Abstract
Objective
To evaluate quantitatively articles that compared effects of second and third generation oral contraceptives on risk of venous thrombosis.
Design
Meta-analysis.
Studies
Cohort and case-control studies assessing risk of venous thromboembolism among women using oral contraceptives before October 1995.
Main outcome measures
Pooled adjusted odds ratios calculated by a general variance based random effects method. When possible, two by two tables were extracted and combined by the Mantel-Haenszel method.
Results
The overall adjusted odds ratio for third versus second generation oral contraceptives was 1.7 (95% confidence interval 1.4 to 2.0; seven studies). Similar risks were found when oral contraceptives containing desogestrel or gestodene were compared with those containing levonorgestrel. Among first time users, the odds ratio for third versus second generation preparations was 3.1 (2.0 to 4.6; four studies). The odds ratio was 2.5 (1.6 to 4.1; five studies) for short term users compared with 2.0 (1.4 to 2.7; five studies) for longer term users. The odds ratio was 1.3 (1.0 to 1.7) in studies funded by the pharmaceutical industry and 2.3 (1.7 to 3.2) in other studies. Differences in age and certainty of diagnosis of venous thrombosis did not affect the results.
Conclusions
This meta-analysis supports the view that third generation oral contraceptives are associated with an increased risk of venous thrombosis compared with second generation oral contraceptives. The increase cannot be explained by several potential biases.
What is already known on this topic
Third generation oral contraceptives have been reported to increase the risk of venous thrombosis compared with second generation oral contraceptives
The findings have been vigorously debated, with suggestions that the results can be explained by confounding or bias, or both.
What this study adds
Women taking third generation oral contraceptives have a 1.7-fold increased risk of venous thrombosis compared with those taking second generation oral contraceptives
Risk is highest in first time users
The biases were not large enough to account for the observed results
Introduction
In 1995-6 increased risks of venous thrombosis were reported among women using so called third generation oral contraceptives compared with second generation products, with odds ratios ranging from 1.5 to 2.2.1–4 Other investigators suggested that confounding, bias, or both, accounted for the findings.5–8 New studies were performed,7,9,10 and many subgroup analyses published,6,11,12 but the debate continues.13 In 1999, Farley et al reported a meta-analysis and found an increased risk of 1.9 (95% confidence interval 1.5 to 2.2).14 However, their aim was to review qualitatively the arguments claiming that the difference in risk for different oral contraceptives is not real. They did not formally consider characteristics of the included studies that might affect their results. In the present meta-analysis we quantified these aspects.
Methods
We searched Medline for articles published from October 1995 to December 2000 using the terms third generation oral contraceptives, desogestrel, and gestodene combined with thromboembolism and venous thrombosis. We retrieved additional references from reviews, other articles of interest, and experts in the field. We reviewed all English language articles containing original data on third generation oral contraceptives and venous thrombosis. Inclusion criteria were (a) cohort or case-control design, (b) cases defined as women with venous thrombosis or thromboembolism, (c) sufficient data provided to reconstruct two by two tables or determine relative risk and confidence intervals, (d) data collected before November 1995, and (e) data collected in Western countries. We chose October 1995 as the end date because at that time four studies were published relating third generation oral contraceptives to venous thrombosis.1–4 Consequently, changes in prescription of oral contraceptives may have potentially affected the results of later studies. To avoid heterogeneity, we included studies in only Western countries.
We systematically abstracted data, resolving ambiguous information through discussion between us. Firstly, we analysed the results of studies that compared the risk of venous thrombosis between third and second generation oral contraceptive users. To assess the influence of different definitions of second and third generation oral contraceptives between studies, we analysed oral contraceptives with specified and unspecified progestagen components separately. Next, we did stratified analyses to explore the patterns of risks in subgroups that may be less or more susceptible to bias. Stratification factors were first time users, age (<25 v ⩾25 years), duration of oral contraceptive use (<1 year v ⩾1 year), confirmed cases, and source of funding (non-industry versus industry sponsored studies explicitly mentioned in the acknowledgement). Cases were considered confirmed when venous thrombosis was objectively diagnosed (by ultrasound examination, plethysmography, or venography). A study was included only once if there were multiple publications. We also did an additional analysis including studies that did not meet the inclusion criteria to determine their effect on the pooled odds ratio.
Some studies reported only frequencies, whereas others reported only unadjusted or adjusted odds ratios. We therefore performed an overall analysis based on the adjusted odds ratios and on the two by two tables separately. We calculated adjusted odds ratios by pooling adjusted odds ratios from individual studies using a general variance based random effects method, weighting individual study results by the inverse of their variance.15 Odds ratios accurately estimate relative risks when risks of disease are small, and we therefore used the same method for case-control and cohort studies.16 We tested homogeneity between studies—that is, the hypothesis that the differences between the reported odds ratios were due only to random error around the true odds ratio. Results were considered heterogeneous when homogeneity was unlikely (P<0.10). To determine the stability of the overall risk estimate, we did a sensitivity analysis in which each study was successively eliminated.
If possible we also extracted or recalculated two by two tables. We combined the odds ratios from the individual studies using the Mantel-Haenszel method,15 providing a crude odds ratio. For subgroup analyses, we pooled adjusted and unadjusted results because of the limited number of studies with subgroup data, resulting in a pooled odds ratio.
Results
Of 114 studies identified, 27 were considered potentially relevant.1–7,9–12,17–32 Ten studies, comprising nine case-control (table 1) and three cohort studies (table 2), examined use of oral contraceptives and risk of venous thrombosis. Three studies provided additional analyses on earlier reported results,6,11,17 and were included in our stratified analysis. Fourteen studies failed to meet one or more inclusion criteria, because they did not contain original data,18–24 included patients after October 1995,12,25–27 or compared third generation oral contraceptives with a combined group of first and second generation oral contraceptives.28–30
Table 1.
Case-control studies of oral contraceptives and the risk of venous thromboembolism
| Author | Study type | Setting | Study period | Study population | Assessment of exposure | Method of ascertainment | % with firm diagnosis | Inclusion criteria | Matching factors | Control factors | Additional and extended studies |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Studies comparing second and third generation oral contraceptives | |||||||||||
| WHO1 | Case- control | Hospital patients in 21 centres worldwide matched with control subjects from same centres | Feb 1989-Jan 1993 | 1143 DVT and PE cases and 2998 controls | All cases and controls interviewed in a standard way by questionnaire. Identification of oral contraceptive type was assisted by showing samples or pictures of locally available formulations | Review of medical history, examination, and investigations | 58% definite, 28% probable, 7% possible, and 8% unspecified (unspecified cases were excluded from analysis) | Women aged 20-44 years with discharge diagnosis of DVT or PE. Those who died within 24 h of admission, who had a history of stroke, DVT, PE, acute MI, or natural or surgical menopause, or who had a recent history of pregnancy (within 6 weeks), major illness causing prolonged bed rest, or surgery were excluded | Age and study centre | Hypertension in pregnancy | |
| WHO31 | Case- control | Hospital patients in 10 centres worldwide matched with control subjects from same centres | Feb 1989-Jan 1993 | 769 VTE cases matched with 1979 hospital controls and 246 community controls (general practice based) | All cases and controls were interviewed in a standard way by questionnaire. Identification of oral contraceptive type was assisted by showing samples or pictures of locally available formulations | Review of medical history, examination, and investigations | 42% definite, 42% probable, 9% possible, and 7% unspecified (unspecified cases were excluded from analysis) | Women aged 20-44 years with discharge diagnosis of DVT or PE. Those who died within 24 h of admission, who had a history of stroke, DVT, PE, acute MI or natural or surgical menopause, or who had a recent history of pregnancy (within 6 weeks), major illness causing prolonged bed rest, or surgery were excluded | Hospital controls: age matched community controls: age and practice matched | Body mass index, alcohol use, varicose veins, hypertension in pregnancy and smoking | Farley17. stratification by duration of use and first time users |
| Jick2 | Nested case- control | General practices in United Kingdom (general practice research database) | 1991-4 | 75 cases of non-fatal VTE and 300 controls who were current oral contraceptive users | Questionnaire to attending general practitioner | Review of medical history (computer records), examinations, and investigations | 64% confirmed and 36% possible cases | Women without a history of venous thromboembolism, stroke, acute MI, cancer, epilepsy, diabetes, treated hypertension, hyperlipidaemia, and cystic fibrosis | Age, general practice and index date of case | Smoking and body mass index | Farmer25. inclusion of patients from 1992-Jun 1997. Jick2. inclusion of patients from Jan 1993 to Dec 1999. Vasilakis27. inclusion of patients to Oct 1996 |
| Bloemenkamp3 | Population based case- control | Three anticoagulant clinics in Netherlands | Jan 1988- Dec 1992 | 126 women with DVT and 159 controls | Interview supplemented by data from hospital discharge letter | Objectively confirmed diagnosis of DVT | 100% | Premenopausal women, aged 15-49, who were at the time of their thrombosis not pregnant, nor in the puerperium, had not had a recent miscarriage, and had not used injectable progestagens | Age, although because of inclusion criteria and age cut-off, many pairs were no longer intact in database. Therefore, analysis was unmatched | Age | |
| Spitzer4 | Hospital and population based case- control | 10 centres in United Kingdom and Germany (transnational study) | 1993-Oct 1995 | 471 cases with venous thrombo- embolism and 1772 controls | Personal interviews. Exposure to oral contraceptives was confirmed by inspecting patients' packets of pills in samples of the cases and controls | Physical examination, imaging procedures, and necropsy reports | 100% | Women aged 16-44 years. The other inclusion and exclusion criteria for both cases and controls are published separately. | Age and hospital or community setting | Age, smoking, alcohol use, study centre, body mass index, and duration of oral contraceptive use | Suissa6. stratification by duration of use among first time users. Lewis11. stratification by age. Suissa24. subgroup analysis in switchers and repeated users; inclusion of patients until 1996 |
| Farmer5 | Nested case- control | General practices in United Kingdom (MediPlus database) | Sept 1991-Sept 1995 | 83 cases with VTE or PE and 313 controls who were current oral contraceptive users | Information from medical records | Recorded diagnosis of DVT or PE and treatment with anticoagulant | ? | Women born between 1941 and 1981, without a previous episode of VTE, a trauma or a surgical operation within the previous 3 months, or were within 3 months of delivery or termination of pregnancy, or had been prescribed “morning-after” oral contraceptives within 4 weeks of the event | Age, general practice | Body mass index, change in type of oral contraceptive within 3 months of event, No of cycles prescribed, previous pregnancy, concurrent disease, and previous use of Shering-PC4 | Todd12. inclusion of patients from Jan 1992 to Mar 1997 |
| Farmer32 | Nested case- control | General practices in Germany (MediPlus database) | Oct 1992 -Sept 1995 | 42 cases with VTE or PE and 168 controls who were current oral contraceptive users | Information from medical records | Recorded diagnosis of VTE or PE and treatment with anticoagulant | Women aged 18-49 years. Patients with superficial venous events, those whose anticoagulant therapy was not related in time to the VTE event, those who did not have a prescription for an oral contraceptive covering the event day, and those who had evidence of a previous episode of VTE were excluded | Age | None. Too few women with body mass index blood pressure, or smoking habits recorded to allow inclusion as possible confounders | ||
| Lidegaard7 | Population based case- control | All Danish hospitals (the national patient register) | 1994-5 | 523 cases and 1074 controls | Postal questionnaire | Computer records based on Danish national patient register. Certainty of diagnosis based on patient's confirmation, diagnostic investigations, and anticoagulant therapy after diagnosis | 62% definite, 34% probable, and 4% uncertain cases | Women aged 15-44 years with a first event of DVT or PE. Pregnant women and women with previous cardiovascular disease were excluded from multivariate analysis. | — | Age, age at first birth, and smoking | |
| Bloemenkamp9 | Case- control | 2 medical centres in the Netherlands | Sept 1982-Oct 1995 | 185 cases with an objective diagnosis of DVT and 591 controls who were referred with the same clinical suspicion but who had no thrombosis | Questionnaire completed by nurse | Clinical evaluation and diagnostic tests | 100% | Women aged 15-49 years. Women without clinical symptoms, with venous thrombosis at sites other than the legs, with a history of DVT or PE, and known to have inherited clotting defects were excluded. Pregnant women and women with malignant neoplasm's were also excluded | — | Age, calendar time, family history of venous thrombosis, study centre | |
| Studies comparing third generation and other oral contraceptives (first and second generation) | |||||||||||
| Andersen28 | Case- control | Regional hospital discharge registries in the counties of North Jutland and Viborg, Denmark | 1977-? | 67 cases with deep venous thrombosis or pulmonary embolism and 134 control women | Information from hospital records | Recorded diagnosis of primary non-fatal VTE. Thrombotic event was confirmed when diagnosed by phlebography, ultrasonograpy, perfusion lung scanning, or echocardiography or when event led to treatment with heparin or anticoagulant | 100% | Women aged 18-49 years without previous episodes of VTE, a VTE related to surgery, trauma, pregnancy, the puerperium, malignancy, immobilisation, chronic inflammatory diseases or heart failure | Age and area of residence | Smoking, body mass index, and parity | |
| Bennet29 | Population based case- control | Regional hospital in Sweden | Jan 1992- Dec 1994 | 27 cases with thromboembolic complications and 16 224 control women | Cases: not described. Controls: statistical information from the Swedish national statistics office | Recorded diagnosis of thromboembolism. Diagnosis was confirmed by intravenous phelebography, pulmonary scintigraphy, or pulmonary angiography | 100% | Women aged 16-47 years. Women taking oral anticoagulants or with malignant diseases were excluded | — | — | |
| Martinelli30 | Population based case- control | Thrombosis centre in Italy | April 1995-April 1998 | 162 cases with a first episode of deep venous thrombosis of the lower extremities and 277 healthy control women | Information on oral contraceptive use recorded at time of thrombosis (for patients) or time of blood sampling (for controls) | Objectively documented episode of deep venous thrombosis | 100% | Availability of DNA. Control women with previous thrombosis were excluded | — | — | |
PE= pulmonary embolism, DVT=deep vein thrombosis, VTE=venous thromboembolism, MI=myocardial infarction.
Table 2.
Cohort studies of oral contraceptives and risk of venous thromboembolism
| Author | Study type | Setting | Study period | Study population | Assessment of exposure | Method of ascertainment | Firm diagnosis | Inclusion criteria | Control factors |
|---|---|---|---|---|---|---|---|---|---|
| Jick2 | Cohort study | General practices in United Kingdom (General Practice Research Database) | Jan 1991-1994 | 238 130 women who were current oral contraceptive users | Information from medical records | Computer records | 64% | Women without a history of venous thromboembolism, stroke, acute myocardial infarction, cancer, epilepsy, diabetes, treated hypertension, hyperlipidaemia, and cystic fibrosis | Age and calendar time |
| Farmer5 | Cohort study | General practices in United Kingdom (MediPlus database) | Sep 1991–Sep 1995 | 491 908 women who were current oral contraceptive users | Information from medical records | Recorded diagnosis of deep vein thrombosis or pulmonary embolus and treatment with anticoagulant | ? | Women born between 1941 and 1981, without a previous episode of venous thromboembolism, trauma, or surgery within past 3 months, or were within 3 months of delivery or termination of pregnancy, or had been prescribed emergency oral contraceptives within 4 weeks of the event | Age |
| Herings10 | Cohort study | Data were obtained from the PHARMO system, which includes information of hospital admissions and drug-dispensing records for all residents of 8 Dutch cities | 1986-95 | All female residents of 8 Dutch cities (about 450 000) | Information from the PHARMO system | Patient's hospital discharge records | ? | Women aged 15-49 years, who had ever used an oral contraceptive during 1986-95, without a history of venous thromboembolism, oral anticoagulants, depots hormone preparations, cardiovascular drugs, emergency contraception, or hospital admission for any reason in the 2 months before start of oral contraceptives | Year and age |
Overall analysis
The overall adjusted odds ratio for third versus second generation oral contraceptives for the risk of venous thrombosis was 1.7 (95% confidence interval 1.4 to 2.0), with no heterogeneity (P=0.78).2–5,7,9,31 In a sensitivity analysis, the adjusted odds ratio varied between 1.6 and 1.8, and the 95% confidence interval never included 1. The crude odds ratio was similar to the adjusted odds ratio (crude odds ratio=1.6, 95% confidence interval 1.3 to 1.9).1–3,4,7,9,32
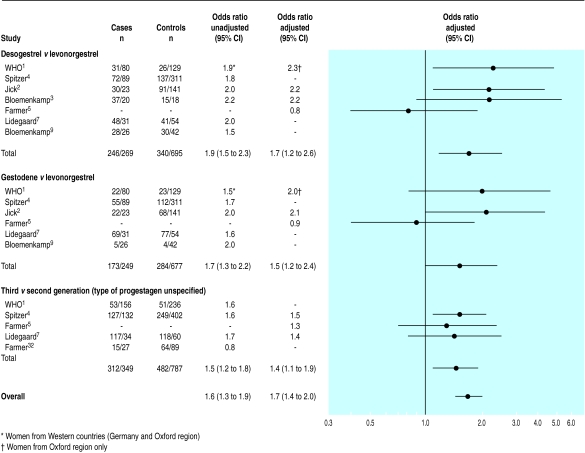
The overall results were not materially dependent on definitions of oral contraceptives (fig 1 ). For all subgroups, crude odds ratios, based on the two by two tables were similar to adjusted odds ratios. In a sensitivity analysis comparing desogestrel with levonorgestrel containing oral contraceptives the adjusted odds ratio varied between 1.6 and 2.2, and 95% confidence intervals never included 1. For gestodene versus levonorgestrel containing oral contraceptives the adjusted odds ratio varied from 1.3 to 2.1 and 95% confidence intervals included 1 twice, and for third versus second generation oral contraceptive use without specifying the progestagen component the adjusted odds ratio ranged from 1.4 to 1.5. The lower boundary of the 95% confidence interval varied between 0.9 and 1.1 and the interval included 1 once.
Figure 1.
Overall odds ratios and 95% confidence intervals for venous thrombosis with different categories of oral contraceptives
Stratified analyses
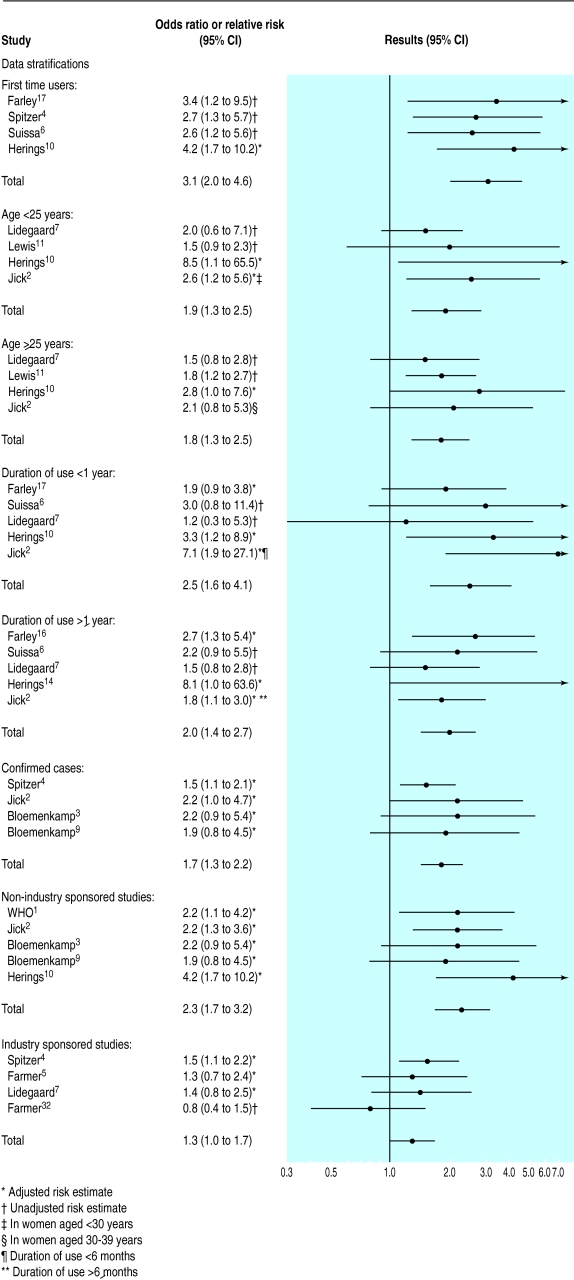
Figure 2 shows that the odds ratio for third versus second generation preparations among first time users was 3.1 (2.0 to 4.6).4,6,10,17 The odds ratio was 2.5 (1.6 to 4.1) for short term users,2,6,7,10,17 and 2.0 (1.4 to 2.7) for longer term users.2,6,7,10,17 Source of funding modified the estimates: the odds ratio was 1.3 (1.0 to 1.7) in studies directly financed by pharmaceutical industries4,5,7,32 and 2.3 (1.7 to 3.2) in other studies.1,2,3,9,10 Differences in age and certainty of diagnosis of venous thrombosis did not affect the results, nor did excluding the cohort study by Herings et al.10
Figure 2.
Effect of patient characteristics on odds ratios or relative risks of third versus second generation oral contraceptives for venous thrombosis
Extended studies
The odds ratio remained essentially the same when the original studies2,5 were replaced by reports updated after October 1995.12,25–27 Three studies compared third generation oral contraceptives with a combined group of first and second generation drugs.28–30 Adding two by two table data from these studies to the overall analysis shown in figure 1 did not change the crude odds ratio (1.6, 1.3 to 1.9).
Discussion
Our meta-analysis shows that third generation oral contraceptives are associated with a 1.7-fold increased risk of venous thrombosis compared with second generation oral contraceptives. After stratifying by various factors and examining selected subgroups, the increased risk remained.
A meta-analysis depends on the quality of the studies included. Observational studies are susceptible to bias because other risk factors of venous thrombosis may be unbalanced across users of second and third generation oral contraceptives. We did not give quality scores to included studies because of their inherent subjectivity and potential to result in diverging summary estimates.33 However, the key elements affecting internal validity (ascertainment, diagnostic and inclusion criteria, exposure assessment, matching, and control factors),34 were listed in the tables and investigated in the stratified and sensitivity analyses.
Quality issue
We believe three issues are important for the quality of our meta-analysis. Firstly, we assessed reliability of outcome by subgroup analysis with confirmed cases only. Secondly, we assessed appropriate adjustment for confounding by comparing adjusted and unadjusted odds ratios and by presenting stratified analyses. The presence of confounding is unlikely because the pooled crude odds ratios were almost equal to the pooled adjusted odds ratios. Source of funding modified the estimates. Some studies provided stratified data only for specific subgroups of women (for example, age in first time users).6,10 Nevertheless, these studies were included. In addition, the sensitivity analysis showed that the overall risk estimates were stable.
Thirdly, we evaluated the quality of assessment of exposure. The definition of second and third generation oral contraceptives was not fully consistent across reports.1,4–32 However, different definitions did not affect the results materially (fig 1). Differential recall of second versus third generation contraceptives is unlikely because most studies collected data before October 1995 or used information from medical records.
Our pooled odds ratios may be underestimates because publication bias can never be excluded. For example, the Dutch press recently reported that a drug company kept results secret that confirmed an increased risk of venous thrombosis with third generation oral contraceptives.35
Another cause of underestimation is that relative risks estimated from the original data are in general lower than those derived from matched regression analysis. However, this cannot be addressed with published data.
Over the past years, the discussion about the findings has concentrated on several potential biases,8,14,36,37 which we recapitulate below.
Healthy user bias
When starting oral contraceptives, women are more likely to receive one of the newer oral contraceptives, whereas older, established users tend to continue with their original brand. New users may include women genetically or otherwise predisposed to venous thrombosis, whereas long term users have shown tolerance to the drug. The predominance of use of new drugs among new oral contraceptive users would create a bias in favour of older products. If true, the difference between second and third generation oral contraceptives should attenuate when first time users are examined separately. This was possible in four studies,4,6,10,17 and, although the definition of first time users differed between the studies, the difference in risk between third and second generation oral contraceptives was higher in this group than in all users.
Recency of introduction bias
Related to possible healthy user bias is the potential for bias due to recency of introduction. Lewis et al argued that there is a relation between the risk of thrombosis and time since a drug's introduction to the market.21 With time, women at a high risk of venous thrombosis stop taking oral contraceptives, leaving a pool of lower risk women taking previously introduced oral contraceptives. However, if depletion of susceptible women distorts the risks for different products, the risk in young women (as a proxy for first time users) should also be analysed. The pooled odds ratio in our meta-analysis showed an increased risk for both younger and older women. Bloemenkamp et al found fourfold to sevenfold increases in risk for use of third versus second generation oral contraceptives among women aged 15-24 years—three to four times higher than the pooled odds ratio we found.3 We could not include Bloemenkamp et al's study in our meta-analysis because no data for a two by two table, relative risk, or confidence intervals were provided.
Duration of oral contraceptive use
A different risk between second and third generation oral contraceptives may reflect lack of adjustment for duration of use.6,7 A reanalysis of the transnational study provided an adjusted rate ratio relative to never users of around 10 in the first year of use, decreasing to around two after two years of use.6 These findings were essentially identical for second and third generation preparations. After correction for duration of use, Lidegaard et al found no significant differences between oral contraceptives with different types of progestagens.7 Our pooled odds ratio stratified by duration of use showed an increased risk for short and long term users. This was most pronounced in women with a short duration of use, again suggesting that young women who take oral contraceptives for the first time are at highest risk.
Diagnostic suspicion and referral bias
Women using third generation oral contraceptives may be more likely to be referred, investigated, and diagnosed with venous thrombosis than users of other oral contraceptives.38 If diagnostic suspicion bias exists, it is likely that the association is diminished among women in whom the diagnosis is so obvious that no clue of oral contraceptive use is needed for diagnosis.36 However, for confirmed cases there was a similar increased risk for women taking third generation oral contraceptives as for those taking second generation formulations. Besides that, the influence of diagnostic suspicion bias would have been stronger in women with less certain diagnosis, because information on use of oral contraceptives might have led to the diagnosis.
Two studies examined risks according to certainty of diagnosis.2,31 Although it was not possible to pool the results since one study did not report the confidence interval, the odds ratios for definite and possible cases remained essentially the same. Moreover, Bloemenkamp et al showed that patients with a clinically confirmed deep vein thrombosis more often used third generation oral contraceptives than patients with the same clinical suspicion who had no thrombosis.9 Therefore, diagnostic bias seems unlikely.
Prescribing bias
Many authors have raised the possibility of selective prescribing of third generation oral contraceptives to high risk women.39–41 Third generation oral contraceptives may have been preferentially prescribed to women with cardiovascular risk factors because of their perceived improved safety profile over second generation oral contraceptives.42 Indeed, patterns of use are different in women with and without cardiovascular risk factors.39–41 However, risk factors screened for at first prescription of oral contraceptives were primarily risk factors for arterial diseases and not for venous thrombosis (that is, tissue damage and haemostatic abnormalities). Moreover, certain genetic markers of venous thrombosis were only recently identified and not widely known at the time women included in the studies were given their oral contraceptives. Furthermore, all studies considered only cases with a first ever venous thrombosis, thus excluding women with a history of venous thrombosis.
Another indicator for genetic predisposition is a family history of venous thrombosis. Two studies addressed this potential confounder, and both showed that increased risks for women using third generation oral contraceptives remained after adjustment.3,9
Switching
Accumulating side effects might lead women to switch their oral contraceptives. This might reflect an increased risk of venous thrombosis.38 One study examined the risk of venous thrombosis among women who switched contraceptives and found an odds ratio of 1.3 (0.7 to 2.4) among those who switched from second to third generation pills relative to those who switched from third to second generation pills,24 although the study recruited until 1996. Women who switched only once had an odds ratio of 1.1 (0.5 to 2.3), whereas those who switched more than once had an odds ratio of 1.8 (0.2 to 16.8). However, the power for subgroup analysis was limited, with large confidence intervals.
Source of funding
The pooled odds ratio of studies without explicitly mentioned industry sponsoring was higher than that of studies without such support, although the increased risk was significant in both groups. Different results for industry and non-industry sponsored studies have also been reported for calcium channel antagonists and non-steroidal anti-inflammatory drugs.43,44
Absolute risks
To appreciate the importance of increases in relative risk, knowledge of absolute risks is required. We estimated that the excess risk for users of third generation oral contraceptives over second generation preparations was 1.5 per 10 000 woman years. This may be an underestimation, because the estimate from the study by Jick et al was confined to cases that met a very strict definition.2 Among new users the incidence is much higher (6.6 per 10 000 woman years).
Death rates from venous thrombosis are low (about 3%),45 although non-fatal events can also have serious effects. We crudely calculated that four deaths per 1 000 000 woman years could be prevented by switching from third to second generation products. Although the risks are small, they should be considered when deciding which oral contraceptive to use.
Conclusion
Our meta-analysis supports the view that third generation oral contraceptives are associated with a 1.7-fold increased risk of venous thrombosis compared with second generation oral contraceptives. The risk is highest in first time users. Although confounding can never be excluded with certainty in observational studies, it seems that the biases that have been suggested and examined are not sufficient to account for the results.
Footnotes
Funding: None.
Competing interests: JMK has worked on a study into second and third generation contraceptives sponsored by the Netherlands Thrombosis Foundation.
References
- 1.World Health Organization Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Venous thromboembolic disease and combined oral contraceptives: results of international multicentre case-control study. Lancet. 1995;346:1575–1582. [PubMed] [Google Scholar]
- 2.Jick H, Jick SS, Gurewich V, Myers MW, Vasilakis C. Risk of idiopathic cardiovascular death and nonfatal venous thromboembolism in women using oral contraceptives with differing progestagen components. Lancet. 1995;346:1589–1593. doi: 10.1016/s0140-6736(95)91928-7. [DOI] [PubMed] [Google Scholar]
- 3.Bloemenkamp KW, Rosendaal FR, Helmerhorst FM, Buller HR, Vandenbroucke JP. Enhancement by factor V Leiden mutation of risk of deep-vein thrombosis associated with oral contraceptives containing a third-generation progestagen. Lancet. 1995;346:1593–1596. doi: 10.1016/s0140-6736(95)91929-5. [DOI] [PubMed] [Google Scholar]
- 4.Spitzer WO, Lewis MA, Heinemann LA, Thorogood M, MacRae KD. Third generation oral contraceptives and risk of venous thromboembolic disorders: an international case-control study. BMJ. 1996;312:83–88. doi: 10.1136/bmj.312.7023.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farmer RD, Lawrenson RA, Thompson CR, Kennedy JG, Hambleton IR. Population-based study of risk of venous thromboembolism associated with various oral contraceptives. Lancet. 1997;349:83–88. doi: 10.1016/s0140-6736(96)07496-x. [DOI] [PubMed] [Google Scholar]
- 6.Suissa S, Blais L, Spitzer WO, Cusson J, Lewis M, Heinemann L. First-time use of newer oral contraceptives and the risk of venous thromboembolism. Contraception. 1997;56:141–146. doi: 10.1016/s0010-7824(97)00119-4. [DOI] [PubMed] [Google Scholar]
- 7.Lidegaard O, Edstrom B, Kreiner S. Oral contraceptives and venous thromboembolism. A case-control study. Contraception. 1998;57:291–301. doi: 10.1016/s0010-7824(98)00033-x. [DOI] [PubMed] [Google Scholar]
- 8.Spitzer WO. The aftermath of a pill scare: regression to reassurance. Hum Reprod Update. 1999;5:736–745. doi: 10.1093/humupd/5.6.736. [DOI] [PubMed] [Google Scholar]
- 9.Bloemenkamp KW, Rosendaal FR, Buller HR, Helmerhorst FM, Colly LP, Vandenbroucke JP. Risk of venous thrombosis with use of current low-dose oral contraceptives is not explained by diagnostic suspicion and referral bias. Arch Intern Med. 1999;159:65–70. doi: 10.1001/archinte.159.1.65. [DOI] [PubMed] [Google Scholar]
- 10.Herings RM, Urquhart J, Leufkens HG. Venous thromboembolism among new users of different oral contraceptives. Lancet. 1999;354:127–128. doi: 10.1016/s0140-6736(99)01257-x. [DOI] [PubMed] [Google Scholar]
- 11.Lewis MA, MacRae KD, Kuhl-Habichl D, Bruppacher R, Heinemann LA, Spitzer WO. The differential risk of oral contraceptives: the impact of full exposure history. Hum Reprod. 1999;14:1493–1499. doi: 10.1093/humrep/14.6.1493. [DOI] [PubMed] [Google Scholar]
- 12.Todd J, Lawrenson R, Farmer RD, Williams TJ, Leydon GM. Venous thromboembolic disease and combined oral contraceptives: a reanalysis of the MediPlus database. Hum Reprod. 1999;14:1500–1505. doi: 10.1093/humrep/14.6.1500. [DOI] [PubMed] [Google Scholar]
- 13.Vandenbroucke JP, Rosing J, Bloemenkamp KW, Middeldorp S, Helmerhorst F, Bouma BN, et al. Oral contraceptives and the risk of venous thrombosis. N Engl J Med. 2001;344:1527–1535. doi: 10.1056/NEJM200105173442007. [DOI] [PubMed] [Google Scholar]
- 14.Farley TM, Meirik O, Collins J. Cardiovascular disease and combined oral contraceptives: reviewing the evidence and balancing the risks. Hum Reprod Update. 1999;5:721–735. doi: 10.1093/humupd/5.6.721. [DOI] [PubMed] [Google Scholar]
- 15.Petitti DB. Meta-analysis, decision analysis, and cost-effectiveness analysis. New York: Oxford University Press; 1994. Statistical methods in meta-analysis; pp. 106–110. [Google Scholar]
- 16.Kleinbaum D, Kupper L, Morgenstern H. Epidemiologic research. New York: Van Nostrand Reinhold; 1982. [Google Scholar]
- 17.Farley TM, Meirik O, Poulter NR, Chang CL, Marmot MG. Oral contraceptives and thrombotic diseases: impact of new epidemiological studies. Contraception. 1996;54:193–198. doi: 10.1016/s0010-7824(96)00166-7. [DOI] [PubMed] [Google Scholar]
- 18.Farmer RD, Todd JC, MacRae KD, Williams TJ, Lewis MA. Oral contraception was not associated with venous thromboembolic disease in recent study. BMJ. 1998;316:1090–1091. [PMC free article] [PubMed] [Google Scholar]
- 19.Farmer RD, Lawrenson RA. Oral contraceptives and venous thromboembolic disease: the findings from database studies in the United Kingdom and Germany. Am J Obstet Gynecol. 1998;179:S78–S86. doi: 10.1053/ob.1998.v179.a92634. [DOI] [PubMed] [Google Scholar]
- 20.Lidegaard O. Smoking and use of oral contraceptives: impact on thrombotic diseases. Am J Obstet Gynecol. 1999;180:S357–S363. doi: 10.1016/s0002-9378(99)70696-4. [DOI] [PubMed] [Google Scholar]
- 21.Lewis MA, Heinemann LA, MacRae KD, Bruppacher R, Spitzer WO. The increased risk of venous thromboembolism and the use of third generation progestagens: role of bias in observational research. Contraception. 1996;54:5–13. doi: 10.1016/0010-7824(96)00112-6. [DOI] [PubMed] [Google Scholar]
- 22.Lawrenson R, Farmer R. Venous thromboembolism and combined oral contraceptives: does the type of progestogen make a difference? Contraception. 2000;62:S21–S28. doi: 10.1016/s0010-7824(00)00147-5. [DOI] [PubMed] [Google Scholar]
- 23.Lewis MA. Transnational study on oral contraceptives and the health of young women. Methods, results, new analyses and the healthy user effect. Hum Reprod Update. 1999;5:707–720. doi: 10.1093/humupd/5.6.707. [DOI] [PubMed] [Google Scholar]
- 24.Suissa S, Spitzer WO, Rainville B, Cusson J, Lewis M, Heinemann L. Recurrent use of newer oral contraceptives and the risk of venous thromboembolism. Hum Reprod. 2000;15:817–821. doi: 10.1093/humrep/15.4.817. [DOI] [PubMed] [Google Scholar]
- 25.Farmer RD, Lawrenson RA, Todd JC, Williams TJ, MacRae KD, Tyrer F, et al. A comparison of the risks of venous thromboembolic disease in association with different combined oral contraceptives. Br J Clin Pharmacol. 2000;49:580–590. doi: 10.1046/j.1365-2125.2000.00198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jick H, Kaye JA, Vasilakis-Scaramozza C, Jick SS. Risk of venous thromboembolism among users of third generation oral contraceptives compared with users of oral contraceptives with levonorgestrel before and after 1995: cohort and case-control analysis. BMJ. 2000;321:1190–1195. doi: 10.1136/bmj.321.7270.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vasilakis C, Jick SS, Jick H. The risk of venous thromboembolism in users of postcoital contraceptive pills. Contraception. 1999;59:79–83. doi: 10.1016/s0010-7824(99)00011-6. [DOI] [PubMed] [Google Scholar]
- 28.Andersen BS, Olsen J, Nielsen GL, Steffensen FH, Sorensen HT, Baech J, et al. Third generation oral contraceptives and heritable thrombophilia as risk factors of non-fatal venous thromboembolism. Thromb Haemost. 1998;79:28–31. [PubMed] [Google Scholar]
- 29.Bennet L, Odeberg H. Resistance to activated protein C, highly prevalent amongst users of oral contraceptives with venous thromboembolism. J Intern Med. 1998;244:27–32. doi: 10.1046/j.1365-2796.1998.00310.x. [DOI] [PubMed] [Google Scholar]
- 30.Martinelli I, Taioli E, Bucciarelli P, Akhavan S, Mannucci PM. Interaction between the G20210A mutation of the prothrombin gene and oral contraceptive use in deep vein thrombosis. Arterioscler Thromb Vasc Biol. 1999;19:700–703. doi: 10.1161/01.atv.19.3.700. [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization Collaborative Study of Cardiovascular Disease and Steroid Hormone Contraception. Effect of different progestagens in low oestrogen oral contraceptives on venous thromboembolic disease. Lancet. 1995;346:1582–1588. [PubMed] [Google Scholar]
- 32.Farmer RD, Todd JC, Lewis MA, MacRae KD, Williams TJ. The risks of venous thromboembolic disease among German women using oral contraceptives: a database study. Contraception. 1998;57:67–70. doi: 10.1016/s0010-7824(98)00002-x. [DOI] [PubMed] [Google Scholar]
- 33.Juni P, Witschi A, Bloch R, Egger M. The hazards of scoring the quality of clinical trials for meta-analysis. JAMA. 1999;282:1054–1060. doi: 10.1001/jama.282.11.1054. [DOI] [PubMed] [Google Scholar]
- 34.Vandenbroucke JP. Scoring the quality of clinical trials. JAMA. 2000;283:1422–1423. [PubMed] [Google Scholar]
- 35.Weber W. Study on risks of third generation pill “kept secret by industry.”. Lancet. 2001;357:779. [Google Scholar]
- 36.Vandenbroucke JP, Helmerhorst FM, Bloemenkamp KW, Rosendaal FR. Third-generation oral contraceptive and deep venous thrombosis: from epidemiologic controversy to new insight in coagulation. Am J Obstet Gynecol. 1997;177:887–891. doi: 10.1016/s0002-9378(97)70289-8. [DOI] [PubMed] [Google Scholar]
- 37.Walker AM. Newer oral contraceptives and the risk of venous thromboembolism. Contraception. 1998;57:169–181. doi: 10.1016/s0010-7824(98)00014-6. [DOI] [PubMed] [Google Scholar]
- 38.Lidegaard O, Milsom I. Oral contraceptives and thrombotic diseases: impact of new epidemiological studies. Contraception. 1996;53:135–139. doi: 10.1016/0010-7824(96)00035-2. [DOI] [PubMed] [Google Scholar]
- 39.Jamin C, de Mouzon J. Selective prescribing of third generation oral contraceptives (OCs) Contraception. 1996;54:55–56. doi: 10.1016/0010-7824(96)00120-5. [DOI] [PubMed] [Google Scholar]
- 40.Van Lunsen HW. Recent oral contraceptive use patterns in four European countries: evidence for selective prescribing of oral contraceptives containing third-generation progestogens. Eur J Contracept Reprod Health Care. 1996;1:39–45. doi: 10.3109/13625189609150654. [DOI] [PubMed] [Google Scholar]
- 41.Lidegaard O. The influence of thrombotic risk factors when oral contraceptives are prescribed. A control-only study. Acta Obstet Gynecol Scand. 1997;76:252–260. [PubMed] [Google Scholar]
- 42.Grobbee DE, Hoes AW. Confounding and indication for treatment in evaluation of drug treatment for hypertension. BMJ. 1997;315:1151–1154. doi: 10.1136/bmj.315.7116.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stelfox HT, Chua G, O'Rourke K, Detsky AS. Conflict of interest in the debate over calcium-channel antagonists. N Engl J Med. 1998;338:101–106. doi: 10.1056/NEJM199801083380206. [DOI] [PubMed] [Google Scholar]
- 44.Rochon PA, Gurwitz JH, Simms RW, Fortin PR, Felson DT, Minaker KL, et al. A study of manufacturer-supported trials of nonsteroidal anti-inflammatory drugs in the treatment of arthritis. Arch Intern Med. 1994;154:157–163. [PubMed] [Google Scholar]
- 45.Farmer RD, Lawrenson RA, Todd JC, Williams TJ, MacRae K. Oral contraceptives and venous thromboembolic disease. Analyses of the UK General Practice Research Database and the UK Mediplus database. Hum Reprod Update. 1999;5:688–706. doi: 10.1093/humupd/5.6.688. [DOI] [PubMed] [Google Scholar]