Abstract
Novel compliant floors aim to decrease the risk for fall-related injury by providing substantial force attenuation during the impact phase of falls. Certain models of compliant flooring have been shown to have limited influence on postural sway and successful completion of dynamic balance tasks. However, the effects of these products on balance recovery mechanisms following an externally induced perturbation have yet to be quantified.
We used a floor translation paradigm to induce a balance perturbation to thirteen elderly community-dwelling women. Outcome measures included the displacement rates and margins of safety for both the underfoot centre-of-pressure and whole-body centre-of-mass across two novel compliant floors (Smart-Cell, SofTile), two basic foam surfaces (Firm-Foam, Soft-Foam) and a standard ‘Rigid’ floor as a control condition.
The centre-of-mass and centre-of-pressure margins of safety, and all centre-of-mass displacement rates, were not significantly lower for the two novel compliant flooring systems compared to the control floor. The centre-of-pressure displacement rates were similar to the control floor for the SmartCell floor condition. The majority of the margin of safety and displacement rate variables for the foam floors were significantly lower than the control condition.
This study illustrates that the SmartCell and SofTile novel compliant floors have minimal influences on balance and balance control responses following externally induced perturbations in older community-dwelling women, and supports pilot installations of these floors to inform decisions regarding the development of clinical trials.
Keywords: Fall-related injuries, Falls, Centre of pressure, Injury prevention, Balance, Aging
1. Introduction
Fall-related injuries in older adults are a major public health issue in Canada. They represent the number one cause of injury-related hospitalizations and deaths for this population, with direct costs in excess of $2 billion annually (Smartrisk, 2009). Serious injuries such as hip fractures and traumatic brain injuries are caused by falls in up to 90% of cases (Grisso et al., 1991; Pickett et al., 2001), and the majority of fall-related injuries in the senior population occur in high-risk environments such as residential care facilities, seniors’ centres, and hospitals (Cameron et al., 2010). In light of North America’s demographic shift towards a more aged population (Health Canada, 2002), it is imperative that effective interventions be developed and implemented to reduce the frequency and severity of falls and fall-related injuries.
A promising intervention approach that is particularly relevant for high-risk settings is to decrease the stiffness of the floor to attenuate impact forces in the event of a fall (Casalena et al., 1998; Maki and Fernie, 1990; Laing et al., 2006; Laing and Robinovitch, 2009; Laforest et al., 2000; Nevitt and Cummings, 1993; Simpson et al., 2004; Healey, 1994). While the clinical effectiveness of intervention strategies such as exercise, pharmacological agents, and wearable hip protectors depend on active user compliance and adherence, novel compliant floors are a passive intervention approach that may protect against multiple types of fall-related injuries. However, evidence exists that some low stiffness surfaces could impair balance maintenance and balance recovery abilities, thereby increasing the risk of falls. Simple compliant foam surfaces have been postulated to impair balance by decreasing the quality of sensory inputs provided by the proprioceptive and pressure receptors in the ankle and foot (Betker et al., 2005, Lord and Menz, 2000; Ring et al., 1989), and by altering gait mechanics including decreased trunk stability and reduced toe clearance (Marigold and Patla, 2005; Maclellan and Patla, 2006). Thus, the challenge for this intervention approach is the design of floors that substantially attenuate impact force while minimizing potential impairments in balance and mobility.
Novel compliant flooring systems are generally designed to provide a dual-stiffness response characterized by minimal deflection during locomotion, and a transition to increased compliance at the higher loads associated with fall-related impacts. Such products have been shown to attenuate the peak force applied to the proximal femur by 25–50% during simulated sideways falls, in addition to having minimal effects on successful completion of static (quiet stance) and dynamic balance and mobility tasks (Timed Up and Go test, backwards floor translation) in older community-dwelling women (Laing and Robinovitch, 2009). However, no information currently exists on the influence of novel compliant floors on biomechanical variables associated with balance control responses following externally induced perturbations (i.e. the biomechanical variables to control balance recovery), despite the fact that evaluating balance recovery abilities is a critical component of a comprehensive balance assessment (Chiu et al., 2003).
From a biomechanical perspective, to maintain an upright posture during quiet stance the vertical projection of the whole-body centre-of-mass (COM) must fall within the limits of the base of support (BOS) (Winter, 2009). To accomplish this, models related to ankle stiffness (Winter et al., 1998; Winter et al., 2001) and reactive muscle strategies (Morasso and Schieppati, 1999; Morasso and Sanguineti, 2002) predict that adjustments in the location of the underfoot centre-of-pressure (COP) are used to guide or ‘shepherd’ the trajectory of the COM towards an equilibrium position. In the event of a balance perturbation that causes the COM to shift anteriorly (such as being nudged from behind), recovering balance without changing the BOS via stepping responses requires the COP to be rapidly shifted anteriorly towards the toes to decelerate the COM. If the COM trajectory cannot be altered quickly enough by the anterior COP displacement and consequently reaches the BOS boundaries, the individual must increase the BOS by taking a step in order to prevent a forward fall (Winter, 2009). Thus, the proximity of the COM to the BOS boundaries after perturbation (margin of safety (MOS)) provides an indication of the degree of instability following the perturbation. For elderly persons, a large MOS may be of increased importance in recovering balance due to age-related declines in strength, reaction time, and other sensori-motor capabilities. Underfoot compliance (as might be associated with a low stiffness floor) has the potential to impair balance recovery responses by decreasing effective ankle stiffness and the rate of COP displacement in response to changes in ankle torque. Consequently, changes in support surface stiffness may influence COP dynamics, which in turn could influence COM trajectories (Marigold and Patla, 2005; Maclellan and Patla, 2006). However, the interplay of COM and COP movements has never been examined in response to balance perturbations (i.e. during balance recovery responses) on novel compliant flooring systems.
Accordingly, our objectives in the current study were to determine the: (a) minimum margins of safety (MMOS) of the whole-body COM and underfoot COP, and (b) displacement rates of the COM and COP, across five different flooring conditions following an externally induced perturbation requiring balance recovery responses. We hypothesized that the novel dual-stiffness compliant flooring systems would have minimal influence on these outcomes, while excessive reductions in floor stiffness would lead to reduced margins of safety and displacement rates.
2. Materials and methods
2.1. Floor conditions
Five different flooring conditions were tested (Table 1) and have been described in detail previously (Laing and Robinovitch, 2009). Briefly, the ‘Rigid’ floor (used as a control condition) was a thin layer of dense engineered rubber appropriate for installation over concrete or wooden subfloors in institutional settings (Noraplan Classic, Nora Systems Inc, Lawrence, MA, USA). Two different novel compliant flooring systems were also tested. ‘SmartCell’ (SATech, Chehalis, WA, USA) was comprised of a continuous surface layer of synthetic rubber overlying an array of cylindrical rubber columns 14 mm in diameter, and spaced at 19 mm intervals. The ‘SofTile’ floor (SofSurfaces, Petrolia, ON, Canada) also utilized a buckling column approach, but had 50 mm diameter columns spaced at 70 mm intervals. Finally, two open-cell polyurethane foams (similar to those used in quiet stance sway (Lord and Menz, 2000; Teasdale et al., 1991; Gill et al., 2001) and gait tests (Marigold and Patla, 2005; Maclellan and Patla, 2006) were tested to provide a broad spectrum of floor stiffness conditions.
Table 1.
Photos and characteristics of the five floor conditions tested in this study. Footfall deflection values were estimated from force-deflection tests under a simulated 1000 N footfall using a rigid foot-shaped indenter mounted within a materials testing system (Laing and Robinovitch, 2009).
| Floor | Photo | Thickness (mm) | Footfall deflection (mm) | Density (kg/m3) |
|---|---|---|---|---|
| Rigid (Control) |
|
2 | – | – |
| SmartCell |

|
25 | 0.8 | 1120 |
| SofTile |

|
100 | 4.0 | 1057 |
| Firm-Foam |
|
110 | 85.4 | 32 |
| Soft-Foam |

|
100 | 92.4 | 22.2 |
2.2. Participants
Thirteen healthy community-dwelling women participated in this study, with ages ranging from 65 to 90 years (mean (SD) = 73.7 (7.9) years), body masses from 57.6 to 93.0 kg (mean (SD) = 70.3 (11.6) kg), heights from 1.51 to 1.76 m (mean (SD) = 1.62 (0.08) m), and body mass indices from 22.3 to 31.3 kg/m2 (mean (SD) = 26.7 (3.0) kg/m2). Exclusionary criteria were: (a) a history of falls within the preceding 6 months; (b) inability to independently stand for 60 s; or (c) inability to walk 10 m without aid. All participants provided written informed consent, and the study was approved by the Office of Research Ethics at the University of Waterloo and the Committee on Research Ethics at Simon Fraser University.
2.3. Perturbation protocol
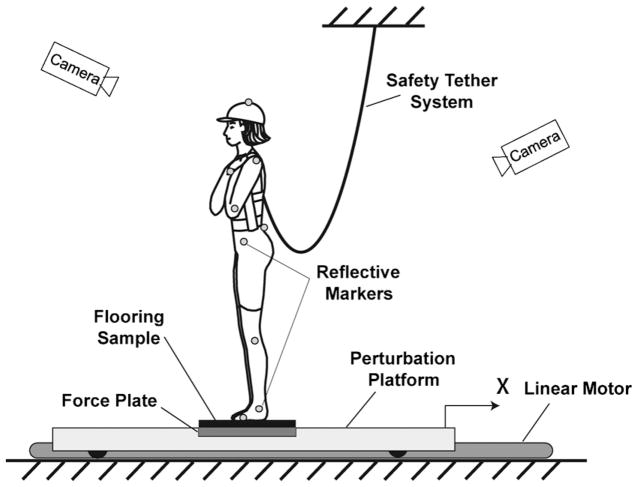
Each participant performed five successive trials on each of the five floor conditions (presented in a random order). The motions of 23 reflective markers placed at anatomical landmarks (Fig. 1) were collected at 120 Hz using an eight-camera motion capture system (Motion Analysis Corporation, Santa Rosa, USA). For the purposes of safety, all subjects were required to wear a chest harness to which a ceiling-mounted safety tether was attached; the apparatus did not impede natural movements or responses.
Fig. 1.
Schematic diagram of the experimental setup for the backwards floor translation task. A force plate measured the time-varying location of the underfoot centre of pressure, while a motion capture system measured the position of 23 markers attached to the following anatomical landmarks: top of the head, spinous process of the C7 vertebra, sacrum, bilaterally on the acromion, lateral epicondyle of the humerus, styloid process of the radius, anterior superior iliac spine, greater trochanter, lateral condyle of the femur, calcaneus, lateral malleolus, head of the fifth metatarsal, and distal phalange of hallux.
For each trial, the participant initially stood barefoot on top of a flooring sample mounted over a force plate (collected at 960 Hz; model 4060-15, Bertec Corp., Columbus, OH, USA), built into a wheeled perturbation platform (Fig. 1). The platform was connected to a linear motor (Triology T4D, Compumotor GV6K driver) and the movement profile was controlled using a custom routine. Prior to the perturbation, participants stood with their feet shoulder width apart, arms across their chests, and were required to maintain the location of the COP within a 1 cm window using real-time visual feedback provided by a custom software routine. After a random time delay between zero and 10 s following trial initiation, the platform was accelerated posteriorly at 5 m/s2 until a velocity of 0.2 m/s was achieved. At this point the accelerative phase ended, but the perturbation continued at a velocity of 0.2 m/s for 2 s, resulting in an overall posterior displacement of 26.5 cm. The participant was required to maintain her balance during and following the perturbation using feet-in-place responses (without taking a step). Hip flexion and arm movements were allowed. One-minute breaks were provided between each trial, and 2-min breaks were offered every five trials (or upon request by the participant). This perturbation paradigm causes the COM to be pitched anteriorly, simulating the type of balance disturbance that occurs following a trip, standing on a bus that quickly decelerates, or being nudged from behind. The perturbation profile we used in this study was equivalent to a ‘moderate severity’ perturbation previously used in a young population (Murnaghan and Robinovitch, 2008), which presented a challenging situation for our aged population.
2.4. Data analysis
Fourth-order, dual-pass, low-pass digital Butterworth filters were used to filter kinematic data (3 Hz cutoff frequency) and force data (5 Hz cutoff frequency). A 12-segment rigid-link model was constructed (Winter, 2009) to calculate the location of the whole-body COM. The anterior–posterior (AP) and medial–laterial (ML) trajectories of the COP were determined, taking into account the differing heights of the flooring samples. Due to the small magnitudes of displacements in the ML direction, this report focuses on the AP trajectories only.
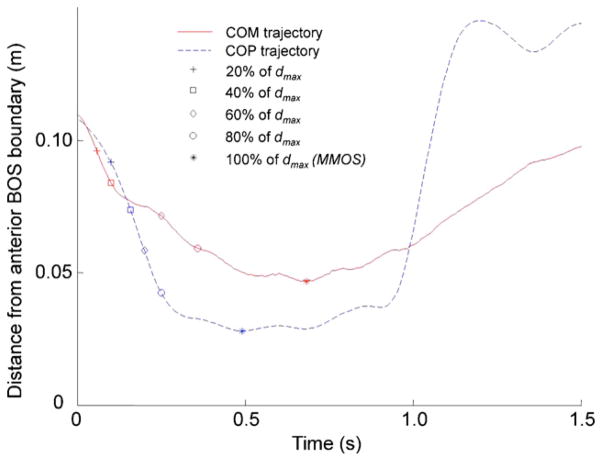
The BOS boundaries were defined by markers on the hallux, heel, and head of the fifth metatarsal for each foot. The minimum margin of safety (MMOS) of the COM (MMOSCOM) in the anterior direction was determined from its displacement profile, defined at the point of maximum anterior displacement (dmax) when the distance between the vertical projection of the COM and the BOS boundary was at a minimum (i.e. the smallest distance between the COM and the toes during the balance recovery response). The COP minimum margin of safety (MMOSCOP) in the anterior direction was also determined for each trial, defined as the minimum distance between the COP and the anterior BOS boundary (Fig. 2). The MMOSCOM and MMOSCOP were averaged over all trials for each floor condition.
Fig. 2.
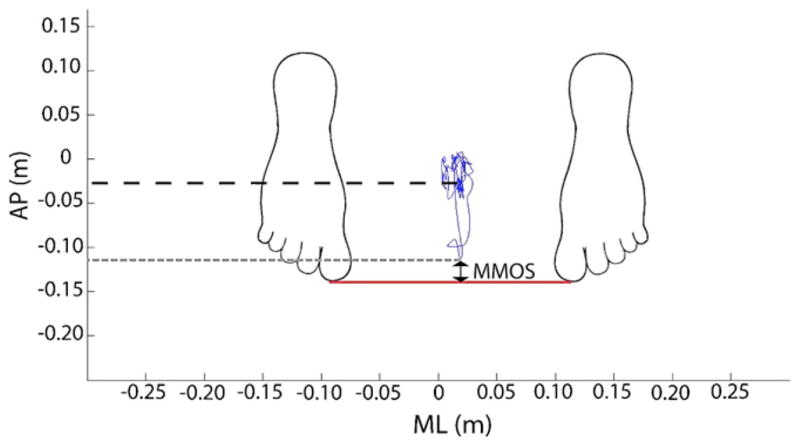
Raw tracing of the location of the underfoot centre of pressure (COP) in the anterior–posterior (AP) and medial–lateral (ML) directions during one trial. The black dashed line indicates the average location of the COP pre-perturbation, while the grey dashed line indicates maximal anterior displacement of COP following perturbation. The minimum margin of safety (MMOS) is derived as the minimum distance between the COP and anterior boundary of the base of support (BOS) defined by the toes.
To provide insight into differing phases of the balance control response, the COM and COP profiles were divided into five equal displacement regions between the instant of perturbation onset and the MMOS (Fig. 3). The rates of change in displacement of the COM and COP were then determined for each of these five relative regions by dividing the COM displacement by the time elapsed in each interval (COM0–20%, COM20–40%, COM40–60%, COM60–80%, COM80–100%, COP0–20%, COP20–40%, COP40–60%, COP60–80%, COP80–100%,). Rates were also determined for absolute portions of the displacement profile in 2 cm intervals. As the average maximum excursion of the COM was 5.9 cm during control trials, the COM displacement rate was determined for the 0–2 cm (COM0–2 cm) and 2–4 cm (COM2–4 cm) regions. The COP travelled an average distance of 10.3 cm on the control floor; therefore COP displacement rates were determined for the 0–2 cm (COP0–2 cm), 2–4 cm (COP2–4 cm), 4–6 cm (COP4–6 cm), and 6–8 cm (COP6–8 cm) regions. Each rate parameter was averaged over all trials for each floor condition.
Fig. 3.
Raw tracing of the centre of mass (COM) and centre of pressure (COP) vs. time for a representative trial for 1.5 s following the instant of perturbation. Displayed on each curve are markers denoting the divisions between the five relative displacement regions (0–20% of maximum displacement (dmax), 20–40% dmax, etc.).
2.5. Statistics
We used a one-factor repeated-measures analysis of variance (ANOVA) to test for the influence of floor condition on MMOSCOM, MMOSCOP, COM0–20%, COM20–40%, COM40–60%, COM60–80%, COM80–100%, COP0–20%, COP20–40%, COP40–60%, COP60–80%, COP80–100%, COM0–2 cm, COM2–4 cm, COP0–2 cm, COP2–4 cm, COP4–6 cm, and COP6–8 cm. A priori post hoc tests were conducted using paired t-tests with Bonferroni adjustments to compare each of the compliant floors to the rigid control condition. All analyses were performed with statistical analysis software (SPSS Version 18.0, SPSS Inc., Chicago, IL, USA) using an experiment-wide significance level of α = 0.05.
3. Results
Table 2 summarizes the data across outcome variables and floor conditions, while Table 3 presents the statistical results associated with each test or comparison.
Table 2.
Mean (SD) of the minimum margin of safety (MMOS) and displacement rate outcomes for centre-of-mass (COM) and centre-of-pressure (COP) across floor conditions for the backwards floor translation task.
| Parameter | Floor condition
|
||||
|---|---|---|---|---|---|
| Rigid | SmartCell | SofTile | Firm-Foam | Soft-Foam | |
| Margin of safety (m) | |||||
| MMOSCOM | 0.058 (0.013) | 0.062 (0.010) | 0.051 (0.013) | 0.027 (0.013) | 0.044 (0.010) |
| MMOSCOP | 0.026 (0.008) | 0.030 (0.007) | 0.021 (0.012) | 0.017 (0.014) | 0.019 (0.011) |
| Relative rates (m/s) | |||||
| COM0–20% | 0.185 (0.014) | 0.182 (0.014) | 0.195 (0.014) | 0.193 (0.041) | 0.189 (0.022) |
| COM20–40% | 0.267 (0.047) | 0.279 (0.037) | 0.270 (0.040) | 0.199 (0.070) | 0.242 (0.049) |
| COM40–60% | 0.116 (0.036) | 0.132 (0.060) | 0.113 (0.043) | 0.076 (0.030) | 0.077 (0.021) |
| COM60–80% | 0.096 (0.015) | 0.091 (0.018) | 0.096 (0.020) | 0.067 (0.025) | 0.078 (0.019) |
| COM80–100% | 0.048 (0.010) | 0.046 (0.012) | 0.044 (0.008) | 0.034 (0.006) | 0.041 (0.019) |
| COP0–20% | 0.217 (0.030) | 0.237 (0.026) | 0.291 (0.038) | 0.238 (0.053) | 0.273 (0.021) |
| COP20–40% | 0.541 (0.073) | 0.542 (0.074) | 0.560 (0.089) | 0.457 (0.099) | 0.538 (0.086) |
| COP40–60% | 0.566 (0.091) | 0.546 (0.090) | 0.495 (0.072) | 0.288 (0.061) | 0.309 (0.109) |
| COP60–80% | 0.471 (0.097) | 0.464 (0.100) | 0.401 (0.087) | 0.306 (0.054) | 0.319 (0.177) |
| COP80–100% | 0.134 (0.066) | 0.154 (0.067) | 0.145 (0.066) | 0.102(0.056) | 0.182 (0.115) |
| Absolute rates (m/s) | |||||
| COM0–2 cm | 0.220 (0.007) | 0.220 (0.006) | 0.226 (0.009) | 0.222 (0.019) | 0.223 (0.008) |
| COM2–4 cm | 0.104 (0.012) | 0.100 (0.015) | 0.112 (0.014) | 0.090 (0.012) | 0.084 (0.015) |
| COP0–2 cm | 0.213 (0.032) | 0.227 (0.026) | 0.268 (0.034) | 0.241 (0.028) | 0.266 (0.029) |
| COP2–4 cm | 0.525 (0.061) | 0.538 (0.074) | 0.571 (0.088) | 0.460 (0.071) | 0.608 (0.154) |
| COP4–6 cm | 0.567 (0.092) | 0.553 (0.085) | 0.499 (0.056) | 0.304 (0.064) | 0.330 (0.119) |
| COP6–8 cm | 0.481 (0.136) | 0.490 (0.102) | 0.462 (0.093) | 0.301 (0.039) | 0.251 (0.087) |
Table 3.
F -ratios (p-value) from the repeated measures ANOVA and t-statistics (p-value) from paired t-tests (compared to the rigid condition) for the minimum margin of safety (MMOS) and displacement rate outcomes for centre-of-mass (COM) and centre-of-pressure (COP) profiles. Paired t-tests were not conducted if ANOVA revealed no significant effect of floor condition.
| Parameter | ANOVA | Paired t-tests
|
|||
|---|---|---|---|---|---|
| SmartCell | SofTile | Firm-Foam | Soft-Foam | ||
| Margin of safety | |||||
| MMOSCOM | 35.482 (<0.001) | −1.543 (0.149) | 2.340 (0.037) | 3.783 (0.003)* | 4.957 (<0.001)* |
| MMOSCOP | 4.542 (0.006) | −1.799 (0.097) | 1.903 (0.081) | 3.212 (0.007)* | 1.146 (0.274) |
| Relative rates | |||||
| COM0–20% | 0.893 (0.409) | – | – | – | – |
| COM20–40% | 8.014 (0.001) | −1.359 (0.199) | −0.43 (0.675) | 3.001 (0.011)* | 1.583 (0.139) |
| COM40–60% | 5.748 (0.006) | −1.429 (0.179) | 0.301 (0.769) | 2.700 (0.019)* | 3.093 (0.009)* |
| COM60–80% | 7.508 (<0.001) | 0.765 (0.459) | −0.014 (0.989) | 7.031 (<0.001)* | 2.789 (0.016)* |
| COM80–100% | 2.5 (0.102) | – | – | – | – |
| COP0–20% | 17.049 (<0.001) | −2.422 (0.032)** | −6.004 (<0.001)** | −1.311 (0.214) | −10.238 (<0.001)** |
| COP20–40% | 3.822 (0.009) | −0.043 (0.966) | −0.633 (0.539) | 2.510 (0.027)* | 0.076 (0.941) |
| COP40–60% | 38.164 (<0.001) | 0.809 (0.434) | 3.522 (0.004)* | 8.036 (<0.001)* | 6.009 (<0.001)* |
| COP60–80% | 8.048 (0.003) | 0.477 (0.642) | 6.332 (<0.001)* | 4.978 (<0.001)* | 2.636 (0.022)* |
| COP80–100% | 2.556 (0.095) | – | – | – | – |
| Absolute rates | |||||
| COM0–2 cm | 0.945 (0.409) | – | – | – | – |
| COM2–4 cm | 11.280 (<0.001) | 1.611 (0.133) | −2.272 (0.042)** | 3.387 (0.005)* | 4.659 (0.001)* |
| COP0–2 cm | 21.908 (<0.001) | −1.952 (0.075) | −6.203 (<0.001)** | −2.673 (0.020)** | −7.282 (<0.001)** |
| COP2–4 cm | 5.014 (0.01) | −0.601 (0.559) | −1.713 (0.112) | 2.415 (0.033)* | −1.633 (0.128) |
| COP4–6 cm | 38.920 (<0.001) | 0.592 (0.565) | 2.803 (0.016)* | 9.102 (<0.001)* | 5.643 (<0.001)* |
| COP6–8 cm | 30.193 (<0.001) | −0.315 (0.758) | 1.036 (0.321) | 5.297 (<0.001)* | 5.669 (<0.001)* |
Significantly lower than control condition (p < 0.0125).
Significantly greater than control condition (p < 0.0125).
3.1. Margins of safety
ANOVA results (Table 3) indicated that floor condition was significantly associated with both MMOSCOM and MMOSCOP. Paired t-tests demonstrated that MMOSCOM values for the Firm-Foam and Soft-Foam conditions were smaller than the control condition. MMOSCOP was significantly smaller than the control condition for the Firm-Foam condition. MMOSCOM and MMOSCOP for the Smart-Cell and SofTile floors were not significantly different from the control.
3.2. Relative displacement rates
Three of the five relative COM rate variables were significantly associated with floor condition. Specifically, floor condition influenced COM20–40%, COM40–60%, and COM60–80%. Paired t-tests (Table 3) demonstrated that displacement rates were slower for the Firm-Foam condition relative to the control condition for COM20–40%, COM40–60%, and COM60–80%. Displacement rates were decreased for the Soft-Foam condition for COM40–60%, and COM60–80%.
We observed an effect of floor condition on four of the five COP displacement rates (Tables 2 and 3). Paired t-tests indicated that COP0–20% was increased for the SmartCell, SofTile, and Soft-Foam floor conditions relative to the control condition. Compared to the control floor, COP20–40% was slower for the Firm-Foam condition, and COP40–60% was decreased for the SofTile, Firm-Foam, and Soft-Foam conditions. Displacement rates were also significantly lower on these three floors for COP60–80%. Floor condition did not have an influence on COP80–100%.
3.3. Absolute displacement rates
Although floor condition did not have an influence on COM0–2 cm, it was significantly associated with COM2–4 cm. Paired t-tests revealed that, compared to the control condition, COM2–4 cm was greater for the SofTile condition, but decreased for the Firm-Foam and Soft-Foam conditions.
Results indicated that floor condition had an influence on all absolute COP displacement rates. Compared to the control condition, COP0–2 cm was higher for the SofTile, Firm-Foam, and Soft-Foam conditions. COP2–4 cm was lower for the Firm-Foam condition, while COP4–6 cm was lower for the SofTile, Firm-Foam, and Soft-Foam floors. COP6–8 cm was slower for the Firm-Foam and Soft-Foam floors.
4. Discussion
In the current study, we examined the influence of floor stiffness (5 conditions) on indices of balance and balance control responses in elderly community-dwelling women following a backwards floor translation perturbation. Our results suggest that appropriately designed novel compliant flooring systems may cause minimal effects on the balance control characteristics of this population. Our first hypothesis was that the MMOS and displacement rates of the COM and COP would not be different for perturbations on the novel compliant floors relative to the control condition, which our results supported in 29 of 36 possible cases (2 floors × 18 dependent variables = 36 possible cases). Regarding our second hypothesis, we observed that excessive reductions in floor stiffness (as created in the two foam conditions) caused substantial negative effects on balance control and balance recovery ability characterized by decreased MMOS in three of four cases (2 floors × 2 dependent variables), and slowed displacement rates in 17 of 32 cases (2 floors × 16 dependent variables). These results indicate that while reducing floor stiffness has the potential to impair balance control responses following a perturbation, the novel compliant floors tested in this study (SmartCell in particular) do not appear to do so.
Our results are in accordance with a series of proposed balance control mechanisms used to maintain feet-in-place balance (Winter et al., 1998; Winter et al., 2001; Morasso and Schieppati, 1999; Morasso and Sanguineti, 2002). In all floor conditions, the COM moved anteriorly within the BOS immediately following the perturbation. In response, we observed a rapid shift of the COP towards the toes to decelerate the COM and shift it back towards its initial position. As a consequence, the MMOS (Table 2) were always lower for the COP relative to COM (average MMOSCOP to MMOSCOM ratios were 0.45, 0.48, 0.41, 0.63, and 0.43 for the Rigid, Smart-Cell, SofTile, Firm-Foam, and Soft-Foam conditions, respectively). In addition to these amplitude differences, we observed displacement rates to be consistently larger for COP compared to COM, with ratios for the largest COP to largest COM rates averaging 2.12, 1.96, 2.07, 2.30, and 2.22 for the Rigid, SmartCell, SofTile, Firm-Foam, and Soft-Foam conditions, respectively. Although these general trends existed in all trials, the differential decreases in MMOS and displacement rates observed across floors (predominantly in the foam conditions) indicates that surface compliance has the potential to impair elements of balance and balance control responses.
During the initial phase of COP movement (i.e. COP0–20% or COP0–2 cm), we unexpectedly found that the displacement rates were often greater for the compliant floors than those on the control floor. One potential explanation for this observation may relate to baseline pre-perturbation ankle stiffness. It is possible that, in response to the lower-stiffness surfaces, participants increased co-contraction of the muscles spanning the ankle to increase the effective stiffness of the ankle joint and the resulting angular displacement in response to applied loads. If this initial co-contraction was strong enough it may have also contributed to faster COP displacements by increasing the gain of the stretch reflex in the plantar flexors immediately post-perturbation (Nielsen et al., 1994). However, the decision was made a priori to avoid controlling baseline ankle stiffness to allow for more realistic balance control responses across floors, rendering this explanation mainly speculative. Nevertheless, these potential benefits are likely outweighed by the decreased MMOS and displacement rates typically observed later in the response for the foam, and to a lesser extent, the SofTile conditions.
These results add to existing literature related to the effects of compliant flooring on balance and postural stability. Postural sway is commonly observed to increase in both the anterior–posterior and medial–lateral directions during quiet stance on compliant foam surfaces compared to rigid surfaces (Lord et al., 1991; Lord and Menz, 2000; Gill et al., 2001). In addition, walking on foam compared to rigid floors has been associated with lowered COM trajectory and toe clearance (Marigold and Patla, 2005), and increases in step length, step width, and step width variability (Maclellan and Patla, 2006). There is less clarity regarding the influence of common flooring products such as carpet. Redfern et al. (1997) report that thick carpet can lead to increases in anterior–posterior sway for older adults when exposed to a moving visual environment, while Dickinson et al. (2001, 2002) found no effect of carpet on sway in older adults. Encouragingly, and with particular respect to novel compliant flooring systems, Laing and Robinovitch (2009) report that the amplitude and velocity of quiet stance sway in the medial–lateral direction were not different between a rigid surface and the SmartCell floor examined in the current study. Furthermore, the times required to complete the Timed Up and Go test (a predictor of fall risk (Podsiadlo and Richardson, 1991; Lundin-Olsson et al., 1998; Chiu et al., 2003) were not different for SmartCell, SofTile and a rigid floor condition. Finally, when exposed to a floor translation task, participants successfully regained balance equally well on the SmartCell, SofTile and rigid floors. Our results extend from their findings, and demonstrate that the displacement profiles of the COM (a balance indicator) are not affected by the novel compliant flooring systems, and that the balance control variable is minimally affected by these surface conditions.
It is important to consider the current results in concert with reports of the force attenuative properties of various flooring materials. For a sideways fall with an impact velocity of 4 m/s, SmartCell and SofTile have been reported to reduce the peak force applied to the proximal femur (compared to a rigid floor) by 33.7% and 51.2% respectively (Laing and Robinovitch, 2009). In contrast, force attenuation values for common compliant floors average 7% for wooden floors, 15% for carpets without underpadding, and 24% for carpets with underpadding (Gardner et al., 1998; Simpson et al., 2004; Maki and Fernie, 1990). That the novel compliant floors tested in this study can more than double the force attenuative capacity of traditional products, without concomitant impairments in balance and stability, supports their value as a promising intervention strategy.
A host of additional factors must be considered when assessing the clinical feasibility of novel compliant floors. The relatively low profile of the SmartCell flooring (25 mm thick) makes it suitable for installation in newly built facilities or via retrofitting. Retrofitting issues that have been successfully addressed include installation of ramps or transition markers between traditional and compliant flooring zones, ensuring sufficient clearance for doors, and maintaining standard heights for infrastructure including toilets and sinks. In contrast, the SofTile system tested (100 mm thick) is likely more appropriate for outdoor applications including patios, gardens, and walkways. However, lower profile models (50 mm thick) do exist that may be adaptable for certain indoor applications. In addition, overlays such as carpet or vinyl may be required for certain settings, which may affect the force attenuation and balance results reported in the literature. Finally, an important consideration is that flooring systems should minimally influence the work demands of facility staff (e.g. rolling wheelchairs or lift-assists). Additional research is warranted to assess the potential influence of novel compliant flooring systems on these issues.
There were several limitations associated with this study. First, we restricted our perturbation to the anterior–posterior direction, and our participants to feet-in-place responses based on recent video footage that demonstrates that 32% of falls occurred as a result of inappropriate transfer skills during primarily feet-in-place activities (e.g. rising from a chair, putting on a jacket while standing) (Robinovitch et al., 2009). However, as change-in-support stepping reactions are also prevalent control responses (Maki and Mcilroy, 2005), additional studies are required to assess the influence of compliant flooring during such balance control strategies in both AP and ML directions. Second, this study population was drawn from community-dwelling elderly women as they are at greater risk of hip fracture compared to both younger adults and age-matched males (Cumming et al., 1997; Jacobsen et al., 1990; Cummings and Melton, 2002). However, as compliant flooring may be most suitable for installation in high-risk environments such as retirement homes, future studies should investigate the potential effects of these floors on the balance control characteristics of the residents in these settings. Third, as this study sought to isolate the influence of flooring type (and not footwear) on balance recovery ability, our participants were barefoot throughout the experimental protocol. Accordingly, our findings may not directly extend to common situations where footwear is worn in which case foot-floor contact areas would likely be higher, and consequently, local floor deformations lower. However, in addition to isolating the influence of flooring, the current results provide insights into how such flooring systems might influence balance during worst-case scenarios where seniors are not wearing shoes during activities of daily living e.g. transferring from the bedroom to the bathroom in the middle of the night. Fourth, although the current study investigated classic variables used to assess stability during feet-in-place responses (including COM and COP) (Winter et al., 1998; Winter et al., 2001; Morasso and Schieppati, 1999; Morasso and Sanguineti, 2002), the use of electromyography in future studies could provide further insights into potential differences in the timing and amplitude of control responses across flooring conditions. Finally, not all commercially available compliant flooring systems were tested in the current study. As the design principles and materials employed across products differ substantially, so too may their influences on force attenuation, balance, and mobility. Consequently, additional tests with a wider range of products are required to provide consumers with an evidence-base to guide purchase and implementation decisions.
Effective intervention strategies are urgently needed to curtail the anticipated rise in incidence of fall-related injuries over the coming decades. Novel compliant flooring systems appear to be a promising approach, capable of providing substantial force attenuative properties with minimal coincident impairments in outcomes from balance and mobility tests (Laing and Robinovitch, 2009). Our findings provide further support for this intervention approach by suggesting that biomechanical indices of balance and balance control responses are generally not impaired by novel compliant floors such as SmartCell or SofTile following a floor translation perturbation. These results support the introduction of pilot installations to inform the development of clinical trials that test the effectiveness of novel compliant floors at reducing fall-related injuries in older adults.
Acknowledgments
The data for this study were collected at the Injury Prevention and Mobility Laboratory at Simon Fraser University (Burnaby, Canada), and the authors are grateful to lab director Stephen N. Robinovitch for use of the facilities. This research was funded in part by an operating grant obtained by ACL from the Natural Sciences and Engineering Research Council of Canada (NSERC; grant # 386544-2010). ADW was supported by the Ontario Graduate Scholarship program.
Footnotes
Conflict of interest statement
The authors have no conflicts of interest to declare. No persons other than ADW and ACL had substantial input into study design, data analysis, or manuscript development.
References
- Betker AL, Moussavi ZM, Szturm T. On modeling center of foot pressure distortion through a medium. IEEE Trans Biomed Eng. 2005;52:345–352. doi: 10.1109/TBME.2004.840466. [DOI] [PubMed] [Google Scholar]
- Cameron ID, Murray GR, Gillespie LD, Robertson MC, Hill KD, Cumming RG, Kerse N. Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database Syst Rev. 2010:CD005465. doi: 10.1002/14651858.CD005465.pub2. [DOI] [PubMed] [Google Scholar]
- Casalena JA, Badre-Alam A, Ovaert TC, Cavanagh PR, Streit DA. The Penn state safety floor: Part II–reduction of fall-related peak impact forces on the femur. J Biomech Eng. 1998;120:527–532. doi: 10.1115/1.2798023. [DOI] [PubMed] [Google Scholar]
- Chiu AY, Au-Yeung SS, Lo SK. A comparison of four functional tests in discriminating fallers from non-fallers in older people. Disabil Rehabil. 2003;25:45–50. [PubMed] [Google Scholar]
- Cumming RG, Nevitt MC, Cummings SR. Epidemiology of hip fractures. Epidemiol Rev. 1997;19:244–257. doi: 10.1093/oxfordjournals.epirev.a017956. [DOI] [PubMed] [Google Scholar]
- Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- Dickinson JI, Shroyer JL, Elias JW. The influence of commercial-grade carpet on postural sway and balance strategy among older adults. Gerontologist. 2002;42:552–559. doi: 10.1093/geront/42.4.552. [DOI] [PubMed] [Google Scholar]
- Dickinson JI, Shroyer JL, Elias JW, Hutton JT, Gentry GM. The effect of selected residential carpet and pad on the balance of healthy older adults. Environ Behav. 2001;33:279–295. [Google Scholar]
- Gardner TN, Simpson AH, Booth C, Sprukkelhorst P, Evans M, Kenwright J, Evans JG. Measurement of impact force, simulation of fall and hip fracture. Med Eng Phys. 1998;20:57–65. doi: 10.1016/s1350-4533(97)00041-6. [DOI] [PubMed] [Google Scholar]
- Gill J, Allum JH, Carpenter MG, Held-Ziolkowska M, Adkin AL, Honegger F, Pierchala K. Trunk sway measures of postural stability during clinical balance tests: effects of age. J Gerontol A Biol Sci Med Sci. 2001;56:M438–M447. doi: 10.1093/gerona/56.7.m438. [DOI] [PubMed] [Google Scholar]
- Grisso JA, Kelsey JL, Strom BL, Chiu GY, Maislin G, O’brien LA, Hoffman S, Kaplan F. Risk factors for falls as a cause of hip fracture in women. The Northeast Hip Fracture Study Group. N Engl J Med. 1991;324:1326–1331. doi: 10.1056/NEJM199105093241905. [DOI] [PubMed] [Google Scholar]
- Healey F. Does flooring type affect risk of injury in older in-patients? Nurs Times. 1994;90:40–41. [PubMed] [Google Scholar]
- Health Canada. Canada’s aging population. In: Canada H, editor. A Report Prepared by Health Canada in Collaboration with the Interdepartmental Committee on Aging and Seniors Issues. Government of Canada; 2002. [Google Scholar]
- Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA. Hip fracture incidence among the old and very old: a population-based study of 745,435 cases. Am J Pub Health. 1990;80:871–873. doi: 10.2105/ajph.80.7.871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laforest S, Robitaille Y, Dorval D, Lesage D, Pless B. Severity of fall injuries on sand or grass in playgrounds. J Epidemiol Community Health. 2000;54:475–477. doi: 10.1136/jech.54.6.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laing AC, Robinovitch SN. Low stiffness floors can attenuate fall-related femoral impact forces by up to 50% without substantially impairing balance in older women. Accid Anal Prev. 2009;41:642–650. doi: 10.1016/j.aap.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Laing AC, Tootoonchi I, Hulme PA, Robinovitch SN. Effect of compliant flooring on impact force during falls on the hip. J Orthop Res. 2006;24:1405–1411. doi: 10.1002/jor.20172. [DOI] [PubMed] [Google Scholar]
- Lord SR, Clark RD, Webster IW. Postural stability and associated physiological factors in a population of aged persons. J Gerontol. 1991;46:M69–76. doi: 10.1093/geronj/46.3.m69. [DOI] [PubMed] [Google Scholar]
- Lord SR, Menz HB. Visual contributions to postural stability in older adults. Gerontology. 2000;46:306–310. doi: 10.1159/000022182. [DOI] [PubMed] [Google Scholar]
- Lundin-Olsson L, Nyberg L, Gustafson Y. Attention, frailty, and falls: the effect of a manual task on basic mobility. J Am Geriatr Soc. 1998;46:758–761. doi: 10.1111/j.1532-5415.1998.tb03813.x. [DOI] [PubMed] [Google Scholar]
- Maclellan MJ, Patla AE. Adaptations of walking pattern on a compliant surface to regulate dynamic stability. Exp Brain Res. 2006;173:521–530. doi: 10.1007/s00221-006-0399-5. [DOI] [PubMed] [Google Scholar]
- Maki BE, Fernie GR. Impact attenuation of floor coverings in simulated falling accidents. Appl Ergon. 1990;21:107–114. doi: 10.1016/0003-6870(90)90132-h. [DOI] [PubMed] [Google Scholar]
- Maki BE, Mcilroy WE. Change-in-support balance reactions in older persons: an emerging research area of clinical importance. Neurol Clin. 2005;23(751–83):vi–vi10. doi: 10.1016/j.ncl.2005.01.002. [DOI] [PubMed] [Google Scholar]
- Marigold DS, Patla AE. Adapting locomotion to different surface compliances: neuromuscular responses and changes in movement dynamics. J Neurophysiol. 2005;94:1733–1750. doi: 10.1152/jn.00019.2005. [DOI] [PubMed] [Google Scholar]
- Morasso PG, Sanguineti V. Ankle muscle stiffness alone cannot stabilize balance during quiet stance. J Neurophysiol. 2002;88:2157–2162. doi: 10.1152/jn.2002.88.4.2157. [DOI] [PubMed] [Google Scholar]
- Morasso PG, Schieppati M. Can muscle stiffness alone stabilize upright standing? J Neurophysiol. 1999;83:1622–1626. doi: 10.1152/jn.1999.82.3.1622. [DOI] [PubMed] [Google Scholar]
- Murnaghan CD, Robinovitch SN. The effect of initial movement dynamics on human responses to postural perturbations. Proceedings of the 2008 International Society of Neuroscience Annual Meeting; Washington, DC. 2008. [DOI] [PubMed] [Google Scholar]
- Nevitt MC, Cummings SR. Type of fall and risk of hip and wrist fractures: the study of osteoporotic fractures. The Study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 1993;41:1226–1234. doi: 10.1111/j.1532-5415.1993.tb07307.x. [DOI] [PubMed] [Google Scholar]
- Nielsen J, Sinkjaer T, Toft E, Kagamihara Y. Segmental reflexes and ankle joint stiffness during co-contraction of antagonistic ankle muscles in man. Exp Brain Res. 1994;102:350–358. doi: 10.1007/BF00227521. [DOI] [PubMed] [Google Scholar]
- Pickett W, Ardern C, Brison RJ. A population-based study of potential brain injuries requiring emergency care. CMAJ. 2001;165:288–292. [PMC free article] [PubMed] [Google Scholar]
- Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- Redfern MS, Moore PL, Yarsky CM. The influence of flooring on standing balance among older persons. Hum Factors. 1997;39:445–455. doi: 10.1518/001872097778827043. [DOI] [PubMed] [Google Scholar]
- Ring C, Nayak US, Isaacs B. The effect of visual deprivation and proprioceptive change on postural sway in healthy adults. J Am Geriatr Soc. 1989;37:745–749. doi: 10.1111/j.1532-5415.1989.tb02237.x. [DOI] [PubMed] [Google Scholar]
- Robinovitch SN, Feldman F, Wan D, Aziz O, Sarraf T. Video recording of real-life falls in long term care provides new insight on the cause and circumstances of falls in older adults. Proceedings of the 19th Annual Meeting of the International Society for Posture and Gait; June 21–25; Bologna, Italy. 2009. [Google Scholar]
- Simpson AH, Lamb S, Roberts PJ, Gardner TN, Evans JG. Does the type of flooring affect the risk of hip fracture? Age Ageing. 2004;33:242–246. doi: 10.1093/ageing/afh071. [DOI] [PubMed] [Google Scholar]
- Smartrisk. The Economic Burden of Injury in Canada. SMARTRISK; Toronto, ON: 2009. [Google Scholar]
- Teasdale N, Stelmach GE, Breunig A. Postural sway characteristics of the elderly under normal and altered visual and support surface conditions. J Gerontol. 1991;46:B238–B244. doi: 10.1093/geronj/46.6.b238. [DOI] [PubMed] [Google Scholar]
- Winter D. Biomechanics and Motor Control of Human Movement. 4. John Wiley & Sons Canada Ltd; Mississauga, Ontario, Canada: 2009. [Google Scholar]
- Winter DA, Patla AE, Prince F, Ishac M, Gielo-Perczak K. Stiffness control of balance in quiet standing. J Neurophysiol. 1998;80:1211–1221. doi: 10.1152/jn.1998.80.3.1211. [DOI] [PubMed] [Google Scholar]
- Winter DA, Patla AE, Rietdyk S, Ishac MG. Ankle muscle stiffness in the control of balance during quiet standing. J Neurophysiol. 2001;85:2630–2633. doi: 10.1152/jn.2001.85.6.2630. [DOI] [PubMed] [Google Scholar]