Abstract
BACKGROUND:
Esophageal adenocarcinoma has one of the fastest rising incidence rates and one of the lowest survival rates of any cancer type in the Western world. However, in many countries, trends in esophageal cancer differ according to tumour morphology and anatomical location. In Canada, incidence and survival trends for esophageal cancer subtypes are poorly known.
METHODS:
Cancer incidence and mortality rates were obtained from the Canadian Cancer Registry, the National Cancer Incidence Reporting System and the Canadian Vital Statistics Death databases for the period from 1986 to 2006. Observed trends (annual per cent change) and five-year relative survival ratios were estimated separately for esophageal adenocarcinoma and squamous cell carcinoma, and according to location (upper, middle, or lower one-third of the esophagus). Incidence rates were projected up to the year 2026.
RESULTS:
Annual age-standardized incidence rates for esophageal cancer in 2004 to 2006 were 6.1 and 1.7 per 100,000 for males and females, respectively. Esophageal adenocarcinoma incidence rose by 3.9% (males) and 3.6% (females) per year for the period 1986 to 2006, with the steepest increase in the lower one-third of the esophagus (4.8% and 5.0% per year among males and females, respectively). In contrast, squamous cell carcinoma incidence declined by 3.3% (males) and 3.2% (females) per year since the early 1990s. The five-year relative survival ratio for esophageal cancer was 13% between 2004 and 2006, approximately a 3% increase since the period from 1992 to 1994. Projected incidence rates showed increases of 40% to 50% for esophageal adenocarcinoma and decreases of 30% for squamous cell carcinoma by 2026.
DISCUSSION:
Although esophageal cancer is rare in Canada, the incidence of esophageal adenocarcinoma has doubled in the past 20 years, which may reflect the increasing prevalence of obesity and gastroesophageal reflux disease. Declines in squamous cell carcinoma may be the result of the decreases in the prevalence of smoking in Canada. Given the low survival rates and the potential for further increases in incidence, esophageal adenocarcinoma warrants close attention.
Keywords: Adenocarcinoma, Esophageal cancer, Incidence, Mortality, Squamous cell carcinoma, Survival
Abstract
HISTORIQUE :
L’adénocarcinome de l’œsophage affiche l’un des taux d’incidence les plus rapides et l’un des taux de survie les plus faibles de tous les cancers de l’hémisphère occidental. Toutefois, dans de nombreux pays, les tendances de cancer de l’œsophage diffèrent selon la morphologie de la tumeur et le foyer anatomique. Au Canada, on ne sait pas grand-chose de l’incidence et des tendances de survie d’après les sous-types de cancer de l’œsophage.
MÉTHODOLOGIE :
Les chercheurs ont extrait l’incidence de cancer et les taux de mortalité du Registre canadien du cancer, du Système national de déclaration des cas de cancer et des bases de données sur les décès de la statistique de l’état civil entre 1986 et 2006. Ils ont évalué séparément les tendances observées (changement annuel en pourcentage) et les ratios de survie relatifs sur cinq ans à l’égard de l’adénocarcinome de l’œsophage et du carcinome spinocellulaire, et compte tenu de leur foyer (tiers supérieur, central ou inférieur de l’œsophage). Ils ont projeté le taux d’incidence jusqu’en 2026.
RÉSULTATS :
Entre 2004 et 2006, le taux d’incidence annuel normalisé de cancer de l’œsophage selon l’âge était de 6,1 hommes et 1,7 femmes sur 100 000 habitants, respectivement. L’incidence d’adénocarcinome de l’œsophage a augmenté de 3,9 % (hommes) et de 3,6 % (femmes) par année entre 1986 et 2006, l’augmentation la plus marquée s’observant dans le tiers inférieur de l’œsophage (4,8 % et 5,0 % par année chez les hommes et les femmes, respectivement). Par contre, l’incidence de carcinome spinocellulaire a diminué de 3,3 % (hommes) et de 3,2 % (femmes) par année depuis le début des années 1990. Le ratio de survie relatif du cancer de l’œsophage correspondait à 13 % entre 2004 et 2006, soit une augmentation d’environ 3 % depuis la période de 1992 à 1994. Le taux d’incidence projeté révèle des augmentations de 40 % à 50 % des adénocarcinomes de l’œsophage et une diminution de 30 % des carcinomes spinocellulaires d’ici 2026.
EXPOSÉ :
Même si le cancer de l’œsophage est rare au Canada, l’incidence d’adénocarcinome de l’œsophage a doublé depuis 20 ans, ce qui peut refléter la prévalence croissante d’obésité et de reflux gastroœsophagien pathologique. La diminution des carcinomes spinocellulaires pourrait découler de la baisse de prévalence du tabagisme au Canada. Étant donné le faible taux de survie et la possibilité d’augmentation continue de l’incidence, il serait justifié d’évaluer attentivement l’adénocarcinome de l’œsophage.
Esophageal cancer is the eighth most commonly diagnosed cancer type and sixth leading cause of cancer deaths worldwide (1). Average rates of incidence in eastern Asia and southern Africa (15 per 100,000 among men, seven per 100,000 among women) are approximately triple those in the Americas, Europe and Oceania (six per 100,000 among men, two per 100,000 among women) (2,3). In less developed parts of the world, esophageal squamous cell carcinoma (ESCC) has long been the predominant subtype of this cancer, with rates up to 100 per 100,000 in parts of China, India and central Asia (the so-called, ‘esophageal cancer belt’ [4]). However, esophageal adenocarcinoma (EAC) incidence is increasing rapidly in Western countries (5–13), while ESCC incidence is generally stable (6,11) or declining (5,14).
In Canada, esophageal cancer is a relatively rare but deadly disease. Although it is only the 19th most common cancer type, it is the 10th leading cause of cancer deaths nationally. During 2012, there will be an estimated 1400 new cases among men and 450 new cases among women in Canada (15). Previous studies reported rising rates of EAC in two provinces: British Columbia (16) and Ontario (17,18). However, a national picture of esophageal cancer incidence and survival, according to tumour morphology and anatomical location, is still lacking for Canada.
METHODS
Cancer incidence and mortality data were obtained from the Canadian Cancer Registry, the National Cancer Incidence Reporting System, and the Canadian Vital Statistics Death (CVS:D) databases for the period 1986 to 2006. Statistics Canada maintains these databases and updates them annually with data received from the provincial and territorial cancer and vital statistics registries (19–21). The topography and morphology of cases followed the International Classification of Diseases for Oncology, Third Edition (22). Anatomical categories were as follows: esophagus, upper one-third (C15.3), middle one-third (C15.4), lower one-third (C15.5), and overlapping, unspecified or other locations (C15.0-C15.2, C15.8 and C15.9). Morphological categories were squamous cell carcinoma (types 8050 to 8078, 8083 to 8084) and adenocarcinoma (types 8140 to 8141, 8143 to 8145, 8190 to 8231, 8260 to 8263, 8310, 8401, 8480 to 8490, 8550 to 8551, 8570 to 8574 and 8576).
Age-standardized incidence rates (ASIRs) were calculated according to age, sex, and anatomical and morphological categories. All rates were standardized to the 1991 Canadian population. Annual percentage change was estimated as the (back transformed) slope from a linear regression of log-transformed annual ASIRs on the calendar year (23). All reported annual percentage change values were statistically significant at P<0.05. Observed trends in EAC and ESCC from 1987 to 2006 were projected to the year 2026 using the Nordpred software package (24). Nordpred is a standard cancer projection method that predicts future rates from a regression model with age, calendar period and birth cohort effects. The model was fit to the observed incidence counts for EAC and ESCC (aggregated into five-year periods and five-year age groups). Future values were estimated for four five-year periods (20 years ahead in total) by projecting forward the model’s linear time trend, with successive reductions in each period while fixing the period and cohort effects. Nordpred default settings were used for all projections. A detailed description of the projection model and methods can be found in Møller et al (25).
Period relative survival analyses (26,27) were calculated based on a publicly available algorithm (28) to which minor adaptations were made. Expected survival proportions were derived from sex-specific, complete provincial life tables using the Ederer II approach (29). Mortality follow-up through December 31, 2006 was determined by record linkage of the Canadian Cancer Registry to the CVS:D (excluding deaths registered in the province of Quebec) and from information reported by provincial/territorial cancer registries. Data from Quebec were excluded from the analysis primarily because of issues in correctly ascertaining the vital status of cases. Records were also excluded if: age at diagnosis was younger than 15 or older than 99 years; diagnosis was established through autopsy only or death certificate only; or the year of birth or death was unknown. Otherwise, all primary cancers were considered (30). Additional detail regarding the survival methodology is provided elsewhere (31).
RESULTS
Incidence trends in Canada
Incidence rates for EAC and ESCC in Canada showed opposing trends. Across all subtypes of esophageal cancer, annual rates have changed little since the mid 1980s, increasing slightly in men (0.3% per year) and decreasing slightly in women (0.5% per year). The average incidence rate was approximately three times higher among men (6.1 per 100,000) than among women (1.7 per 100,000) (Table 1). However, from 1986 to 2006, the rate of EAC doubled in men (1.8 to 3.5 per 100,000) and women (0.2 to 0.5 per 100,000), amounting to average annual increases of 3.9% and 3.6% per year, respectively (Figure 1). EAC has become increasingly common across age groups, with the fastest rising rates seen in individuals 15 to 44 years of age (6.9% per year, both sexes). Projections of the observed trends suggests that rates of EAC will increase by an additional 40% in men (up to 4.8 per 100,000) and 50% in women (up to 0.8 per 100,000) by 2026.
TABLE 1.
New cases, age-standardized incidence rates and predicted five-year relative survival ratio (RSR) for esophageal cancer according to anatomical location, morphology, sex and age in Canada, 2004 to 2006
| New cases, n | Age-standardized rate, per 100,000 | Five-year RSR* % (95% CI) | |
|---|---|---|---|
| All esophageal cancers | 4388 | 3.73 | 13 (12–15) |
| Sex | |||
| Male | 3233 | 6.09 | 13 (11–14) |
| Female | 1155 | 1.72 | 15 (13–18) |
| Location | |||
| Upper esophagus | 267 | 0.23 | 12 (8–17) |
| Middle esophagus | 724 | 0.62 | 13 (10–16) |
| Lower esophagus | 2199 | 1.88 | 14 (12–15) |
| Not specified as upper, middle or lower† | 1198 | 0.20 | 13 (11–16) |
| Morphology | |||
| Squamous cell carcinoma | 1567 | 1.35 | 14 (12–16) |
| Adenocarcinoma | 2201 | 1.87 | 14 (12–15) |
| Lower esophageal adenocarcinoma | 1563 | 1.33 | 14 (12–16) |
| All other adenocarcinoma | 638 | 0.54 | 12 (9–16) |
| Other specified and unspecified types | 620 | 0.10 | 9 (6–12) |
| Age‡, years | |||
| 15–44 | 108 | 0.23 | 18 (12–26) |
| 45–54 | 471 | 3.12 | 16 (12–20) |
| 55–64 | 1031 | 9.94 | 16 (13–18) |
| 65–74 | 1235 | 18.17 | 14 (12–16) |
| 75–99 | 1543 | 25.83 | 10 (8–12) |
Excludes cases diagnosed in the province of Quebec;
Includes cancers classified as cervical (76 cases), thoracic (59 cases), abdominal (16 cases), overlapping across subsites (145 cases) or unspecified with respect to location (902 cases);
No new cases observed among individuals <15 years of age. Data adapted from reference 49
Figure 1).
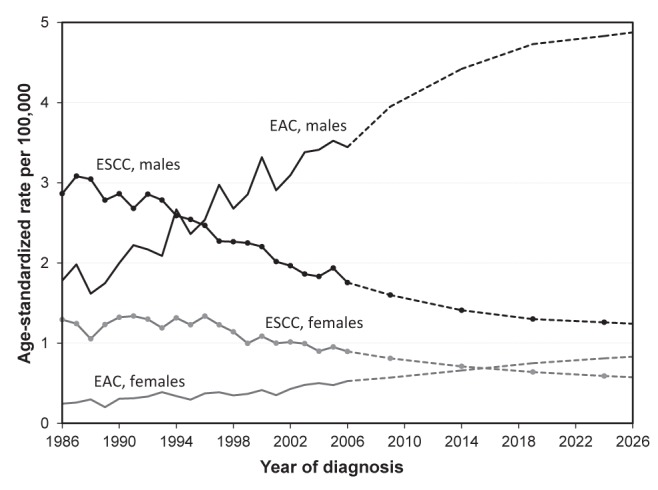
Age-standardized incidence rates for esophageal adenocarcinoma (EAC) and esophageal squamous cell carcinoma (ESCC) according to sex in Canada. Solid lines represent actual observed rates during the period from 1986 to 2006. Dashed lines indicate projected rates up to 2026
In terms of anatomical location, EAC has increased to the greatest extent in the lower one-third of the esophagus, rising on average by 4.8% per year in men (1.1 to 2.4 per 100,000) and 5.0% per year in women (0.1 to 0.4 per 100,000). Of all new esophageal cancer cases ascribed to a specific location, 69% now occur in the lower one-third of this organ (Table 1) and the majority of cases in the lower one-third are EAC (71%) (Table 1). In the nearby gastroesophageal junction and gastric cardia (region of the stomach nearest to the esophagus), in contrast, incidence rates for adenocarcinoma increased only slightly in the period from 1986 to 2006 (0.6% per year, both sexes; data not shown).
Compared with the rising rates of EAC, ESCC incidence in Canada has declined across all age groups and in all parts of the esophagus. Since the early 1990s, incidence rates for ESCC have decreased by a mean of 3.3% per year in men (3.0 to 1.8 per 100,000, 1992 to 2006) and 3.2% per year in women (1.3 to 0.9 per 100,000, 1994 to 2006). Among all ESCC cases ascribed to a specific location, 63% occur in the middle and upper one-thirds of the esophagus. ESCC is still twice as common as EAC in Canadian women, but only one-half as common in Canadian men (Figure 1). Projection of these trends suggests that rates of ESCC will decline an additional 30% in both men (to 1.3 per 100,000) and women (to 0.6 per 100,000) by 2026. If these projections hold, ESCC will be approximately four times less common than EAC among men by 2026, whereas the two subtypes will occur at approximately equivalent rates among women (Figure 1).
Relative survival
Survival rates for individuals with esophageal cancer are low. In Canada, individuals diagnosed with this cancer had a five-year relative survival ratio of 13% compared with similar individuals in the general population (Table 1). Five-year survival was similar regardless of the sex of the person diagnosed, whether the cancer occurred in the upper, middle or lower esophagus, or whether the cancer was EAC or ESCC. However, survival generally decreases with age at diagnosis, from 18% among individuals 15 to 44 years of age to 10% among those 75 to 99 years of age. The age-standardized five-year relative survival ratio increased by 3% from 1992 to 1994 (10%), to 2004 to 2006 (13%).
DISCUSSION
Rates of esophageal cancer in Canada are relatively low, and similar to those in the United States, Australia, New Zealand and northern Europe, but less than those in China, India, southern Asia and southeastern Africa (1). However, the two major subtypes of esophageal cancer – EAC and ESCC – show opposing incidence trends: rates of EAC roughly doubled (increase of approximately 4% per year), whereas rates of ESCC declined by one-third (decrease of approximately 3% per year) in Canada during the period 1986 to 2006. Similar or greater changes in EAC and ESCC have been reported for British Columbia and Ontario (16,18). Regional variation in EAC across Canada may be attributable, in part, to differing rates among ethnic groups (17). Our projections suggest that rates of EAC will continue to rise in Canada (approximately 50% increase by 2026, compared with 2006 levels) and rates of ESCC will continue to fall (approximately 30% decrease by 2026, compared with 2006 levels). It should be noted, however, that the projected rates are only estimates, and depend on the assumption that past trends continue.
Risk factors
The risk factors for esophageal cancer differ between EAC and ESCC (summarized in Table 2) (32–35). EAC is most strongly associated with three often related conditions: gastroesophageal reflux disease (GERD), damage to the lower esophagus resulting in the development of abnormal tissue (‘Barrett’s esophagus’) and obesity. In contrast, the dominant risk factors for ESCC are tobacco smoke and alcohol consumption. In terms of protective effects, dietary fruits and vegetables reduce the risk of both subtypes of esophageal cancer. Chronic inflammation of the stomach due to infection by Helicobacter pylori may also reduce the risk of EAC by decreasing gastric acidity (36). Worldwide, variation in the incidence of esophageal cancer may reflect the fact that EAC risk factors are more common in developed countries, whereas those for ESCC are more common in developing countries (34).
TABLE 2.
Risk factors and strength of association for esophageal cancers
| Risk factor | EAC | ESSC |
|---|---|---|
| Old age | +++ | +++ |
| Male sex | +++ | +++ |
| Barrett’s esophagus | +++ | n/a |
| Gastroesophageal reflux | ++ | n/a |
| Obesity | ++ | n/a |
| Tobacco use | ++ | +++ |
| Family history | ± | + |
| Helicobacter pylori infection | – | ± |
| Frequent consumption of: | ||
| Alcohol | ± | +++ |
| Saturated fats and red meat | + | ± |
| Hot or spicy foods and liquids | n/a | + |
| Fruits and vegetables | – | – |
Very strong effect;
Moderate effect;
Marginal effect;
Equivocal evidence;
– Protective effect. EAC Esophageal adenocarcinoma; ESSC Esophageal squamous cell carcinoma; n/a No proven effect
The prevalences of GERD and obesity have increased rapidly in Western countries over the past two decades (37–40), supporting causal associations with EAC. Nevertheless, the actual incidence of EAC among individuals with GERD is still very low except among white males >60 years of age (41). Given the relative rarity of EAC compared with the high incidence of GERD, developing a screening program for EAC may be impractical and has not been shown to be effective (42). Obesity, in addition to its contribution to the development of GERD, is an important independent risk factor for EAC (43). In particular, abdominal obesity (‘male-pattern obesity’) may be important and help explain the higher rates of EAC among men compared with women (43). Tobacco smoke, family history, and consumption of red meats and saturated fats also contribute to EAC risk, but less strongly than do GERD and obesity (32). Although there is no strong evidence that established therapies to treat GERD reduce the incidence of EAC (44), certain therapies, such a proton pump inhibitors, have shown promise in preventing the dysplasia that can lead to EAC (45).
Regarding ESCC, tobacco smoke and alcohol consumption both elevate risk in a dose-dependent fashion and, together, increase risk synergistically (46). Reduced rates of cigarette smoking in Canada (47,48) may help explain the declining incidence of ESCC. A diet lacking in fruits and vegetables can also increase the risk of ESCC and, together with smoking and alcohol, may account for 90% of this type of esophageal cancer (35).
Staging and treatment
Treatment of esophageal cancer depends on tumour stage. Diagnosis is usually by endoscopy and biopsy. Additional investigations may include endoscopic ultrasound, computed tomography scan and positron emission tomography scan. In Canada, data from the Manitoba cancer registry (2005 to 2007) show that one-half of the cases (of a known stage) of esophageal cancer were late stage (stage IV) at diagnosis, while the remaining were roughly equally distributed among earlier stages (stage I, II and III) (49). This pattern is consistent for EAC and ESCC. The survival rate of people diagnosed with stage IV is low, whereas those diagnosed in stages I to III have a good to moderate prognosis (50).
The standard treatment for early esophageal cancer is surgery (51). Patients with esophageal carcinoma in situ and very early invasive cancer may be treated with local therapies using endoscopy. More advanced tumours can be treated by surgery or combined chemotherapy and radiation therapy. Triple modality therapy (usually chemoradiation followed by surgery) is being recommended more frequently (52). In Canada, the five-year relative survival rate for individuals diagnosed with esophageal cancer is 13%, which is slightly higher than that in Europe (53) but slightly lower than that in the United States (54). Such poor survival reflects the fact that many people are diagnosed after the esophageal cancer has metastasized or spread to other organs. For these people, treatment may include a stent to relieve obstruction of the esophagus, radiotherapy or chemotherapy, or a combination of these treatments.
CONCLUSION.
In Canada, the incidence of lower EAC has increased rapidly among men and women, while ESCC has declined. Increasing rates of EAC may reflect the rising prevalence of obesity and gastroesophageal reflux disease. Decreases in ESCC may be the result of the declining prevalence of smoking. Efforts aimed at controlling tobacco use and obesity (eg, public education regarding tobacco cessation, healthy diet and healthy weight), could reduce the incidence of esophageal cancer. Although the prognosis for individuals with esophageal cancer is generally poor, five-year relative survival rates have improved slightly since the early 1990s, possibly due to earlier detection and multimodality treatments. Promising future directions include identifying high-risk individuals who may benefit from screening, continued research into better therapeutic treatment regimens and improved palliative therapies given the low survival rates of esophageal cancer.
Acknowledgments
The data contained in this article were provided to the Public Health Agency of Canada from the Canadian Cancer Registry database at Statistics Canada with the knowledge and consent of the provincial and territorial cancer registries which supply the data to Statistics Canada. Their cooperation is gratefully acknowledged. The Steering Committee for Canadian Cancer Statistics includes individuals from the Canadian Cancer Society, the Public Health Agency of Canada, Statistics Canada, the Canadian Council of Cancer Registries, as well as researchers based in universities and provincial or territorial cancer agencies. This committee is responsible for the annual production of Canadian Cancer Statistics (15).
Footnotes
DISCLAIMER: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008 v12, Cancer Incidence and Mortality Worldwide: IARC CancerBase No 10 [Internet] Lyon, France: International Agency for Research on Cancer; < http://globocan.iarc.fr> (Accessed December 7, 2011) [Google Scholar]
- 2.Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: Defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006;24:2137–50. doi: 10.1200/JCO.2005.05.2308. [DOI] [PubMed] [Google Scholar]
- 3.IARC. Cancer Incidence in Five Continents, Vol IX. Lyon, France: International Agency for Research on Cancer; 2007. Report No.: Scientific Publications No. 160. [Google Scholar]
- 4.Kamangar F, Malekzadeh R, Dawsey SM, Saidi F. Esophageal cancer in Northeastern Iran: A review. Arch Iran Med. 2007;10:70–82. [PubMed] [Google Scholar]
- 5.Trivers KF, Sabatino SA, Stewart SL. Trends in esophageal cancer incidence by histology, United States, 1998–2003. Int J Cancer. 2008;123:1422–8. doi: 10.1002/ijc.23691. [DOI] [PubMed] [Google Scholar]
- 6.Powell J, McConkey CC, Gillison EW, Spychal RT. Continuing rising trend in oesophageal adenocarcinoma. Int J Cancer. 2002;102:422–7. doi: 10.1002/ijc.10721. [DOI] [PubMed] [Google Scholar]
- 7.Armstrong RW, Borman B. Trends in incidence rates of adenocarcinoma of the oesophagus and gastric cardia in New Zealand, 1978–1992. Int J Epidemiol. 1996;25:941–7. doi: 10.1093/ije/25.5.941. [DOI] [PubMed] [Google Scholar]
- 8.Lord RVN, Law MG, Ward RL, Giles GG, Thomas RJS, Thursfield V. Rising incidence of oesophageal adenocarcinoma in men in Australia. J Gastroenterol Hepatol. 1998;13:56–62. doi: 10.1111/j.1440-1746.1998.tb00646.x. [DOI] [PubMed] [Google Scholar]
- 9.Hansen S, Wiig JN, Giercksky KE, Tretli S. Esophageal and gastric carcinoma in Norway 1958–1992: Incidence time trend variability according to morphological subtypes and organ subsites. Int J Cancer. 1997;71:340–4. doi: 10.1002/(sici)1097-0215(19970502)71:3<340::aid-ijc5>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 10.Sihvo EIT, Salminen JT, Ramo OJ, Salo JA. The epidemiology of oesophageal adenocarcinoma: Has the cancer of gastric cardia an influence on the rising incidence of oesophageal adenocarcinoma? Scand J Gastroenterol. 2000;35:1082–6. doi: 10.1080/003655200451216. [DOI] [PubMed] [Google Scholar]
- 11.Vizcaino AP, Moreno V, Lambert R, Parkin DM. Time trends incidence of both major histologic types of esophageal carcinomas in selected countries, 1973–1995. Int J Cancer. 2002;99:860–8. doi: 10.1002/ijc.10427. [DOI] [PubMed] [Google Scholar]
- 12.Tuyns AJ. Oesophageal cancer in France and Switzerland: Recent time trends. Eur J Cancer Prevent. 1992;1:275–8. doi: 10.1097/00008469-199204000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Botterweck AAM, Schouten LJ, Volovics A, Dorant E, Van Den Brandt PA. Trends in incidence of adenocarcinoma of the oesophagus and gastric cardia in ten European countries. Int J Epidemiol. 2000;29:645–54. doi: 10.1093/ije/29.4.645. [DOI] [PubMed] [Google Scholar]
- 14.Pohl H, Welch HG. The role of overdiagnosis and reclassification in the marked increase of esophageal adenocarcinoma incidence. J Natl Cancer Inst. 2005;97:142–6. doi: 10.1093/jnci/dji024. [DOI] [PubMed] [Google Scholar]
- 15.Canadian Cancer Society’s Steering Committee on Cancer Statistics. Canadian Cancer Statistics 2012. Toronto: Canadian Cancer Society; 2012. [Google Scholar]
- 16.Bashash M, Shah A, Hislop G, Brooks-Wilson A, Le N, Bajdik C. Incidence and survival for gastric and esophageal cancer diagnosed in British Columbia, 1990 to 1999. Can J Gastroenterol. 2008;22:143–8. doi: 10.1155/2008/645107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tinmouth J, Green J, Ko Y, et al. A population-based analysis of esophageal and gastric cardia adenocarcinomas in Ontario, Canada: Incidence, risk factors, and regional variation. J Gastrointest Surg. 2011;15:782–90. doi: 10.1007/s11605-011-1450-9. [DOI] [PubMed] [Google Scholar]
- 18.Parfitt JR, Miladinovic Z, Driman DK. Increasing incidence of adenocarcinoma of the gastroesophageal junction and distal stomach in Canada: An epidemiological study from 1964 to 2002. Can J Gastroenterol. 2006;20:271–6. doi: 10.1155/2006/175751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Statistics Canada. Canadian Cancer Registry (CCR) Ottawa: Minister of Industry; Updated May 26, 2010. < www.statcan.gc.ca/cgi-bin/imdb/p2SVpl?Function=getSurvey&SDDS=3207&lang=en&db=imdb&adm=8&dis=2;> (Accessed September 21, 2010) [Google Scholar]
- 20.Statistics Canada. Vital Statistics – Death Database. Ottawa: Minister of Industry; Updated January 26, 2010; < www.statcan.gc.ca/cgi-bin/imdb/p2SVpl?Function=getSurvey&SDDS=3233&lang=en&db=imdb&adm=8&dis=2;> (Accessed September 21, 2010). [Google Scholar]
- 21.Statistics Canada. Definitions, data sources and methods. Ottawa: Minister of Industry; Updated July 6, 2010 < www.statcan.gc.ca/concepts/index-eng.htm;> (Accessed September 21, 2010) [Google Scholar]
- 22.Fritz A, Percy C, Jack A, et al., editors. International Classification of Diseases for Oncology. 3rd edn. Geneva: World Health Organization; 2000. [Google Scholar]
- 23.Kim H, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 24.Fekjaer H, Moller B. Nordpred: R ( www.r-project.org) & S-PLUS ( www.insightful.com) functions for prediction of cancer incidence (as used in the Nordpred Project), 2003 < www.kreftregisteret.no/software/nordpred/> (Accessed January 19, 2012)
- 25.Møller B, Fekjaer H, Hakulinen T, et al. Prediction of cancer incidence in the Nordic countries up to the year 2020. Eur J Cancer Prevent. 2002;11:S1–S96. [PubMed] [Google Scholar]
- 26.Brenner H, Ziegler H. Monitoring and projecting cancer incidence in Saarland, Germany, based on age-cohort analyses. J Epidemiol and Comm Health. 1992;46:15–20. doi: 10.1136/jech.46.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brenner H, Gefeller O. An alternative approach to monitoring cancer patient survival. Cancer. 1996;78:2004–10. [PubMed] [Google Scholar]
- 28.Dickman PW. Estimating and modeling relative survival using SAS. < www.pauldickman.com/rsmodel/sas_colon/> (Accessed January, 2010)
- 29.Ederer F, Heise H. The effect of eliminating deaths from cancer on general population survival rates, methodological note 11. End Results Evaluation section, National Cancer Institute; 1959. [Google Scholar]
- 30.Ellison LF. Measuring the effect of including multiple cancers in survival analyses using data from the Canadian Cancer Registry. Cancer Epidemiol. 2010;34:550–5. doi: 10.1016/j.canep.2010.06.015. [DOI] [PubMed] [Google Scholar]
- 31.Statistics Canada. Cancer Survival Statistics. Ottawa: Minister of Industry; 2011. Report No. Catalogue 82-226-XIE-2011001. [Google Scholar]
- 32.Falk GW. Risk factors for esophageal cancer development. Surg Oncol Clin N Am. 2009;18:469. doi: 10.1016/j.soc.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 33.Enzinger PC, Mayer RJ. Esophageal cancer. N Engl J Med. 2003;349:2241–52. doi: 10.1056/NEJMra035010. [DOI] [PubMed] [Google Scholar]
- 34.Hongo M, Nagasaki Y, Shoji T. Epidemiology of esophageal cancer: Orient to Occident. Effects of chronology, geography and ethnicity. J Gastroenterol Hepatol. 2009;24:729–35. doi: 10.1111/j.1440-1746.2009.05824.x. [DOI] [PubMed] [Google Scholar]
- 35.Engel LS, Chow WH, Vaughan TL, et al. Population attributable risks of esophageal and gastric cancers. J Natl Cancer Inst. 2003;95:1404–13. doi: 10.1093/jnci/djg047. [DOI] [PubMed] [Google Scholar]
- 36.Chow W, Blaser MJ, Blot WJ, et al. An inverse relation between cagA+ strains of Helicobacter pylori infection and risk of esophageal and gastric cardia adenocarcinoma. Cancer Res. 1998;58:588–90. [PubMed] [Google Scholar]
- 37.El-Serag HB. Time trends of gastroesophageal reflux disease: A systematic review. Clin Gastroenterol Hepatol. 2007;5:17–26. doi: 10.1016/j.cgh.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 38.Tjepkema M. Adult obesity. Health Reports/Statistics Canada, Canadian Centre for Health Information. 2006;17:9–25. [PubMed] [Google Scholar]
- 39.Veugelers PJ, Porter GA, Guernsey DL, Casson AG. Obesity and lifestyle risk factors for gastroesophageal reflux disease, Barrett esophagus and esophageal adenocarcinoma. Dis Esophag. 2006;19:321–8. doi: 10.1111/j.1442-2050.2006.00602.x. [DOI] [PubMed] [Google Scholar]
- 40.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. J Am Med Assoc. 2002;288:1723–7. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 41.Rubenstein JH, Scheiman JM, Sadeghi S, Whiteman D, Inadomi JM. Esophageal adenocarcinoma incidence in individuals with gastroesophageal reflux: Synthesis and estimates from population studies. Am J Gastroenterol. 2011;106:254–60. doi: 10.1038/ajg.2010.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rubenstein JH, Sonnenberg A, Davis J, McMahon L, Inadomi JM. Effect of a prior endoscopy on outcomes of esophageal adenocarcinoma among United States veterans. Gastrointest Endosc. 2008;68:849–55. doi: 10.1016/j.gie.2008.02.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vial M, Grande L, Pera M. Epidemiology of adenocarcinoma of the esophagus, gastric cardia, and upper gastric third. Recent Results Cancer Res. 2010;182:1–17. doi: 10.1007/978-3-540-70579-6_1. [DOI] [PubMed] [Google Scholar]
- 44.Lagergren J, Ye W, Lagergren P, Lu Y. The risk of esophageal adenocarcinoma after antireflux surgery. Gastroenterology. 2010;138:1297–301. doi: 10.1053/j.gastro.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 45.Triadafilopoulos G. Proton pump inhibitors in Barrett’s esophagus: Pluripotent but controversial. European Surgery – Acta Chirurgica Austriaca. 2008;40:58–65. [Google Scholar]
- 46.Pandeya N, Williams G, Green AC, Webb PM, Whiteman DC. Alcohol consumption and the risks of adenocarcinoma and squamous cell carcinoma of the esophagus. Gastroenterology. 2009;136:1215, 1224.e2. doi: 10.1053/j.gastro.2008.12.052. [DOI] [PubMed] [Google Scholar]
- 47.Gilmore J. Report on Smoking in Canada, 1985–2001. Ottawa: Ministry of Industry; 2002. Report No. Catalogue no. 82F0077XIE. [Google Scholar]
- 48.Shields M. Smoking bans: Influence on smoking prevalence. Health Reports / Statistics Canada, Canadian Centre for Health Information. 2007;18:9–24. [PubMed] [Google Scholar]
- 49.Canadian Cancer Society’s Steering Committee on Cancer Statistics. Canadian Cancer Statistics. Toronto: Canadian Cancer Society; 2010. [Google Scholar]
- 50.Daly JM, Fry WA, Little AG, et al. Esophageal cancer: Results of American College of Surgeons patient care evaluation study. J Am Coll Surg. 2000;190:562–73. doi: 10.1016/s1072-7515(00)00238-6. [DOI] [PubMed] [Google Scholar]
- 51.Schuchert MJ, Luketich JD, Landreneau RJ. Management of esophageal cancer. Curr Prob Surg. 2010;47:845–946. doi: 10.1067/j.cpsurg.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 52.Malthaner R, Wong RKS, Spithoff K. Preoperative or postoperative therapy for resectable oesophageal cancer: An updated practice guideline. Clin Oncol. 2010;22:250–6. doi: 10.1016/j.clon.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 53.Brenner H, Francisci S, de Angelis R, et al. Long-term survival expectations of cancer patients in Europe in 2000–2002. Eur J Cancer. 2009;45:1028–41. doi: 10.1016/j.ejca.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 54.Altekruse SF, Kosary CL, Krapcho M, et al. SEER Cancer Statistics Review 1975–2007. National Cancer Institute; Bethesda, MD: 2011. [Google Scholar]


