Abstract
Previous research has linked parents’ social support to decreased child maltreatment but questions remain surrounding the mechanisms explaining this association. Further, it is unclear whether this association applies to support provided by family alone (and not friends), and whether it is moderated by the presence of neighborhood violence. Based on a sample of parents of children aged 3–15 in Chicago, we find that parents’ family support is associated with a lower risk of child maltreatment. This association is partly mediated by reduced parental depression, but only in neighborhoods with average or high levels of violence. In neighborhoods with low levels of violence, the inverse association between family support and maltreatment is equally strong, but it is not mediated by reduced depression.
Keywords: child maltreatment, family relations, social support, maternal depression, neighborhoods
The most recent federal statistics indicate that over three-quarters of a million American children are maltreated annually, and in 80% of cases, parents are the perpetrators (U.S. Department of Health and Human Services, 2010). These figures are based on reported cases of maltreatment, which are assumed underestimates; the prevalence of parent-to-child maltreatment may far exceed rates suggested by official data. The implications of such widespread abuse for the well-being of children are substantial. Child maltreatment has been linked to many adverse outcomes in childhood and beyond, including anxiety, depression, delinquency, aggression, substance abuse, neurocognitive deficits (see Margolin & Gordis, 2000 for a review), and physical health problems (e.g., musculoskeletal problems, respiratory problems, cardiovascular problems; Wegman & Stetler, 2009). Identifying the factors that place parents at risk for child maltreatment is thus essential to promoting healthy development.
Ecological theories of human development (Bronfenbrenner, 1979) suggest that a parent’s propensity to commit maltreatment is shaped at least in part by social context. Indeed, over 30 years ago, Garbarino (1977) observed that families with maltreated children were distinguished by their social isolation, and subsequent studies have largely confirmed these findings (Bishop & Leadbetter, 1999; Sidebotham & Heron, 2006). Complementing this research, a small but growing literature documents positive associations between social support and parenting skills (Ceballo & McLoyd, 2002; Lee, Anderson, Horowitz, & August, 2009; Taylor, Seaton, & Dominguez, 2008), and inverse associations between parents’ social support and child maltreatment (Li, Godinet, & Arnsberger, 2011; Sidebotham & Heron, 2006). However, the mechanisms through which social support protects against child maltreatment are not well understood. Thus, in the present study, we asked whether lower rates of depression among parents mediated associations between support from their families and the maltreatment of their children. Moreover, in keeping with ecological theories that emphasize the interdependence of the contexts in which families live (Belsky, 1984; Bronfenbrenner, 1979; Leventhal & Brooks-Gunn, 2003), we also considered the possibility that the degree of neighborhood violence moderates associations between family support, parent depression, and child maltreatment. These questions are considered in greater detail below.
Social Support, Parent Depression, and Child Maltreatment
Social support is thought to be advantageous for parents facing the challenges of child-rearing, particularly among single and low-income mothers (Ceballo & McLoyd, 2002; Mason, Cauce, Gonzales, Hiraga, & Grove, 1994; Taylor et al., 2008). Accumulating research indicates that social support may even deter parents’ maltreating behaviors. In one study, mothers with a poor social network were nearly twice as likely as others to maltreat their child in the first 6 years of life (Sidebotham & Heron, 2006). In another study, social support from family alone halved the risk of committing child maltreatment among less educated mothers in a poor and minority sample (Li et al., 2011). Social support has also been found to mitigate the effects of stress on child maltreatment (Kotch, Browne, Ringwalt, Dufort, & Rubina, 1997; Muller, Fitzgerald, Sullivan, & Zucker, 1994). Social welfare professionals therefore routinely promote social support as a coping strategy for at-risk mothers (e.g., Richey, Lovell, & Reid, 1991). Little is known, however, about precisely how social support helps parents (Lyons, Henly, & Schuerman, 2005).
We hypothesize that social support may protect against child maltreatment by reducing parental depression. This expectation is based on findings from two bodies of research. The first shows that social support not only has a direct effect on psychological wellbeing (a main effect), but it also has an indirect effect by protecting against the deleterious effects of stress (a buffering effect; Cohen & Wills, 1985). Accordingly, the literature documents inverse associations between parents’ social support and their psychological distress and depression (Brugha et al., 1998; Kalil, Born, Kunz, & Caudill, 2001; Lyons et al., 2005). The support of one’s family, in particular, might play an important role in protecting against depression. Family support may include spousal support, which is a parent’s “first-order support system” (Belsky, 1984, p.90). Indeed, spousal support, relative to friend support, more effectively buffers against stress (Jackson, 1992; Simons, Lorenz, Wu, & Conger, 1993) and promotes wellbeing (Coyne & DeLongis, 1986). The second relevant body of research links mothers’ depression to detrimental parenting behaviors, such as disengagement and hostility (for reviews see Dix & Meunier, 2009; Lovejoy, Graczyk, O’Hare, & Neuman, 2000). Most germane to the present study is the evidence linking maternal depression to child maltreatment (Chaffin, Kelleher, & Hollenberg, 1996; Lyons et al., 2005; Windham et al., 2004).
Taken together, these two strands of research suggest that associations between parents’ lack of social support, particularly family support, and child maltreatment are at least partly mediated by psychological distress. Two studies have already demonstrated that maternal depression mediates associations between social support and parenting behaviors other than maltreatment; however, one study measured social support only outside the immediate family (Simons et al., 1993), while the other included all sources of support (family plus friend; Lee et al., 2009). Prior studies finding direct associations between social support and child maltreatment also included all sources of support (Li et al., 2011; Sidebotham & Heron, 2006). Thus there remain unanswered questions about the unique contribution of family support to child maltreatment, and the intervening role of depression. Therefore the present study tests for an inverse association between parents’ family support and maltreating behaviors, and asks whether it can be explained, at least in part, by their depression.
Neighborhood Violence and Social Support
Ecological models of child maltreatment suggest that the neighborhoods in which families reside shape the family processes that contribute to child maltreatment (Belsky, 1984; Bronfenbrenner, 1979; Garbarino, 1977). There is increasing evidence that neighborhood violence and disorder (often defined as lawlessness and physical decay) influence family functioning in general (Leventhal & Brooks-Gunn, 2003) and child maltreatment in particular (Molnar, Buka, Brennan, Holton, & Earls, 2003). Studies have also documented associations between residence in highly disordered neighborhoods and higher levels of depression and stress (Curry, Latkin, & Davey-Rothwell, 2008; Latkin & Curry, 2003; Mulia, Schmidt, Bond, Jacobs, & Korcha, 2008; Tonorezos et al., 2008). An extension of the family stress model – which posits that parental distress mediates the influence of economic stressors on parenting behaviors (Conger, Ge, Elder, Lorenz, & Simons, 1994; McLoyd, 1998) – may used to integrate these findings. Like economic stressors, neighborhood stressors such as violence and disorder may lead to less optimal parenting behaviors by increasing parental distress (Kotchick, Dorsey, & Heller, 2005).
The role of family support as a buffer against the effects of stress on psychological distress (Cohen & Wills, 1985) may therefore be critically important to parents residing in high-violence neighborhoods. Although it is conceivable that exposure to high neighborhood violence may overwhelm the ameliorative effects of family support on depression, we expect that it is precisely in the most violent neighborhoods where family support will be most protective against depression. Thus, in the present study, we test the hypothesis that neighborhood violence enhances the mental health advantage conferred by family support, thereby enhancing the protective effect of family support on child maltreatment. Prior studies have not, to our knowledge, investigated the extent to which neighborhood violence moderates associations between family support, parent depression, and child maltreatment, but research on a related construct, neighborhood disorder, provides some support for our hypothesis. At least two studies have found that neighborhood disorder enhanced the positive effects of social support on psychological distress (Ajrouch, Reisine, Lim, Sohn, & Ismail, 2010; Cutrona, Russell, Hessling, Brown, & Murray, 2000). Contradictory evidence exists, however; one study found that neighborhood disorder weakened the effect of social support on distress (Rajaratnam, O’Campo, O’Brien, Muntaner, & Muntaner, 2008) and two others found no moderating role for disorder (Fagg et al., 2008; Mulia et al., 2008). We thus acknowledge the uncertainty in our expectation that neighborhood violence will strengthen the inverse link between family support and depression.
The Present Study
Using a diverse sample of families in Chicago, we first asked whether family support reduced primary caregivers’ risk of child maltreatment. Second, we asked whether the inverse association between family support and child maltreatment was mediated by reduced levels of primary caregiver depression. Finally, we asked whether family support exerted the same protective effect against primary caregiver depression, and by extension, child maltreatment, in all neighborhoods, regardless of level of violence.
Method
Data
Individual-level data for the present study were taken from the Project on Human Development in Chicago Neighborhoods (PHDCN), which is a multilevel, longitudinal study designed to examine child and adolescent development in context. Neighborhood-level data were taken from the 1990 U.S. Decennial Census and 1990 Chicago police records.
Individual-level sample
Child- and primary caregiver-level data were collected as part of the PHDCN Longitudinal Cohort Study, which began in 1994. Participants were recruited using a multi-stage sampling strategy. First, each of Chicago’s 847 census tracts was assigned to one of 343 neighborhood clusters (NCs) based on information from three sources: findings from cluster analyses of 1990 U.S. Census data, knowledge of Chicago neighborhoods, and major geographic boundaries (e.g., parks, freeways). The resulting NCs were then stratified by ethnic composition (7 categories) and SES (3 categories: high, medium, and low), yielding 21 strata. Roughly equal numbers of NCs were randomly selected from all but three empty strata (low SES primarily White NCs, high SES primarily Latino NCs, and high SES primarily Black and Latino NCs). This selection process yielded a final representative sample of 80 NCs.
Approximately 35,000 households within the 80 NCs were randomly selected and screened for eligibility (eligible households were those whose members included at least 1 child within 6 months of one of 7 target ages). This resulted in a sample of 6,234 children and adolescents in 7 age groups (ages 0, 3, 6, 9, 12, 15, and 18 years), or cohorts, for the first wave of data collection (75% acceptance rate). Wave 2 and 3 assessments were administered at approximately 2½ year intervals. Retention rates were relatively high; 86% of the original sample enrolled at wave 2 and 77% of the original sample enrolled at wave 3 (Martin & Schoua-Glusberg, 2002). There was a home visit at each wave, during which children and their primary caregivers completed measures of functioning in a variety of physical, social, psychological, behavioral, and academic domains. Primary caregivers provided informed consent and children provided informed assent before each wave. Procedures were reviewed by Institutional Review Boards at the Harvard School of Public Health and Harvard Medical School.
Individual-level data for the present analyses were taken from the first two waves of the PHDCN. Measures of primary caregivers’ family support and several control variables were constructed using wave 1 data, and measures of primary caregiver depression and child maltreatment were constructed using wave 2 data. We restricted the analytic sample to age cohorts 3, 6, 9, 12, and 15 (N = 4,960). Cohorts 0 and 18 were excluded because necessary data on maltreatment were not available. Analyses were conducted for only those cases with complete data on the independent variables (family support and all controls) and either primary caregiver depression or child maltreatment. The number of cases included in models predicting caregiver depression and maltreatment ranged from 2,762 to 3,139. Descriptive statistics on all study variables were computed for all cases that were included in at least one of the regression models described below (N = 3,156; see Table 1).
Table 1.
Descriptive statistics for all study variables
| Percentage | Mean (SD) | |
|---|---|---|
| Level 1 | ||
| Key variables | ||
| Family support | -- | 2.69 (0.38) |
| Child maltreatment (W2) | -- | 0.33 (0.72) |
| PC depression (W2) | 6.1% | -- |
| Control variables | ||
| Child maltreatment (W1) | -- | 0.88 (1.03) |
| PC depression (W1) | 10.2% | -- |
| PC race/ethnicity | ||
| Hispanic | 44.9% | -- |
| African American | 34.4% | -- |
| White | 16.7% | -- |
| Other | 4.0% | -- |
| PC marital status | ||
| Married | 56.4% | -- |
| Cohabiting | 11.7% | -- |
| Single | 31.9% | -- |
| Family size | -- | 5.29 (1.98) |
| Per capita income | -- | 6,249.70 (5,181.78) |
| Male child | 50.3% | -- |
| Female PC | 91.8% | -- |
| PC education > HS | 45.0% | -- |
| Age of PC | -- | 35.81 (8.33) |
| Age of child | -- | 8.56 (4.20) |
| Level 2 | ||
| Key variable | ||
| Neighborhood violence | -- | 2.75 (1.27) |
| Control variables | ||
| Concentrated poverty | -- | −0.10 (0.79) |
| Immigrant concentration | -- | 0.28 (1.04) |
| Residential stability | -- | −0.22 (1.04) |
Note. Descriptive statistics were computed using the analytic sample (N=3,156), which comprises cases with complete data for wave 1 predictors and controls and wave 2 primary caregiver depression or child maltreatment. W = wave; PC = primary caregiver.
To determine whether sample selection procedures introduced a source of bias, we compared our analytic sample of 3,156 cases to the full sample of cases in cohorts 3, 6, 9, 12, and 15 on all nine individual-level demographic characteristics listed in Table 1. Analyses revealed the following differences: (1) children in the analytic sample were, on average, younger (M = 8.56, SD = 4.20) than were children in the full sample (M = 9.83, SD = 5.06; t = −11.76, p < .001), (2) primary caregivers in the analytic sample were less likely to cohabit (11.7%) than were caregivers in the full sample (13.3%; χ2(1) = 6.62, p < .05), and (3) primary caregivers in the analytic sample reported a higher per capita household yearly income (M = $6,249.70, SD = $5,181.78) than did caregivers in the full sample (M = $5,955.06, SD = $5,150.83; t = 2.47, p < .05), and were more likely to have completed some education beyond high school (45.0%) than were caregivers in the full sample (43.0%; χ2(1) = 4.97, p < .05).
Neighborhood-level sample
One of the above-described 80 NCs was excluded because none of the families in our sample resided in it; 79 NCs were thus included in our analyses. The number of families per NC ranged from 1 to 102 (M = 65).
Measures
Family support
The Provision of Social Relations (PSR) scale (Turner, Frankel, & Levin, 1983) was administered to primary caregivers at wave 1. The PSR demonstrates acceptable reliability and validity (Turner et al., 1983) and includes 6 items (α = .76) that assess the extent to which caregivers feel supported by family (e.g., “I know my family will always stand by me”). Responses to these items (1 = not true to 3 = very true) were averaged.
Child maltreatment
At waves 1 and 2, primary caregivers completed the Conflict Tactics Scale (CTS; Straus, 1979). Characterized by robust psychometric properties (Straus, 1979), the CTS assesses parents’ strategies for resolving problems with their children. At each wave, caregivers were asked whether they or any other adult family or household member had used each of 6 forms of physical maltreatment (e.g., throwing something at the child) against their children within the past year. Affirmative responses to these items were summed to construct a count of types of maltreatment. The wave 2 maltreatment measure served as our dependent variable and the wave 1 measure was used as a control.
Primary caregiver depression
At wave 2, primary caregivers completed the Composite International Diagnostic Interview Short Form (CIDI-SF; Kessler & Mrozek, 1997) depression module, which is a fully structured diagnostic interview. Two sets of screener questions first identified caregivers at risk for a diagnosis of past-year depression. Caregivers were considered at risk if they had experienced at least one two-week period within the past 12 months during which they either “felt sad, blue, or depressed” or “lost interest in most things like hobbies, work, or [pleasurable] activities,” for most of the day, almost every day. At-risk caregivers then responded to follow-up questions about other symptoms of depression (e.g., whether they experienced problems sleeping, weight gain or loss) and indicated how much these symptoms interfered with their lives (1 = not at all to 4 = a lot). Using DSM-IV criteria for a Major Depressive Episode as a guide, caregivers were diagnosed as depressed only if they (1) endorsed a screener item, (2) endorsed at least 4 other symptoms, and (3) indicated that their symptoms interfered with their lives “a lot.” Just over 6% of the caregivers in our sample met criteria for a depressive episode. This figure is slightly lower than those from nationally representative samples which estimate that 7–8% of U.S. women meet criteria for a past-year Major Depressive Episode (Hasin, Goodwin, Stinson, & Grant, 2005; Vesga-López et al., 2008).
Although the CIDI-SF was not administered prior to wave 2, primary caregivers at wave 1 responded to a single question about whether they had ever “felt so low for a period of at least two weeks that they hardly ate or slept, or couldn’t work or do whatever they usually [did].” This item was used as a control for depression at wave 1.
Individual-level demographic control variables
All analyses controlled for child sex, primary caregiver sex, primary caregiver race/ethnicity (white, African American, Hispanic, other race/ethnicity), child age at wave 1, primary caregiver age at wave 1, household per capita income, primary caregiver education (1 = some education beyond high school), family size, and primary caregiver marital status (single, married, cohabiting).
Neighborhood violence
Homicide rates were used as an indicator of neighborhood violence shortly before wave 1. Data on the number of homicides in each NC were taken from 1990 Chicago Police Department records, and data on the size of the population in each NC were taken from the 1990 U.S. Decennial Census. A logged indicator of the homicide rate in each NC was computed using the following formula: ln{[(homicides/population count) × 100,000] + 1}.
Neighborhood-level demographic control variables
To isolate the effect of neighborhood violence per se, we controlled for several demographic characteristics of neighborhoods. Previously published factor analyses of 1990 U.S. Decennial Census data (Sampson, Raudenbush & Earls, 1997) identified three dimensions of neighborhood socioeconomic structure: (1) a concentrated disadvantage dimension defined by the percentage of residents living below the poverty level, the percentage of residents on public assistance, the percentage of female-headed households, the percentage of unemployed residents, the percentage of residents under age 18, and the percentage of African American residents; (2) an immigrant concentration dimension defined by the percentage of foreign-born residents and the percentage of Latino residents; and, (3) a residential stability dimension defined by the percentage of residents in owner-occupied houses and the percentage of residents living in the same home over a five-year period. In all analyses, we used factor scores on these three dimensions as controls for neighborhood-level socioeconomic status.
Analytic Strategy
General approach
We used two-level Poisson and logistic regression models in HLM 6.08 (Raudenbush, Bryk, & Congdon, 2009) to examine the associations between family support, depression, and child maltreatment. Our dependent and mediating variables – child maltreatment and primary caregiver depression, respectively – were modeled as a function of family support and individual-level controls at level 1 and neighborhood violence and neighborhood-level controls at level 2. Continuous predictors and controls at both levels were centered around their grand means. Because preliminary analyses revealed overdispersion in maltreatment and underdispersion in depression, we estimated a dispersion parameter for outcomes in all models rather than using the default dispersion estimates that are assumed by HLM 6.08 for Poisson and logistic models.1
Model-building
To address our first question, we examined the direct associations between family support and child maltreatment net of the contributions of all other individual-and neighborhood-level variables. At level 1 (eq. 1), the log of the expected count of types of child maltreatment, λ, (henceforth referred to as the “log of maltreatment”) for each child i in
| (1) |
neighborhood j was modeled as a function of a level-1 intercept (β0j), the effect (β1j) of family support, the effects (βqj) of q = 13 individual-level control variables (X), and a level-1 error term (r). At level 2 (see equation 2), the level-1 intercept (β0j) from equation 1 was modeled as a function of a level-2 intercept (γ00), the effects (γ01− γ04) of 4 neighborhood characteristics
| (2) |
(neighborhood violence, concentrated disadvantage, immigrant concentration, and residential stability), and a level-2 error term (μ0j). Additionally, the level-1 slopes for family support (β1j) and all individual-level controls (βqj) were modeled as a function of level-2 intercepts (γ10 and γq0, respectively; see equations 3 and 4). Thus, the main effect of family support on maltreatment, averaged across j neighborhoods, is ultimately represented by the level-2 intercept, γ10.
| (3) |
| (4) |
To answer our second research question, we assessed the extent to which caregiver depression mediated the link between wave 1 family support and wave 2 maltreatment. We followed Baron’s and Kenny’s (1986) guidelines for establishing mediation, which require: 1) a significant coefficient, a, for the path between the independent variable and the mediator; 2) a significant coefficient, b, for the path between the mediator and the dependent variable while controlling for the independent variable; and 3) a significant coefficient for the indirect path between the independent and dependent variable through the mediator (i.e., the product of a × b). Thus, we first tested the link between wave 1 family support and wave 2 caregiver depression (our a path) using a two-level logistic model that was nearly identical to the model represented by equations 1 through 4; it differed only in that the distribution of the dependent variable (primary caregiver depression) was logistic (rather than Poisson) and it included a control for wave 1 depression (instead of a control for wave 1 maltreatment). We then examined associations between caregiver depression at wave 2 and maltreatment at wave 2 (our b path). To test these associations, we entered wave 2 primary caregiver depression as a level-1 predictor in the above-described Poisson model of wave 2 child maltreatment (see equations 1 through 4). Because these analyses revealed significant a and b paths, we used the Sobel method to test the statistical significance of the indirect path between family support and child maltreatment via primary caregiver depression (Sobel, 1982).
Finally, to answer our third question, we examined the extent to which neighborhood violence moderated the association between wave 1 social support and wave 2 primary caregiver depression (and by extension, the indirect association between wave 1 family support and wave 2 child maltreatment). Building on the two-level models of wave 2 maltreatment and primary caregiver depression described above, we added neighborhood violence and a neighborhood-level error term to the level-2 model predicting the level-1 slope for family support (β1j; see resulting equation 5). In this model, the slope γ11 represents the cross-level interactions between neighborhood violence and family support.2
| (5) |
Because analyses revealed significant interactions between family support and neighborhood violence, we used “regions of significance” testing to precisely identify the regions on the neighborhood violence scale within which the effects of family support on depression were statistically significant (see Preacher, Curran, & Bauer, 2006 for a description of the web utility used to perform these tests).
Results
Direct Association between Family Support and Child Maltreatment
Two-level Poisson models revealed a significant direct inverse association between family support at wave 1 and child maltreatment at wave 2 (γ [SE] = −0.31 [0.08], t = −3.76, p < .001), net of controls for wave 1 child maltreatment, individual-level demographic characteristics, and neighborhood-level characteristics (see Table 2, Model 1).
Table 2.
Regression models of primary caregiver depression and child maltreatment
| Model 1: Child maltreatment | Model 2: PC depression | Model 3: Child maltreatment | Model 4: PC depression | |
|---|---|---|---|---|
|
| ||||
| γ (SE) | γ (SE) | γ (SE) | γ (SE) | |
| Intercept | −1.36 (0.18)*** | −3.38 (0.47)*** | −1.35 (0.20)*** | −3.53 (0.47)*** |
| Level 1 predictors | ||||
| Family support | −0.31 (0.08)*** | −0.72 (0.17)*** | −0.26 (0.09)** | −0.60 (0.23)* |
| Child maltreatment (W1) | 0.47 (0.03)*** | -- | 0.47 (0.03)*** | -- |
| PC depression (W2) | -- | -- | 0.31 (0.13)* | -- |
| PC depression (W1) | -- | 1.52 (0.18)*** | -- | 1.56 (0.18)*** |
| PC race/ethnicity | ||||
| Hispanic | −0.12 (0.13) | 0.15 (0.28) | −0.10 (0.13) | 0.26 (0.28) |
| African American | 0.19 (0.14) | 0.20 (0.32) | 0.21 (0.15) | 0.24 (0.32) |
| Other | −0.02 (0.21) | −0.07 (0.51) | −0.52 (0.29) | −0.01 (0.50) |
| PC marital status | ||||
| Married | −0.08 (0.09) | −0.17 (0.20) | −0.05 (0.10) | −0.16 (0.19) |
| Cohabiting | 0.09 (0.12) | 0.34 (0.23) | 0.13 (0.12) | 0.40 (0.22) |
| Family size | −0.02 (0.02) | 0.14 (0.04)** | −0.03 (0.02) | 0.14 (0.04)** |
| Per capita income | 0.00 (0.00)* | 0.00 (0.00) | 0.00 (0.00)* | 0.00 (0.00) |
| Male child | 0.24 (0.07) | −0.10 (0.15) | 0.18 (0.08)* | −0.12 (0.15) |
| Female PC | −0.13 (0.13) | 0.32 (0.36) | −0.17 (0.14) | 0.30 (0.35) |
| PC education > HS | 0.12 (0.08) | −0.06 (0.18) | 0.15 (0.09) | −0.05 (0.18) |
| Age of PC | −0.01 (0.01) | 0.02 (0.01) | −0.00 (0.01) | 0.02 (0.01) |
| Age of child | 0.02 (0.01)* | 0.02 (0.02) | 0.02 (0.01)* | 0.02 (0.02) |
| Level 2 predictors | ||||
| Neighborhood violence | −0.09 (0.05) | −0.09 (0.16) | −0.10 (0.06) | −0.10 (0.16) |
| Concentrated poverty | 0.13 (0.08) | −0.12 (0.26) | 0.15 (0.09) | −0.17 (0.26) |
| Immigrant concentration | −0.04 (0.05) | 0.19 (0.12) | −0.04 (0.05) | 0.24 (0.12) |
| Residential stability | 0.05 (0.04) | −0.43 (0.13)** | 0.04 (0.05) | −0.45 (0.13)** |
| Cross-level interaction | ||||
| PC depression X neighborhood violence | -- | -- | -- | −0.47 (0.19)* |
| N | 3,139 | 2,762 | 2,816 | 2,762 |
Note. Table presents results of two-level Poisson (Models 1 and 3) and logistic (Models 2 and 4) regression models that account for over-/ under-dispersion. W = wave; PC = primary caregiver; -- = not included in model.
p < .05,
p < .01,
p < .001.
Mediated Association between Family Support and Child Maltreatment via Depression
After finding that wave 1 family support was inversely associated with child maltreatment at wave 2, we then sought to determine whether primary caregiver depression at wave 2 mediated this association. We found, first, that wave 1 family support was inversely associated with primary caregiver depression at wave 2 (γ [SE] = −0.72 [0.17], t = −4.32, p < .001), even after controlling for primary caregiver depression at wave 1, individual-level demographic characteristics, and neighborhood-level characteristics (see Table 2, Model 2). Primary caregiver depression at wave 2 was, in turn, positively associated with child maltreatment at wave 2 (γ [SE]= 0.31 [0.13], t = 2.42, p < .05), net of all controls (see Table 2, Model 3). Moreover, a Sobel test revealed that the indirect path from family support to child maltreatment via primary caregiver depression was statistically significant (γ [SE]= −0.22 [0.11], z = −2.11, p < .05). Primary caregiver depression explained 16% of the association between family support and child maltreatment.
Moderated Association between Family Support and Maltreatment via Depression
Finally, we sought to determine whether neighborhood violence moderated the association between social support and primary caregiver depression (and, by extension, the association between social support and child maltreatment). To be thorough, we also tested whether neighborhood violence moderated the direct pathway from family support to child maltreatment and found that it did not (results not shown). As noted by Muller, Judd, and Yzerbyt (2005), however, moderation of an indirect path can exist even in the absence of moderation of the direct path; that is, the intervening mechanism that explains an association between an independent and dependent variable can vary across groups within a population, even when the strength and significance of the direct link between the independent and dependent variables does not vary across groups. Thus, we proceeded to test for, and subsequently identified, a significant interaction between neighborhood violence and family support in the model predicting our mediating variable, primary caregiver depression (Table 2, Model 4; γ [SE] = −0.47 [0.19], t = −2.47, p < .05).
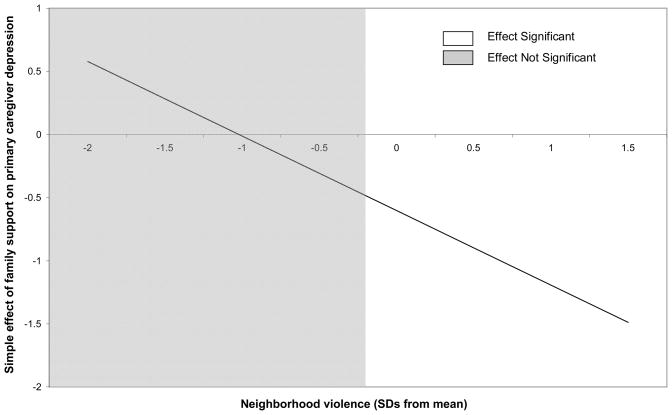
Regions of significance testing revealed that the protective influence of family support on primary caregiver depression was only significant in neighborhoods with scores on violence above 2.49 (which is 0.21 SDs below the mean on violence; see Figure 1). In other words, family support protected against primary caregiver depression in neighborhoods with average to high, but not low, scores on violence. Additionally, as shown in Figure 1, we found that the protective influence of family support against primary caregiver depression grew stronger as scores on neighborhood violence increased. Because the a path in our mediation model (i.e., the path between family support and primary caregiver depression) was only significant in neighborhoods with scores on violence above 2.49, the indirect path between family support and child maltreatment via primary caregiver depression could only be significant in neighborhoods with scores on violence that were greater than 2.49. However, there remained a significant direct path between family support and child maltreatment in all neighborhoods, regardless of their score on violence.
Figure 1.
Graph represents the interaction between wave 1 family support and neighborhood violence in a model predicting primary caregiver depression at wave 2. Unshaded area shows the values of neighborhood violence at which the effect of family support is significant.
Discussion
In the present study, we found that family support was inversely associated with child maltreatment, and that this association was partially mediated by lower primary caregiver depression. This result is consistent with past studies showing both direct effects of social support on parenting behaviors and indirect effects via depression (Lee et al., 2009; Simons et al., 1993), but it is the first study to demonstrate that primary caregiver depression mediates associations between social support and maltreatment of children per se. However, it is noteworthy that the mediation of the path from family support to child maltreatment by primary caregiver depression did not occur in all neighborhoods. In neighborhoods with average or high levels of violence only, primary caregivers who received more social support from family were less likely to be depressed; as a result, they were less likely to maltreat their child. In neighborhoods with low levels of violence, however, primary caregiver depression did not mediate associations between social support and maltreatment. The present study is the first to document this pattern of moderated mediation.
It should be noted that these results do not indicate the absence of an association between family support and child maltreatment in neighborhoods with below-average violence. Rather, in less violent neighborhoods there was a direct path from greater family support to lower child maltreatment. This path was also found in more violent neighborhoods, but it was supplemented with an indirect path via reduced primary caregiver depression. Further, it should not be concluded that family support plays a larger role in reducing child maltreatment in more violent neighborhoods, where it had both direct and indirect effects, than in less violent neighborhoods, where it had direct effects alone. The test for an interaction between family support and neighborhood violence in the model predicting child maltreatment was not significant (not shown), indicating that the strength of the association between family support and child maltreatment did not vary by neighborhood violence. The results suggest, instead, that the mechanisms by which family support reduces child maltreatment vary by level of neighborhood violence.
Differences in the role of family support across more and less violent neighborhoods may reflect differences in the types of social support that are most relevant to parents who live in those neighborhoods. The literature on social support often distinguishes between emotional support (e.g., comfort, companionship) and instrumental support (e.g., material or practical assistance). Perhaps the direct effects of family support on maltreatment reflect the provision of instrumental supports – for example, help with child care or monetary assistance – that can avert some of the triggers for maltreatment without reducing parental depression. Such supports may be relevant and helpful regardless of the type of neighborhood in which parents reside. However, family support which indirectly protects against child maltreatment by reducing depression may reflect emotional support that is more salient for parents residing in violent neighborhoods. It has been noted that buffering is possible only when the type of social support provided is relevant to the needs of the recipient (Cohen & Wills, 1985). Thus, if neighborhood violence is conceptualized as a source of stress (as has been demonstrated empirically; Curry et al., 2008; Tonorezos et al., 2008), emotional support provided by family may exert a buffering effect on child maltreatment by reducing parents’ stress-related depression.
Unfortunately, the measure of family support used in the present study did not specify the type of support primary caregivers received. The items that measured high levels of family support (e.g., “I know my family will always stand by me”) may have been interpreted by respondents as indicating either or both types of support. Thus, additional studies will be needed to explicitly test whether the main and buffering effects of family support on child maltreatment differentially reflect instrumental versus emotional support. Another question that deserves further study is whether parents living in less versus more violent neighborhoods differ with respect to the type of support they tend to receive from their families. For example, parents living in more violent neighborhoods may have family members with fewer material resources of their own, and are thus less equipped to offer instrumental support than emotional support.
There are three facets of the present study that may limit its interpretability. First, depression (our mediator variable) and child maltreatment (our dependent variable) were measured at the same wave. It might be argued that in an ideal test of mediation, the mediator temporally precedes the dependent variable. However, limitations on available measures prevented us from capitalizing on the third wave of data collected for this study. Further, because the ecological model of parenting posits that parents’ mental health and social support have immediate impacts on parenting behaviors (Belsky, 1984), it may be appropriate that depression and child maltreatment were measured simultaneously. Second, our measure of child maltreatment was self-reported rather than drawn from child protective service records. However, it is unclear which type of measure is more accurate. Although parents may underreport maltreating behaviors due to social desirability, self-reports are thought to be more accurate than administrative records, which are flawed by underreporting and the inability of child protective service agencies to substantiate claims (Hussey, Chang, & Kotch, 2006). Last, the generalizability of our findings to non-urban parents is unknown. Even the generalizability to parents in Chicago may be limited, given that our analytic sample excluded the parents of infants, and was slightly more socioeconomically advantaged than the full sample of cohorts 3–15 in PHDCN.
In sum, we find that family support directly lowers the risk of child maltreatment in all neighborhoods, and also indirectly lowers it by decreasing primary caregiver depression in more violent neighborhoods. It thus appears that efforts to prevent child maltreatment may profitably focus on two types of interventions: programs to help parents forge closer bonds with family members, and programs to alleviate parents’ depressive symptoms.
Acknowledgments
This research was supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development Grant R01HD060719. We gratefully acknowledge the assistance of Erin Bumgarner and Todd Hoffman.
Footnotes
Consistent with the defaults in HLM 6.08, we estimated all models using the restricted maximum likelihood method with a “penalized quasi-likelihood” (PQL) approximation. Some have argued that for logistic and poisson models, the Laplace approximation yields more accurate estimates than does the PQL approximation (e.g., Raudenbush & Bryk, 2002). However, HLM 6.08 does not allow for the estimation of dispersion parameters when the Laplace approximation option is selected. Because our analyses revealed evidence of both overdispersion and underdispersion, we chose to use the PQL approximation, thereby retaining the ability to estimate dispersion parameters. To ensure, however, that our results were not badly biased, we reran all of the models described in this paper using the Laplace approximation. The results did not change substantially; all patterns of significance and non-significance described in our results were replicated in analyses that used the Laplace approximation.
Moderation of the path between caregiver depression and maltreatment was not of primary interest. However, in supplementary analyses, we tested for interactions between neighborhood violence and caregiver depression in models predicting maltreatment. These analyses did not reveal significant interactions (results not shown).
References
- Ajrouch K, Reisine S, Lim S, Sohn W, Ismail A. Situational stressors among African American women living in low-income urban areas: The role of social support. Women & Health. 2010;50:159–175. doi: 10.1080/03630241003705045. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Belsky J. The determinants of parenting: A process model. Child Development. 1984;55:83–96. doi: 10.1111/j.1467-8624.1984.tb00275.x. [DOI] [PubMed] [Google Scholar]
- Bishop SJ, Leadbeater BJ. Maternal social support patterns and child maltreatment: Comparison of maltreating and nonmaltreating mothers. American Journal of Orthopsychiatry. 1999;69:172–181. doi: 10.1037/h0080419. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Brugha TS, Sharp HM, Cooper SA, Weisender C, Britto D, Shinkwin R, …Kirwan PH. The Leicester 500 Project. Social support systems and the development of postnatal depressive symptoms, a prospective cohort survey. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 1998;28:63–79. doi: 10.1017/s0033291797005655. [DOI] [PubMed] [Google Scholar]
- Ceballo R, McLoyd VC. Social support and parenting in poor, dangerous neighborhoods. Child Development. 2002;73:1310–1321. doi: 10.1111/1467-8624.00473. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Kelleher K, Hollenberg J. Onset of physical abuse and neglect: Psychiatric, substance abuse and social risk factors from prospective community data. Child Abuse & Neglect. 1996;20:191–203. doi: 10.1016/s0145-2134(95)00144-1. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Conger RD, Ge N, Elder GH, Lorenz FO, Simons RL. Economic stress, coercive family process, and developmental problems of adolescents. Child Development. 1994;65:541–561. [PubMed] [Google Scholar]
- Coyne JC, DeLongis A. Going beyond social support: The role of social relationships in adaptation. Journal of Consulting and Clinical Psychology. 1986;54:454–460. doi: 10.1037//0022-006x.54.4.454. [DOI] [PubMed] [Google Scholar]
- Curry A, Latkin C, Davey-Rothwell M. Pathways to depression: The impact of neighborhood violent crime on inner-city residents in Baltimore, Maryland, USA. Social Science & Medicine. 2008;67:23–30. doi: 10.1016/j.socscimed.2008.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW, Hessling RM, Brown PA, Murry V. Direct and moderating effects of community context on the psychological well-being of African American women. Journal of Personality and Social Psychology. 2000;79:1088–1101. doi: 10.1037//0022-3514.79.6.1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dix T, Meunier LN. Depressive symptoms and parenting competence: An analysis of 13 regulatory processes. Developmental Review. 2009;29:45–68. [Google Scholar]
- Fagg J, Curtisb S, Stansfeldc S, Cattellc V, Tupuolac A, Arephinc M. Area social fragmentation, social support for individuals and psychosocial health in young adults: Evidence from a national survey in England. Social Science & Medicine. 2008;66:242–254. doi: 10.1016/j.socscimed.2007.07.032. [DOI] [PubMed] [Google Scholar]
- Garbarino J. The human ecology of child maltreatment: A conceptual model for research. Journal of Marriage and Family. 1977;39:721–735. [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of Major Depressive Disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Archives of General Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hussey JM, Chang JJ, Kotch JB. Child maltreatment in the United States: Prevalence, risk factors, and adolescent health consequences. Pediatrics. 2006;118:933–942. doi: 10.1542/peds.2005-2452. [DOI] [PubMed] [Google Scholar]
- Jackson PB. Specifying the buffering hypothesis: Support, strain, and depression. Social Psychology Quarterly. 1992;55:363–378. [Google Scholar]
- Kalil A, Born CE, Kunz J, Caudill PJ. Life stressors, social support, and depressive symptoms among first-time welfare recipients. American Journal of Community Psychology. 2001;29:355–369. doi: 10.1023/A:1010351302196. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mrozek C. UM-CIDI Short Form. Ann Arbor, MI: University of Michigan, Institute for Social Research; 1997. [Google Scholar]
- Kotch JB, Browne DC, Ringwalt CL, Dufort V, Rubina E. Stress, social support, and substantiated maltreatment in the second and third years of life. Child Abuse & Neglect. 1997;21:1025–1037. doi: 10.1016/s0145-2134(97)00063-x. [DOI] [PubMed] [Google Scholar]
- Kotchick BA, Dorsey S, Heller L. Predictors of parenting among African American single mothers: Personal and contextual factors. Journal of Marriage and Family. 2005;67:448–460. [Google Scholar]
- Latkin C, Curry A. Stressful neighborhoods and depression: A prospective study of the impact of neighborhood disorder. Journal of Health and Social Behavior. 2003;44:34–44. [PubMed] [Google Scholar]
- Lee CS, Anderson JR, Horowitz JL, August GJ. Family income and parenting: The role of parental depression and social support. Family Relations. 2009;58:417–430. [Google Scholar]
- Leventhal T, Brooks-Gunn J. Moving on up: Neighborhood effects on children and families. In: Bornstein M, Bradley RH, editors. Socioeconomic status, parenting, and child development. Mahwah, NJ: Erlbaum; 2003. pp. 209–230. [Google Scholar]
- Li F, Godinet MT, Arnsberger P. Protective factors among families with children at risk of maltreatment: Follow up to early school years. Children and Youth Services Review. 2011;33:139–148. [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Lyons SJ, Henly JR, Schuerman JR. Informal support in maltreating families: Its effect on parenting practices. Children and Youth Services Review. 2005;27:21–38. [Google Scholar]
- Margolin G, Gordis EB. The effects of family and community violence on children. Annual Review of Psychology. 2000;51:445–479. doi: 10.1146/annurev.psych.51.1.445. [DOI] [PubMed] [Google Scholar]
- Martin KR, Schoua-Glusberg A. Project on Human Development in Chicago Neighborhoods Longitudinal Cohort Study: Field data collection report. Cambridge, MA: Harvard University; 2002. Jun, [Google Scholar]
- Mason CA, Cauce AM, Gonzales N, Hiraga Y, Grove K. An ecological model of externalizing behaviors in African-American adolescents: No family is an island. Journal of Research on Adolescence. 1994;4:639–655. [Google Scholar]
- McLoyd VC. Socioeconomic disadvantage and child development. American Psychologist. 1998;53:185–204. doi: 10.1037//0003-066x.53.2.185. [DOI] [PubMed] [Google Scholar]
- Molnar BE, Buka SL, Brennan RT, Holton JK, Earls F. A multilevel study of neighborhoods and parent-to-child physical aggression: Results from the Project on Human Development in Chicago Neighborhoods. Child Maltreatment. 2003;8:84–97. doi: 10.1177/1077559502250822. [DOI] [PubMed] [Google Scholar]
- Mulia L, Schmidt J, Bond L, Jacobs R, Korcha R. Stress, social support and problem drinking among women in poverty. Addiction. 2008;103:1283–1293. doi: 10.1111/j.1360-0443.2008.02234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller RT, Fitzgerald HE, Sullivan LA, Zucker RA. Social support and stress factors in child maltreatment in alcoholic families. Canadian Journal of Behavioral Science. 1994;26:438–461. [Google Scholar]
- Muller D, Judd CM, Yzerbyt VY. When moderation is mediated and mediation is moderated. Journal of Personality and Social Psychology. 2005;89:852–863. doi: 10.1037/0022-3514.89.6.852. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Rajaratnam J, O’Campo P, O’Brien M, Muntaner C, Muntaner C. The effect of social isolation on depressive symptoms varies by neighborhood characteristics: A study of an urban sample of women with pre-school aged children. International Journal of Mental Health and Addiction. 2008;6:464–475. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2. Newbury Park, CA: Sage; 2002. [Google Scholar]
- Raudenbush A, Bryk A, Congdon R. HLM (Version 6.08) [Computer software] Lincolnwood, IL: Scientific Software International; 2009. [Google Scholar]
- Richey CA, Lovell ML, Reid K. Interpersonal skill training to enhance social support among women at risk for child maltreatment. Children and Youth Services Review. 1991;13:41–59. [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Sidebotham P, Heron J. Child maltreatment in the “Children of the Nineties”: A longitudinal study of parental risk factors. Child Abuse & Neglect. 2006;30:497–522. doi: 10.1016/j.chiabu.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Simons RL, Lorenz FO, Wu C, Conger RD. Social network and marital support as mediators and moderators of the impact of stress and depression on parental behavior. Developmental Psychology. 1993;29:368–381. [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Social Methodology. 1982;13:290–312. [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactics Scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- Taylor RD, Seaton E, Dominguez A. Kinship support, family relations, and psychological adjustment among low-income African American mothers and adolescents. Journal of Research on Adolescence. 2008;18:1–22. [Google Scholar]
- Tonorezos ES, Breysse PN, Matsui EC, McCormack MC, Curtin-Brosnan J, Williams D, …Diette GB. Does neighborhood violence lead to depression among caregivers of children with asthma? Social Science & Medicine. 2008;67:31–37. doi: 10.1016/j.socscimed.2008.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RJ, Frankel B, Levin D. Social support: Conceptualization, measurement, and implications for mental health. In: Greenley JR, editor. Research in Community and Mental Health. III. Greenwich: JAI Press; 1983. pp. 67–111. [Google Scholar]
- U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau. Child Maltreatment 2008. 2010 Available from http://www.acf.hhs.gov/programs/cb/stats_research/index.htm#can.
- Vesga-López O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Archives of General Psychiatry. 2008;65:805–815. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegman HL, Stetler C. A meta-analytic review of the effects of child abuse on medical outcomes in adulthood. Psychosomatic Medicine. 2009;71:805–812. doi: 10.1097/PSY.0b013e3181bb2b46. [DOI] [PubMed] [Google Scholar]
- Windham AM, Rosenberg L, Fuddy L, McFarlane E, Sia C, Duggan AK. Risk of mother-reported child abuse in the first 3 years of life. Child Abuse & Neglect. 2004;28:645–667. doi: 10.1016/j.chiabu.2004.01.003. [DOI] [PubMed] [Google Scholar]