Abstract
Study Design
Combined prospective randomized controlled trial and observational cohort study of intervertebral disc herniation (IDH), an as-treated analysis.
Objective
To determine modifiers of the treatment effect (TE) of surgery (the difference between surgical and nonoperative outcomes) for intervertebral disc herniation (IDH) using subgroup analysis.
Summary of Background Data
SPORT demonstrated a positive surgical TE for IDH at the group level. However, individual characteristics may affect TE. No prior studies have evaluated TE modifiers in IDH.
Methods
IDH patients underwent either discectomy (n=788) or nonoperative care (n=404) and were analyzed according to treatment received. Thirty-seven baseline variables were used to define subgroups for calculating the time-weighted average TE for the Oswestry Disability Index (ODI) over 4 years (TE=ΔODIsurgery-ΔODInonoperative). Variables with significant subgroup by* treatment interactions (p<0.1) were simultaneously entered into a multivariate model to select independent TE predictors.
Results
All analyzed subgroups improved significantly more with surgery than with nonoperative treatment (p<0.05). In minimally adjusted univariate analyses: being married, absence of joint problems, worsening symptom trend at baseline, high school education or less, older age, no worker’s compensation, longer duration of symptoms, and an SF-36 mental component score (MCS) less than 35 were associated with greater TEs. Multivariate analysis demonstrated: being married (TE −15.8 vs. −7.7 single, p<0.001), absence of joint problems (TE −14.6 vs. −10.3 joint problems, p=0.012), and worsening symptoms (TE −15.9 vs. −11.8 stable symptoms, p=0.032) were independent TE modifiers. TE’s were greatest in married patients with worsening symptoms (−18.3) vs. single patients with stable symptoms (−7.8).
Conclusions
IDH patients who met strict inclusion criteria improved more with surgery than with nonoperative treatment, regardless of specific characteristics. However, being married, without joint problems, and worsening symptom trend at baseline were associated with a greater treatment effect.
INTRODUCTION
The Spine Patient Outcomes Research Trial (SPORT) demonstrated a clear benefit of surgery compared to nonoperative treatment for lumbar intervertebral disc herniation (IDH) over four years.1–3 However, these findings were at the group level, and it has been shown that demographic, radiographic, clinical, and psychological characteristics can affect individual outcomes.4–13 The Institute of Medicine and Congress have defined comparative effectiveness research as a top priority with a goal of “assisting consumers, clinicians, purchasers, and policy makers to make informed decisions that will improve health care at both the individual and population levels.”14 As such, we wanted to determine which individuals were the best candidates for surgical and nonoperative treatment. Most prior studies evaluating potential predictors of outcomes have focused on surgical outcomes only.5,8,12,13 While these studies were helpful, the decision between surgical and nonoperative treatment should be based on the relative benefit of one treatment compared to the other (i.e. the treatment effect of surgery, TE). By considering only predictors of surgical outcome rather than factors that affect TE in making treatment decisions, surgeons may erroneously suggest nonoperative treatment to patients likely to fail without surgery and surgical treatment to patients who could succeed nonoperatively. In an ideal setting, physicians would be able to predict the likely TE for an individual patient based on their specific characteristics in order to make their treatment decision a truly informed choice. To do this, the predicted surgical and nonoperative outcomes must be known. While the Maine Lumbar Spine Study (MLSS) compared surgical and nonoperative outcomes for IDH patients, it did not focus on subgroup analyses to determine TE modifiers.6,15,16 As such, SPORT is the first large-scale trial with both surgical and nonoperative arms that is able to evaluate a large number of potential TE modifiers.
Previous SPORT investigations have focused on subgroups that authors selected a priori as potential TE modifiers.9,10,17,18 We felt that a systematic analysis of all potential TE modifiers would be beneficial in order to determine which patient characteristics were associated with TE and could be used to counsel IDH patients making informed treatment decisions. As such, the goals of this study were to 1) perform subgroup analyses for all potential TE modifiers, and 2) develop a multivariate model to determine independent TE modifiers.
MATERIALS AND METHODS
Study Design
SPORT consisted of a randomized controlled trial with a concurrent observational cohort study conducted in 11 states at 13 institutions with multidisciplinary spine practices.19 In the first year of follow-up in the randomized trial, 43% of patients assigned to surgery did not have surgery, and 41% of patients assigned to non-operative treatment did have surgery.3 By 4 years, 41% of the patients randomized to surgery had still not undergone surgery, and 45% of the patients assigned to non-operative treatment had received surgery.2 Given this rate of protocol nonadherence and the consistency of the findings between the randomized and the observational cohorts, the data were combined in an as-treated analysis in this study.1,2 The rational for this decision has been discussed previously.20
Patient Population
Patients were considered for inclusion in the study if they were over 18 years old, had radicular pain with a positive nerve root tension sign or neurologic deficit, a confirmatory imaging study demonstrating IDH corresponding to their symptoms, and presence of symptoms for at least six weeks. Exclusion criteria included cauda equina syndrome, malignancy, significant deformity, prior back surgery and other established contraindications to elective surgery.19
Study Interventions
Surgery consisted of a standard open diskectomy with examination and decompression of the involved nerve root.21,22 Surgeons were encouraged to use loupe magnification or a microscope. The non-operative treatment group received “usual care”--defined as including at least physical therapy, education and counseling with home exercise instruction, and non-steroidal anti-inflammatory drugs if tolerated. Physicians were instructed to individualize non-operative treatment and explore a wide range of non-operative options.19
Imaging Studies
Imaging studies included MRI in 97% of the patients and CT scan in the remaining 3%. Radiographic assessment was performed by the treating physician at the time of initial evaluation. Herniation location was classified as central, posterolateral, foraminal, or far lateral.23 Herniation morphology was classified as a protrusion, extrusion or sequestration.23
Baseline Characteristics and Primary Outcome Measure
At baseline, patients and clinicians answered questionnaires evaluating demographic, socioeconomic, clinical, and radiographic characteristics.1,3 Baseline scores on the Short-Form 36 (SF-36),24 AAOS/Modems version of the Oswestry Disability Index (ODI),25 Sciatica Bothersomeness Index,26,27 and Leg and Back Pain Bothersomeness (0–6 point Likert-type scale) were also recorded. The ODI was also recorded at 6 weeks, 3 months, 6 months, 1 year and yearly thereafter out to 4 years. Thirty-seven variables were selected as potential modifiers of the treatment effect of surgery. Continuous variables were converted to categorical variables as follows: ODI defined by quartiles; Sciatica Bothersomeness and Age by the median; Duration of Symptoms categorized as 6 weeks, 6 weeks to 6 months, or greater than 6 months; Income as greater than $50,000, less than $50,000 or not working; and the SF-36 Mental Component Score (MCS) as less than or equal to 35 or greater than 35.28 Herniation Location was classified as posterolateral versus other (central, foraminal or far lateral), and Herniaton Level was defined as upper lumbar (L2–3 and L3–4), L4–5 or L5-S1.
Statistical Considerations
The primary aim of the analysis was to identify baseline variables that were significant indicators of differential treatment effects of surgery (i.e. variables with significant subgroup by*treatment interactions). The treatment effect (TE) of surgery was defined as:
Treatment Effect = Change in ODIsurgery - Change in ODInonoperative
In all analyses, TE was calculated as the time-weighted average (area under the curve) over 4 years. Note that a negative TE indicated that surgery was more effective than nonoperative treatment. To identify candidate variables, a “minimally-adjusted” analysis (controlling only for age, gender, center, and baseline ODI score) was performed for each of the thirty-seven variables to identify those that had substantial TE differences across subgroups. Those that were identified as potential TE modifiers (p<0.1) were then entered along with their treatment interaction terms into a longitudinal regression model that controlled for factors predicting treatment received or missing data in order to control for selection and attrition bias (age, gender, marital status, smoking status, race, compensation, herniation location, working status, stomach comorbidity, other comorbidity, self-rated health trend, duration of most recent episode, treatment preference, and baseline ODI score).2 Variables with significant treatment interaction terms (p<0.05) were identified as independent TE modifiers and included in the final multivariable mixed effects longitudinal regression model including a random individual effect to account for correlation between repeated measurements within individuals. The outcomes were stratified by modifiers and overall comparisons of area-under-the-curve across the four-year follow-up were made using a Wald test.29 This analytical approach, starting with “minimally adjusted” analyses with a less stringent (p<0.1) criterion for significance, was performed in order to ensure that no potential independent modifiers were missed in the first stage. In the second stage, the complete multivariate model was used with the traditional threshold of significance (p < 0.05) in order to definitively identify independent TE modifiers.
RESULTS
Patient Distribution and Follow-Up
There were 1,244 patients enrolled overall, with 501 in the randomized trial and 743 in the observational cohort. By 4 years, 805 (65%) had undergone surgery. Ninety-six percent of patients (1,196) had completed at least one follow-up visit and were included in the analysis. Completeness of follow-up ranged from 87% at 6 weeks to 65% at 4 years. Details can be found in the primary analysis.2
Minimally Adjusted Analyses
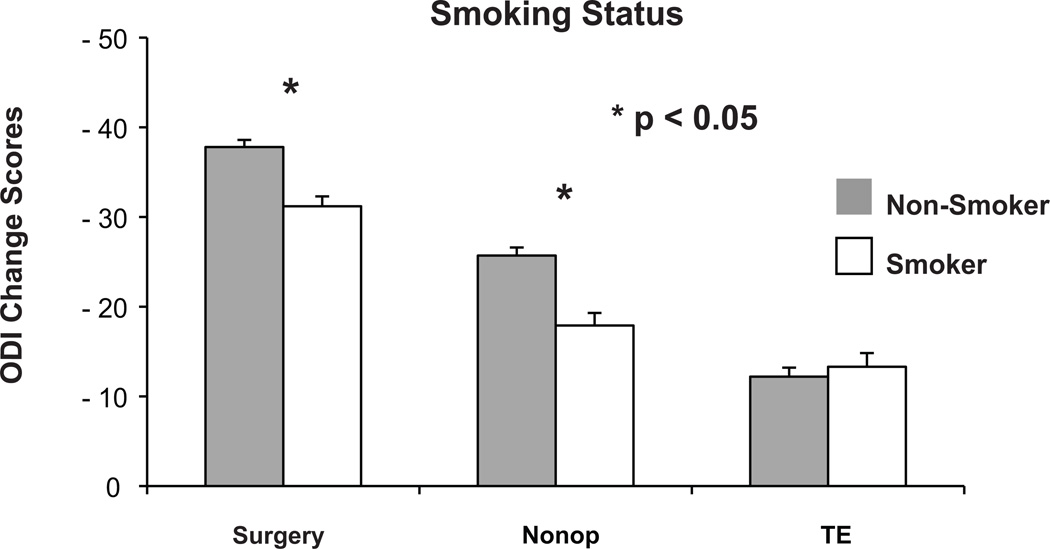
All examined subgroups with the exception of patients without insurance had a significant surgical TE (Table 1). While patients without insurance had a TE of −7, indicating surgery was more effective than nonoperative treatment, this subgroup was quite small (n=38) and its TE was associated with a broad confidence interval that crossed zero (−16.9 – 2.9). The majority of variables were significantly associated with both surgical and nonoperative outcomes, with the direction of the association always being the same for both treatments (e.g. smokers had worse surgical and nonoperative outcomes but similar TE as non-smokers, Figure 1). Age greater than 41 years (TE −13.3 vs. −10.6 for age less than 41 years, p = 0.06), the absence of joint problems (TE −12.6 vs. −8.2 for the presence of joint problems, p = 0.01), a high school education or less (TE −16.1 vs. −10.7 vs. for at least some college, p = 0.001), no worker’s compensation (TE −12.6 vs. −9.0 for receiving or applying for worker’s compensation, p = 0.06), duration of symptoms for over 6 months (TE −14.7 vs. −11.5 for 6 weeks to 6 months vs. −9.9 for 6 weeks, p = 0.09, Figure 2), being married (TE −14.2 vs. −10.3 for divorced vs. −5.2 for single, p < 0.001), worsening symptom trend at baseline (TE −15.4 vs. −12.4 for getting better vs. −10.7 for unchanging, p = 0.02), and an MCS score of less than 35 (TE −13.9 vs. −11.0 for MCS above 35, p = 0.1) were associated with greater treatment effects of surgery.
Table 1.
Area under curve subgroup results for Oswestry Disability Index (ODI) change scores, adjusted for age, gender, center, and baseline ODI score (Time weighted average 4 years treatment effects).
| N | Surgical (n = 788) |
Non-operative (n = 404) |
Treatment Effect†(95% CI) | |
|---|---|---|---|---|
| Baseline ODI ≤ 31 | 258 | −21.4 (1.5) | −5.2 (1.2) | −16.1 (−19.1, −13.1) |
| 31 < Baseline ODI ≤ 45 | 252 | −29.4 (1.3) | −14.9 (1.4) | −14.5 (−17.5, −11.4) |
| 45 < Baseline ODI ≤ 60 | 293 | −39.2 (1.1) | −23.1 (1.6) | −16 (−19.3, −12.8) |
| Baseline ODI > 60 | 386 | −50.8 (1) | −39.1 (1.6) | −11.7 (−14.9, −8.4) |
| p-value | <0.001 | <0.001 | 0.18 | |
| Sciatica Bothersomeness ≤ 16 | 625 | −37.3 (0.8) | −25.4 (0.9) | −11.9 (−13.7, −10) |
| Sciatica Bothersomeness > 16 | 556 | −33.7 (0.8) | −21.5 (1.1) | −12.2 (−14.5, −10) |
| p-value | 0.001 | 0.006 | 0.82 | |
| Age <= 41 | 644 | −35.6 (0.7) | −25 (1) | −10.6 (−12.6, −8.6) |
| Age > 41 | 548 | −35.7 (0.8) | −22.5 (0.9) | −13.3 (−15.3, −11.2) |
| p-value | 0.89 | 0.06 | 0.06 | |
| Female | 507 | −35 (0.8) | −22.3 (1) | −12.7 (−14.9, −10.5) |
| Male | 685 | −36.1 (0.7) | −24.7 (0.9) | −11.4 (−13.2, −9.5) |
| p-value | 0.31 | 0.068 | 0.35 | |
| Body Mass Index < 30 | 854 | −38.1 (0.6) | −25.6 (0.8) | −12.4 (−14.1, −10.7) |
| Body Mass Index ≤30 | 336 | −29.9 (1) | −18.1 (1.3) | −11.9 (−14.5, −9.2) |
| p-value | <0.001 | <0.001 | 0.71 | |
| Reflex Asymmetry | 481 | −36 (0.8) | −25.1 (1.1) | −10.9 (−13.1, −8.6) |
| No Reflex Asymmetry | 710 | −35.4 (0.7) | −22.8 (0.9) | −12.6 (−14.4, −10.7) |
| p-value | 0.60 | 0.095 | 0.24 | |
| Positive Straight Leg Raise | 970 | −35.8 (0.6) | −24.2 (0.8) | −11.6 (−13.2, −10) |
| Negative Straight Leg Raise | 221 | −34.4 (1.4) | −22.9 (1.4) | −11.4 (−14.7, −8.2) |
| p-value | 0.35 | 0.42 | 0.93 | |
| No Joint Problem | 963 | −37.1 (0.6) | −24.5 (0.8) | −12.6 (−14.2, −11) |
| Joint Problem | 221 | −28.2 (1.3) | −20 (1.4) | −8.2 (−11.3, −5.1) |
| p-value | <0.001 | 0.005 | 0.01 | |
| Not Depressed | 1044 | −36.5 (0.6) | −24.5 (0.7) | −12 (−13.5, −10.4) |
| Depressed | 141 | −28.9 (1.6) | −16.4 (1.9) | −12.5 (−16.4, −8.5) |
| p-value | <0.001 | <0.001 | 0.82 | |
| No Other Comorbidities** | 666 | −38.1 (0.7) | −25.8 (0.9) | −12.3 (−14.2, −10.4) |
| Other Comorbidities | 526 | −32.3 (0.8) | −21.2 (1) | −11.2 (−13.2, −9.1) |
| p-value | <0.001 | <0.001 | 0.41 | |
| No Missed Work | 318 | −37.9 (1) | −26.9 (1.3) | −11 (−13.7, −8.4) |
| Missed Work | 724 | −34.8 (0.7) | −23.7 (0.9) | −11.1 (−13, −9.3) |
| p-value | 0.015 | 0.04 | 0.96 | |
| No Opiod Use | 520 | −38.6 (0.9) | −27 (1) | −11.6 (−13.7, −9.5) |
| Opiod Use | 542 | −34.8 (0.8) | −22.8 (1.1) | −12 (−14.3, −9.8) |
| p-value | 0.001 | 0.005 | 0.80 | |
| No Prior Injections | 625 | −37.7 (0.8) | −25.7 (0.9) | −12 (−13.9, −10.1) |
| Prior Injections | 567 | −33.5 (0.8) | −21.3 (1) | −12.2 (−14.3, −10) |
| p-value | <0.001 | 0.001 | 0.91 | |
| No Insurance | 38 | −20.1 (3.1) | −13.1 (4.7) | −7 (−16.9, 2.9) |
| Insured | 1151 | −36.1 (0.5) | −24.1 (0.7) | −12 (−13.4, −10.5) |
| p-value | <0.001 | 0.019 | 0.33 | |
| No Litigation | 1110 | −36.9 (0.5) | −24.9 (0.7) | −11.9 (−13.4, −10.4) |
| Litigation Pending/Resolved | 81 | −17.4 (2) | −7.7 (2.7) | −9.7 (−15, −4.4) |
| p-value | <0.001 | <0.001 | 0.42 | |
| Dissatisfied with Symptoms | 1134 | −35.7 (0.6) | −23.7 (0.7) | −12 (−13.5, −10.5) |
| Satisfied with Symptoms or Neutral | 57 | −33.4 (2.9) | −24.7 (2.6) | −8.7 (−14.8, −2.6) |
| p-value | 0.44 | 0.69 | 0.30 | |
| Predominant back pain | 221 | −31.9 (1.3) | −21.8 (1.4) | −10.1 (−13.1, −7.1) |
| Predominant leg pain | 962 | −36.4 (0.6) | −24 (0.8) | −12.4 (−14, −10.8) |
| p-value | 0.002 | 0.18 | 0.18 | |
| High school education or less | 287 | −32.2 (1.1) | −16.1 (1.4) | −16.1 (−19, −13.2) |
| At least some college or more | 884 | −36.8 (0.6) | −26.1 (0.8) | −10.7 (−12.3, −9) |
| p-value | <0.001 | <0.001 | 0.001 | |
| Sensory Deficit | 603 | −34.6 (0.7) | −22.3 (1) | −12.3 (−14.3, −10.3) |
| Sensory Intact | 588 | −36.8 (0.8) | −24.9 (0.9) | −11.9 (−13.9, −9.9) |
| p-value | 0.046 | 0.055 | 0.78 | |
| Motor Deficit | 501 | −35.3 (0.8) | −23.8 (1.1) | −11.5 (−13.8, −9.2) |
| Motor Intact | 690 | −35.9 (0.7) | −23.8 (0.9) | −12.2 (−14, −10.4) |
| p-value | 0.56 | 1 | 0.66 | |
| Other Herniation Location | 272 | −32 (1.2) | −21.6 (1.3) | −10.4 (−13.3, −7.4) |
| Posterolateral Herniation | 919 | −36.6 (0.6) | −24.5 (0.8) | −12.1 (−13.7, −10.4) |
| p-value | <0.001 | 0.055 | 0.31 | |
| No Stomach Problem | 1042 | −36.5 (0.6) | −24.4 (0.7) | −12.2 (−13.7, −10.6) |
| Stomach Problem | 142 | −28 (1.6) | −17.3 (1.9) | −10.7 (−14.6, −6.7) |
| p-value | <0.001 | <0.001 | 0.49 | |
| No Hypertension | 1022 | −36 (0.6) | −24.1 (0.7) | −11.9 (−13.5, −10.3) |
| Hypertension | 163 | −33.4 (1.5) | −20.3 (1.7) | −13.1 (−16.6, −9.5) |
| p-value | 0.11 | 0.042 | 0.55 | |
| No Antidepressants Use | 1011 | −37.3 (0.6) | −25.6 (0.7) | −11.8 (−13.3, −10.2) |
| Taking Antidepressants | 51 | −22.1 (2.6) | −14.1 (3.6) | −8 (−15.3, −0.7) |
| p-value | <0.001 | 0.002 | 0.32 | |
| No NSAID Use | 578 | −36 (0.8) | −24.9 (1) | −11.1 (−13.3, −9) |
| Taking NSAID | 484 | −37.4 (0.9) | −25.3 (1) | −12.1 (−14.3, −9.9) |
| p-value | 0.23 | 0.78 | 0.52 | |
| No Physical Therapy | 314 | −37.6 (1.1) | −24.7 (1.2) | −12.9 (−15.6, −10.2) |
| Had Physical Therapy | 878 | −35 (0.6) | −23.4 (0.8) | −11.6 (−13.3, −9.9) |
| p-value | 0.036 | 0.35 | 0.42 | |
| No Lifting at Work | 497 | −39.7 (0.8) | −27.7 (1) | −12 (−14.2, −9.8) |
| Lifting at Work | 694 | −32.8 (0.7) | −20.6 (0.9) | −12.2 (−14.1, −10.3) |
| p-value | <0.001 | <0.001 | 0.89 | |
| Worker's Compensation | 208 | −27.2 (1.2) | −18.2 (1.8) | −9 (−12.5, −5.5) |
| No Worker's Compensation | 981 | −37.5 (0.6) | −24.9 (0.7) | −12.6 (−14.2, −11) |
| p-value | <0.001 | <0.001 | 0.06 | |
| L2-L3 / L3-4 Herniation | 88 | −32.7 (2.3) | −22.7 (2.2) | −10.1 (−15.6, −4.5) |
| L4-L5 Herniation | 456 | −36.8 (0.9) | −23.7 (1.1) | −13 (−15.3, −10.8) |
| L5-S1 Herniation | 647 | −35.1 (0.7) | −24.2 (0.9) | −10.9 (−12.8, −8.9) |
| p-value | 0.14 | 0.80 | 0.30 | |
| Protruding Herniation | 322 | −34.3 (1) | −21.6 (1.2) | −12.8 (−15.3, −10.3) |
| Extruded Herniation | 783 | −35.5 (0.7) | −24.6 (0.9) | −11 (−12.8, −9.1) |
| Sequestered Herniation | 86 | −41.9 (2.1) | −25.6 (2.4) | −16.4 (−21.6, −11.2) |
| p-value | 0.004 | 0.084 | 0.11 | |
| 6 Weeks or Less Duration | 165 | −40.6 (1.5) | −30.7 (1.7) | −9.9 (−13.6, −6.2) |
| 1.5 to 6 Months Duration | 765 | −36.3 (0.7) | −24.8 (0.8) | −11.5 (−13.2, −9.7) |
| More than 6 Months Duration | 262 | −30.5 (1.1) | −15.8 (1.4) | −14.7 (−17.7, −11.7) |
| p-value | <0.001 | <0.001 | 0.09 | |
| Non-Smoker | 607 | −37.8 (0.8) | −25.7 (0.9) | −12.2 (−14.1, −10.2) |
| Ex-Smoker | 298 | −35.1 (1.1) | −24.1 (1.3) | −11.1 (−13.8, −8.3) |
| Smoker | 282 | −31.2 (1.1) | −17.9 (1.4) | −13.3 (−16.3, −10.3) |
| p-value | <0.001 | <0.001 | 0.57 | |
| White | 1033 | −36.2 (0.6) | −24.9 (0.7) | −11.4 (−12.9, −9.8) |
| Black | 75 | −28 (2.5) | −12.8 (2.4) | −15.2 (−21, −9.4) |
| Other Race | 84 | −34.1 (2) | −21 (2.6) | −13.1 (−18.4, −7.8) |
| p-value | 0.004 | <0.001 | 0.40 | |
| Married | 835 | −36.9 (0.6) | −22.7 (0.8) | −14.2 (−15.9, −12.5) |
| Divorced/Widowed | 130 | −29.1 (1.6) | −18.9 (2.1) | −10.3 (−14.5, −6) |
| Single | 212 | −35.4 (1.4) | −30.1 (1.6) | −5.2 (−8.5, −2) |
| p-value | <0.001 | <0.001 | <0.001 | |
| Not working | 206 | −33.5 (1.3) | −18.8 (1.5) | −14.7 (−18, −11.4) |
| Income Over $50,000 | 446 | −38.7 (0.9) | −28.3 (1.1) | −10.4 (−12.8, −8.1) |
| Income Under $50,000 | 535 | −34 (0.8) | −22.2 (1) | −11.9 (−14, −9.8) |
| p-value | <0.001 | <0.001 | 0.11 | |
| Problem getting better | 179 | −42.3 (1.6) | −29.8 (1.4) | −12.4 (−15.8, −9.1) |
| Problem staying about the same | 534 | −35.8 (0.8) | −25.1 (1) | −10.7 (−12.8, −8.6) |
| Problem getting worse | 472 | −32.9 (0.8) | −17.5 (1.3) | −15.4 (−18, −12.9) |
| p-value | <0.001 | <0.001 | 0.02 | |
| Baseline MCS <= 35 | 263 | −30.2 (1.2) | −16.4 (1.4) | −13.9 (−16.9, −10.8) |
| Baseline MCS > 35 | 927 | −37 (0.6) | −26 (0.8) | −11 (−12.6, −9.4) |
| p-value | <0.001 | <0.001 | 0.10 | |
Treatment effect is the difference between the surgical and non−operative mean change from baseline.
Other comorbidities include: stroke, diabetes, osteoporosis, cancer, fibromyalgia, cerebrospinal fluid leak, PTSD, alcohol, drug dependency, heart, lung, liver, kidney, blood vessel, nervous system, hypertension, migraine, anxiety, stomach, or bowel problems.
Figure 1.
This graph demonstrates that non-smokers improved more with surgery and non-operative treatment than smokers though had a similar TE. This pattern was observed for the majority of variables in the minimally adjusted analyses.
Figure 2.
This graph demonstrates that patients with a longer duration of symptoms improved less with surgery and non-operative treatment than those with a shorter duration of symptoms but had a greater TE (minimally adjusted analysis).
Multivariate Analyses
The above variables that were associated with TE and their treatment interaction terms were added to a previously published model predicting the time-weighted average treatment effect over four years of follow-up.2 Being married, the absence of joint problems, and worsening symptom trend at baseline remained significant indicators of greater TE in this model (p < 0.05, Table 2, Figures 3–5). Age, education, worker’s compensation status, duration of symptoms, and baseline MCS scores were not significant independent TE modifiers in the multivariate model. To illustrate the range of TEs across subgroups, we compared outcomes among the various groups defined by marital status and symptom trend. Married patients with worsening symptoms (n=327) improved 37.9 points with surgery and 19.6 points with nonoperative treatment, yielding a TE of −18.3 (95% CI −21.3 to −15.2). In contrast, single patients with unchanging symptoms (n=107) improved 34.8 points with surgery and 27 points with nonoperative treatment, a TE of −7.8 (95% CI −12.2 to −3.4). This difference in TE (−18.3 vs. −7.8) was clinically and statistically significant (p < 0.001). Comparing subgroups defined by all three independent modifiers (i.e. marital status, joint problems, and symptom trend) was not possible due to the small number of single patients with joint problems and unchanging symptoms (n=15).
Table 2.
Area Under Curve subgroup results from the adjusted* as-treated Oswestry Disability Index (ODI) outcome analysis for the three significant treatment effect predictors (joint, martial status, baseline health trend) (Time weighted average 4 years treatment effects)
| Predictors | N | Surgical (n = 788) |
Non-operative (n = 404) |
Treatment Effect†(95% CI) |
|---|---|---|---|---|
| No Joint Problem | 963 | −37.9 (0.6) | −23.3 (0.7) | −14.6 (−16.3, −12.9) |
| Joint Problem | 221 | −30.8 (1.2) | −20.5 (1.4) | −10.3 (−13.4, −7.3) |
| p-value | <0.001 | 0.062 | 0.012 | |
| Married | 835 | −37.4 (0.6) | −21.5 (0.8) | −15.8 (−17.6, −14) |
| Divorced/Widowed | 130 | −33.1 (1.5) | −21.6 (2) | −11.5 (−15.7, −7.3) |
| Single | 212 | −36.2 (1.3) | −28.5 (1.5) | −7.7 (−10.9, −4.5) |
| p-value | 0.023 | <0.001 | <0.001 | |
| Problem getting better | 179 | −39.9 (1.5) | −27.3 (1.3) | −12.6 (−15.9, −9.3) |
| Problem staying about the same | 534 | −36.4 (0.8) | −24.6 (0.9) | −11.8 (−13.8, −9.7) |
| Problem getting worse | 472 | −34.8 (0.8) | −18.9 (1.2) | −15.9 (−18.5, −13.4) |
| p-value | 0.013 | <0.001 | 0.032 | |
Adjusted for age, gender, marital status, smoking status, race, compensation, herniation location, working status, stomach comorbidity, depression, othe**comorbidity, self-rated health trend, duration of most recent episode, treatment preference and baseline score (for SF-36 and ODI), and center.
Treatment effect is the difference between the surgical and non-operative mean change from baseline.
Other comorbidities include: stroke, diabetes, osteoporosis, cancer, fibromyalgia, cerebrospinal fluid leak, PTSD, alcohol, drug dependency, heart, lung, liver, kidney, blood vessel, nervous system, hypertension, migraine, anxiety, stomach, or bowel problems.
Figure 3.
This graph demonstrates that patients without joint problems improved more with surgery and non-operative treatment than those with joint problems and also had a greater TE (multivariate analysis).
Figure 5.
This graph demonstrates that patients getting worse at baseline improved less with surgery and non-operative treatment than patients getting better or with stable symptoms and also had a greater TE (multivariate analysis).
DISCUSSION
In order for discectomy candidates to make informed treatment decisions, they must have an estimate of the likely benefit of surgery compared to nonoperative treatment. While SPORT and the MLSS have demonstrated the long-term benefit of discectomy compared to nonoperative treatment for the “average” patient meeting the specific inclusion criteria of these studies, the associations between specific individual characteristcs and TE have not been formally evaluated.2,16 Consistent with the aims of comparative effectiveness research laid out by the Institute of Medicine, we shifted our focus from the population to the individual level.14 The current study demonstrated that patient characteristics consistently predicted both surgical and nonoperative outcomes in the same direction (i.e. smokers did worse with both surgical and nonoperative treatment compared to nonsmokers). These variables are useful for patient counseling about likely outcomes but are less useful for selecting treatment since they are not associated with differential TEs (i.e. smokers and nonsmokers had comparable TEs).
Similar to prior studies, we found that general health characteristics (e.g. comorbidities, body mass index, mental health problems, smoking, etc.) and socioeconomic factors (e.g. work status, insurance status, worker’s compensation, marital status, education, race, etc.) tended to be the strongest predictors of both surgical and nonoperative outcomes.4,6,8,12,16 Some disease specific findings like baseline ODI score, duration of symptoms, predominant pain location, and treatment with opioids were also relatively strong predictors of outcomes. Interestingly, specific physical exam findings such as a positive straight leg raise test, motor weakness, and asymmetric reflexes, which have been found to be associated with surgical outcomes in the past,4 were not associated with surgical or nonoperative outcomes in the current study. While evaluation of these individual characteristics can be useful for advising patients of their likely surgical and nonoperative outcomes, most of these variables do not assist in decision making since they are not associated with TE.
Thirty-seven variables were evaluated as TE modifiers in minimally adjusted, univariate analyses. These analyses revealed only eight characteristics that modified TE, even with a threshold of p < 0.1. The majority of these factors were general health (joint problems and MCS score) and socioeconomic (age, education, worker’s compensation, and marital status) factors, though the symptom trend at baseline and the duration of symptoms also modified TE. Multivariate analysis that simultaneously included all of the significant factors from the univariate analyses yielded only three independent TE modifiers (marital status, joint problems, and symptom trend at baseline). However, TE did vary markedly across these subgroups, ranging from −7.7 for single patients to −15.8 for married patients and from −7.8 for single patients with unchanging symptoms to −18.3 for married patients with worsening symptoms at baseline. While nearly all subgroups improved significantly more with surgery than with nonoperative treatment, the magnitude of this benefit varied significantly depending on individual patient characteristics.
The current analysis showed that marital status, joint problems, and health trend independently modified TE. It is well known that marriage is associated with positive health outcomes in many conditions, including cancer and heart failure.30–33 The literature on the role of marital status in spine outcomes is relatively sparse. Boos et al. found that patients with symptomatic disk herniations were more likely to be married than asymptomatic controls, and Lehman et al. reported that married patients with low back pain returned to work sooner than similar single patients.34,35 We found that married and single patients had similar surgical outcomes, but single patients improved significantly more with nonoperative treatment, leading to a significantly higher TE for married patients. The current study does not provide an explanation for why single patients did better with nonoperative treatment, though marital status is likely a marker for other characteristics that were responsible for these outcomes. In considering the role of joint problems, our findings are consistent with the those of Slover et al. who reported that the presence of comorbidities resulted in less improvement on the ODI following lumbar spine surgery.36,37 The current data showed that while the presence of joint problems reduced the improvement following both surgical and nonoperative treatment, this effect was more pronounced for surgical outcomes, resulting in a diminished TE for these patients. This may have represented a ceiling effect in that the degree of ODI improvement experienced by patients with joint problems could have been limited by their non-spine joint problems, even if their spine symptoms were completely resolved. The greater treatment effect observed for patients with worsening baseline symptoms was not surprising given that these patients were worsening with nonoperative treatment at baseline yet had surgical outcomes that were nearly as good as patients who were getting better at baseline.
Many prior studies have evaluated potential predictors of diskectomy outcomes, though none have evaluated TE modifiers. Abramovitz and Neff found that predominant leg pain, the absence of worker’s compensation, the presence of leg but not back pain on straight leg raising, a radicular distribution of pain, and reflex asymmetry predicted better surgical outcomes.4 We also found that predominant leg pain and the absence of worker’s compensation were associated with better surgical outcomes, though we did not find such associations with the straight leg raise test or reflex asymmetry. The MLSS also found that worker’s compensation was associated with worse outcomes at 10 years, though that analysis did not separate surgical and nonoperative outcomes and did not evaluate TE.16,17 In Peul et al.’s randomized trial comparing early discectomy to initial nonoperative care, no TE modifiers were found.11 However, this trial did not compare surgical and nonoperative outcomes but rather an early surgery group to a group consisting of a combination of patients treated with delayed surgery or continued nonoperative treatment. As such, direct comparison to the current study is difficult. Additional studies have also demonstrated the associations between clinical, psychological, and socioeconomic factors with discectomy outcomes, though these studies did not evaluate nonoperative outcomes and were thus unable to evaluate TE modifiers.8,12
There are a number of limitations of this study. While SPORT was designed with a randomized IDH cohort, the high rate of protocol non-adherence precluded meaningful interpretation of those data on an intent-to-treat basis alone.3 This phenomenon underscores the difficulty of conducting and analyzing a randomized trial of an elective surgical procedure that is primarily performed for pain relief. Additionally, the subgroup analyses used to evaluate potential TE modifiers were possibly underpowered for some variables (as indicated by broad confidence intervals around the TEs), and this may have resulted in the failure to detect some meaningful modifiers (Type II error). On the other hand, thirty-seven potential TE modifiers were evaluated, which put the study at risk for finding spurious associations due to chance alone (Type I error). We intentionally performed the initial analyses with minimally adjusted models to generate a list of potential TE modifiers that could be tested in the complete multivariate model. As such, the findings of these minimally adjusted analyses were subject to confounding and could yield slightly different results from those reported previously using the complete model.9,18 Five of eight variables found to be associated with TE in the minimally adjusted analyses did not remain significant in the multivariate model, indicating they were not independent TE modifiers. However, details from these analyses were included as clinicians might still find these relationships helpful in counseling patients. In order to improve the generalizability of our findings, nonoperative treatment was specified as “usual care”. Nonoperative treatment resulted in greater improvement in the current study compared to the MLSS, suggesting that it was generally effective.6,16 However, a specified, intensive program of nonoperative treatment may have been more effective for some patients. In addition, 35% of patients were lost to follow-up by four years, and this could have contributed to attrition bias if outcomes among those lost to follow-up were different from those who remained in the study. To address this, we did control for variables associated with missing data in the statistical model. Finally, we used the AAOS/Modems modified version of the ODI. This may give slightly different absolute results than either the original or the latest version (2.1a); however since our analysis was concerned with relative differences between treatment groups all using the same instrument, this is unlikely to have substantially affected the results.
Among patients meeting the strict inclusion criteria of SPORT, essentially all subgroups improved significantly more with surgery than with nonoperative treatment. This underscores the importance of ensuring that patients meet well-defined indications for surgery (i.e. duration of symptoms for at least 6 weeks, imaging consistent with clinical findings, and the presence of neurological signs) prior to undergoing discectomy. Though patients improved more with surgery than nonoperative treatment regardless of individual characteristics, the magnitude of benefit associated with surgery (i.e. TE) varied significantly across some subgroups. While the current study supported prior literature reporting the powerful effects of certain psychological, socioeconomic, and clinical factors on discectomy outcomes, only three variables (marital status, the presence or absence of joint problems, and symptom trend) were found to be significant independent TE modifiers.
How should these data be used in treatment decision making? We feel that the treatment decision in IDH should be based on the comparison of likely surgical and nonoperative outcomes (i.e. TE) rather than on the overall magnitude of change associated with either type of treatment. This is illustrated by the fact that patients with lower educational attainment, longer duration of symptoms, and lower MCS scores, characteristics associated with worse overall outcomes, actually had higher surgical TEs. Based on prior studies and anecdotal evidence, surgeons might be reluctant to offer surgery to these patients.4,8,12 However, the current data suggest these patients might benefit more from surgery (relative to their likely nonoperative outcomes) despite not improving to the same degree as patients without these characteristics. In the shared decision making process, this information should be used to create realistic expectations for surgical and nonoperative outcomes and allow patients to make well-informed decisions consistent with their values.38,39
So who should have surgery for intervertebral disk herniation? These data suggest diskectomy is appropriate treatment for all patients who meet the strict inclusion criteria of SPORT and select surgery after going through a thorough shared decision making process educating them about the risks, benefits and likely outcomes of surgical and nonoperative treatment. Future work will involve the creation and evaluation of real time computer models that can be used by individual patients with their providers in the clinical setting to predict their likely surgical and nonoperative outcomes.40
Figure 4.
This graph demonstrates that married patients improved more with surgery and less with non-operative treatment than single patients and also had a greater TE (multivariate analysis).
KEY POINTS.
Disc herniation patients who met strict inclusion criteria improved more with surgery than with nonoperative treatment, regardless of specific characteristics.
Being married, without joint problems, and worsening symptom trend at baseline were associated with a greater treatment effect of surgery.
Some characteristics associated with worse overall outcomes were associated with greater surgical treatment effects (i.e. low education, low MCS score, longer duration of symptoms).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical vs nonoperative treatment for lumbar disk herniation. The Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296:2451–2459. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT) Spine. 2008;33:2789–2800. doi: 10.1097/BRS.0b013e31818ed8f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disc herniation. The Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441–2445. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abramovitz JN, Neff SR. Lumbar disc surgery: results of the Prospective Lumbar Discectomy Study of the Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons. Neurosurgery. 1991;29:301–307. discussion 7–8. [PubMed] [Google Scholar]
- 5.Astrand P, Maattanen H, Vucetic N, Svensson O. Pain and orthopaedic and neurologic signs after lumbar discectomy: a 2-year followup. Clinical orthopaedics and related research. 2000:154–160. doi: 10.1097/00003086-200010000-00018. [DOI] [PubMed] [Google Scholar]
- 6.Atlas SJ, Keller RB, Chang Y, Deyo RA, Singer DE. Surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: five-year outcomes from the Maine Lumbar Spine Study. Spine. 2001;26:1179–1187. doi: 10.1097/00007632-200105150-00017. [DOI] [PubMed] [Google Scholar]
- 7.Atlas SJ, Tosteson TD, Blood EA, Skinner JS, Pransky GS, Weinstein JN. The impact of workers' compensation on outcomes of surgical and nonoperative therapy for patients with a lumbar disc herniation: SPORT. Spine (Phila Pa 1976) 35:89–97. doi: 10.1097/BRS.0b013e3181c68047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Junge A, Dvorak J, Ahrens S. Predictors of bad and good outcomes of lumbar disc surgery. A prospective clinical study with recommendations for screening to avoid bad outcomes. Spine. 1995;20:460–468. doi: 10.1097/00007632-199502001-00009. [DOI] [PubMed] [Google Scholar]
- 9.Lurie JD, Faucett SC, Hanscom B, et al. Lumbar discectomy outcomes vary by herniation level in the Spine Patient Outcomes Research Trial. The Journal of bone and joint surgery. 2008;90:1811–1819. doi: 10.2106/JBJS.G.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pearson AM, Blood EA, Frymoyer JW, et al. SPORT lumbar intervertebral disk herniation and back pain: does treatment, location, or morphology matter? Spine. 2008;33:428–435. doi: 10.1097/BRS.0b013e31816469de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peul WC, van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment for sciatica. The New England journal of medicine. 2007;356:2245–2256. doi: 10.1056/NEJMoa064039. [DOI] [PubMed] [Google Scholar]
- 12.Voorhies RM, Jiang X, Thomas N. Predicting outcome in the surgical treatment of lumbar radiculopathy using the Pain Drawing Score, McGill Short Form Pain Questionnaire, and risk factors including psychosocial issues and axial joint pain. Spine J. 2007;7:516–524. doi: 10.1016/j.spinee.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 13.Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. The Journal of bone and joint surgery. 2003;85-A:102–108. [PubMed] [Google Scholar]
- 14.Committee on Comparative Effectiveness Research Prioritization IoM. Initial National Priorities for Comparative Effectiveness Research. Washington DC: National Academies Press; 2009. [Google Scholar]
- 15.Atlas SJ, Deyo RA, Keller RB, et al. The Maine Lumbar Spine Study, Part II. 1-year outcomes of surgical and nonsurgical management of sciatica. Spine. 1996;21:1777–1786. doi: 10.1097/00007632-199608010-00011. [DOI] [PubMed] [Google Scholar]
- 16.Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the maine lumbar spine study. Spine. 2005;30:927–935. doi: 10.1097/01.brs.0000158954.68522.2a. [DOI] [PubMed] [Google Scholar]
- 17.Atlas SJ, Chang Y, Keller RB, Singer DE, Wu YA, Deyo RA. The impact of disability compensation on long-term treatment outcomes of patients with sciatica due to a lumbar disc herniation. Spine. 2006;31:3061–3069. doi: 10.1097/01.brs.0000250325.87083.8d. [DOI] [PubMed] [Google Scholar]
- 18.Atlas SJ, Tosteson TD, Blood EA, Skinner JS, Pransky GS, Weinstein JN. The impact of workers' compensation on outcomes of surgical and nonoperative therapy for patients with a lumbar disc herniation: SPORT. Spine (Phila Pa 1976) 2010;35:89–97. doi: 10.1097/BRS.0b013e3181c68047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Birkmeyer NJ, Weinstein JN, Tosteson AN, et al. Design of the Spine Patient outcomes Research Trial (SPORT) Spine. 2002;27:1361–1372. doi: 10.1097/00007632-200206150-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tosteson TD, Hanscom B, Blood EA, Lurie JD, Tosteson ANA, Weinstein JN. Statistical methods for cross-over in the SPORT lumbar disc herniation trial. International Society for the Study of the Lumbar Spine Annual Meeting; Hong Kong. 2007. [Google Scholar]
- 21.Delamarter R, McCullough J. Microdiscectomy and microsurgical laminotomies. In: Frymoyer J, editor. The Adult Spine: Princicples and Practice. 2nd ed. Philadelphia, PA: Lippincott-Raven Publishers; 1996. [Google Scholar]
- 22.Spengler DM. Lumbar discectomy. Results with limited disc excision and selective foraminotomy. Spine. 1982;7:604–607. [PubMed] [Google Scholar]
- 23.Fardon DF, Milette PC. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine. 2001;26:E93–E113. doi: 10.1097/00007632-200103010-00006. [DOI] [PubMed] [Google Scholar]
- 24.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical care. 1992;30:473–483. [PubMed] [Google Scholar]
- 25.Daltroy LH, Cats-Baril WL, Katz JN, Fossel AH, Liang MH. The North American spine society lumbar spine outcome assessment Instrument: reliability and validity tests. Spine. 1996;21:741–749. doi: 10.1097/00007632-199603150-00017. [DOI] [PubMed] [Google Scholar]
- 26.Atlas SJ, Deyo RA, Patrick DL, Convery K, Keller RB, Singer DE. The Quebec Task Force classification for Spinal Disorders and the severity, treatment, and outcomes of sciatica and lumbar spinal stenosis. Spine. 1996;21:2885–2892. doi: 10.1097/00007632-199612150-00020. [DOI] [PubMed] [Google Scholar]
- 27.Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health-related quality of life in patients with sciatica. Spine. 1995;20:1899–1908. doi: 10.1097/00007632-199509000-00011. discussion 909. [DOI] [PubMed] [Google Scholar]
- 28.Walsh TL, Homa K, Hanscom B, Lurie J, Sepulveda MG, Abdu W. Screening for depressive symptoms in patients with chronic spinal pain using the SF-36 Health Survey. Spine J. 2006;6:316–320. doi: 10.1016/j.spinee.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 29.Fitzmaurice G, Laird N, Ware J. Applied Longitudinal Analysis. Philadelphia, PA: John Wiley & Sons; 2004. [Google Scholar]
- 30.Chung ML, Lennie TA, Riegel B, Wu JR, Dekker RL, Moser DK. Marital status as an independent predictor of event-free survival of patients with heart failure. Am J Crit Care. 2009;18:562–570. doi: 10.4037/ajcc2009388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Graff-Baker A, Roman SA, Thomas DC, Udelsman R, Sosa JA. Prognosis of primary thyroid lymphoma: demographic, clinical, and pathologic predictors of survival in 1,408 cases. Surgery. 2009;146:1105–1115. doi: 10.1016/j.surg.2009.09.020. [DOI] [PubMed] [Google Scholar]
- 32.Schoenborn CA. Marital status and health: United States: 1999–2002. Advance data. 2004:1–32. [PubMed] [Google Scholar]
- 33.Sprehn GC, Chambers JE, Saykin AJ, Konski A, Johnstone PA. Decreased cancer survival in individuals separated at time of diagnosis: critical period for cancer pathophysiology? Cancer. 2009;115:5108–5116. doi: 10.1002/cncr.24547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boos N, Rieder R, Schade V, Spratt KF, Semmer N, Aebi M. 1995 Volvo Award in clinical sciences. The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine (Phila Pa 1976) 1995;20:2613–2625. doi: 10.1097/00007632-199512150-00002. [DOI] [PubMed] [Google Scholar]
- 35.Lehmann TR, Spratt KF, Lehmann KK. Predicting long-term disability in low back injured workers presenting to a spine consultant. Spine (Phila Pa 1976) 1993;18:1103–1112. doi: 10.1097/00007632-199306150-00023. [DOI] [PubMed] [Google Scholar]
- 36.Slover J, Abdu WA, Hanscom B, Weinstein JN. The impact of comorbidities on the change in short-form 36 and oswestry scores following lumbar spine surgery. Spine (Phila Pa 1976) 2006;31:1974–1980. doi: 10.1097/01.brs.0000229252.30903.b9. [DOI] [PubMed] [Google Scholar]
- 37.Slover J, Abdu WA, Hanscom B, Lurie J, Weinstein JN. Can condition-specific health surveys be specific to spine disease? An analysis of the effect of comorbidities on baseline condition-specific and general health survey scores. Spine (Phila Pa 1976) 2006;31:1265–1271. doi: 10.1097/01.brs.0000217635.67693.40. [DOI] [PubMed] [Google Scholar]
- 38.Weinstein JN, Clay K, Morgan TS. Informed patient choice: patient-centered valuing of surgical risks and benefits. Health affairs (Project Hope) 2007;26:726–730. doi: 10.1377/hlthaff.26.3.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weinstein JN. The missing piece: embracing shared decision making to reform health care. Spine (Phila Pa 1976) 2000;25:1–4. doi: 10.1097/00007632-200001010-00002. [DOI] [PubMed] [Google Scholar]
- 40.Tosteson TD, Pearson AM, Lurie J, et al. Improving predictions of outcomes for surgical and non-operative treatment of intervertebral disc herniation. International Society for the Study of the Lumbar Spine Annual Meeting; 2010; Auckland. 2010. [Google Scholar]