Abstract
Male sexual behavior influences the rates of cervical dysplasia and invasive cervical cancer, as well as male human papillomavirus (HPV) infection and disease. Unfortunately, little is known regarding male HPV type distribution by age and across countries. In samples combined from the coronal sulcus, glans penis, shaft, and scrotum of 1,160 men from Brazil, Mexico, and the United States, overall HPV prevalence was 65.2%, with 12.0% oncogenic types only, 20.7% nononcogenic types only, 17.8% both oncogenic and nononcogenic, and 14.7% unclassified infections. Multiple HPV types were detected in 25.7% of study participants. HPV prevalence was higher in Brazil (72.3%) than in the United States (61.3%) and Mexico (61.9%). HPV16 (6.5%), HPV51 (5.3%), and HPV59 (5.3%) were the most commonly detected oncogenic infections, and HPV84 (7.7%), HPV62 (7.3%), and HPV6 (6.6%) were the most commonly detected nononcogenic infections. Overall HPV prevalence was not associated with age. However, significant associations with age were observed when specific categories of HPV, nononcogenic, and unclassified HPV infections were considered. Studies of HPV type distribution among a broad age range of men from multiple countries is needed to fill the information gap internationally with respect to our knowledge of HPV infection in men.
Introduction
Male human papillomavirus (HPV) infection significantly contributes to infection and subsequent cervical disease in women (1–4). Case-control studies of women with cervical cancer and their husbands have shown that men's sexual behavior affects women's risk of cervical neoplasia, even when controlling for female sexual activity (1–7). In areas with a high incidence of cervical cancer, men's sexual behavior is in itself a risk factor for cervical neoplasia (7). More recently, we have recognized that HPV contributes to men's burden of diseases such as anal, penile, and oropharyngeal cancers and genital warts (8). A growing interest in understanding HPV infection in men necessitates the characterization of these infections in terms of type distribution across countries. Unfortunately, there is a paucity of studies that can shed light on male HPV type distribution in any one country or across countries.
Few HPV studies have been conducted among heterosexual men, with only a subset reporting HPV type distribution and age-specific prevalence estimates (9). No studies to date have included a broad age range of men from multiple countries, which limits our ability to draw conclusions about differences in HPV type distribution among men. For example, observed differences in HPV type distribution in men may be due to differences in tissue tropism for particular HPV types due to anatomic site sampled. Alternatively, there may be due to differences in the populations studied, similar to what we understand for cervical HPV (10). This information is needed to inform future prevention efforts that may influence infection and disease reduction in men and consequently in women. The purpose of the current study was to assess HPV type distribution among men ages 18 years and older recruited from three different countries using a common protocol for sampling and HPV detection, and to evaluate whether HPV detection differs by age and country.
Materials and Methods
Men enrolled from March 2005 to December 2006 in the ongoing HPV in Men (HIM) Study were included in this analysis. Participants were recruited from São Paulo, Brazil; Cuernavaca, Mexico; Tampa, Florida; and its surrounding areas. To encourage compliance with follow-up, men received compensation or food or transportation reimbursement for their participation. Prior to study initiation, the Human Subjects Committees of the University of South Florida, the Centro de Referencia e Tratamento de Doencas Sexualmente Transmissiveis e AIDS, Brazil, and the National Institute of Public Health of Mexico approved all study procedures. All participants gave written informed consent.
Population
The study population consisted of men who met the following eligibility criteria: (a) ages 18 to 70 years; (b) residents of one of three sites—São Paulo, Brazil; the state of Morelos, Mexico; or southern Florida, United States; (c) reported no prior diagnosis of penile or anal cancers; (d) have never been diagnosed with genital or anal warts; (e) currently report no symptoms of a sexually transmitted infection or treatment for a sexually transmitted infection; (f) not participating in an HPV vaccine study; (g) no history of HIV or AIDS; (h) no history of imprisonment, homelessness, or drug treatment during the past 6 months; and (i) willing to comply with 10 scheduled visits every 6 months for 4 years with no plans to relocate within the next 4 years.
Men were recruited from three different population sources—the general population, universities, and organized health care systems (Mexico only)—to increase access to men with a broad range of ages, sexual behaviors, and HPV risk. In Brazil, men were recruited from the general population at a facility for urogenital care (Centro de Referencia e Tratamento de Doencas Sexualmente Transmissiveis e AIDS) and through general media advertising. Men presenting for non–sexually transmitted infection–related conditions were enrolled in the present study. In addition, the spouses and partners of women participating in a large cohort study of the natural history of HPV infection and risk of cervical neoplasia conducted in São Paulo since 1993 were also recruited.
At the Cuernavaca, Mexico site, the underlying population was comprised of employees and beneficiaries of the Instituto Mexicano de Seguro Social, factory employees, and officials of the Mexican army that are permanently assigned to this geographic area. In the United States, the underlying population was from the University of South Florida and the greater Tampa metropolitan area. Flyers and posters were distributed throughout the campus and community, and we administered monthly educational presentations. In addition, men from the broader Tampa Bay, FL community were recruited through the mail and media using brochures and flyers as well as advertisements in local and university papers.
Study Protocol
The HIM Study protocol includes a pre-enrollment run-in visit, a baseline (enrollment) visit, and nine additional visits after enrollment scheduled 6 months apart. For this analysis, the first 1,160 men who completed both the run-in and baseline visit were included.
Risk Factor Questionnaire
An extensive sexual history and health questionnaire given at enrollment assessed sociodemographic characteristics, sexual and contraceptive history, condom use practices, alcohol and tobacco use, and history of abnormal Pap smears in female partners. The questionnaire required ~20 min to complete and was self-administered using computer-assisted self-interviewing.
HPV Penile and Scrotal Sampling
To maximize sampling and prevent fraying of applicators, three different prewetted Dacron applicators were used to sample the external genitalia of the participants, and were later combined to form a single sample for the detection of HPV. This method has been previously shown to maximize HPV detection among men and to result in reproducible detection of genital HPV in men (11, 12). The study clinician at each site first swept 360 degrees around the coronal sulcus and then another 360 degrees around the glans penis and placed this swab into a separate collection vial with standard transport media labeled by anatomic site. A second wet swab was used to sample the entire skin surface of each of the quadrants of the shaft of the penis (left and right ventral, and left and right dorsal) and placed into a vial labeled “shaft.” A third Dacron swab moistened with normal saline was used for scrotum sampling and stored in 450 μL of the standard transport medium. Among uncircumcised men, the foreskin was sampled at the time of collection of the coronal sulcus/glans penis sample. All HPV samples were stored at −70°C until PCR analyses and genotyping were conducted. Prior to DNA extraction, the three samples of normal anogenital skin were combined to produce one DNA extract per participant clinic visit.
HPV Analyses
HPV testing of the combined DNA extract was conducted using PCR for amplification of a fragment of the HPV L1 gene (13). DNA extraction was done using the QIAamp DNA Mini Kit (Qiagen) according to the instructions of the manufacturer. Briefly, 200 μL aliquots of clinical material were digested with 20 μL of proteinase K solution for 1 h at 65°C, followed by 200 μL of lysis buffer.
Specimens were tested for the presence of HPV by amplifying 50 μL of the DNA extracts using the Linear Array HPV genotyping test following the instructions of the manufacturer (Roche Diagnostics). Samples were amplified using Perkin-Elmer GeneAmp PCR System 9700 as directed by the linear array protocol. HPV genotyping was conducted on all samples regardless of HPV PCR result (14). β-Globin was detected in 99.7% of samples tested (1,156 of 1,160). A total of 53 samples (4.6%) were PCR-negative but were genotype-positive upon hybridization. Samples that amplified HPV on PCR but did not hybridize with a specific HPV type upon genotyping were categorized as unclassified infections. Because it is unclear whether these were HPV infections or coamplifications of other genes, we report the prevalence of these products separately in the tables. The following 13 HPV types were categorized as oncogenic: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 66 (15). The other (nononcogenic) HPV types detected with the Linear Array methodology of Roche were 6, 11, 26, 40, 42, 44, 53, 54, 61, 62, 64, 67, 68, 69, 70, 71, 72, 73, 81, 82, 83, 84, IS39, and CP6108.
All unclassified samples were characterized by direct sequencing of a fragment of the L1 gene. Amplicons for sequencing were generated by nested PCR using the PGMY09/11 (13) and GP5/6+ primers (16) in a 50 μL reaction. In brief, 1 μL of DNA isolated from the biological specimen was first used in the PGMY09/11 reaction; these products were diluted 1:50 prior to use in the GP5/6+ reaction, with standard reagents and reaction conditions, except for the use of a lower concentration of GP5/6+ primers (0.1 μmol/L). After visualization of PCR products by gel electrophoresis, 1 μL of the nested PCR products of ~ 150 bp were submitted to sequencing using the GP6+ primer. Uncoupled dyes were eliminated from samples by ethanol precipitation prior to sequencing on an Applied Biosystems 3130×l Genetic Analyzer apparatus using the “BigDye Terminator v3.1 Sequencing Kit” according to the protocols of the manufacturer. Sequence identity was determined by comparison with the “BlastN database” of the National Center for Biotechnology Information, and those with scores greater than “e-15” were conclusively typed.
Statistical Analysis
A participant was considered positive for “any HPV” if he tested HPV-positive by PCR or by genotyping. The category of “any oncogenic type” included those who were positive for only oncogenic genotypes and those who were positive for both oncogenic and nononcogenic types. Only single or multiple infections with nononcogenic HPV types were classified as “any nononcogenic type.” Samples testing positive for HPV by PCR but negative for all of the 37 genotypes were labeled “unclassified.”
Differences in the distribution of demographic characteristics and HPV prevalence were explored by country and by age, and associations tested with Pearson's χ2 test. Participants were given the option of refusing to answer each of the questions on the web-based survey, and these refusals were treated as missing observations. Associations between types of HPV infections and country were evaluated using Pearson's χ2 test, and the raw P values were adjusted for multiple comparisons using the step-down Bonferroni approach (17). Differences in the distribution of HPV6, HPV11, HPV16, and HPV18 by country were evaluated using Fisher's exact test.
Results
A total of 1,160 men completing an enrollment visit (362 from Mexico, 382 from Brazil, and 416 from the United States) were included in this analysis. Forty-nine percent of participants were ages 18 to 29 years, 41.4% were ages 30 to 44 years, and 9.6% were ages 45 to 70 years (Table 1). The majority of study participants were non-white, with 33.0% reporting mixed race and 41.9% reporting Hispanic ethnicity. Approximately 45% of participants were either married or cohabiting, and 46.9% report being single or never married. The majority (53.1%) of participants had completed 13 or more years of education. Overall, 8.9% of participants reported never having had sexual intercourse with a female. The majority of men reported one to nine female sexual partners in his lifetime. Circumcision was common in the United States (83.2%) and rare in Mexico (14.1%) and Brazil (14.9%). Statistically significant differences were observed in the distribution of all study characteristics evaluated by country.
Table 1.
Sociodemographic characteristics of HIM Study participants by country
| Brazil (N = 382) |
Mexico (N = 362) |
United States (N = 416) |
Total (N = 1,160) |
|
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| Age | ||||
| 18–19 | 12 (3.1) | 15 (4.1) | 95 (22.8) | 122 (10.5) |
| 20–24 | 56 (14.7) | 51 (14.1) | 155 (37.3) | 262 (22.6) |
| 25–29 | 67 (17.5) | 75 (20.7) | 43 (10.3) | 185 (16.0) |
| 30–34 | 75 (19.6) | 69 (19.1) | 30 (7.2) | 174 (15.0) |
| 35–39 | 51 (13.4) | 66 (18.2) | 34 (8.2) | 151 (13.0) |
| 40–44 | 65 (17.0) | 64 (17.7) | 26 (6.3) | 155 (13.4) |
| 45–70 | 56 (14.7) | 22 (6.1) | 33 (7.9) | 111 (9.6) |
| Median | 34.0 | 32.9 | 23.1 | 30.0 |
| Race | ||||
| White | 229 (60.6) | 13 (3.6) | 303 (73.2) | 545 (47.3) |
| Black | 115 (30.4) | 1 (1.3) | 52 (12.6) | 168 (14.6) |
| Asian/Pacific Islander | 5 (1.4) | 0 (0.0) | 21 (5.1) | 26 (2.3) |
| American Indian | 22 (5.8) | 0 (0.0) | 0 (0.0) | 22 (1.9) |
| Mixed | 0 (0.0) | 343 (95.0) | 37 (8.9) | 380 (33.0) |
| Unknown | 7 (1.9) | 4 (1.1) | 1 (0.2) | 12 (1.0) |
| Ethnicity | ||||
| Hispanic | 66 (17.9) | 361 (100.0) | 52 (12.6) | 479 (41.9) |
| Non-Hispanic | 303 (82.1) | 0 (0.0) | 362 (87.4) | 665 (58.1) |
| Marital status | ||||
| Single, never married | 148 (39.3) | 91 (25.2) | 300 (72.8) | 539 (46.9) |
| Married | 118 (31.3) | 208 (57.6) | 61 (14.8) | 387 (33.6) |
| Cohabiting | 71 (18.8) | 45 (12.5) | 16 (3.9) | 132 (11.5) |
| Divorced/separated/widow | 40 (10.6) | 17 (4.7) | 35 (8.5) | 92 (8.0) |
| Education (y) | ||||
| Less than 12 | 122 (32.3) | 128 (35.6) | 6 (1.5) | 256 (22.3) |
| 12 | 144 (38.1) | 82 (22.8) | 58 (14.1) | 284 (24.7) |
| 13–16 | 102 (27.0) | 135 (37.5) | 310 (75.2) | 547 (47.6) |
| 17 or more | 10 (2.7) | 15 (4.2) | 38 (9.2) | 63 (5.5) |
| Lifetime no. of female partners | ||||
| None | 40 (11.9) | 27 (7.7) | 29 (7.3) | 96 (8.9) |
| 1 | 23 (6.9) | 22 (6.3) | 45 (11.3) | 90 (8.3) |
| 2–9 | 103 (30.8) | 214 (61.0) | 171 (42.9) | 488 (45.0) |
| 10–19 | 63 (18.8) | 46 (13.1) | 66 (16.5) | 175 (16.1) |
| 20–49 | 80 (23.9) | 34 (9.7) | 61 (15.3) | 175 (16.1) |
| 50–1,000 | 26 (7.8) | 8 (2.3) | 27 (6.8) | 61 (5.6) |
| Circumcised | 57 (14.9) | 51 (14.1) | 346 (83.2) | 454 (39.1) |
NOTE: Distribution of all variables examined differed significantly by country (P < 0.0001).
Table 2 presents HPV prevalence by country for oncogenic, nononcogenic, unclassified, and multiple infections, and compares prevalence across countries. Overall HPV prevalence in the study population was 65.2%. Twelve percent of infections were with oncogenic HPV types only, 20.7% with nononcogenic HPV types only, 17.8% were mixed oncogenic and nononcogenic, and 14.7% were with unclassified HPV infections only. Multiple HPV types were detected in 25.7% of study participants. The prevalence of any HPV infection was highest in Brazil (72.3%) and lowest in the United States (61.3%) and Mexico (61.9%; P = 0.03). A similar trend in prevalence across countries was observed for oncogenic HPV (P = 0.002), nononcogenic HPV (P < 0.0001), and multiple HPV infections (P < 0.0001). Unclassified infections were highest in the United States (20.0%), with lower prevalence observed in Mexico (13.5%) and Brazil (10.0%; P = 0.002).
Table 2.
Summary results for grouped HPV type distribution by country at enrollment
| Brazil (N = 382) |
Mexico (N = 362) |
United States (N = 416) |
Total (N = 1,160) |
Adjusted P* | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | ||
| Any HPV type | 276 (72.3) | 224 (61.9) | 255 (61.3) | 755 (65.1) | 0.03 |
| Any oncogenic type | 138 (36.1) | 110 (30.4) | 97 (23.3) | 345 (29.7) | 0.002 |
| Oncogenic type(s) only† | 45 (11.8) | 48 (13.3) | 46 (11.1) | 139 (12.0) | 0.6 |
| Any nononcogenic type | 193 (50.5) | 127 (35.1) | 126 (30.3) | 446 (38.5) | <0.0001 |
| Nononcogenic type(s) only† | 100 (26.2) | 65 (18.0) | 75 (18.0) | 240 (20.7) | 0.02 |
| Oncogenic and nononcogenic† | 93 (24.4) | 62 (17.1) | 51 (12.3) | 206 (17.8) | <0.0001 |
| Unclassified type(s) only†,‡ | 38 (10.0) | 49 (13.5) | 83 (20.0) | 170 (14.7) | 0.002 |
| PCR−/genotype+ | 22 (5.8) | 18 (5.0) | 13 (3.1) | 53 (4.6) | 0.200 |
| Multiple types | 138 (36.2) | 86 (23.8) | 74 (17.8) | 298 (25.7) | <0.0001 |
Adjusted by Holm's method: step-down Bonferroni approach (17).
The n and percentage in these four rows sum to the top row (categories are complete and mutually exclusive).
Samples were HPV-positive by PCR but not by genotyping.
Results from sequencing “unclassified infection” specimens showed that most unclassified infections probably represent spurious PCR products. We were able to reamplify, with a nested PCR protocol aiming a smaller PCR fragment (150 bp), only 60 of the 204 specimens, and were able to generate readable sequences from 41 of these. Of those specimens that generated readable sequences, 41.2% contained cutaneous HPV types (HPV types 2, 3, 12, 17, 22, 23, 62, 69, 74, 87, 91, and 107), 39% had very low copy number anogenital types (HPV types 6, 33, 39, 42, 44, 52, 56, 59, and 84), and 1% contained novel HPV types.
Across the three international populations, HPV16 (6.5%), HPV51 (5.3%), and HPV59 (5.3%) were the most commonly detected oncogenic infections, followed by HPV66 (5.0%), HPV39 (3.6%), and HPV52 (3.5%; Table 3). Among the nononcogenic infections, HPV84 was most commonly detected (7.7%), followed by HPV62 (7.3%), HPV6 (6.6%), and CP6108 (5.7%). HPV type distribution varied across countries. For example, in Brazil and in the United States, HPV16 was the most common oncogenic infection detected, whereas in Mexico, HPV59 was the most common HPV type. Among the nononcogenic infections, HPV62 was the most commonly detected in Brazil, and HPV84 was the most commonly detected HPV type in Mexico and the United States. Prevalence of the current prophylactic HPV vaccine types were 5.5% to 7.1% for HPV16, 0.5% to 3.1% for HPV18, 4.1% to 9.4% for HPV6, and 0.0% to 2.9% for HPV11. Significant differences in the prevalence of HPV6, HPV11, and HPV18 were observed by country, with Brazil having the highest prevalence of these infections (all P < 0.01).
Table 3.
Type-specific HPV infection distribution by country at enrollment
| Brazil (N = 382) |
Mexico (N = 362) |
United States (N = 416) |
Total (N = 1,160) |
|
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| Oncogenic types | ||||
| 16 | 27 (7.1) | 20 (5.5) | 28 (6.7) | 75 (6.5) |
| 18* | 12 (3.1) | 6 (1.7) | 2 (0.5) | 20 (1.7) |
| 31 | 7 (4.2) | 5 (1.4) | 2 (0.5) | 14 (1.2) |
| 33 | 1 (0.6) | 1 (0.3) | 0 (0.0) | 2 (0.2) |
| 35 | 13 (3.4) | 3 (0.8) | 5 (1.2) | 21 (1.8) |
| 39 | 12 (3.1) | 18 (5.0) | 12 (2.9) | 42 (3.6) |
| 45 | 11 (2.9) | 1 (0.3) | 1 (0.2) | 13 (1.1) |
| 51 | 11 (2.9) | 24 (6.6) | 26 (6.3) | 61 (5.3) |
| 52 | 15 (3.9) | 13 (3.6) | 13 (3.1) | 41 (3.5) |
| 56 | 12 (3.1) | 7 (1.9) | 5 (1.2) | 24 (2.1) |
| 58 | 15 (3.9) | 7 (1.9) | 5 (1.2) | 27 (2.3) |
| 59 | 19 (5.0) | 26 (7.2) | 17 (4.1) | 61 (5.3) |
| 66 | 25 (6.5) | 15 (4.1) | 18 (4.3) | 58 (5.0) |
| Nononcogenic types | ||||
| 6* | 36 (9.4) | 15 (4.1) | 26 (6.3) | 77 (6.6) |
| 11* | 11 (2.9) | 6 (1.7) | 0 (0.0) | 17 (1.5) |
| 26 | 3 (0.8) | 0 (0.0) | 1 (0.2) | 4 (0.3) |
| 40 | 6 (1.6) | 4 (1.1) | 5 (1.2) | 15 (1.3) |
| 42 | 7 (1.8) | 3 (0.8) | 4 (1.0) | 14 (1.2) |
| 44 | 10 (2.6) | 7 (1.9) | 6 (1.4) | 23 (2.0) |
| 53 | 29 (7.6) | 8 (2.2) | 19 (4.6) | 56 (4.8) |
| 54 | 12 (3.1) | 11 (3.0) | 8 (1.9) | 31 (2.7) |
| 61 | 35 (9.2) | 16 (4.4) | 8 (1.9) | 59 (5.1) |
| 62 | 41 (10.7) | 20 (5.5) | 24 (5.8) | 85 (7.3) |
| 64 | 0 (0.0) | 1 (0.3) | 0 (0.0) | 1 (0.1) |
| 67 | 2 (0.5) | 1 (0.3) | 1 (0.2) | 4 (0.3) |
| 68 | 10 (2.6) | 12 (3.3) | 9 (2.2) | 31 (2.7) |
| 69 | 2 (0.5) | 0 (0.0) | 1 (0.2) | 3 (0.3) |
| 70 | 14 (3.7) | 7 (1.9) | 5 (1.2) | 26 (2.2) |
| 71 | 4 (1.1) | 9 (2.5) | 0 (0.0) | 13 (1.1) |
| 72 | 8 (2.1) | 3 (0.8) | 3 (0.7) | 14 (1.2) |
| 73 | 13 (3.4) | 2 (0.6) | 0 (0.0) | 15 (1.3) |
| 81 | 23 (6.0) | 13 (3.6) | 6 (1.4) | 42 (3.6) |
| 82 | 0 (0.0) | 2 (0.6) | 6 (1.4) | 8 (0.7) |
| 83 | 11 (2.9) | 12 (3.3) | 11 (2.6) | 34 (2.9) |
| 84 | 35 (9.2) | 24 (6.6) | 30 (7.2) | 89 (7.7) |
| CP6108 | 31 (8.1) | 16 (4.4) | 19 (4.6) | 66 (5.7) |
| IS39 | 3 (0.8) | 0 (0.0) | 2 (0.5) | 5 (0.4) |
NOTE: Due to infection with multiple HPV types, the percentages of infection exceed 100%.
HPV type distribution significantly different by region (P < 0.010).
Table 4 presents the prevalence of vaccine-related HPV6, HPV11, HPV16, and HPV18 by country. The prevalence of any single HPV vaccine type alone was low at 2.5% for HPV16, 0.9% for HPV18, and 2.8% for HPV6/HPV11. Approximately 20% of men included in the study had an infection with one or more HPV vaccine types, with significant differences observed across countries. No study participant had an infection with all four HPV vaccine types.
Table 4.
Prevalence of vaccine-related HPV6, HPV11, HPV16, and HPV18 by country
| Brazil (N = 382) |
Mexico (N = 362) |
United States (N = 416) |
Total (N = 1,160) |
|
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| HPV16 only | 14 (3.7) | 7 (1.9) | 8 (1.9) | 29 (2.5) |
| HPV16 + other types | 27 (7.1) | 20 (5.5) | 28 (6.7) | 75 (4.5) |
| HPV18 only* | 9 (2.4) | 0 (0) | 1 (0.2) | 10 (0.9) |
| HPV18 + other types* | 12 (3.1) | 6 (1.7) | 2 (0.5) | 20 (1.7) |
| HPV16 and/or HPV18 only* | 27 (7.1) | 16 (4.4) | 13 (3.1) | 56 (4.8) |
| HPV18 and/or HPV18 + other types | 39 (10.2) | 24 (6.6) | 29 (7.0) | 92 (7.9) |
| HPV6 and/or HPV11 only | 15 (3.9) | 9 (2.5) | 9 (2.2) | 33 (2.8) |
| HPV6 and/or HPV11 + other types* | 44 (11.5) | 20 (5.5) | 26 (6.3) | 90 (7.8) |
| HPV6 and/or HPV11 and/or HPV16 and/or HPV18* | 77 (20.2) | 41 (11.3) | 52 (12.5) | 170 (14.7) |
| HPV6 and HPV11, and HPV16 and HPV18 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
NOTE: Due to infection with multiple HPV types, the percentages of infection exceed 100%.
HPV type distribution significantly different by region (P < 0.010).
No significant differences in overall HPV prevalence were observed by age, regardless of country examined (Table 5). Similarly, there was no clear association with age when unclassified HPV infections were eliminated from the analysis. However, when men ages 18 to 19 years old were compared with all other age groups, prevalence estimates were significantly lower among the younger men (27.9% versus 50.4%; data not shown).
Table 5.
Age-specific prevalence of any HPV type by country at enrollment
| Age | Brazil (N = 382) |
Mexico (N = 362) |
United States (N = 416) |
Total (N = 1,160) |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| 18–19 | 10 (83.3) | 9 (60.0) | 49 (51.6) | 68 (55.7) |
| 20–24 | 44 (78.6) | 30 (58.8) | 95 (61.3) | 169 (64.5) |
| 25–29 | 47 (70.2) | 46 (61.3) | 30 (69.8) | 123 (66.5) |
| 30–34 | 55 (73.3) | 47 (68.1) | 22 (73.3) | 124 (71.3) |
| 35–39 | 38 (74.5) | 36 (54.6) | 22 (64.7) | 96 (63.6) |
| 40–44 | 46 (70.8) | 44 (68.8) | 17 (65.4) | 107 (69.0) |
| 45–70 | 36 (64.3) | 12 (54.6) | 20 (60.6) | 68 (61.3) |
| P | 0.7 | 0.6 | 0.3 | 0.1 |
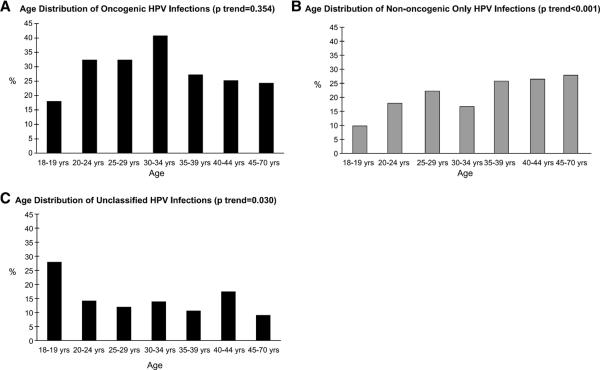
When HPV infections were grouped by oncogenic potential and examined by age across the three countries combined, we did not observe a significant association between age and oncogenic HPV infections (Fig. 1). Nononcogenic infections significantly increased with age with a low prevalence of 9.8% among 18- to 19-year-olds and a peak prevalence of 27.9% among men ages 45 to 70 years (P < 0.001). Unclassified infections significantly decreased with age (P = 0.030).
Figure 1.
HPV prevalence at enrollment by age: A, any oncogenic HPV infection; B, nononcogenic HPV infection only; C, unclassified infections.
Discussion
In this article, we present HPV type distribution by country and associations with HPV infections and age. A common protocol was used in clinics in the United States, Mexico, and Brazil, allowing for direct comparisons of HPV prevalence. This is the first international comparison of HPV type distribution across 37 genotypes in a general population of men. Among men enrolled in the HIM Study, overall HPV prevalence based on genotyping was 50.5%, with 62.3% in Brazil, 48.4% in Mexico, and 41.3% in the United States. Approximately 15% of men were positive for unclassified HPV types, defined as samples positive by PCR but negative based on genotyping by hybridization against 37 individual HPV types. These genotype prevalence estimates were higher than previously reported in men (9). This may be a result of more complete genital sampling in men than previously conducted, along with the application of a more sensitive HPV detection methodology with genotyping of 37 different HPV types (18). Due to these differences, as well as inconsistencies in the HPV types considered oncogenic (13 or more HPV types) in previous publications, it is difficult to make direct comparisons of HPV prevalence across studies. This problem is accentuated when examining infection with any HPV and grouped infections such as oncogenic or nononcogenic HPV prevalence.
Prophylactic HPV6 and HPV11 (nononcogenic) and HPV16 and HPV18 (oncogenic) vaccine types were detected in 14.7% of participants; whereas HPV6 was detected in 6.6%, HPV11 in 1.5%, HPV16 in 6.5%, and HPV18 in 1.7% of HIM Study participants. Significant differences in the prevalence of vaccine-related HPV infections were observed by country for HPV6, HPV11, and HPV18, although there was no significant difference in the prevalence of HPV16. This trend mirrored the observed overall HPV prevalence differences by country: Brazil had the highest prevalence overall as well as for individual vaccine-related HPV types.
To our knowledge, only two prior studies examined HPV prevalence among men in Brazil. One study was a small cross-sectional study (19), and in the other, all men were husbands of wives enrolled in a cervical cancer case-control study (20). Among husbands of controls, HPV prevalence was ~40%, and ~16% were HPV16-positive. The overall HPV prevalence estimates in that study were lower than the Brazil arm of the HIM Study (72.3%), although the HPV16 prevalence detected was higher than in the Brazil cohort (7.1%).
Three previous studies estimated HPV prevalence among men residing in Mexico. Excluding unclassified infections, prevalence estimates were 44.6% (21) and 42.7% (22) in each of the first two studies, and were similar to those observed in the Mexican arm of the HIM Study. In the third study, conducted among men attending vasectomy clinics nationally, the prevalence estimate was considerably lower, at 8.7% (23). Prevalence of any oncogenic HPV infection (14 HPV types) in the cross-sectional study of students and factory workers was 19.8%, a value lower than the 30.4% observed in the current study (22). Prevalence of type-specific infection was not reported in this study. Interestingly, among Mexican military men enrolled in a prospective study (21), the prevalence of any oncogenic infection at baseline was 34.8% (16 HPV types). The prevalence of HPV6, HPV11, HPV16, and HPV18 was 4.3%, 3.4%, 6.0%, and 3.7%, respectively, values similar to those observed among Mexican men in the HIM Study.
Four HPV studies among men from the United States have been published to date, with a reported range in HPV prevalence of 28.2% (in which limited sampling and genotyping was conducted) to 42% to 45.5% (18, 24, 25, 26). The latter studies from the United States included men residing in Hawaii (24), Seattle (25), and Arizona (18), and used sampling and genotyping methods similar to those reported in the current study. Among community men residing in Arizona and Florida who were sampled at both external genital sites and anal canal, HPV prevalence was 51.2%, whereas another 14.3% were infected with unclassified infections (18). The prevalences of HPV6, HPV11, HPV16, and HPV18 were 4.8%, 0.4%, 11.4%, 1.9%, respectively. In a small cross-sectional study conducted in Hawaii, ~2.5%, 1.5%, 6.5%, and 3.0% were positive for HPV6, HPV11, HPV16, and HPV18, respectively, values similar to those reported in the HIM Study (24). Collectively, it seems that HPV infection in men is common and consistently high among men in different regions of the United States and the Americas. HPV type distribution seems to vary by population included within countries as well as across countries.
We observed a relatively high proportion of unclassified infections (10–20%) in the HIM Study cohort, similar to other reports (18, 22, 27, 28). Using the Linear Array HPV genotyping test in this study, we were able to detect 37 HPV types. However, due to the large number of HPV types that infect the human epithelium, this assay is unable to characterize a portion (14.7% in this study) of the infections detected on PCR. We recently reported a similar prevalence of unclassified HPV infections detected in the external genital epithelium of men from the United States (18). Likewise, among studies that have tested for at least 20 HPV types in male genital skin, the range of unclassified HPV types reported is between 1.8% and 11.6% (6, 22, 26–28).
The significance of the unclassified infections is not known. This may represent infection with HPV types other than the 37 that are included in the linear array assay of Roche, or this may represent nonspecific amplification of gene sequences that are not HPV-related. As HPV type distribution seems to differ in men compared with women, it is important to characterize the HPV types that comprise this “unclassified” group. Results from direct sequencing of the gene products of PCR of the specimens included in this study indicate the presence of HPV2, HPV3, HPV12, HPV17, HPV22, HPV23, HPV74, HPV87, HPV91, and HPV107—types not currently included in the linear array assay. Bleeker and colleagues (27), sequenced “unclassified” specimens and found six additional HPV types (HPV3, HPV10, HPV32, HPV34, HPV86, and jc9710) that are not included in the linear array assay, accounting for between 0.8% and 3.8% of the HPV-positive results. Studies of anal HPV infection among men who have sex with men have also reported the presence of HPV types that are not included in the linear array genotyping detection system used in the current study. These types include HPV2, HPV13, HPV34, HPV57 (29), along with Pap155, Pap291, and AE2 (30). Understanding the significance of these HPV types requires additional study.
Overall, the prevalence of any HPV among men enrolled in the HIM Study was not associated with age. However, differing patterns of age association were observed depending on the category of HPV infection assessed. For example, a linear increase in nononcogenic infections with age was observed, a bimodal distribution with age was observed for oncogenic infections such that the younger and older males had the lowest prevalence of HPV. In contrast to these two patterns, a significant linear decrease in unclassified infections was observed with age. This may reflect a higher prevalence of low-level infections in younger men. Among men participating in a small cross-sectional study in Mexico, HPV prevalence was lower in the youngest age group (<20 years); however, these differences did not reach statistical significance (22). In contrast to this, risk of HPV acquisition seemed to be higher in the younger age group in a small prospective study conducted in Mexico (21). Among studies conducted in the United States, no association with age was observed (18, 26). Although in a cross-sectional study conducted in Denmark, an inverse association with age was observed (31). These data illustrate the complexity of HPV infection in men and highlight the need for prospective data that can distinguish differences in incidence and duration of infection by age in men.
As with any study, there are limitations that influence the interpretation of results. By recruiting men from a variety of sources in the community, we have attempted to enroll a representative population of men for study. However, this approach somewhat limits the comparability of the three study populations. The use of a common protocol for defining eligibility and assessing HPV status has minimized potential differences across study populations. Due to sample size limitations and differences in the age distribution of enrolled men by country, we did not examine age-specific HPV prevalence trends by country. As with any study, men who are interested and committed actually enrolled in the study, reducing the generalizability of the study findings. In addition, recruitment of study participants occurred in only one metropolitan area per country. Therefore, the results do not represent the country as a whole. Study entry criteria that excluded men with active sexually transmitted infections were intended to decrease the likelihood of overestimating HPV prevalence. However, men who were interested in study participation may have had a sexual partner with HPV-related lesions, therefore increasing their interest and likelihood of participation in the study. This may have increased the observed HPV prevalence.
In conclusion, we observed a high prevalence of HPV infections in men across the three countries evaluated (Brazil, Mexico, and the United States). Differences in overall HPV prevalence and type-specific prevalence between countries were observed. The relationship between age and HPV prevalence in men enrolled in the HIM Study varies by type of infection examined. Studies of HPV type distribution in other regions of the world, using rigorous methods of sampling and sample analyses, are needed to further clarify HPV type distribution and age differences among men.
Acknowledgments
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
We thank the following staff for their dedication in recruiting, examining, and maintaining cohort participants, as well conducting HPV DNA laboratory analyses: Kathy Eyring (CCRP), Christine Gage (ARNP), Kayoko Kay, Pauline Schwalm-Andel, Rana Zaki (MPH), Sireesha Banduvula (MS), Kyle Wolf, Danelle Smith (MS), Steven McAnany, Shannon McCarthy, and the Tissue Core staff of the Moffitt Cancer Center for their help in managing biological samples from the United States site; B. Fietzek, E. Brito, F. Cernicchiaro, F. Silva, G. Ribeiro, J. Antunes, L. Galan, R. Bocalon, R. Hessel, R. Matsuo, R. Otero, R. Terreri, S. Araujo, V. Relvas, and V. Souza from the Brazil site; A. Cruz, P. Hernández, A. Rodríguez-Cid, G. Alvarez, O. Rojas, D.A. Salazar, N. Herrera, A. Rodríguez, R. Alvear, A.L. Landa, and P. Román from the Mexico site.
The authors thank the Digene Corporation for kindly providing standard transport medium for the collection and storage of samples at no charge to the study.
Grant support: National Cancer Institute, NIH, CA no. RO1CA098803. National Cancer Institute grant R25 CA078447 (C.M. Nielson). Publication and report contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCI/NIH.
Footnotes
Disclosure of Potential Conflicts of Interest A. Giuliano receives consultant fees and honoraria from Merck and Co. The other authors disclosed no potential conflicts of interest.
References
- 1.Agarwal SS, Sehgal A, Sardana S, Kumar A, Luthra UK. Role of male behavior in cervical carcinogenesis among women with one lifetime sexual partner. Cancer. 1993;72:1666–9. doi: 10.1002/1097-0142(19930901)72:5<1666::aid-cncr2820720528>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 2.Buckley JD, Harris RW, Doll R, Vessey MP, Williams PT. Case-control study of the husbands of women with dysplasia or carcinoma of the cervix uteri. Lancet. 1981;2:1010–5. doi: 10.1016/s0140-6736(81)91215-0. [DOI] [PubMed] [Google Scholar]
- 3.Thomas DB, Ray RM, Pardthaisong T, et al. Prostitution, condom use, and invasive squamous cell cervical cancer in Thailand. Am J Epidemiol. 1996;143:779–86. doi: 10.1093/oxfordjournals.aje.a008815. [DOI] [PubMed] [Google Scholar]
- 4.Zunzunegui MV, King MC, Coria CF, Charlet J. Male influences on cervical cancer risk. Am J Epidemiol. 1986;123:302–7. doi: 10.1093/oxfordjournals.aje.a114238. [DOI] [PubMed] [Google Scholar]
- 5.Bosch FX, Castellsague X, Munoz N, et al. Male sexual behavior and human papillomavirus DNA: key risk factors for cervical cancer in Spain. J Natl Cancer Inst. 1996;88:1060–7. doi: 10.1093/jnci/88.15.1060. [DOI] [PubMed] [Google Scholar]
- 6.Castellsague X, Bosch FX, Munoz N, et al. Male circumcision, penile human papillomavirus infection, and cervical cancer in female partners. N Engl J Med. 2002;346:1105–12. doi: 10.1056/NEJMoa011688. [DOI] [PubMed] [Google Scholar]
- 7.Shah KV. Human papillomaviruses and anogenital cancers. N Engl J Med. 1997;337:1386–8. doi: 10.1056/NEJM199711063371911. [DOI] [PubMed] [Google Scholar]
- 8.Giuliano AR, Salmon D. The case for a gender neutral (universal) HPV vaccination policy in the US. Cancer Epidemiol Biomarkers Prev. 2008;17:805–8. doi: 10.1158/1055-9965.EPI-07-0741. [DOI] [PubMed] [Google Scholar]
- 9.Dunne EF, Nielson CM, Stone KM, Markowitz LE, Giuliano AR. Prevalence of HPV infection among men: a systematic review of the literature. J Infect Dis. 2006;194:1044–57. doi: 10.1086/507432. [DOI] [PubMed] [Google Scholar]
- 10.Clifford GM, Smith JS, Aguado T, Franceschi S. Comparison of HPV type distribution in high-grade cervical lesions and cervical cancer: a meta-analysis. Br J Cancer. 2003;89:101–5. doi: 10.1038/sj.bjc.6601024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flores R, Abalos TA, Nielson CM, Abrahamsen M, Harris RB, Giuliano AR. Reliability of sample collection and laboratory testing for HPV detection in men. J Virol Methods. 2008;149:136–43. doi: 10.1016/j.jviromet.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 12.Giuliano AR, Nielson CM, Flores R, et al. The optimal anatomic sites for sampling heterosexual men for human papillomavirus (HPV) detection: the HPV detection in men study. J Infect Dis. 2007;196:1146–52. doi: 10.1086/521629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gravitt PE, Peyton CL, Alessi TQ, et al. Improved amplification of genital human papillomaviruses. J Clin Microbiol. 2000;38:357–61. doi: 10.1128/jcm.38.1.357-361.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gravitt PE, Peyton CL, Apple RJ, Wheeler CM. Genotyping of 27 human papillomavirus types by using L1 consensus PCR products by a single-hybridization, reverse line blot detection method. J Clin Microbiol. 1998;36:3020–7. doi: 10.1128/jcm.36.10.3020-3027.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cogliano V, Baan R, Straif K, et al. Carcinogenicity of human papillomaviruses. Lancet Oncol. 2005;6:204. doi: 10.1016/s1470-2045(05)70086-3. [DOI] [PubMed] [Google Scholar]
- 16.de Roda Husman AM, Walboomers JM, van den Brule AJ, Meijer CJ, Snijders PJ. The use of general primers GP5 and GP6 elongated at their 3′ ends with adjacent highly conserved sequences improves human papillomavirus detection by PCR. J Gen Virol. 1995;76:1057–62. doi: 10.1099/0022-1317-76-4-1057. [DOI] [PubMed] [Google Scholar]
- 17.Holm S. A simple sequentially rejective Bonferroni test procedure. Scand J Stat. 1979;6:65–70. [Google Scholar]
- 18.Nielson CM, Flores R, Harris RB, et al. Human papillomavirus prevalence and type distribution in male anogenital sites and semen. Cancer Epidemiol Biomarkers Prev. 2007;16:1107–14. doi: 10.1158/1055-9965.EPI-06-0997. [DOI] [PubMed] [Google Scholar]
- 19.Rombaldi RL, Serafini EP, Villa LL, et al. Infection with human papillomaviruses of sexual partners of women having cervical intraepithelial neoplasia. Braz J Med Biol Res. 2006;39:177–87. doi: 10.1590/s0100-879x2006000200003. E-pub 2006 Feb 2. [DOI] [PubMed] [Google Scholar]
- 20.Franceschi S, Castellsague X, Dal Maso L, et al. Prevalence and determinants of human papillomavirus genital infection in men. Br J Cancer. 2002;86:705–11. doi: 10.1038/sj.bjc.6600194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lajous M, Mueller N, Cruz-Valdez A, et al. Determinants of prevalence, acquisition, and persistence of human papillomavirus in healthy Mexican military men. Cancer Epidemiol Biomarkers Prev. 2005;14:1710–6. doi: 10.1158/1055-9965.EPI-04-0926. [DOI] [PubMed] [Google Scholar]
- 22.Lazcano-Ponce E, Herrero R, Munoz N, et al. High prevalence of human papillomavirus infection in Mexican males: comparative study of penile-urethral swabs and urine samples. Sex Transm Dis. 2001;28:277–80. doi: 10.1097/00007435-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Vaccarella S, Lazcano-Ponce E, Castro-Garduno JA, et al. Prevalence and determinants of human papillomavirus infection in men attending vasectomy clinics in Mexico. Int J Cancer. 2006;119:1934–9. doi: 10.1002/ijc.21992. [DOI] [PubMed] [Google Scholar]
- 24.Hernandez BY, McDuffie K, Goodman MT, et al. Comparison of physician- and self-collected genital specimens for detection of human papillomavirus in men. J Clin Microbiol. 2006;44:513–7. doi: 10.1128/JCM.44.2.513-517.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weaver BA, Feng Q, Holmes KK, et al. Evaluation of genital sites and sampling techniques for detection of human papillomavirus DNA in men. J Infect Dis. 2004;189:677–85. doi: 10.1086/381395. Epub 2004 Jan 29. [DOI] [PubMed] [Google Scholar]
- 26.Baldwin SB, Wallace D, Papenfuss MR, et al. Condom use and other factors affecting penile human papillomavirus detection in men attending a sexually transmitted disease clinic. Sex Transm Dis. 2004;31:601–7. doi: 10.1097/01.olq.0000140012.02703.10. [DOI] [PubMed] [Google Scholar]
- 27.Bleeker MC, Hogewoning CJ, Berkhof J, et al. Concordance of specific human papillomavirus types in sex partners is more prevalent than would be expected by chance and is associated with increased viral loads. Clin Infect Dis. 2005;41:612–20. doi: 10.1086/431978. E-pub 2005, Jul 25. [DOI] [PubMed] [Google Scholar]
- 28.Shin HR, Franceschi S, Vaccarella S, et al. Prevalence and determinants of genital infection with papillomavirus, in female and male university students in Busan, South Korea. J Infect Dis. 2004;190:468–76. doi: 10.1086/421279. Epub 2004 Jul 1. [DOI] [PubMed] [Google Scholar]
- 29.Palefsky JM, Holly EA, Ralston ML, Jay N. Prevalence and risk factors for human papillomavirus infection of the anal canal in human immunodeficiency virus (HIV)-positive and HIV-negative homosexual men. J Infect Dis. 1998;177:361–7. doi: 10.1086/514194. [DOI] [PubMed] [Google Scholar]
- 30.Piketty C, Darragh TM, Da Costa M, et al. High prevalence of anal human papillomavirus infection and anal cancer precursors among HIV-infected persons in the absence of anal intercourse. Ann Intern Med. 2003;138:453–9. doi: 10.7326/0003-4819-138-6-200303180-00008. [DOI] [PubMed] [Google Scholar]
- 31.Svare EI, Kjaer SK, Worm AM, et al. Risk factors for genital HPV DNA in men resemble those found in women: a study of male attendees at a Danish STD clinic. Sex Transm Infect. 2002;78:215–8. doi: 10.1136/sti.78.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]