Abstract
Oral healthcare providers are likely to encounter a number of sensitive oral/systemic health issues while interacting with patients. The purpose of the current study was to develop and evaluate a framework aimed at oral healthcare providers to engage in active secondary prevention of eating disorders (i.e., early detection of oral manifestations of disordered eating behaviors, patient approach and communication, patient-specific oral treatment, and referral to care) for patients presenting with signs of disordered eating behaviors. The EAT Framework was developed based on the Brief Motivational Interviewing (B-MI) conceptual framework and comprises three continuous steps: Evaluating, Assessing, and Treating. Using a group-randomized control design, 11 dental hygiene (DH) and 7 dental (D) classes from 8 institutions were randomized to either the intervention or control conditions. Both groups completed preand post-intervention assessments. Hierarchical linear models were conducted to measure the effects of the intervention while controlling for baseline levels. Statistically significant improvements from pre-to post-intervention were observed in the Intervention group compared with the Control group on knowledge of eating disorders and oral findings, skills-based knowledge, and self-efficacy (all p < .01). Effect sizes ranged from .57–.95. No statistically significant differences in outcomes were observed by type of student. Although the EAT Framework was developed as part of a larger study on secondary prevention of eating disorders, the procedures and skills presented can be applied to other sensitive oral/systemic health issues. Because the EAT Framework was developed by translating B-MI principles and procedures, the framework can be easily adopted as a non-confrontational method for patient communication.
Introduction
Effective communication between health care professionals and their patients is necessary for improved health care quality through patient-centered health information and services.1, 2 Healthy People 2020, the science-based 10-year health agenda for the United States (U.S.), includes the following Health Communication and Health Information Technology objective: Increase the proportion of persons who report that their health care provider: a) has satisfactory communication skills; b) always listened carefully to them; c) always explained things so they could understand them; d) always showed respect for what they had to say; e) always spent enough time with them.2 Nonetheless, health care professionals report difficulty communicating with patients especially when addressing sensitive health care issues.1, 3
Oral healthcare providers (i.e., dentists and dental hygienists) are likely to encounter a number of sensitive oral/systemic health issues4 while interacting with patients. Sensitive oral/systemic health issues may include: disordered eating behaviors5–15, tobacco use16–18, alcohol abuse19–21, methamphetamine use22, child/partner/elder abuse23–30, depression31, and other mental illness32–34. Successful treatment and/or management of the oral complications associated with these issues often depend upon the underlying causal factors being identified and addressed with the patient. Accordingly, the Commission on Dental Accreditation's standards for Dental and Dental Hygiene programs35 contain several patient communication and behavioral science competencies including: critical thinking and problem solving with emphasis on their use in the comprehensive care of patients; interpersonal and communication skills to function successfully in a multicultural work environment; the application of the fundamental principles of behavioral sciences as they pertain to patient-centered approaches for promoting, improving, and maintaining oral health; and, communicating and collaborating with other members of the oral health care team to facilitate the provision of health care. Moreover, the likelihood of identifying and addressing oral/systemic health issues may increase as a consequence of the newly developed Healthy People 2020 oral health objective: Increase the proportion of adults who receive preventive interventions in dental offices.2
Various programs and techniques have been implemented in oral health clinical and educational settings to teach these specific techniques for communicating regarding sensitive health care topics.36–38 Such health care topics include: tobacco cessation, dental caries prevention, cancer screenings and eating disorders.39, 40 Techniques used to teach oral healthcare providers how to approach these topics with their patients include: motivational interviewing; objective, structured clinical examination evaluation; and patient instructors.36, 40, 41
Although the greatest support for motivational interviewing (MI) is with alcohol and smoking interventions, MI has been used as a basis for interventions regarding physical activity, dietary change, eating disorders, diabetes management and treatment adherence44 in addition to behaviors related to oral health issues.45, 46 A meta-analysis of randomized controlled trials using MI revealed a significant effect for MI, with an equal effect on physiological and psychological health issues.49 Moreover, the same study revealed 65% of B-MI (15 minute patient/provider sessions) randomized controlled studies showed a positive effect on patient behavior change.49
Purpose of the Study
This study was part of a larger study aimed at increasing secondary prevention of eating disorders, a sensitive oral/systemic health issue, among oral health providers. The purpose of the current study was to develop and evaluate a framework aimed at oral healthcare providers to engage in active secondary prevention of eating disorders (i.e., early detection of oral manifestations of disordered eating behaviors, patient approach and communication, patient-specific oral treatment, and referral to care) for patients presenting with signs of disordered eating behaviors. The evaluation and analyses were designed to assess the extent that the EAT framework (described below), improved knowledge of eating disorders and oral findings (related to those disorders), secondary prevention skills, and self-efficacy among dental and dental hygiene students regarding early detection, patient communication, and patient-specific oral treatment.
Materials and Methods
Intervention Development
The EAT Framework is a theory-based framework that translates extensive formative research6–12, 42 into a combination of interactive text, graphics, and videos used to increase knowledge, skill and self-efficacy among dental and dental hygiene students on evaluation, patient communication, and patient-specific oral treatment when oral manifestations of disordered eating behaviors are evident and identified by the provider. The intervention was delivered via the Web and access was restricted to allow evaluation of the program by users given a specific log-in number.
Theoretical Framework
The EAT Framework was based on the brief motivational interviewing (B-MI) conceptual framework.43 Focusing on the patient's stage of readiness to change his/her health risk behavior(s), motivational interviewing (MI) is a client-centered approach to the management of health issues that are associated with behavior change.43 The process of MI activates a patient's motivation to change and treatment adherence (e.g., follow treatment plans, follow-through with treatment referrals, and participating in follow-up visits) via the following: core communication skills: a) asking where the patient want to go regarding their health; b) informing the patient about options and letting them determine what makes sense to them,; and c) listening and respecting what the patient wants to do with regard to their health.43 The five basic MI principles that establish collaborative patient relationships include: 1) express patient empathy pertaining to the health issue and associated behavior; 2) develop discrepancy between the patient's problem behavior and broader personal values; 3) avoid the “righting reflex” (i.e., I am the professional and I know best); 4) accept and work with patient resistance using reflective listening skills; and 5) build patient confidence to cope with barriers to change (e.g., focus on small achievable goals based on patient's stage of readiness).47, 48
One constraint of using MI in health care settings is the lack of time needed for implementation.43 Thus, B-MI is an adapted version of MI that is designed to be used in health care settings where providers have limited time with patients (e.g., dentist encounters during regular oral healthcare visits).44 Following the same five principles of MI, B-MI comprises a set of brief strategies and techniques that can be used to effectively communicate with patients on sensitive health issues and tailor the most appropriate treatment plan to the patient's current stage of readiness. Thus, the EAT framework was developed to be part of a multi-component intervention that include educational materials as well some non-MI interactions.
Intervention Content
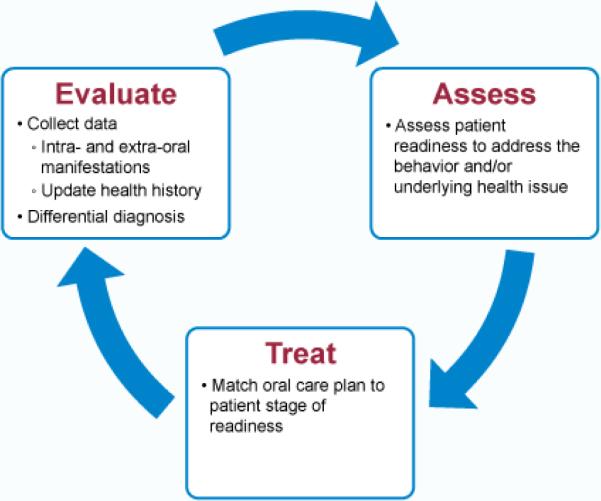
The EAT Framework (EVALUATE, ASSESS, TREAT) was developed based on the principles and strategies of B-MI. Generally speaking, the EAT skills are organized around three overarching and continuous steps including: Step 1) Evaluating patients presenting with oral signs of disordered eating behaviors; Step 2) Assessing patient readiness for managing disordered eating behaviors; and Step 3) providing Treatment strategies based upon patient's stage of readiness. Table 1 depicts B-MI principles and translation to EAT Framework steps. The intervention employs text screens, corresponding flowcharts, sample staging questions to ask patients at each step, and realistic video examples of OHPs demonstrating each of these steps. The EAT steps are illustrated in Figure 1 and described in detail below.
Table 1.
Translation of B-MI principles into EAT Framework components
| B-MI Principles | EAT Framework components | |
|---|---|---|
| Express empathy | Evaluate | Establish rapport |
| Collect data | ||
| Set agenda | ||
| Avoid righting reflex | Discuss etiology | |
| Discuss behaviors | ||
| Summarize outcome | ||
| Develop discrepancy | Assess | Assess patient readiness |
| Work with resistance | ||
| Setting small goals | Treat | Develop tailored treatment plan based on patient stage of readiness |
Figure 1.
Steps in the EAT Framework
The EVALUATE step focuses on how to evaluate patients presenting with signs of disordered eating behaviors through comprehensive data collection and differential diagnosis (i.e., determining if the oral finding may be caused by behaviors associated with disordered eating). These two phases of EVALUATE are further subdivided into specific sequential behaviors including: Establish Rapport, Collect Data, Set Agenda, Discuss Etiology, Discuss Behaviors, and Summarize Outcome—all with the objective of eliciting sensitive information from the patient without offending or breaching the patient's trust.
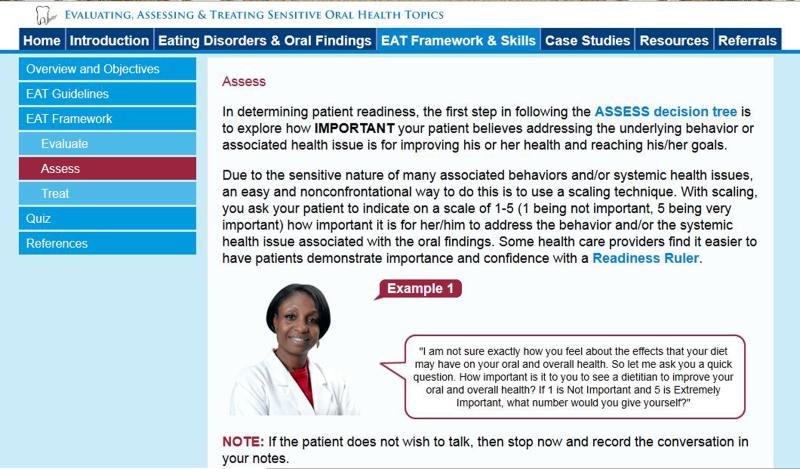
Building on the critical patient readiness aspect of brief motivational interviewing, the ASSESS step presents information that describes how oral health professionals can assess a patient's stage of readiness with regard to addressing the underlying behavior(s) associated with the oral findings (Figure 2). Skills include learning an easy and non-confrontational scaling method to assess how important it is for the patient to address the underlying cause of the oral findings and how confident the patient is in taking the appropriate next step(s).
Figure 2.
Example of the ASSESS section of the EAT Framework
Lastly, the TREAT step includes skills for delivery of patient-specific treatment plans tailored to a patient's stage of readiness, which was determined in the ASSESS step. Specific treatment plans are presented for patients determined to be at the Not Ready, Almost Ready, and Ready stages. In addition, there are treatment plans for patients currently seeking mental health treatment for their eating disorder, and patients who have relapsed to disordered eating behaviors. Each treatment plan is presented in a printer-friendly table with a patient profile, treatment options, and detailed instructions on how to provide patient-specific treatment. Video case studies demonstrate how to deliver a treatment plan that is well-suited to a patient's needs and is most likely to be followed by the patient at their stage of readiness. Printer-friendly handouts are also provided to give to patients, based on their stage of readiness.
Pilot Testing
The intervention web prototype was first reviewed by our expert panel of five members who represented the fields of eating disorders, curriculum development, dentistry, motivational interviewing, and dental hygiene. We requested that the expert panel members review the prototype and provide written feedback on the content, organizational structure, educational objectives, pedagogical activities, and design. Overall, feedback from our expert panel was positive. Suggestions for improvement included the following: a) reduce text and replace with graphics; b) create videos that model behavior with patients who are in “not ready” stage of readiness; and c) create videos that model communication with a patient under the age of 18 years and the patient's legal guardian.
The intervention prototype was also pilot tested with a convenience sample of dental and dental hygiene faculty at collaborating accredited dental schools and dental hygiene programs in the Eastern, Southeastern, Midwestern, and Pacific regions of the U.S. by using focus group methodology. Eight focus groups were implemented: three conducted with dental faculty and five conducted with dental hygiene faculty.
Prior to the focus groups, each participant was asked to log into the program and review the EAT Framework for content, interface, and pedagogical methods. Feedback from the pilot test identified the following themes regarding how the EAT Framework: a) can be used for other sensitive topics (e.g., smoking, intimate partner violence); b) can be included in a variety of didactic and clinic courses; c) provides simple organizational structure for differential diagnosis, communication and treatment skills; and e) encourages communication with all ancillary professionals. Representative quotes include the following:
“…even though you're gearing it towards a sensitive topic of eating disorders, it can also be applied to a lot of areas where you take those same skills and you use them again to deal with another topic that is very uncomfortable to address” (DH).
“…this EAT model I thought was a helpful way to sort of structure how and why to deal with this issue as a dental health services provider as opposed to—as a psychologist teaching dental students” (D).
“One of the things I like best [about the framework] is that it invites and encourages not just the health professional, but all the ancillary professionals to know what to look for” (D).
Suggestions for improvement that were identified during the focus group process included: a) links to resources used for tailoring treatment plans; and b) more graphics and visuals to make the steps more interesting and easier to follow.
Program revision
Feedback from the expert panel and faculty focus groups were triangulated and discussed by the research team. The intervention was then revised to address suggestions from the pilot study. Revisions included the following: a) inclusion of a diverse set of patients and providers to model behaviors; b) videos representing patients who are in the “Not Ready” stage; c) reduction of text and inclusion of graphics and “roll-overs”; d) inclusion of interactive audio sections to model communication skills.
Program Evaluation
Accredited dental schools and dental hygiene programs within institutions located in the Eastern, Southwestern, Midwestern, and Southern regions of the U.S. were recruited to participate in the evaluation. Using a group-randomized control design, 11 dental hygiene (DH) and 7 dental (D) classes were randomized to either the intervention (Intervention Condition; 7 DH and 5 D classes) or to instruction-as-usual (Control Condition; 4 DH and 2 D classes). Inclusion criteria: dental or dental hygiene student currently enrolled in one of the participating accredited dental or dental hygiene programs; 18 years of age or older. Exclusion criteria: not currently enrolled in one of the participating accredited dental or dental hygiene programs; under the age of 18.
Procedures
Contact faculty at participating dental and dental hygiene programs provided the investigators with the names of two courses within the program that would be included in the evaluation. Courses were stratified by dental and dental hygiene and by clinical exposure and then randomly assigned to the intervention or control condition. Upon random assignment by the investigators, course directors were provided with log-in information and code numbers for distribution to students enrolled in participating classes.
After providing online consent, all participants completed an online baseline assessment. Intervention participants were then provided with the educational module and were required to use the program on their own time and complete all components within 3 weeks. After three weeks, participants in both the intervention and control conditions were asked to complete the post-assessment. During the three week period, participants in the control condition received usual course content and no special instruction.
Measures
A web-based instrument, developed as part of the larger study, was employed to assess knowledge, behavioral skill, and self-efficacy regarding patient/provider communication using the three steps of the EAT Framework. Assessment of knowledge of eating disorders and oral findings included a composite score of 7 multiple choice questions. A representative sample of questions included the following (correct responses in parentheses):
-
■
Oral findings associated with disordered eating behaviors can be categorized as signs of…(dehydration, vomiting, malnutrition);
-
■
Which of the following is/are true about eating disorders…(Some individuals with eating disorders will die from complications of their disordered eating behaviors, Some individuals with eating disorders are male, some individuals with eating disorders are overweight);
-
■
Angular chelitis is an extra-oral finding that can be associated with the following disordered eating behavior(s) (Severe food restriction);
Correct responses were coded with a 1 and incorrect responses were coded with a 0. Responses were summed and ranged from 0–7 with larger composite scores indicating greater knowledge.
Assessment of behavioral skill included skills-based knowledge regarding the steps in the EAT Framework (10-item composite score). A sample of questions included the following (correct responses in parentheses):
-
■
Which of the following would be best when evaluating a patient who exhibits oral signs of disordered eating behaviors (Rule out the most common and/or least sensitive of the possible underlying causes first);
-
■
If a patient shows resistance when discussing a sensitive topic related to his/her oral findings it would be appropriate to…(Explain to the patient that knowing the underlying cause is important for determining the best possible care, but assure him/her that you will provide other treatment options in the meantime);
-
■
In order to provide the most effective care, a patient treatment plan should…(be tailored based on a patient's stage of readiness to address the underlying problem);
Correct responses were coded with a 1 and incorrect responses were coded with a 0. Responses were summed and ranged from 0–10 with larger composite scores indicating greater knowledge.
Perceived self-efficacy was assessed with 7-items on a 4-point Likert-type scale ranging from very confident to not at all confident (scale points ranging from 3–0 respectively). In the current study, the Cronbach's alpha for self-efficacy was .911, representing good internal reliability. A sample of representative behaviors included the following: recognizing oral findings associated with disordered eating behaviors; approaching a patient who presents with oral signs associated with disordered eating behaviors; prescribing patient-specific home-dental care instructions for patients with oral signs associated with disordered eating behaviors; and, assessing patient readiness to determine and/or address the underlying cause of the oral finding(s). Scores were summed to create a scale measure ranging from 0 to 21, with higher scores indicating higher self-efficacy. Socio-demographic and/or modifying factors included sex, race, age, dental or dental hygiene student, any prior clinical experience, previous course on eating disorders and oral findings, and year in academic training.
Data analysis
SPSS version 19.0 was used for initial analyses and HLM version 6.0 was used to perform multilevel linear modeling to account for the effects of cluster randomization. Descriptive analyses and bivariate comparisons of socio-demographic factors were conducted between intervention and control groups. Potential moderating effects of student characteristics, (e.g., sex, age, program of study, clinical experience, and having a previous course on disordered eating behaviors and oral health) were explored by including the moderator as a between-subjects factor and testing condition X moderator interaction terms. In addition, frequency distributions and descriptive statistics were calculated to examine the usability and satisfaction measures among the intervention participants.
Three hierarchical linear models (HLM), one for each of the outcome variables (i.e., self-efficacy, knowledge of eating disorders and oral findings, and skills-based knowledge), were conducted using restricted maximum likelihood estimation and the Newton-Raphson algorithm. The independent variables included a constant, the baseline measure for the respective outcome variable (grand-mean centered), and a group indicator. Because three models were tested, Bonferroni correction was applied to control the Type I error rate. Effect sizes are reported using a conservative Hedge's g statistic, which was calculated by dividing each respective intervention indicator coefficient (which represents the group mean difference adjusted for baseline) by the total pooled standard deviation at post-test. The total pooled standard deviation was computed by taking the square root of the sum of the squares for the between-student and within-student standard deviations that were both obtained from an unconditional HLM regression in which the dependent variable was the outcome at post-test and the independent variables included a constant and the intervention indicator.
Results
Among the students who completed the pre-test (n=384), 314 also completed the post-test for an 82% completion rate. Participants (n=314) included 182 students in the Intervention condition and 132 in the Control condition. No statistically significant differences were observed between the Intervention and Control participants with regard to sex, race, program of study (dental hygiene or dental), and year in the academic program. However, ethnic differences were observed with more Hispanic/Latino participants in the control condition (p = .005). Ethnic differences may have occurred because more control group classes were from the Southwestern U.S., whereas more classes in the Northwestern and Northeastern U.S. ended up being assigned to the intervention group. No statistically significant differences were observed with the following moderating variables: a) previous course in eating disorders; b) clinical exposure; and c) knowing someone with an eating disorder (Table 2).
Table 2.
Participant Demographic Characteristics
| Intervention Participants (n=182) |
Control Participants (n=132) |
||
|---|---|---|---|
| Characteristic | n(%) | n(%) | p-value* |
| Sex | |||
| Male | 60(33.0) | 37(28.0) | .350 |
| Female | 122(67.0) | 95(72.0) | |
| Ethnicity | |||
| Hispanic or Latino | 11(15.9) | 21(24.1) | .005* |
| Race | |||
| White | 134(73.6) | 89(67.4) | .232 |
| Black/African American | 4(2.2) | 2(1.5) | 1.00a |
| Asian | 32(17.6) | 24(18.2) | .891 |
| Native Hawaiian/Pacific Islander | 4(2.2) | 0 | .142a |
| American Indian/Alaska Native | 3(1.6) | 3(2.3) | .669a |
| Program of Study | |||
| Dental | 99(54.4) | 81(61.4) | .281 |
| Dental Hygiene | 83(45.6) | 51(38.6) | |
| Year in program | |||
| First | 89(49.2) | 63(47.7) | .801 |
| Second or more | 92(50.8) | 69(52.3) | |
| Previous course in eating disorders | |||
| Yes | 90(49.5) | 68(51.5) | .718 |
| No | 92(50.5) | 64(48.5) | |
| Currently or previously enrolled in a clinical practice course | |||
| Yes | 146(80.2) | 98(74.2) | .209 |
| No | 36(19.8) | 34(25.8) | |
| Know someone with an eating disorder | |||
| Yes | 117(64.3) | 75(56.8) | .180 |
| No | 65(35.7) | 57(43.2) |
Chi-Square Tests are significant at p<.05
Fishers Exact test was performed to due to small categorical sample
Table 3 depicts pre- and post-assessment means and standard deviations with regard to outcome measures. After adjusting for baseline levels, HLM regression results reveal statistically significant improvements among Intervention group participants from pre- to post-assessments as compared with Control group participants regarding the following outcome measures: knowledge of eating disorders and oral findings, skills-based knowledge, and self-efficacy (all p < .01). Effect sizes ranged from .57–.95 (Table 3).
Table 3.
Means and standard deviations for Intervention and Control group baseline and posttest outcome measures and effect sizes from HLM regression
| Control (n=132) |
Intervention (n=182) |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcome Measure | Scale range | Baseline M (SD) | Post M (SD) | M adj | Baseline M (SD) | Post M (SD) | M adj | p value* | Effect size (g) |
| Knowledge of eating disorders and oral findings | 0–7 | 3.61 (.913) | 3.95 (.868) | 3.96 | 3.69 (.832) | 4.58 (1.12) | 4.57 | <.001* | 0.57 |
| Skills-based Knowledge | 0–10 | 3.95 (1.61) | 5.16 (1.54) | 5.23 | 4.29 (1.41) | 6.79 (1.81) | 6.72 | <.001* | 0.95 |
| 16.2 | |||||||||
| Self-Efficacy | 0–21 | 13.40 (4.37) | 13.66 (4.13) | 13.23 | 11.64 (3.90) | 15.95 (3.29) | 7 | <.001* | 0.79 |
Madj = Posttest mean adjusted for baseline levels
Tests are significant at p<.01
With regard to the second research question, tests for interaction effects between Intervention group and type of student (dental versus dental hygiene) revealed no significant interactions (all p > .05). All other interactions that were tested were not significant either (p >.05).
Discussion
The purpose of the current study was to develop and evaluate the EAT Framework aimed at increasing the capacity among dental and dental hygiene students to communicate effectively with patients regarding secondary prevention of eating disorders. The results of our evaluation provide strong support for the efficacy of the EAT Framework with dental and dental hygiene students. Generally speaking, the intervention had a medium effect on knowledge and a large effect on skills-based knowledge, and self-efficacy with regard to Evaluating, Assessing, and Treating oral signs of disordered eating behaviors—a sensitive oral/systemic health issue. Moreover, based on the lack of statistically significant interactions, the effect of the intervention appeared to be consistent among both dental and dental hygiene students and was independent of whether or not they had prior clinical experience or a prior course on eating disorders and oral findings.
Although the EAT Framework was developed as part of a larger study on secondary prevention of eating disorders, this approach can be applied to other sensitive oral/systemic health issues. The EAT Framework was developed by translating B-MI principles and procedures, which facilitates easy adoption of the framework as a non-confrontational method for patient communication. Additionally, this web-based interactive training framework can be adopted into existing dental and dental hygiene didactic and clinical courses.
The ability of dentists and dental hygienists to communicate effectively with patients regarding sensitive oral/systemic health issues is critical for improving oral and overall health. There is a growing body of research indicating an association between oral health and overall health. Therefore, the ability of oral healthcare providers to identify connections, communicate findings, and tailor treatment programs is necessary to bridge the oral and physical health care divide. The EAT Framework, and delivery via the Web, may serve as a foundation for preventive intervention in dental offices—as outlined in a proposed Healthy People 2020 oral health objective.
Acknowledgements
This research was supported by the National Institute of Health Grant 1RC1DE020274-01. We would like to acknowledge the following colleges and universities that collaborated with us on the development and evaluation of this project: Virginia Commonwealth University's Departments of Dentistry and Dental Hygiene; Armstrong Atlantic State University's Department of Dental Hygiene; Hillsborough Community College Department of Dental Hygiene; University of Florida Department of Dentistry; University of Illinois Department of Dentistry; Kennedy King Community College Department of Dental Hygiene; University of Texas Health Science Center at San Antonio, Dental School and School of Health Professions; Oregon Health Sciences University Department of Dentistry; Lane Community College Department of Dental Hygiene.
This research was supported by the National Institute of Health Grant 1rc1de020274-01.
References
- 1.Tannen D, Wallat C. Medical professionals and parents: A linguistic analysis of communication across contexts. Language in Society. 1986;15(3):295–311. [Google Scholar]
- 2.U.S. Department of Health and Human Services. 2011 doi: 10.3109/15360288.2015.1037530. Healthy People.gov: http://www.healthypeople.gov/2020/default.aspx. [DOI] [PubMed]
- 3.Yoshida T, Milgrom P, Coldwell S. How do U.S. and Canadian Dental Schools Teach Interpersonal Communication Skills? Journal of Dental Education. 2002;66(11):1281–88. [PubMed] [Google Scholar]
- 4.Kidd E, Smith B. Toothwear histories: a sensitive issue. Dental Update. 1989;20:174–78. [PubMed] [Google Scholar]
- 5.DeMoor R. Eating disorder-induced dental complications: a case report. Journal of Oral Rehabilitation. 2004;31:725–32. doi: 10.1111/j.1365-2842.2004.01282.x. [DOI] [PubMed] [Google Scholar]
- 6.DeBate R, Plichta S, Tedesco L, Kerschbaum W. Integration of Oral Health Care and Mental Health Services: Dental Hygienists' Readiness and Capacity for Secondary Prevention of Eating Disorders. Journal of Behavioral Health Services and Research. 2005 doi: 10.1007/s11414-005-9003-1. [DOI] [PubMed] [Google Scholar]
- 7.DeBate R, Plichta S, Tedesco L, Kerschbaum W. Assessing Readiness and Capacity for Secondary Prevention of Eating Disorders Among Dental Practitioners. Journl of Health Services & Research. 2006;33(1) doi: 10.1007/s11414-005-9003-1. [DOI] [PubMed] [Google Scholar]
- 8.DeBate R, Severson H, Zwald M, Shaw T, Christiansen S, Koerber A, et al. Development and evaluation of a web-based training program for oral health care providers on secondary prevention of eating disorders. Journal of Dental Education. 2010;73(6):718–29. [PMC free article] [PubMed] [Google Scholar]
- 9.DeBate R, Shuman D, Tedesco L. Eating Disorders in the Oral Health Dental Curriculum. Journal of Dental Education. 2007;71(5):655–63. [PubMed] [Google Scholar]
- 10.DeBate R, Tedesco L, Kerschbaum W. Oral Health Practitioners and Secondary Prevention of Eating Disorders: An Application of the Transtheoretical Model. Journal of Dental Hygiene. 2005;79(4):10–10(1). [Google Scholar]
- 11.DeBate R, Tedesco L, Kerschbaum W. Knowledge of Oral and Physical Manifestations of Anorexia Nervosa and Bulimia Nervosa Among Dentists and Dental Hygienists. Journnal of Dental Education. 2005;69:346–54. [PubMed] [Google Scholar]
- 12.DeBate R, Tedesco L, Kerschbaum W. Oral Health Providers and Secondary Prevention of Disordered Eating: An Application of the Transtheoretical Model. Journal of Dental Hygiene. 2005;79(4):1–10. [Google Scholar]
- 13.Gurenlian J. Eating Disorders. The Journal of Dental Hygiene. 2002;76(111):219–34. [PubMed] [Google Scholar]
- 14.Moor RD. Eating disorder-induced dental complications: a case report. Journal of Oral Rehabilitation. 2004;31:725–32. doi: 10.1111/j.1365-2842.2004.01282.x. [DOI] [PubMed] [Google Scholar]
- 15.Ohrn R, Angmar-Mansson B. Oral status of 35 subjects with eating disorders--A 1-year study. European Journal of Oral Sciences. 2000;108:275–80. doi: 10.1034/j.1600-0722.2000.108004275.x. [DOI] [PubMed] [Google Scholar]
- 16.Chambrone L, Chambrone D, Pustiglioni F, Chambrone L, Lima L. The influence of tobacco smoking on the outcomes achieved by root-coverage procedures: a systematic review. Journal of the American Dental Association. 2009;140(3):297–306. doi: 10.14219/jada.archive.2009.0158. [DOI] [PubMed] [Google Scholar]
- 17.Dolan T, McGorray S, Grinstead-Skigen C, Mecklenburg R. Tobacco control activities in US dental practices. Journal of the American Dental Association. 1997;128:1669–79. doi: 10.14219/jada.archive.1997.0129. [DOI] [PubMed] [Google Scholar]
- 18.Warnakulasuriya S. Effectiveness of tobacco counseling in the dental office. Journal of Dental Education. 2002;66(9):1079–86. [PubMed] [Google Scholar]
- 19.Friedlander A, Marder S, Pisegna J, Yagiela J. Alcohol abuse and dependence: psychopathology, medical management and dental implications. ournal of the American Dental Association. 2003;134(6):731–40. doi: 10.14219/jada.archive.2003.0260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kwasnicki A, Longman L, Wilkinson G. The significance of alcohol misuse in the dental patient. Dental Update. 2008;35(1):7–16. doi: 10.12968/denu.2008.35.1.7. [DOI] [PubMed] [Google Scholar]
- 21.Johnson D, Hearn A, Barker D. A pilot survey of dental health in a group of drug and alcohol abusers. The European Journal of Prosthodontics and Restorative Dentistry. 2008;16(4):181–84. [PubMed] [Google Scholar]
- 22.Hamamoto D, Rhodus N. Methamphetamine abuse and dentistry. Oral Diseases. 2009;15(1):27–37. doi: 10.1111/j.1601-0825.2008.01459.x. [DOI] [PubMed] [Google Scholar]
- 23.Cowen H, Cowen P. Elder mistreatment: dental assessment and intervention. Special Care in Dentistry: Official Publication of the American Association of Hospital Dentists, the Academy of Dentistry for the Handicapped, and the American Society for Geriatric Dentistry. 2002;22(1):23–32. doi: 10.1111/j.1754-4505.2002.tb01206.x. [DOI] [PubMed] [Google Scholar]
- 24.Gwinn C, McClane G, Shanel-Hogan K, Strack G. Domestic Violence: No Place for a Smile. Journal of the California Dental Association. 2004;32(5):399–409. [PubMed] [Google Scholar]
- 25.Hsieh N, Herzig K, Gansky S, Danley D, Gerbert B. Changing dentists' knowledge, attitudes, and behavior about domestic violence through an interactive multimedia tutorial. Journal of the American Dental Association. 2006;137(5):596–603. doi: 10.14219/jada.archive.2006.0254. [DOI] [PubMed] [Google Scholar]
- 26.Kenney J. Domestic violence: a complex health care issue for dentistry today. Forensic Science International. 2006;159(Suppl 1):S121–25. doi: 10.1016/j.forsciint.2006.02.025. [DOI] [PubMed] [Google Scholar]
- 27.Love C, Gerbert B, Caspers N, Bronstone A, Perry D, Bird W. Dentists' attitudes and behaviors regarding domestic violence: The need for an effective response. Journal of the American Dental Association. 2001;132:85–93. doi: 10.14219/jada.archive.2001.0032. [DOI] [PubMed] [Google Scholar]
- 28.Mehra V. Culturally Competent Responses for Identifying and Responding to Domestic Violence in Dental Care Settings. Journal of the California Dental Association. 2004;32:387–95. [PubMed] [Google Scholar]
- 29.Senn D, McDowell J, Alder M. Dentistry's role in the recognition and reporting of domestic violence, abuse, and neglect. Dental Clinics of North America. 2001;45(2):343–63. [PubMed] [Google Scholar]
- 30.Welbury R, Hobson R, Stephenson J, Jepson N. Evaluation of a computer-assisted learning programme on the oral-facial signs of child physical abuse (non-accidental injury) by general dental practitioners. British Dental Journal. 2001;190(12):668–70. doi: 10.1038/sj.bdj.4801070. [DOI] [PubMed] [Google Scholar]
- 31.Rosania A, Low K, McCormick C, Rosania D. Stress, depression, cortisol, and periodontal disease. Journal of Periodontology. 2009;80(2):260–66. doi: 10.1902/jop.2009.080334. [DOI] [PubMed] [Google Scholar]
- 32.Friedlander A, Friedlander I, Marder S. Bipolar I disorder: psychopathology, medical management and dental implications. Journal of the American Dental Association. 2002;133(9):1209–17. doi: 10.14219/jada.archive.2002.0362. [DOI] [PubMed] [Google Scholar]
- 33.Friedlander A, Friedlander I, Marder S. Posttraumatic stress disorder: psychopathology, medical management, and dental implications. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 2004;97(1):5–11. doi: 10.1016/j.tripleo.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 34.Clark D. Dental care for the patient with bipolar disorder. Journal of the Canadian Dental Association. 2003;69(1):20–24. [PubMed] [Google Scholar]
- 35.Commission on Dental Accreditation . Accreditation standards for dental education programs. Chicago: 2010. [Google Scholar]
- 36.Cannick G, Horowitz A, Garr D, Reed S, Neville B, Day T, et al. Use of of OSCE to Evaluate Brief Communication Skills Training for Dental Students. Journal of Dental Education. 2007;71(9):1203–09. [PMC free article] [PubMed] [Google Scholar]
- 37.Wagner J, Arteaga S, D'Ambrosio J, Hodge C, Loannidou E, Pfieffer C, et al. A Patient-Instructor Program to Promote Dental Students' Communication Skills with Diverse Patients. Journal of Dental Education. 2007;71(12):1554–60. [PubMed] [Google Scholar]
- 38.Wiltshire A, Ross M, Brimlow D. Empathic Communication Between Dental Professionals and Persons Living with HIV and AIDS. Journal of Dental Education. 2002;66(1) [PubMed] [Google Scholar]
- 39.Weinstein P, Harrison R, Benton T. Motivating mothers to prevent caries: Confirming the beneficial effect of counseling. JADA. 2006;137:789–93. doi: 10.14219/jada.archive.2006.0291. [DOI] [PubMed] [Google Scholar]
- 40.Coan L, Christen A, Romito L. Evolution of a Tobacco Cessation Curriculum for Dental Hygiene Students at Indiana University School of Dentistry. Journal of Dental Education. 2007;71(6):776–84. [PubMed] [Google Scholar]
- 41.Weinstein P, Harrison R, Benton T. Motivating parents to prevent caries in their young children: One-year findings. JADA. 2004;135(June):731–38. doi: 10.14219/jada.archive.2004.0299. [DOI] [PubMed] [Google Scholar]
- 42.DeBate R, Cragun D, Severson H, Shaw T, Christiansen S, Koerber A, et al. Exploring factors for increasing adoption of e-courses among dental and dental hygiene faculty. Journal of Dental Education. In press. [PMC free article] [PubMed] [Google Scholar]
- 43.Rollnick S, Mason P, Butler C. Motivational interviewing in health care: Helping patients change behavior. The Guilford Press; New York, NY: 2008. [Google Scholar]
- 44.Britt E, Hudson S, Blamied N. Motivational interviewing in health settings: A review. Patient Education and Counseling. 2004;53:147–55. doi: 10.1016/S0738-3991(03)00141-1. [DOI] [PubMed] [Google Scholar]
- 45.Koerber A, Crawford J, O'Connell K. The effects of teaching dental students brief motivational interviewing for smoking cessation counseling: A pilot study. Journal of Dental Education. 2003;67(4):439–47. [PubMed] [Google Scholar]
- 46.Weinstein P, Harrison R, Benton T. Motivating parents to prevent caries in their young children: One-year findings. Journal of the American Dental Association. 2004;135:731–38. doi: 10.14219/jada.archive.2004.0299. [DOI] [PubMed] [Google Scholar]
- 47.Burke B, Arkowitz A, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Counseling and Clinical Psychology. 2003;71(5):843–61. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- 48.Adamian M, Golin C, Shain L, DeVellis B. Brief motivational interviewing to improve adherence to antiretrovial therapy: Development and qualitative piolot assessment of an intervention. AIDS Patient Care and STDs. 2004;(18):229–38. doi: 10.1089/108729104323038900. [DOI] [PubMed] [Google Scholar]
- 49.Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational Interviewing: a systematic review and meta-analysis. The British Journal of General Practice. 2005;55(513):305–12. [PMC free article] [PubMed] [Google Scholar]