Abstract
Background
A dimension of negatively oriented affect within oppositional defiant disorder (ODD) symptoms, which has been described as irritability, has been shown to predict depression and anxiety. Related constructs have been linked to temperament and personality constructs. Yet, only a few studies have examined the prediction from irritability within ODD to psychopathology or personality outcomes. Further, no studies have investigated whether irritability distinguishes among classes of youth.
Methods
Data from a clinic-referred sample of 7 to 12 year old boys followed up to age 18 were used. Measures included structured clinical interviews with parents through adolescence, and youth self-report of depression and personality domains at age 18.
Results
Variable oriented analyses found predictive links between irritability and outcomes of depression, anxiety and Neuroticism. Latent classes of youth were distinguished by the presence or absence of irritability symptoms. Youth classified by irritability symptoms at baseline were significantly more likely to show anxiety and depression through adolescence and depression and Neuroticism at 18. No relationship was observed for the other of the Big Five personality factors.
Conclusion
Irritability symptoms within ODD distinguish youth at risk for persisting problems with internalizing disorders and Neuroticism into adulthood. The findings are suggestive of a model in which the early emergence of irritability marks life-course risks for specific types of psychopathology and personality problems.
Keywords: Oppositional defiant disorder, irritability, depression, anxiety, neuroticism
Introduction
Recent evidence indicates that a subset of symptoms among the criteria for Oppositional Defiant Disorder (ODD) distinguish a dimension of affective dysregulation from symptoms of headstrong, antagonistic or oppositional behavior (Aebi et al., 2010; Burke, Hipwell, & Loeber, 2010; Rowe, Costello, Angold, Copeland, & Maughan, 2010; Stringaris & Goodman, 2009b). Apart from disagreeing as to whether losing temper or being spiteful load on the affective or behavioral dimension, most studies of these dimensions within ODD symptoms agree that arguing, defying, annoying others and blaming others are not indicators of affect (Burke, et al., 2010; Stringaris & Goodman, 2009b) and that the behavioral dimensions are not predictive of later mood or anxiety problems (Burke, et al., 2010; Rowe, et al., 2010; Stringaris & Goodman, 2009a).
The implications of this work are significant. First, since ODD typically has an age of onset by mid-childhood, to the degree that affective symptoms among ODD predict depression, anxiety or other disorders, they may provide an early indication of risk for such outcomes. An insufficient evidence base exists to determine the specificity and discrimination among various psychopathological outcomes of affective ODD symptoms, or the degree to which they might predict from childhood to adulthood. Secondly, contrary to prior models (Puig-Antich, 1982; World Health Organization, 1992) it appears that ODD, rather than CD, explains the observed co-occurrence of depression and CD (Burke, Loeber, Lahey, & Rathouz, 2005; Copeland, Shanahan, Costello, & Angold, 2009; Rowe, et al., 2010). This evidence suggests hypotheses about important broad revisions to etiological and developmental models of psychopathology from childhood to adulthood.
Studies examining outcomes associated with an affective dimension of ODD have found prediction to depression (Burke, et al., 2010; Stringaris & Goodman, 2009a) and to anxiety (Rowe, et al., 2010). A similar irritability construct consisting of ODD symptoms of anger and tantrums measured in early adolescence was predictive of depression and anxiety at follow-up 20 years later in a community sample of boys and girls (Stringaris, Cohen, Pine & Leibenluft, 2009). Less consistent prediction from the affective dimension of ODD to CD has been observed (Burke, et al., 2010; Stringaris & Goodman, 2009a). An ODD behavioral dimension was predictive of borderline personality disorder (BPD), whereas the affective dimension was not (Burke & Stepp, 2012). Given the relatively small set of studies on the topic to this point, a great deal of further research is needed to more fully describe the development of irritability and the degree to which it does or does not indicate risk for other disorders.
A separate line of research has described an overlapping construct: negative affectivity (NA; Watson & Clark, 1984). NA generally reflects a disposition to feelings of distress or aversive emotional states, and explains a significant degree of covariation between anxiety and depression (Clark & Watson, 1991; Garber & Weersing, 2010). Regarded as a dispositional tendency, it has been suggested that NA may be specifically related to the personality construct of Neuroticism (Garber & Weersing, 2010; Watson, 2000). Neuroticism is characterized as a temperament or disposition to a negativistic cognitive style, negative interpretation of ambiguous stimuli, and poor coping strategies related to distress (Watson, 2000). Despite superficial similarities, whether the affective dysregulation within ODD is related to Neuroticism is unknown.
It should be noted that in prior publications regarding this affective dimension of ODD symptoms, different labels for the construct have been used. Burke (Burke & Loeber, 2010; Burke, et al., 2010) has used the term “negative affect” to refer to a construct consisting of the ODD items of being touchy, angry and spiteful. Alternatively, (Stringaris & Goodman, 2009b) and (Rowe, et al., 2010) have used the label “irritability” to refer to a construct consisting of being touchy, angry and losing temper. Consistent across these constructs is the presence of being touchy and angry, and both constructs have been shown to predict to later depression. However, the differences between negative affect within ODD (e.g. Burke, et al., 2010) and NA (e.g. Watson & Clark, 1984) are much more substantial. NA is broad, and includes referents related to anxiety, guilt, dysphoric mood, hostility and shame, whereas affect dysregulation within ODD is circumscribed and does not include indicators of anxiety or dysphoria. Given the potential for confusion with the existing literature and in the present analyses, hereafter the term irritability will be used to refer to the affective dimension of ODD.
Latent variable analysis
Studies of irritability within ODD have to this point employed only variable oriented analyses. These have generated important insights as described above. What these types of analyses are not able to reveal is whether and how these items distinguish among groups of people. Are there youths with ODD who show high levels of affective symptoms and low levels of behavioral symptoms, or vice versa? Are youths instead simply differentiated by showing high, medium and low levels of severity of symptoms? If substantial groups of youth are distinguished by the presence or absence of irritability within ODD, and if these groups differ from one another in terms of risk for different outcomes, classification systems will need to reflect these distinctions.
The present paper examines affective dysregulation in the form of irritability within ODD symptoms, considering several important issues related to development and classification: (1) Does irritability predict proximal changes in depression and anxiety across annual measurements through adolescence, and is it distinct from the behavioral dimensions of ODD in this? (2) Does irritability through adolescence predict adult self-report of depression and neuroticism? Is any relationship between irritability and neuroticism specific, or is it instead due to a general link between irritability and personality functioning? (3) Does irritability distinguish classes of children, and if so, are those with irritability at greater risk for anxiety and depression through adolescence and for mood and personality outcomes in adulthood?
Method
Data for the present analyses come from the Developmental Trends Study (Loeber, Green, Lahey, Frick, & McBurnett, 2000), a sample of 177 boys between the ages of 7 and 12 who were recruited from psychiatric clinics in Pennsylvania and Georgia. Boys were followed up annually to age 17. Young adult assessments were conducted with the youth as the respondent at 18. All study procedures were approved and monitored by the Institutional Review Board of the University of Pittsburgh. Informed consent was obtained for all participants.
Enrollment criteria included: boys living with at least one biological parent; no history of mental retardation or psychosis, no inpatient psychiatric treatment within the last six months, and no psychotropic medication that could not be discontinued for two days prior to baseline assessment. The sample was over-representative of ADHD, ODD and CD.
Retention rates through adolescence ranged from a high of 100% in Year 2 to 87.1% in Year 10, with an average across all years of 93.4%. There were 162 participants (91.5% of the original sample) assessed at age 18. The sample was composed of non-Hispanic white (70%) and African-American boys (30%).
Measures
Depression and anxiety
A modified version (Loeber, Green, Lahey, & Stouthamer-Loeber, 1989) of the DISC (Costello, Edelbrock, Dulcan, Kalas, & Klaric, 1987) was used for this study. Parent report of symptoms of CD, ODD, ADHD, depression and anxiety was obtained at each wave. Although child and teacher report were also collected, neither included assessment of all symptoms of interest past year 4 of the study.
Parent DISC report was used to create a composite depression variable by combining reports of symptoms of dysthymia (DYS) and major depression (MD). As defined by the DSM (APA, 1994), MD includes anhedonia, psychomotor agitation or retardation and recurrent thoughts of death, whereas DYS does not. Conversely, DYS includes hopelessness, MD does not. To avoid counting overlapping symptoms twice, depression in these analyses is the sum of ten unique symptoms across MD and DYS. Further, irritability was not considered as a substitute for dysphoric mood in these analyses. Parents reported an average of 1.43 symptoms (sd = 1.86), ranging from 0 to 8 symptoms at baseline. Cronbach's alpha at baseline was .77.
An index of anxiety was created using the sum of symptoms of overanxious disorder (OAD) and separation anxiety disorder (SAD). OAD measures general anxiety, such as unrealistic worry or preoccupation, concerns about competence and physical tension. SAD measures concerns involving separation from caregivers and fears of harm befalling caregivers. At baseline, parents reported a range from 0 to 12 symptoms (m= 3.18, sd = 2.5). Cronbach's alpha at baseline was .78.
Dimensions of ODD
Based on factor analyses described in previous work (Burke, et al., 2010), three separate dimensions of ODD symptoms were created. An affective dimension, called irritability, was indexed by the sum of the symptoms of angry, spiteful and touchy. Symptoms of oppositional behavior (OB) included often loses temper, argues, and defies. Antagonistic behavior (AB) consisted of annoys others and blames others.
Other psychopathology
Parents reported an average of 1.29 symptoms (sd=1.4) of CD at baseline, ranging from 0 to 6 symptoms. The reliability alpha for CD symptoms at baseline was poor, at .58. At baseline, parents reported an average of 8.15 symptoms (sd=3.5) of ADHD (range 0 to 14), with a reliability alpha of .83.
Young Adult Self-reported Depression
At age 18, participants were administered the Diagnostic Interview Schedule, including measures of DYS and MD. Participant responses to the symptoms of these disorders were combined in the same fashion as for youth reports. As a measure of adult psychopathology, irritability was not a potential proxy for dysphoric mood. The alpha for these items was .85. Scores ranged from 0 to 9, with a mean of 2.26 (sd = 2.5).
Young Adult Personality
When youth reached age 18, the NEO Personality Inventory (NEO PI-R; Costa & McCrae, 1992) was completed via self-report. This measure assesses the “Big Five” personality factors: Neuroticism, Openness, Conscientiousness, Extraversion, and Agreeableness. Neuroticism is a measure of disposition to emotional distress, including fear, sadness, anger, guilt, embarrassment and disgust. Neuroticism scores ranged from 34 to 155 (m = 87, sd = 19.74). Cronbach's alpha was 0.87. This mean score falls in the “High” category (Costa & McCrae, 1992), where domain scores are categorized as being “Very Low,” “Low,” “Average,” “High,” or “Very High.”
The Extraversion domain reflects a disposition to like others, to be assertive, talkative and cheerful (alpha = .85). Scores ranged from 54 to 162 (m = 110, sd = 18.14), falling in the Average category. The Openness domain reflects attentiveness to inner feelings, intellectual curiosity, and an active imagination (alpha = .82). Scores ranged from 70 to 161 (m = 105, sd = 16.9), which is considered Average. Agreeableness items reflect altruistic and sympathetic interpersonal tendencies or, in contrast, disagreeableness is described as an antagonistic, competitive interpersonal style (alpha = .84). These scores ranged from 52 to 146 (m = 103, sd = 17.1), falling in the Low category. Finally, the items of the Conscientiousness scale reflect active self-control, planning, and organization, as well as having a scrupulous and reliable character (alpha = .88). These scores ranged from 37 to 156 (m = 106, sd=19.6), falling in the Low category.
Other covariates
A small set of covariates was included to test for the influence of other factors on psychopathology, including parental psychopathology and demographic factors. A structured diagnostic interview (Endicott & Spitzer, 1978) for DSM-III-R diagnoses of Antisocial Personality Disorder (APD), major depression, and anxiety (generalized anxiety, social phobia, panic disorder, and obsessive compulsive disorder) was used to assess parental psychopathology at baseline. Parent report of their own psychopathology, as well as that of the child's other biological parent, was obtained. At baseline, 26.6% (n=47) reported any history of depression by either parent, 30% (n=53) reported any history of anxiety, and 26% (n=46) reported any history of APD. Demographic covariates included child race as reported by parents, socioeconomic status and parent marital status at baseline.
Analyses
Latent class analysis (LCA) was conducted using Latent Gold (Vermunt & Magidson, 2005). Regression modeling was conducted using Stata (StataCorp, 2009). Specific issues regarding each regression model are detailed in the results. Across models, where repeated waves of data were included simultaneously, correlated observations were accounted for through clustering by participant. Models predicting to outcomes measured repeatedly through adolescence were structured to examine the relationship between predictors at time t and outcomes at time t+1 across each of the 10 waves of data. Where count variables were outcomes, the incidence rate ratio (IRR) statistic is reported. The IRR is the exponentiated beta value for count variable models, and is interpretable in a manner similar to an odds ratio. It indicates the proportional difference in rates of the outcome associated with each unit increase in the predictor. Values greater than one indicate a positive relationship; less than one, an inverse relationship. Where appropriate, predictors were centered about their means in order to reduce multicollinearity. The variance inflation factor (VIF) and tolerance statistics were examined for each model to ensure that multicollinearity was not a concern, using a VIF of 4 or greater as the criterion level.
Results
In order to describe the associations among ODD dimensions at baseline, given that they are count variables, polychoric correlations were estimated. These suggested a high degree of association: Irritability and OB (rho = .58); Irritability and AB (rho = .58) and AB and OB (rho = .66).
Outcomes from childhood through adolescence
Depression
A negative binomial regression model was used, predicting from the dimensions of ODD (Irritability, OB and AB) at time t to parent-reported depression symptoms at time t+1 through adolescence. Only irritability (IRR = 1.34, se = .08, p < .001) predicted depression, while OB (IRR = 1.03, se = .08, p = .66) and AB (IRR = 1.12, se = .12, p = .27) did not. Subsequently, depression, anxiety, ADHD and CD symptoms at time t were tested along with irritability and age as predictors of depression at time t+1. Irritability (IRR = 1.22, se = .07, p < .001), depression (IRR = 1.16, se = .03, p < .001), anxiety (IRR = 1.10, se = .03, p < .001) and age (IRR = 1.06, se = .03, p = 0.23) remained in the model after step-wise removal of non-significant predictors (ADHD: IRR = 1.01, se = .02, p = 0.67; CD: IRR = 1.04, se = .04, p = .31).
The set of demographic and parental psychopathology covariates was then tested in the prediction of depression, controlling for depression symptoms at time t. African American race (inversely related; IRR = 0.67, se = .12, p = .03), parental anxiety (IRR = 1.34, se = 0.19, p = .04) and parental APD (IRR = 1.48, se = 0.23, p = .01) were significant predictors of depression. These were introduced into a final model of predictors of depression, along with irritability, anxiety, depression and age (Table 1). Parental anxiety (IRR = 1.15, se = .17, p = .35) and parental APD (IRR = 1.32, se= .19, p = .06) were removed from the model.
Table 1.
Significant predictors of parent-reported depression symptoms through adolescence.
| IRR | p | 95% confidence interval | ||
|---|---|---|---|---|
| ODD Irritability | 1.24 | <.001 | 1.11 | 1.39 |
| depression | 1.14 | <.001 | 1.08 | 1.21 |
| anxiety | 1.10 | <.001 | 1.05 | 1.16 |
| African American race | 0.67 | 0.02 | 0.47 | 0.94 |
| age | 1.05 | 0.03 | 1.01 | 1.10 |
Note: Predictors in the model were parent-reported symptom counts lagged one year relative to the outcome. ODD = oppositional defiant disorder.
Anxiety
A model predicting anxiety disorder symptoms at time t+1, with only ODD dimensions at time t as predictors, found that both irritability (IRR = 1.23, se = .06, p < .001) and AB (IRR = 1.22, se = .09, p = .006) predicted anxiety, while OB did not (IRR = 1.09, se = .06, p = .14). When anxiety, ADHD, CD, depression at time t and age were included in the model, a step-wise removal of non-significant predictors resulted in irritability (IRR = 1.11, se = .05, p = .01), anxiety (IRR= 1.22, se = .02, p < .001), ADHD (IRR = 1.03, se = .01, p = .01) and age (IRR = 0.97, se = .01, p = .01) remaining in the model. AB was marginally significant (IRR = 1.13, se = .07, p = .05), and was retained for further testing in a final model.
Among the demographic and parental psychopathology covariates, parental anxiety (IRR = 1.31, se = .12, p = .002) and parental APD (IRR = 1.33, se = .12, p = .002) were predictive of anxiety symptoms. A final model tested irritability, AB, anxiety, ADHD, parental anxiety, parental APD and age (Table 2). AB (IRR = 1.12, se = .07, p = .07) was removed from the model.
Table 2.
Significant predictors of parent-reported anxiety symptoms through adolescence.
| IRR | p | 95% confidence interval | ||
|---|---|---|---|---|
| ODD Irritability | 1.13 | .001 | 1.05 | 1.21 |
| Anxiety | 1.20 | <.001 | 1.16 | 1.24 |
| ADHD | 1.04 | 0.003 | 1.01 | 1.06 |
| parental APD | 1.28 | .01 | 1.06 | 1.55 |
| parental anxiety | 1.31 | .004 | 1.09 | 1.57 |
| age | 0.96 | 0.002 | 0.93 | 0.98 |
Note: Predictors in the model were symptom counts lagged one year relative to the outcome. ODD = oppositional defiant disorder, ADHD = attention deficit hyperactivity disorder, APD = antisocial personality disorder.
Prediction from ODD dimensions to outcomes in young adulthood
Self-reported depression symptoms
The prediction from ODD dimensions to self-reported depression symptoms was examined using a negative binomial regression model, again clustering by participant. When all three dimensions were in the model, none were significantly predictive of self-reported depression in adulthood. After stepwise removal, only irritability remained (IRR = 1.15, se = .06, p = .01). Subsequently, other parent reported psychopathology constructs were entered into the model. Irritability was marginally significance (IRR = 1.10, se = .06, p = .08) after accounting for depression symptoms (IRR = 1.06, se = .02, p = .002).
Self-reported Neuroticism
A Gaussian family was specified for a regression model predicting Neuroticism, clustered on participant, with each of the ODD dimensions as predictors. Irritability was significantly predictive of neuroticism (B = 4.05, se = 1.26, p = .001), while OB (B = 1.51, se = 0.98, p = .12) and AB (B = -1.70, se = 1.54, p = .27) were not. Testing a model of child psychopathology, irritability (B = 3.11, se = 1.02, p = .002), depression (B = 0.97, se = 0.39, p = .01) and anxiety (B = 0.97, se = 0.46, p = .0), along with age (B = 0.45, se = 0.22, p = .05) were predictive of neuroticism. CD (B = -0.55, se =.83, p = .50) and ADHD (B = 0.24, se = 0.36, p = .48) were not significant and were removed from the model.
To evaluate whether irritability in childhood was related to a general disposition to difficulty in interpersonal functioning in young adulthood, the specificity of the relationship between irritability and neuroticism was examined after accounting for the other personality factors of agreeableness, extraversion, openness and conscientiousness. Each was, not surprisingly, significantly associated with neuroticism, but their inclusion in the model did not substantially alter the relationship between irritability and neuroticism (B = 2.24, se = 0.86, p = .009). Anxiety also remained significantly predictive of neuroticism (B = 0.72, se = .34, p = .03), while depression was rendered non-significant (B = 0.32, se = .30, p = .29).
Classification in childhood by ODD dimensions
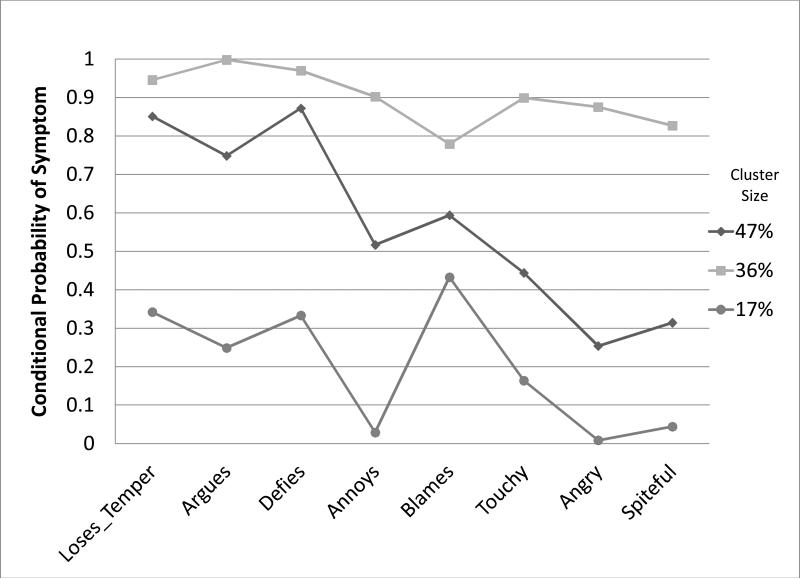
LCA was conducted using parental report of each ODD symptom in Year 1. Based on the model fit indicators, the best fitting model was a 3-class solution. The 2-class solution did not provide an adequate fit for the data (L2 = 192.27, p = .04). Comparing the 3- and 4-class solutions, each of which had acceptable overall goodness of fit (L2=158.41, p = 0.32 versus L2=141.63, p = 0.49, respectively), the AIC (1566.6 versus 1567.8) and BIC (1649.2 versus 1679.0) for each were lower for the 3-class solution, suggesting that it was the better fitting model. Furthermore, a bootstrap test of differences between nested models suggested that the 4-class model was not a significant improvement over the 3-class model (-2LL difference = 16.77, df = 142, p = 0.25), arguing for a 3-class model on the basis of parsimony. Finally, on theoretical grounds, the 4-class solution yielded two groups who differed from one another almost exclusively on the basis of whether or not the symptom of “blames others” was endorsed or not. In contrast, the 3-class model was conceptually consistent with previous evidence for dimensions of ODD (Burke, et al., 2010) where the symptoms of being touchy, angry and spiteful were distinct from losing temper, arguing and defying. For these reasons, a three class solution was selected as the best fitting and conceptually most sound model. The probabilities of symptom endorsement for individuals in each class are shown in Figure 1.
Figure 1.
Latent classes of youth distinguished by ODD symptom probabilities at study year 1.
Individuals were placed into classes based on the estimated posterior probabilities generated using Latent Gold. Analyses using these classifications were conducted keeping in mind the caveat (Collins & Lanza, 2010) that classification based on posterior probabilities is subject to uncertainty. In year 1, 47.5% of youth (class 1, hereafter oppositional behavior (BEH)) were distinguished by a high probability of ODD behavioral symptoms and relatively low negative affect symptoms, and 36.0% were in a class with high probability for behavioral and affective symptoms (class 2, hereafter irritability (IRRIT)). Class 3 (LOW) was low in probability for all symptoms (16.4%). The mean posterior probability estimate for BEH was .86, for IRRIT was .88, and for LOW was .90. An acceptable mean posterior probability of assignment is .7 (Nagin, 1999). Additionally, the odds of correct classification exceeded 5 for each class, suggesting good latent class separation (Collins & Lanza, 2010). Finally, the entropy R2 was .70; values for entropy range from 0 to 1, with values closer to 1 indicating higher certainty of classification.
Predicting from baseline classification through adolescence
Depression symptoms
ODD class was entered as a predictor in a negative binomial regression model, with annual measures (after baseline) of depression symptoms through age 17 as an outcome, clustered by participant. Across waves, youth who were in the IRRIT class at baseline showed a 57% higher rate of depression symptoms (IRR = 1.57, se = .32, p = .03) than the BEH class, and a 124% higher rate of depression symptoms than the LOW class (IRR = 2.24, se = 0.73, p = .014). These values were found after controlling for baseline anxiety symptoms (IRR = 1.12, se = .04, p < .001) and depression symptoms (IRR = 1.17, se = .06, p = .001). CD (IRR = 1.09, se = .06, p = .09) and ADHD symptoms (IRR = 0.96, se = .03, p = .22) were excluded from the model.
Anxiety symptoms
In negative binomial models predicting to anxiety symptoms after baseline through age 17 as an outcome, youth in the IRRIT class showed a 31% greater rate of anxiety symptoms over time than the BEH class (IRR = 1.31, se = .16, p = .03) and a 179% higher rate than the LOW class (IRR = 2.79, se = .60, p < .001). The model was clustered on participant, and included anxiety symptoms at baseline (IRR = 1.15, se = .02, p <.001). Symptoms of depression (IRR = 1.07, se = .04, p = .07), CD (IRR = 1.01, se = .04, p = 0.80) and ADHD (IRR = 1.02, se = .02, p = .24) were removed from the model.
Predicting to young adult outcomes
Self-reported depression symptoms
Self-reported depression symptoms at 18 were 58% higher among those in the IRRIT group (IRR = 1.58, se = .31, p = .02) than the BEH group, and 75% higher among the LOW class (IRR = 1.75, se = .44, p = .03), controlling for depression symptoms (IRR = 1.05, se = .02, p = .01). Symptoms of CD (IRR = 1.00, se = .04, p = .91), ADHD (IRR = 1.01, se = .02, p = .68), and anxiety (IRR = 1.02, se = .02, p = .35) were removed from the model.
Neuroticism
Linear regression models were employed, with latent class membership at Year 1 used to predict Neuroticism at 18. The IRRIT class was specified as the contrast category. Those in the IRRIT class in year 1 were significantly higher in Neuroticism at age 18 than those in the BEH class (B = 10.84, se = 3.37, p = .002), and LOW class (B = 14.12, se = 2.46, p < .001). This effect held after controlling for the other four Big Five personality factors (see Table 3).
Table 3.
Prediction from latent classes at Year 1 to Neuroticism at age 18.
| B | se | t | p | 95% CI | ||
|---|---|---|---|---|---|---|
| Class 1: BEH | -9.30 | 2.65 | -3.51 | 0.001 | -14.52 | -4.07 |
| Class 3: LOW | -11.34 | 2.79 | -4.07 | 0.000 | -16.85 | -5.84 |
| Extraversion | -0.16 | .07 | -2.45 | 0.016 | -0.30 | -0.03 |
| Openness | 0.29 | .08 | 3.75 | 0.000 | 0.14 | 0.44 |
| Agreeableness | -0.31 | .07 | -4.28 | < .001 | -0.45 | -0.16 |
| Conscientiousness | -0.46 | .06 | -7.35 | < .001 | -0.59 | -0.34 |
Note: LCA Class parameters in this model were contrast coded relative to the Irritability class. All personality factors were measured at age 18. BEH = only oppositional behavior symptoms, LOW = low across all oppositional defiant disorder
Subsequently, the symptoms of depression, anxiety, CD and ADHD at year 1 were included in the model. No meaningful change in the parameter values for the contrasts between classes was observed. None of the other measures of psychopathology were themselves significant in the model: CD (B = -0.55, se = 0.81, p = .50), anxiety (B = 0.44, se = 0.36, p = .23), ADHD (B = -.47, se = .34, p = .17) and depression (B = 1.47, se = .78, p = .06).
Further evidence for the specificity of the relationship between classes at baseline and Neuroticism was found in the absence of any predictive relationship between latent classes and any of the other four factors as outcomes when controlling for the remaining personality factors. The parameter values for contrasts between classes in the prediction of these outcomes are shown in Table 4. For the sake of efficiency, the parameter values for each of the other personality domains are not provided in the table.
Table 4.
Prediction from latent classes to other personality factors.
| B | se | t | p | 95% CI | ||
|---|---|---|---|---|---|---|
| Agreeableness | ||||||
| Class 1: BEH | 1.41 | 3.48 | 0.41 | .69 | -5.47 | 8.29 |
| Class 2: IRRIT | 3.20 | 3.74 | 0.86 | .39 | -4.18 | 10.59 |
| Conscientiousness | ||||||
| Class 1: BEH | 2.90 | 3.51 | 0.83 | .41 | -4.03 | 9.83 |
| Class 2: IRRIT | 6.28 | 3.75 | 1.68 | .10 | -1.12 | 13.68 |
| Extraversion | ||||||
| Class 1: BEH | -5.55 | 3.76 | -1.48 | .14 | -12.99 | 1.88 |
| Class 2: IRRIT | -0.58 | 4.07 | -0.14 | .89 | -8.62 | 7.47 |
| Openness | ||||||
| Class 1: BEH | 2.32 | 3.52 | 0.66 | .51 | -4.63 | 9.28 |
| Class 2: IRRIT | -3.35 | 3.78 | -0.89 | .38 | -10.82 | 4.12 |
BEH = only oppositional behavior symptoms, IRRIT = affective symptoms
Discussion
The present analyses extend the existing literature on irritability among ODD symptoms. In a clinically-referred sample of boys, the symptoms of being touchy, angry and spiteful predicted increasing symptoms of depression and anxiety over annual assessments through adolescence, and predicted to young adult self-reported symptoms of depression and Neuroticism. Additionally, the presence of these symptoms also distinguished a class of boys in childhood who were at risk for increased mood, anxiety and Neuroticism through adolescence and young adulthood. Those observed by parents as being high in irritability were themselves likely to describe impairments in mood and personality difficulties as young adults.
Although it was anticipated that a class of youth would be identified as being high in affect and low in behavioral symptoms, this was not the case. Instead, in this data set, two classes of youth with high likelihood of behavioral symptoms were distinguished by the presence of affective ODD symptoms. A third class was low across all symptoms of ODD. As efforts to evaluate revisions to the DSM-V move forward, this finding has significant implications. Foremost among them, it suggests that ODD subtypes are warranted. In this data, ODD with or without irritability was meaningful in terms of describing both distinct groups of children and in terms of their risk for future clinically-oriented outcomes. The present data set is relatively small. It may be the case that additional classes, including one denoted by irritability without behavioral problems, would be observed in a larger data set.
The classes found here were consistent with prior evidence from a community sample of girls (Burke et al., 2010), in that the symptoms of being touchy, angry and spiteful identify irritability. Other research groups (Rowe, et al., 2010; Stringaris & Goodman, 2009b) have found evidence suggesting that the symptom of losing temper functions to identify affectively oriented problems, and that the symptom of being spiteful does not. The consistencies across the literature very robustly suggest that anger and irritability within ODD symptoms are indicative of risk for future affective problems. The differences in indicators across studies are relatively small, but do have important implications. Changes proposed for DSM 5 regarding subgroups of symptoms within ODD indicate the items of losing temper, being touchy and being angry as indicators of affect. The present results would suggest, to the contrary, that such a classification system would potentially reduce the accuracy with which clinicians might predict future mood and anxiety problems. These inconsistencies may be due to differences between samples or assessment methods. Future research should focus on evaluating these dimensions in other data sets, and should evaluate whether additional indicators of irritability would improve its identification and classification among children.
The specificity observed in these findings - with irritability predicting Neuroticism even after controlling for the other four personality factors at age 18 - indicates that rather than a general risk across outcomes, irritability poses circumscribed risks. This is consistent with prior studies that have found a lack of prediction from irritability to borderline personality disorder (Burke & Stepp, 2012) and to bipolar disorder (Brotman et al., 2006). The present results indicate that irritability is not particularly related to personality features of disagreeableness, conscientiousness, openness, or extraversion. Further research will be needed to more fully disentangle evidence for outcomes related to the presence of persisting irritability in childhood and adolescence.
Although it remains possible that the distinction between the IRRIT and BEH class is a function of symptom severity rather than content, the results tend to suggest otherwise. First, the latent classes observed here did not suggest differences of low, medium and high severity across all symptoms, but showed that some children overlap in behavioral problems while showing low levels of irritability. Secondly, the variable-oriented analyses demonstrated that mood and anxiety problems change in accord with changes in irritability, but not with behavioral symptoms. Finally, accounting for levels of other psychopathology, which might be anticipated to vary in accord with ODD severity, did not alter the relationship between irritability and mood, anxiety and personality outcomes. There appears to be a particular link in terms of the affective content of these items rather than the overall severity of ODD symptoms.
Although not testable in the present data, the results are consistent with a developmental model in which indicators of irritability emerge early in development, persist over time, and presage elevated levels of anxiety and depression. Previous evidence for such a developmental model includes the finding that temperamental emotionality early in childhood helps to distinguish a developmental progression towards ODD comorbid with internalizing disorders, in contrast to temperamental activity to ODD comorbid with ADHD (Stringaris, Maughan, & Goodman, 2010). It may be that the children in the latent class noted by the presence of irritability are those who would have been measured high in temperamental emotionality, were such data available here. If anxiety and depression are seen as reflective of maladaptive coping strategies, perhaps chronic irritability is indicative of a diathesis to such outcomes. Further research should focus on measuring and distinguishing between irritability, NA, depression, anxiety and temperamental dysregulation from earlier points in development. Additionally, examination of evidence at the level of genetics or neurological functioning will help to evaluate whether phenotypic distinctions based on irritability have any biological basis.
Limitations
The present analyses must be regarded with recognition of a number of limitations. First, the present sample includes only boys. Although evidence suggests overall consistency with the results from a study of ODD in girls (Burke et al., 2010), further work is needed to know how well the present findings would generalize across gender. Secondly, the present sample was recruited from clinic referral, and is over-representative of behavioral problems. While this is a desirable feature for the evaluation of questions pertinent to clinical functioning and prognosis, it is a limitation in regards to the degree to which the present results represent the population of youth as a whole. Additionally, the relatively small sample size may have limited the ability to detect significant results. In particular, larger samples would allow a greater possibility of finding meaningful distinctions among a greater number of latent classes of individuals. Finally, as noted, the characterization of diagnoses in the present data were limited both by the absence of information regarding impairment, and by the number of depression and anxiety diagnoses measured. In particular, the present data included measurements only of OAD and SAD. Not only would the measurement of other anxiety disorders likely increase rates of comorbidity, but meaningful distinctions are often evident how different types of anxiety disorders relate to other constructs.
Key Points.
Irritability as a dimension within Oppositional Defiant Disorder (ODD) predicts changes in depression and anxiety over short-term and long-term follow up.
Irritability has specific relationships to personality measures, namely predicting Neuroticism but not other Big Five personality domains.
Slight variations across studies exist as to which symptoms best identify irritability; these variations have implications for subtyping ODD as proposed for DSM 5.
Treatment and prevention efforts for affective disorders, as well as behavioral disorders, will be improved through increased awareness of the presence and import of irritability.
Acknowledgements
I am grateful to Dr Rolf Loeber (R.L.) and colleagues for their input into the research program for which the study reported here forms part. This work was supported by grants to J.D.B. (MH074148) and to R.L. (MH42529) from the National Institute of Mental Health.
This work was supported by a grant to Dr. Burke (MH074148), and to Dr. Rolf Loeber, (MH42529), both from the National Institute of Mental Health.
Footnotes
Dr. Burke is with the Western Psychiatric Institute and Clinic at the University of Pittsburgh.
Conflict of interest statement: No conflicts declared
References
- Aebi M, Muller UC, Asherson P, Banaschewski T, Buitelaar J, Ebstein R, Steinhausen HC. Predictability of oppositional defiant disorder and symptom dimensions in children and adolescents with ADHD combined type. Psychological Medicine. 2010;40(12):2089–2100. doi: 10.1017/S0033291710000590. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; Washington, D. C.: 1994. [Google Scholar]
- Brotman MA, Schmajuk M, Rich BA, Dickstein DP, Guyer AE, Costello EJ, Leibenluft E. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry. 2006;60(9):991–997. doi: 10.1016/j.biopsych.2006.08.042. [DOI] [PubMed] [Google Scholar]
- Burke J, Loeber R. Oppositional Defiant Disorder and the explanation of the comorbidity between behavioral disorders and depression. Clinical Psychology-Science and Practice. 2010;17(4):319–326. [Google Scholar]
- Burke JD, Hipwell AE, Loeber R. Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(5):484–492. doi: 10.1097/00004583-201005000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. Journal of Child Psychology and Psychiatry. 2005;46(11):1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- Burke JD, Stepp SD. Adolescent disruptive behavior and borderline personality disorder symptoms in young adult men. Journal of Abnormal Child Psychology. 2012;40(1):35–44. doi: 10.1007/s10802-011-9558-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100(3):316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Collins LM, Lanza ST. Latent class and latent transition analysis for the social, behavioral, and health sciences. Wiley; New York: 2010. [Google Scholar]
- Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Archives of general psychiatry. 2009;66(7):764–772. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa PT, Jr., McCrae RR. NEO PI-R professional manual. Psychological Assessment Resources, Inc.; Odessa, FL: 1992. [Google Scholar]
- Costello AJ, Edelbrock C, Dulcan MK, Kalas R, Klaric S. Diagnostic Interview Schedule for Children (DISC) Western Psychiatric Institute and Clinic; Pittsburgh, PA: 1987. [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: the schedule for affective disorders and schizophrenia. Arch Gen Psychiatry. 1978;35(7):837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Garber J, Weersing VR. Comorbidity of Anxiety and Depression in Youth: Implications for Treatment and Prevention. Clinical Psychology-Science and Practice. 2010;17(4):293–306. doi: 10.1111/j.1468-2850.2010.01221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibenluft E, Cohen P, Gorrindo T, Brook JS, Pine DS. Chronic versus episodic irritability in youth: A community-based, longitudinal study of clinical and diagnostic associations. Journal of Child and Adolescent Psychopharmacology. 2006;16(4):456–466. doi: 10.1089/cap.2006.16.456. [DOI] [PubMed] [Google Scholar]
- Loeber R, Green SM, Lahey BB, Frick PJ, McBurnett K. Findings on disruptive behavior disorders from the first decade of the Developmental Trends Study. Clin Child Fam Psychol Rev. 2000;3(1):37–60. doi: 10.1023/a:1009567419190. [DOI] [PubMed] [Google Scholar]
- Loeber R, Green SM, Lahey BB, Stouthamer-Loeber M. Optimal informants on childhood disruptive behaviors. Development and Psychopathology. 1989;1:317–337. [Google Scholar]
- Puig-Antich J. Major depression and conduct disorder in prepuberty. J Am Acad Child Psychiatry. 1982;21(2):118–128. doi: 10.1016/s0002-7138(09)60910-9. [DOI] [PubMed] [Google Scholar]
- Rowe R, Costello EJ, Angold A, Copeland WE, Maughan B. Developmental pathways in oppositional defiant disorder and conduct disorder. Journal of Abnormal Psychology. 2010;119(4):726–738. doi: 10.1037/a0020798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 11. StataCorp LP; College Station, TX: 2009. [Google Scholar]
- Stringaris A, Cohen P, Pine DS, Leibenluft E. Adult outcomes of youth irritability: a 20-year prospective community-based study. Am J Psychiatry. 2009;166(9):1048–1054. doi: 10.1176/appi.ajp.2009.08121849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris A, Goodman R. Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. J Am Acad Child Adolesc Psychiatry. 2009a;48(4):404–412. doi: 10.1097/CHI.0b013e3181984f30. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Goodman R. Three dimensions of oppositionality in youth. J Child Psychol Psychiatry. 2009b;50(3):216–223. doi: 10.1111/j.1469-7610.2008.01989.x. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Maughan B, Goodman R. What's in a Disruptive Disorder? Temperamental Antecedents of Oppositional Defiant Disorder: Findings from the Avon Longitudinal Study. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(5):474–483. doi: 10.1097/00004583-201005000-00008. [DOI] [PubMed] [Google Scholar]
- Vermunt JK, Magidson J. Latent GOLD 4.0 User's Guide. Statistical Innovations Inc.; Belmont, MA: 2005. [Google Scholar]
- Watson D. Mood and temperament. Guilford Press; New York: 2000. [Google Scholar]
- Watson D, Clark LA. Negative Affectivity - the Disposition to Experience Aversive Emotional States. Psychological Bulletin. 1984;96(3):465–490. [PubMed] [Google Scholar]
- World Health Organization . ICD-10 Classifications of Mental and Behavioural Disorder: Clinical Descriptions and Diagnostic Guidelines. World Health Organization; Geneva: 1992. [Google Scholar]