Abstract
End stage renal disease impacts many Americans, however, transplant is the best treatment option increasing life years and offering a higher quality of life than possible with dialysis. Ironically, many who are eligible for transplant do not follow through on the complex work-up protocols required to be placed on the transplant waiting list. Here we surveyed vascular access clinic patients at an academic medical center referred for transplant that did not follow up on the needed work-up to be added to the national transplant waiting list. The most frequent responses of 83 patients for not pursuing transplantation were that the patients did not think they would pass the medical tests, they were scared of getting a transplant, and they could not afford the medicine or the transplantation. These impediments may result from unclear provider communication, misinformation received from peers or other sources, misperceptions related to transplant surgery, or limited health literacy/health decision making capacity. Thus, patients with end stage renal disease lost to follow up after referral for kidney transplant faced both real and perceived barriers pursuing transplantation.
Keywords: Lost to follow up, ESRD, Access to Kidney Transplant, Barriers to Transplant
Introduction
Kidney disease is a prevalent and expensive disease that affects nearly 5.5 million Americans. Kidney transplantation is the standard of care for many patients with end stage renal disease (ESRD), and has been found to be significantly more effective in improving patient quality of life, physical functioning, and psychosocial functioning (1). Since 1988, the prevalence of both dialysis patients and transplant patients with ESRD has tripled (2). The cost to treat kidney disease is high, and may be increasing as the population ages and medical care costs escalate. More than 400 000 Americans required dialysis or kidney transplant in 1999, and the Medicare expenditure for kidney disease was $11 billion during this year (3).
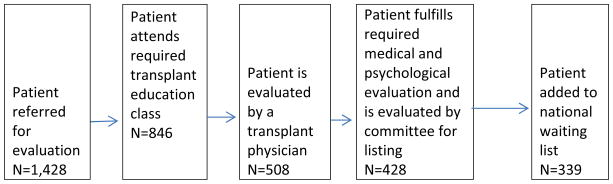
A single kidney transplant center serves all patients in South Carolina (SC). Patients in SC who are referred for transplant are required to attend a transplant education class as part of the pre-transplant evaluation process. These classes are held in different geographic locations (upstate, midlands, low-country) and at different time points throughout the month. In addition to attending the educational session, the patient is required to complete various medical and psychosocial evaluations and tests based on CMS regulations and transplant center protocol prior to being placed on the transplant waiting list. The criteria for being listed for a kidney transplant in SC are provided in Figure 1, along with the number of patients who completed each step in 2010. This figure illustrates the number of patients that are lost at each step, and only 29.5% of those referred are eventually listed for transplant. The process is monitored for each patient, and any lack of patient follow through is communicated to the patient, the dialysis units and to the referring community nephrologist. The methods of communication include visits to the vascular access clinic, mailings from the transplant center, and phone calls to the patients. Despite this well-structured system of communications, a large number of patients do not progress through the process to fulfill the requirements for wait-listing for a kidney transplant. In SC, only 16.89% of the dialysis patients who are younger than 70 years of age are on the waiting list for a transplant relative to the 18.15% in Network 6 and 24.23% nationally, indicating that many eligible South Carolina patients are either not referred to transplant or are lost to follow up for a kidney transplant. We define lost to follow up as a patient that does not pursue full evaluation for kidney transplant by not completing required components such as the educational class or medical tests. The purpose of this paper is to identify barriers to kidney transplant for patients who have been referred by a physician for transplant. This group of patients receives dialysis and follow-up on referrals to the clinic for vascular access issues, yet they do not complete the required steps to be listed on the kidney transplant waiting list.
Figure 1.
Steps required for kidney transplant listing (data from 2010)
Results
One hundred and twenty-seven patients met the criteria for inclusion in the study, and responses were received from 83 eligible patients for a response rate of 65.4%. Those that did not provide responses either declined to participate or did not show up for their appointment in the vascular access clinic. Of these 83 patients in the sample, 49 (59.0%) were female, 31 (37.3%) were male, and three (3.6%) did not answer the gender question. For race, 66 (79.5%) were African American, and twelve (14.5%) were white with the remaining being Hispanic, Other, or did not answer. Fifty-five (66.3%) of the patients were married, while 25 (30.1%) were not, and three (3.6%) did not answer. The age of the patient sample ranged from 20–78 years with the mean being 53.5 years. The mean number of months on dialysis was 70.4 (5.8 years) with a range of 0–216 months. The average drive time to the transplant center was 68.5 minutes with a range from 5–180. The majority of the patients reported that they did not live in a rural area (n=55 or 66.3%). These descriptive statistics are reported in Table 1. For comparison of characteristics, we used information of about waitlisted patients from internal data and the Scientific Registry of Transplant Recipients from the same time period (SRTR 7/1/2010-6/3/2011) to identify similiarities or differences between those waitlisted and those that were lost to follow up and found that a majority of waitlisted patients were in the same age range as lost to follow up patients (50–64 years), a majority of waitlisted patients were also African American (55.6%), and a majority of waitlisted patients were also married (51.0%). We find that a majority of those waitlisted were males (55.6%) while a majority of those lost to follow-up were females (59.0%).
Table 1.
Descriptive Statistics of Lost to Follow Up Versus
| Mean (s.d) | Minimum | Maximum | Total | |||
|---|---|---|---|---|---|---|
| Age (years) | 53.46 (14.16) | 20 | 78 | 83 | ||
| Time to Transplant Center (minutes) | 68.51 (49.13) | 5 | 180 | 80 | ||
| Time on Dialysis (months) | 70.42 (62.52) | 0 | 216 | 79 | ||
| Yes | No | No Answer/Not sure | Total | |||
| Married | 25 (30.1%) | 55 (66.3%) | 3 (3.6%) | 83 | ||
| Rural Area | 24 (28.9%) | 55 (66.3%) | 4 (4.8%) | 83 | ||
| Doctor Ever Talk To You about Transplant | 71 (85.5%) | 9 (10.8%) | 3 (3.6%) | 83 | ||
| Did you attend the class | 32 (38.6%) | 47 (56.6%) | 4 (4.8%) | 83 | ||
| Were you ever evaluated for Transplant | 35 (42.2%) | 39 (47.0%) | 5 (10.8%) | 83 | ||
| Male | Female | No Response | Total | |||
| Gender | 31 (37.3%) | 49 (59.0%) | 3 (3.6%) | 83 | ||
| Black | White | Hispanic | Other | No Answer | Total | |
| Race/Ethnicity | 66 (79.5%) | 12 (14.5%) | 1 (1.2%) | 1 (1.2%) | 3 (3.6%) | 83 |
A large majority (n=71 or 85.5%) reported that a doctor had talked to them about transplantation. Nine patients (10.8%) said a doctor had not talked to them about transplant, two were unsure, and one did not answer. When asked when the doctor spoke to them about transplant, 43 (51.81%) did not answer or recall. The majority of respondents who provided an answer said it had been more than five years (12 patients, 15.7%). The next most frequent response was 2–5 years (11 patients, 13.3%). Seven patients (8.4 %) said their doctor spoke to them about transplant a year ago, and three (3.6%) said less than a year ago. Only six patients (7.2%) stated that their doctor had talked to them about transplant on more than one occasion.
To determine if the patients had taken any steps in pursuing a kidney transplant, they were asked if they had attended a mandatory transplant education class at one of the transplant center locations. A majority (47 patients 56.6%) had not, while thirty-two patients (38.6%) had attended. One patient (1.2%) was not sure if he/she had attended, and three (3.6%) did not answer. Respondents were then asked if they had seen a doctor to be evaluated for transplant at our center. Again, the most frequent response was no, (39 patients 47.0%), following by yes (35 patients, 42.2%), followed by not sure (8 patients, 9.6%). One patient did not answer (1.2%).
When asked why the patients had not pursued transplant, a variety of answers were given. Since patients were encouraged to select or provide all reasons that applied, there were multiple responses for each individual, thus the percentages reported are greater than 100%. The most frequent response was “I did not think I would pass the medical tests,” (15 patients 18.1%). The second most frequent response was, “Scared of getting a transplant,” (13 patients 15.7%) followed by “Cannot afford transplant or medicines” (12 patients 14.5%), and “Dialysis is not that bad” (11 patients 13.3%). Nine patients (10.8%) were “not sure how to proceed,” and eight (9.6%) were “worried about how long the wait for a kidney would be.” Seven patients (8.4%) reported that they, “did not believe anyone would serve as a living donor for me,” “Did not have money or transportation to get to transplant center for tests,” and “did not understand the transplant process.” The least frequent responses with five patients each (6.0%) were that they, “do not understand the benefits of transplantation” and that the process, “did not fit their schedule.” These frequencies are presented in Table 2.
Table 2.
Frequencies of barriers to transplantation
| Barrier/Reason for Not Following Up | N (%) |
|---|---|
| Did not think I would pass medical tests | 15 (18.1%) |
| Scared of getting transplant | 13 (15.7%) |
| Cannot afford transplant or medicines | 12 (14.5%) |
| Dialysis not that bad | 11 (13.3%) |
| Not sure how to proceed | 9 (10.8%) |
| Worried about how long wait for a kidney would be | 8 (9.6%) |
| Did not believe anyone would serve as a donor for me | 7 (8.4%) |
| Did not have money or transportation to get to transplant center for tests | 7 (8.4%) |
| Did not understand the transplant process | 7 (8.4%) |
| Do not understand the benefits of transplantation | 5 (6.0%) |
| Did not fit my schedule | 5 (6.0%) |
Respondent patients were also offered a narrative response category to provide other reasons that they had not pursued transplant. More than half the respondents (43 patients) provided information in this field. While some of the responses were similar to choices given, others provided new reasons that we had not considered for not pursuing a kidney transplant. Several listed specific medical reasons including need for tooth extraction, need to have a catheter put in the chest at that time, having bipolar disorder, being overweight and unwilling to lose weight, being pre-myeloma, or that infection is too bad. Others reported that they did follow up on transplant and did not give further information about where they were in the process. Given the selection criteria, this seems an unlikely response, thus these patients may believe that they followed up, but most likely did not understand the next step in the process that they needed to accomplish. Three patients provided comments that indicated that they believed they were too old for a transplant and preferred that a kidney be offered instead to a younger person. A few respondents blamed physicians either by name or by city of practice (i.e. “Georgetown doctor”) or stated that they had not gotten a referral. A few indicated that they had already had a transplant that failed or that they had been listed but were removed from the list for various reasons (i.e. amputation). Others provided additional details about their fear of transplant including, “heard the horror stories of rejection of kidneys and needing multiple transplants,” and “people tell me that even with a transplant you end up back on dialysis,” or “scared of transplant failing.” Others provide additional information about their confusion about how to proceed including, “I have thought about it but I don’t know how to get the whole thing started.” Others indicated that they were in various stages of the process and that they, “haven’t attended the class yet,” or that “I need three more appointments for completion (psychiatry, colonoscopy, stress test).” Some indicated they either forgot about the appointment or that they had dialysis at the time of the class. One indicated that he/she planned to call to make an appointment, indicating the survey may have served as a reminder. One patient claimed to have been on the waiting list for 15 years, but not in South Carolina. Finally, others seem to blame the system for their lack of knowledge of how to proceed including “never received information about a transplant,” “never was talked to or introduced about a transplant,” and “they seem to be making it harder to get transplant.”
To test for patterns of statistical significance, we used Chi-square analysis to determine if respondents who had attended the transplant education class were less likely to report any particular reasons for not pursuing transplant. We did not identify any patterns or relationships of statistical significance, indicating that those who attended the class were not any more or less likely to face certain barriers or misinformation about transplant.
Discussion
Previous studies have examined the barriers to evaluation and listing for kidney transplantation. Schold and colleagues reported that older age, lower median income, and noncommercial insurance were associated with decreased likelihood for kidney transplant and listing (4). This same study reported that disparities in race and ethnicity are largely explained by the aforementioned factors. Another study found significant differences in the waiting list registration rates, relative transplant rates, and waiting times for transplant patients who were living in rural versus urban locations (5). We sought to identify individual barriers to kidney transplantation not previously identified by surveying patients who were referred for kidney transplant evaluation, but who never followed up on the referral.
As of July 29, 2011, there were 312 whites, 600 African Americans, eight Hispanics, 13 Asians, and three American Indian/Alaska Native on the waiting list for a kidney transplant in South Carolina (6). Given these numbers, our study patients who are lost to follow up appears to be approximately representative to the waiting list given that African Americans make up the greatest number of ESRD patients in South Carolina and the greatest number of those on the waiting list for a kidney transplant. Without knowing the exact number and characteristics of all eligible patients not on the waiting list, it is difficult to identify if our sample is completely representative, but we have sampled patients given the demographic information we do have about our population. Previous research has shown that there are racial and ethnic disparities in kidney transplant and organ donation, but these factors may be reduced through education (7). Because of the high percentage of African Americans with ESRD in South Carolina, we sought to oversample this population to identify barriers to kidney transplant.
The main finding of our study is that the most frequent reason that patients are lost to follow-up is that they do not believe they will pass the required medical tests. While there are medical reasons for not listing patients for a kidney transplant, it appears as though many patients are self-selecting out for perceived medical contraindications to transplant. Given that the criteria for transplant and listing are constantly evolving and vary from center to center, it is essential that physicians be the ones to make the decision as to whether or not patients are medically eligible for transplantation. It is likely that patients have heard rumors of eligibility from doctors in the community, from peers at their dialysis centers, or from other ESRD patients. Dispelling such rumors and providing accurate information is essential, and patients should be told that they are being referred because they might be eligible for transplant and that the only way to find out is to complete the process.
Second, there is a great deal of patient fear about transplantation. Patients have fear of both the surgery and the follow up and believe, in some cases, that transplant is not effective or that it will fail. While this is a possibility, presenting an accurate picture of life after kidney transplant is necessary and should be the responsibility of the transplant center to ensure accuracy of patients’ understanding. Although our transplant center conducts small group patient education classes in the community it is likely that the fear of transplant is perpetuated because patients in dialysis units are more likely to see post-transplant patients whose grafts have failed than those who are doing well. This may skew the perception of patients. Transplant centers or dialysis units may wish to invite healthy post- transplant patients to visit and share an alternative perspective. A network of support groups in the communities can perhaps address many of the transplant related concerns and address most of the fears of dialysis patients.
Third, patients frequently reported that they did not have the money for transportation or evaluation for transplantation. Schold et al reported similar results of lower listings in lower income and non commercial insured group of patients (4). These barriers may be addressed through outreach clinics that allow patients to be seen in their own communities so that significant travel is not required in states where only one transplant center exists. Additionally, support that allows these patients to activate and use their Medicaid and Medicare eligibility to seek care may also be warranted. Such support may require more active involvement of social workers or the addition of patient navigator services.
Many of the patients indicated that they were uncertain about the process of transplantation, the requirements for listing, their own eligibility, and where they were in the process. Some of the patients that had been referred stated that their physicians had never talked to them about transplant, when in fact they had been referred. Only 6% of patients recalled that the doctor had discussed transplant with them on more than one occasion, and for the vast majority the discussion was almost five years ago. This indicates poor communication between physicians and patients is present. This may be the result of communication styles or channels or the health literacy of patients. Furthermore, a lack of understanding of the overall process should be addressed by improved education. While our transplant center has sought to decrease confusion about the process and requirements for listing, we did not find any significant differences in barriers between those who did and did not attend the education class. Our education classes have been modified based on feedback surveys from attendees. However it is evident that the current education sessions are not meeting patients’ information needs. Patients may be at different stages of learning and many patients may require a modified program tailored to suit their health literacy levels. Additionally, our program has sought to provide patients with multiple reminders (at least three) about requirements still pending for their evaluation as well as accessible coordinators to schedule appointments for the clinic. This may be especially important due to scheduling difficulties that patients may face at large medical centers, and our survey showed that only five (6.0%) patients identified scheduling as an issue in being lost to follow up.
Of the patients included in the study, thirty-five (42.2%) reported that they had been evaluated for transplant by a doctor at the transplant center, and thirty-two (38.6%) reported that they had attended the required educational class. This group, nearly a majority, represents a group that took some steps in the direction of being listed. Whether they were overwhelmed at the requirements for being listed or more fearful after learning about the process is not clear. Again, additional support such as that of a patient navigator may help patients better fulfill the requirements for listing.
ESRD is a highly prevalent illness. Various treatments including dialysis and transplantation are available, but the benefits and processes are difficult for patients to understand and navigate. We find that the most barriers to follow up and listing for patients who have been referred are the result of misunderstanding, misinformation, or fear. Additional outreach and education for these patients at an appropriate health literacy level may reduce these barriers by providing accurate information in ways the patients can understand.
Given the poor rate of listing in South Carolina (16.89% of Dialysis Patients < 70 years), steps must be taken to address barriers to follow up for patients who are referred for transplant. Our study provided a unique contribution in that is identified and examined individual barriers to pursuing transplant evaluation in a sample that is likely eligible for kidney transplant. Despite this eligibility, many patients do pursue dialysis access perhaps out of necessity, but do not follow through on the steps to be placed on the kidney transplant wait listing.
Our study has some limitations. We examined only responses from SC patients, thus our findings may not be relevant to other programs, and our generalizability may be limited. Additionally, there is possible selection bias in patients since we collected information from patients at a single center/clinic setting. However, since we have a unique population, we also have an opportunity to reach these lost to follow-up patients through our affiliated vascular access clinic. This means that we should be able to measure the effect of any interventions that we will undertake in response to the issues raised by this study. One challenge of studying those who are lost to follow-up is that they generally cannot be located. Our study provides a rare glimpse into the barriers, both real and perceived, that are facing this population. Also, while not explicitly stated, patients at our center have the option of either being added to the national waiting list or pursuing living donation. Therefore, patients who are lost to follow up have not pursued the required tests and steps to pursue either option. Another possible weakness is the recall bias that patients may have about their own care, particularly related to when events occurred such as a doctor talking to them about transplantation. Finally, while there may be racial differences in the rates and reasons for being lost to follow up, we do not explicitly explore this in our current study. Given the population served at our center and the sample for this study, we do not have a representative sample and statistical power to explore this area.
Future studies should consider examining the role of individual patients’ health literacy level and their stage of learning in the area of transplant. The transplant process is complex, and the benefits and steps to pursue being added to the waitlist can be confusing and overwhelming. Interventions to individualize the education process rather than the one step that fits all would be of particular value. Future research may also examine the presence of racial disparities in lost to follow up status and whether there are racial differences in reasons for being lost to follow up. Finally, a similar study could be conducted in which individuals who were successfully transplanted can provide information about how they overcame barriers (e.g. family support, understanding of illness, information about ESRD).
Methods
An expert panel of six clinicians and researchers developed a set of questions to explore issues of barriers to transplantation. The experts were selected because of their advanced training (MD and/or PhD) in kidney transplant or health services research as well as their experience in the field of kidney transplant surgery, treating ESRD patients, or the design of survey questions and qualitative data collection. The survey questions then were piloted tested in key informant interviews to assure that it was clear, complete, of appropriate health literacy level, and would gather the desired information. The key informants were vascular access patients who met our selection criteria by not completing an evaluation for transplant (as described below) and were asked the questions of the survey to ensure that the questions were being properly understood, that the survey was capturing the desired information, and that the categorical responses were inclusive of all possibilities.
Patients qualified for participation in the study if they had been referred for transplant but: 1) had not attended the required transplant educational class; 2) if they did not respond after three attempts at contact; 3) if they did not complete a component of the medical or psychological testing; or 4) if they refused a transplant by asking that their case be closed for consideration. Each week, the research team would identify patients scheduled to come into the vascular access clinic who met these criteria. The nurses in the clinic would then request that these patients complete the survey. Surveying the patients in vascular access clinic as opposed to the referrals was preferred because we wanted to identify if the barriers to evaluation were individual patient barriers or a function of limited referrals from physicians/nephrologists who did not believe individual patients were candidates for transplant. By surveying the vascular access patients, we believe our sample was more representative. The study was approved by the organization’s IRB, and patients were given letters explaining the purpose of the study and were asked to participate by completing the survey. Survey collection began in December 2009 and ended in June 2011. Responses to the survey were anonymous, but we tracked the characteristics of the cohort of patients who agreed to participate in the study. Thus, the survey responses were not linked to individual patients, but the researchers know the status in the transplant process of the sample as a whole.
The survey asked patients demographic information such as their age, race, gender, marital status, educational status, and whether they lived in a rural areas. Patients were also asked how long they had been on dialysis, if a health care provider ever spoke to them about a kidney transplant and when this discussion took place, whether they had attended the transplant education class, and had been evaluated for a kidney transplant. Patients were then asked why they did not pursue transplantion and were provided a list of choices including: Didn’t think I would pass all medical tests, Didn’t fit my schedule, Did not have transportation or money to get to MUSC for the tests required before transplant, Dialysis isn’t that bad, Scared of getting a transplant, Cannot afford the transplant and/or medicines, Don’t understand the transplant process, Don’t understand the benefits of transplant, Wasn’t sure how to proceed, Didn’t believe anyone would serve as a living donor for me, or Worried how long the wait for a kidney would be plus an open narrative response category. Patients were encouraged to circle all reasons that applied to them. The survey is provided at the end of this manuscript.
The responses were aggregated, coded, and analyzed using SPSS. Descriptive analyses included frequencies, means, ranges, and standard deviations. Additional analyses to detect differences were conducted using chi-square.
Acknowledgments
This work was funded by a grant from NIH/NIDDK “A Program to Increase Living Donations in African Americans.”
Footnotes
Disclosure
The authors do not have any disclosures regarding this work.
Contributor Information
Abby S Kazley, Email: swansoaj@musc.edu, Department of Health Care Leadership and Management, Medical University of South Carolina, 151 Rutledge Avenue, Charleston, SC 29464, 843-792-0012.
Kit N. Simpson, Department of Health Care Leadership and Management, Medical University of South Carolina.
Kenneth D. Chavin, Transplant Surgery, Medical University of South Carolina.
Prabhakar Baliga, Transplant Surgery, Medical University of South Carolina.
References
- 1.Landreneau K, Lee K, Landreneau MD. Quality of life in patients undergoing hemodialysis and renal transplantation—a meta-analytic review. Neprhology Nursing Journal. 2010;37(1):37–44. [PubMed] [Google Scholar]
- 2.USRDS Annual Data Report. http://www.usrds.org/adr.htm. Retrieved August 8, 2011.
- 3.Brown WW, Peters RM, Ohmit SE, Keane WF, Collins A, Chen SC, King K, Klag MJ, Molony DA, Flack JM. Early detection of kidney disease in community settings: the Kidney Early Evaluation Program (KEEP) American Journal of Kidney Diseases. 2003 Jul;42(1):22–35. doi: 10.1016/s0272-6386(03)00405-0. [DOI] [PubMed] [Google Scholar]
- 4.Schold JD, Gregg JA, Harman JS, Hall AG, et al. Barriers to evaluation and wait list for kidney transplantation. Clin J Am Soc Nephrol. 2011;6(7):1760–7. doi: 10.2215/CJN.08620910. [DOI] [PubMed] [Google Scholar]
- 5.Axelrod DA, Guidinger MK, Finlayson S, Schaubel DE, Goodman DC, Chobanian M, Merion RM. Rates of solid-organ waiting-list, transplantation, and survival among residents of rural and urban areas. JAMA. 2008;299(2):202–7. doi: 10.1001/jama.2007.50. [DOI] [PubMed] [Google Scholar]
- 6.OPTN. http://optn.transplant.hrsa.gov/latestData/stateData.asp?type=state Retrieved August 8, 2011.
- 7.Goldfarb-Rumyantzev AS, Sandhu GS, Baird B, Barendbaum A, et al. Effect of education on racial disparities in access to kidney transplantation. Clin Transplant. 2010 doi: 10.1111/j.1399-0012.2010.01390.x. [DOI] [PubMed] [Google Scholar]