Rockville, MD: Agency for Healthcare Research and Quality; 2005. AHRQ Publication No. 05-E018-1. [cited 2011 May 20]; Available from: http://www.ahrq.gov/clinic/epcsums/midepsum.htm. [PMC free article] [PubMed] [Google Scholar]
- 25.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. Journal of the American Medical Association. 1993;270(15):1819–1825. [PubMed] [Google Scholar]
- 26.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160(14):2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 27.Duru OK, Mangione CM, Hsu J, Steers WN, Quiter E, Turk N, Ettner SL, Schmittdiel JA, Tseng CW. Generic-only drug coverage in the Medicare Part D gap and effect on medication cost-cutting behaviors for patients with diabetes mellitus: the translating research into action for diabetes study. J Am Geriatr Soc. 2010;58(5):822–828. doi: 10.1111/j.1532-5415.2010.02813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gu Q, Zeng F, Patel BV, Tripoli LC. Part D coverage gap and adherence to diabetes medications. Am J Manag Care. 2010;16(12):911–918. [PubMed] [Google Scholar]
- 29.Centers for Medicare & Medicaid Services. Chronic condition data warehouse -User Manual. Baltimore, MD: 2008. [cited 2010 September 6]; Available from: http://www.resdac.umn.edu/CCW/data_available.asp. [Google Scholar]
- 30.Kaiser Family Foundation. Part D plan availability in 2011 and key changes since 2006. Menlo Park, CA, USA: 2010. [updated 2010; cited 2011 July 10]; Available from: http://kff.org/medicare/upload/8107.pdf. [Google Scholar]
- 31.Kaiser Family Foundation. Medicare Part D 2010 data spotlight: the coverage gap. Menlo Park, CA, USA: 2009. [updated 2009; cited 2011 April 22]; Available from: http://kff.org/medicare/upload/8008.pdf. [Google Scholar]
- 32.Kaiser Family Foundation. The Medicare Prescription Drug Benefit. 2010 [cited 2011 July 19]; Available from: http://kff.org/medicare/upload/7044-11.pdf.
- 33.Meyer BD. Natural and quasi-experiments in economics. Journal of Business and Economics Statistics. 1995;13:151–161. [Google Scholar]
- 34.Zhang Y, Baik S, Zhou L, Reynolds C, Lave J. Effects of Medicare Part D Coverage Gap on Medication and Medical Treatment Among Elderly Beneficiaries with Depression. Archives of General Psychiatry. 2011 doi: 10.1001/archgenpsychiatry.2011.1402. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leslie S, Thiebaud P. Using propensity scores to adjust for treatment selection bias. Proceedings of the SAS® Global Forum 2007 Conference; Cary, NC,. 2007. p. 184. [Google Scholar]
- 36.Centers for Medicare & Medicaid Services. Centers for Medicare & Medicaid Services Prescription Drug Hierarchical Condition Category (RxHCC) Model Software. Baltimore, MD, USA: 2010. [cited 2010 February 3]; Available from: http://www.cms.hhs.gov/MedicareAdvtgSpecRateStats/06_Risk_adjustment.asp. [Google Scholar]
- 37.Stürmer T, Joshi M, Glynn RJ, Avorn J, Rothman KJ, Schneeweiss S. A review of the application of propensity score methods yielded increasing use, advantages in specific settings, but not substantially different estimates compared with conventional multivariable methods. Journal of clinical epidemiology. 2006;59(5):437. e431–437. e424. [Google Scholar]
- 38.Zhang Y, Baik S, Zhou L, Lave J. The impact of Medicare Part D coverage gap on medication use and medical spending. International Health Economics Association (iHEA); Toronto, Canada: 2011. [Google Scholar]