Abstract
Objective
To test whether gender differences in the prevalence of major depressive disorder differ by longitudinal patterns of alcohol use disorder symptoms.
Method
Data are from a prospective longitudinal study examining a broad range of mental health and substance use problems. A gender-balanced sample of 808 participants was interviewed at ages 21, 24, 27, and 30. The sample was divided into subgroups corresponding to longitudinal patterns of alcohol use disorder derived from latent class growth analysis.
Results
Four patterns of alcohol use disorder symptoms were identified: A “low disorder symptom” group, a “decreaser” group, an “increaser” group, and a “chronic disorder symptom” group. Rates of depression were significantly higher for females only among those with a pattern of chronic or decreasing alcohol disorder symptoms.
Conclusions
Elevated rates of depression among females in young adulthood may depend on patterns of co-occurring alcohol disorder symptoms. Practitioners should pay particular attention to signs of chronic alcohol use disorders and associated risks for depression among young adult women.
1. Introduction
In the United States, 16.2% of adults age 18 years or older were estimated to be diagnosed with lifetime major depressive disorder [1]. Depression imposes a considerable toll at both personal and societal levels. In an international study, depression was classified among the leading causes of disease burden and was projected to be the single leading cause by 2020 [2], indicating that depression is a major clinical and public health concern.
Depression has been found to co-occur with problem drinking in clinical as well as community samples [3-5]. Using a nationally representative sample of the US adult population, Hasin and Grant [6] reported that the odds of depression among those who reported alcohol dependence in the past 12 months was over 4 times greater than among those who reported no alcohol dependence. Other studies suggest that the link between alcohol use and depression may vary by the level or severity of alcohol consumption. Rodgers et al. [7] reported that depression scores were higher among non-drinkers and heavy drinkers, compared to lower level drinkers. Skogen [8] found that moderate drinking did not significantly elevate the risk of clinical depression, whereas heavy drinking (above the 95th percentile) did significantly increase this risk (odds ratio = 1.43).
An important clinical consideration, which has not been widely investigated in extant depression literature, is the likelihood that most people will experience changes in level of alcohol involvement over their life course. Studies have especially documented longitudinal changes in alcohol use during young adult development. On average, alcohol use tends to increase during young adulthood [9], especially from ages 18 to 25 [10]. However, around this average there is great heterogeneity in drinking patterns from adolescence throughout young adulthood [11-14]. For example, many young people experience problem drinking early on but then appear to “mature out” of this behavior [15]. Yet, there remains a substantial number of young adults who will experience persistent [16-18] or escalating [19] alcohol use problems throughout adulthood. Many others will abstain from alcohol use or drink moderately without associated problems. Few studies examining depression have accounted for such heterogeneity in longitudinal changes in alcohol involvement exhibited by young adults.
A large body of research examining depression has revealed gender differences. Women are at increased risk for having a lifetime occurrence of major depression [20], being diagnosed with major depression in the preceding 12 months [1], and experiencing chronic major depression disorder [21] compared to men. A few studies have provided empirical evidence suggesting different levels of alcohol involvement are a potential explanation for gender differences in depression. Rodgers et al. [7] reported estimated marginal means of depression scores for men and women by 5 different levels of alcohol consumption, including nondrinkers, occasional drinkers, lower level, higher level, and hazardous/harmful level. In this study, women who were classified as being at the hazardous/harmful level were reported to have the highest depression scores. Along this line, gender differences in depression, with women reporting higher depression scores, were most prominent at the hazardous/harmful alcohol consumption level, although a statistical test for this gender difference was not provided [7].
Using cross-sectional data, Goldstein and Levitt [22] also classified their sample into 3 alcohol consumption subgroups: a minimal consumption group, a moderate consumption group, and a heavy consumption group. Next, they examined the relation of these alcohol subgroups to the lifetime prevalence of depression for women and men. Gender differences in depression were most evident in the heavy consumption group, where the prevalence of major depression diagnosis was 44% for women and 16.1% for men. In the moderate consumption group, the prevalence was 30.3% and 18.8%, respectively, whereas in the minimal consumption group, the prevalence was 24.6% and 22.8%, respectively. Along this line, Goldstein and Levitt concluded that the drinking group variable was significantly related to lifetime prevalence of depression only among women. These prior investigations suggest a possible role of different levels of alcohol problems in gender differences in depression. However, these studies did not directly address the question of whether longitudinal change in alcohol involvement, common among young adults, can help explain elevated depression rates among females.
Given substantial heterogeneity in alcohol use patterns across young adulthood and variation in gender differences in depression by level of alcohol problems, the current study seeks to examine the degree to which young adult alcohol use patterns may account for gender differences in depression. Two main research questions are addressed:
Is the number of depressive episodes associated with longitudinal patterns of alcohol use disorder symptoms in young adulthood? We expect significant differences in depressive episodes across alcohol use patterns in line with prior studies reporting substantially higher rates of depression among heavy drinkers [6].
To what extent do patterns of alcohol use in young adulthood account for gender differences in depression? We hypothesize greater gender differences in depression among those with patterns including more alcohol disorder symptoms, in line with prior studies of gender and co-occurrence of depression and heavy alcohol use. However, we are aware of no prior studies examining the interaction between gender, depression, and longitudinal alcohol use patterns in young adulthood.
2. Methods
2.1. Sample
Data are from the Seattle Social Development Project (SSDP), a longitudinal study examining a broad range of behavior, health, and mental health outcomes. In September 1985, 18 Seattle elementary schools were identified that overrepresented students from high-crime neighborhoods. The study population included all fifth-grade students in these schools (N = 1053). From this population, 808 students (77%) consented to participate in the longitudinal study and constitute the SSDP sample. Analyses presented here focus on adult data collected at ages 21, 24, 27, and 30. Prior to age 18, parents of study participants provided consent (and the SSDP child provided assent) that was informed, voluntary, and written. At each assessment since age 18, the SSDP participant him/herself provided informed, voluntary, and written consent to participate. All data collection procedures have been approved by the University of Washington Institutional Review Board.
Fifty-one percent of the sample is male. The sample includes European Americans (47%), African Americans (26%), Asian Americans (22%), and Native American (5%). Sample retention rates have been consistently high; out of those still living (18 participants were deceased by age 30), 91% (n = 719) of respondents participated in interviews at age 30.
2.2. Measures
2.2.1. Major depressive episodes (ages 21 through 30)
Measures of past-year major depressive episode were assessed using the Diagnostic Interview Schedule (DIS) [23] at ages 21, 24, 27, and 30. The DIS has been demonstrated to be valid and reliable in studies of psychiatric disorders among adults [24-27]. Those meeting the diagnostic threshold in the past year prior to each interview were assigned a 1 at each age, and 0 otherwise. These dichotomized measures were summed into a single measure reflecting the number of interview times the participant had met past-year DSM-IV diagnostic threshold at ages 21, 24, 27, and 30 (potentially ranging from 0 to 4 times) to tap into the persistence of depression across the study points. Of note, measures of manic episodes were not available at all study waves precluding the screening out of those with bipolar disorder.
2.2.2. Alcohol use disorder symptoms (ages 21 through 30)
Also assessed using the DIS, measures of alcohol use disorder symptoms were computed at ages 21, 24, 27, and 30 by combining the number of DSM-IV [28] alcohol abuse and dependence criteria met at each age in the past 12 months. Consistent with other recent studies [29-31], our alcohol use disorder measure assessed symptoms rather than the presence or absence of a disorder diagnosis, thus including sub-threshold alcohol use problems that many young adults experience. Reliabilities of these alcohol use measures (Cronbach’s α) at ages 21, 24, 27, and 30 were .75, .77, .84, and .83, respectively. Although 11 symptoms were possible (4 for abuse; 7 for dependence), the measures were recoded to 0, 1, 2, 3, 4, or 5 or above since few participants exceeded this range.
2.3. Analysis
To explore the possibility that young adults in this sample followed different trajectories of alcohol use disorder symptoms, a series of latent class growth analyses (LCGA) were estimated using Mplus 5.21. LCGA, a mixture modeling approach for longitudinal data, assumes that a population includes distinct subgroups or classes of trajectories that can be identified using iterative procedures [32, 33]. The number of trajectory classes was chosen by consideration of model fit statistics, sufficient class sizes, and the theoretical meaningfulness of the solution. To address concerns about potential local optima [34], the number of random starts was increased to 2000 and the second stage of optimization increased to 50. Missingness in the data was handled with full-information maximum likelihood estimation in Mplus [35-37]. Readers interested in more details about mixture model building strategies, including fit statistics and estimation processes, are referred to prior studies [for example, 32, 33, 34, 38-41].
After selecting the optimal model representing trajectories of alcohol use disorder symptoms in young adulthood, we examined whether the mean number of depressive episodes varies across patterns of alcohol use disorder symptoms using regression and a post hoc test for a linear combination of regression parameters in STATA 10. Gender differences in depression within each subgroup of alcohol use disorder symptoms were also examined using regression and a post hoc test.
3. Results
3.1. Trajectories of alcohol use disorder symptoms
To identify patterns of alcohol use disorder in young adulthood, we first examined single-group growth curve models to determine the overall shape of the full-sample trajectory (e.g. intercept only; intercept and a linear slope; intercept, a linear slope, and a quadratic term; and a latent basis model) as recommended by Ram and Grimm [39]. Single-group growth curve results supported the intercept and a linear slope model for the latent class growth analysis models. Accordingly, a series of latent class growth analysis models with an intercept and a linear slope were estimated, ranging from 2 to 6 classes. BIC, SABIC, the Lo-Mendell-Rubin Adjusted Likelihood Ratio Test, and the Bootstrapped Likelihood Ratio Test each indicated that the model fit improved through the 4-class solution, but not always through the 5-class solution (see Table 1). Entropy was .73, which is between a medium (.60) and a high (.80) entropy value [42]. The 4-class solution also provided conceptually meaningful and distinct subgroups. Thus, the 4-class solution was accepted as providing the most optimal model fit to the data and parsimonious conceptual interpretation.
Table 1.
Fit indices for latent class growth models, with the selected 4-class model indicated by shading.
| No. of classes |
BICa | SABIC | Log Likelihood |
Entropy | Average class probabilities | Adjusted LMRT b, c |
BLRT b,d |
|---|---|---|---|---|---|---|---|
| C1 | 7198.8 | 7182.9 | -3582.7 | -- | -- | -- | -- |
| C2 | 7270.0 | 7254.1 | -3618.3 | .87 | .96, .97 | --f | -- f |
| C3 | 7121.5 | 7096.1 | -3534.1 | .75 | .81, .94, .90 | < .001 | < .001 |
| C4 | 7076.4 | 7041.5 | -3501.5 | .73 | .92, .89, .73, .77 | < .001 | < .001 |
| C5 | 7082.8 | 7038.3 | -3494.7 | .71 | .82, .67, .90, .85, .60 | 0.1336 | < .001 |
| C6 | 7091.6 | 7037.7 | -3489.1 | .63 | .70, .90, .76, .73, .61, .59 | 0.2217 | E e |
Note:
Decrease greater than 6 indicates “strong” improvement in fit [52]
P-value, a lower p-value indicates that the k-class model is preferable over the k-1 class model.
Lo-Mendell-Rubin Adjusted likelihood Ratio Test
Parametric Bootstrapped Likelihood Ratio Test
Not all the bootstrap draws converged.
These two tests were not applicable, since within-class variances were specified differently across these two models.
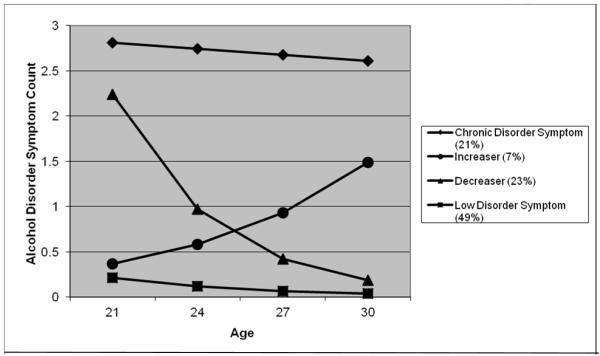
Figure 1 shows the 4 alcohol disorder trajectory groups. Two groups had multiple alcohol disorder symptoms at age 21, but one, a “chronic disorder symptom” group (21%), persisted with multiple symptoms through age 30, while the other, a “decreaser” group (23%), declined in symptoms through age 30. Two other groups had almost no symptoms of alcohol use disorders at age 21. A large “low disorder symptom” group (49%) reported few symptoms of alcohol use disorder consistently from age 21 to 30, while a relatively small “increaser” group (7%) reported a growth in symptoms from age 21 to 30. Males and females were distributed differently within each trajectory group: 75% of the chronic symptom group was male. Conversely, about 38% of the low disorder group was male. About 55% of the decreaser group was male and about the same percentage of the increaser group was male.
Figure 1.
Alcohol use disorder symptoms trajectories
3.2. Patterns of alcohol use disorder symptoms and depression
We first tested for whether the mean of depressive episodes varies by the patterns of alcohol use disorder by creating dummy variables to represent the alcohol subgroups (with the low alcohol disorder symptom group as the referent), and then regressing the depression measure on these dummy variables.
The average rate of depressive episodes for the full sample was .55 (SD=.88) from age 21 to 30. The chronic and decreasing alcohol disorder group averaged nearly double the rate of depressive episodes (.78 and .70, respectively), compared with the low disorder group (.39). The increaser group averaged .42. Post hoc tests showed that the low disorder symptom group had fewer depressive episodes on average than the chronic disorder symptom group (F = 24.15, p-value < .05) and the decreaser group (F = 15.87, p-value < .05). However, there was no group difference found in depression between the low disorder symptom group and the increaser group. The chronic disorder symptom group reported more depressive episodes on average than the increaser group (F = 7.41, p-value < .05). However, the chronic disorder symptom group did not differ from the decreaser group in depression. The increaser group showed a lower depression rate than the decreaser group (F = 4.55, p < .05). In sum, these analyses indicated that the mean of depressive episodes varied by the longitudinal patterns of alcohol use disorder symptoms in young adulthood.
3.3. Patterns of alcohol use and gender difference in depression
We first examined generally whether gender differences exist in the association between depression and alcohol problems by regressing a dichotomous adult depression measure (any major depressive episode from age 21 to 30 = 1, else = 0) on the average number of alcohol use disorder symptoms from age 21 to 30, gender, and their interaction. These analyses found a stronger overall association between depression and alcohol problems for females than males (β for the interaction term = .43, p <.05). Further analyses examined gender differences over time in the comorbidity of depression and alcohol problems by regressing past-year major depressive episode on alcohol use disorder symptoms, gender, and their interaction at ages 21, 24, 27, and 30, respectively. A significant interaction effect (β for the interaction term = .28, p-value <.05) was found at age 27, indicating greater comorbidity for females than males. No interaction effects were found at the other ages. These preliminary analyses showed evidence for a stronger association between depression and alcohol problems for females than males, though not consistently over time.
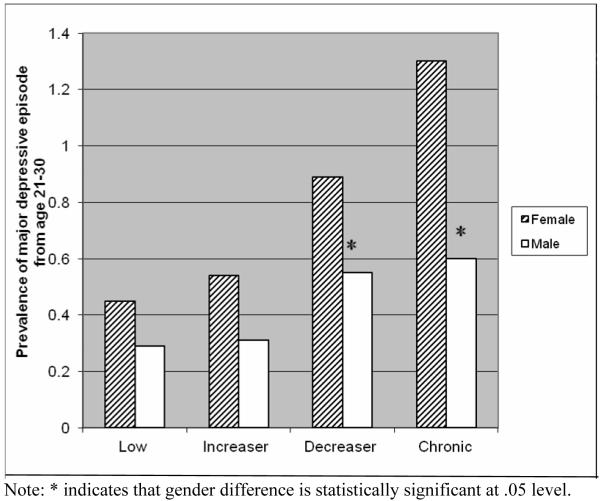
Next, gender differences in depression within each subgroup of alcohol use disorder symptoms were examined by regressing the depression measure on the dummy variables representing the alcohol subgroups, gender, and their interaction terms. Although women reported significantly more depressive episodes overall than did men from age 21 to 30 (.64 vs. .46, respectively, p < .05), within trajectory groups women were significantly higher in rates of depression only among those with a pattern of chronic or decreasing alcohol disorder symptoms (F = 23.74, p < .05 and F = 7.22, p < .05, respectively), as shown in Figure 2. No significant gender differences in depression were found in the low alcohol disorder group or the increasing group.
Figure 2.
Depressive episodes by alcohol use disorder symptoms subgroups and gender
Finally, we conducted a sensitivity analysis to examine if similar patterns of gender differences in depression across alcohol subgroups were evident when considering depression only at age 30. This analysis aimed to address the concern that the relationships found are mostly attributable to depression at age 21 co-occurring with higher rates of alcohol disorder for women. The substantive findings remained unchanged.
4. Discussion
Diverse patterns of alcohol use disorder symptoms were found among this community sample of young adults, and depressive episodes were strongly associated with these patterns. These findings were largely in line with prior studies and our initial expectations that higher rates of depression would be associated with alcohol use patterns consistent with a greater number or more chronic disorder symptoms [7, 8]. Interestingly, those with a decreasing alcohol use pattern were similar to those with more chronic disorder symptoms in their depression, whereas those with an increasing alcohol use pattern were similar to the low disorder group in their depression.
Also consistent with prior research, women consistently reported more depressive episodes overall than did men. However, the central finding of the present study was that anticipated gender differences in depression were only found among those reporting a pattern of decreasing or, especially, chronic alcohol use disorder symptoms, but not in the low disorder and increasing groups. These findings suggest that patterns of alcohol use in young adulthood may be an important moderator of gender differences in depression. Problem drinking patterns which are elevated in the early 20s, characteristic of the chronic and decreasing groups, may be more detrimental for young women’s depression than for young men’s depression.
Why might these patterns of alcohol use disorder in particular exacerbate gender differences in depression? Studies examining the reasons people drink in their early 20s, that have noted differences between young men and women, may help inform these findings. Males at the beginning of young adulthood are more likely to report using alcohol to “get high” or for social reasons, compared to their female counterparts [43]. In another study, drinking to “feel high” was found to be related to alcohol-related problems among college males but not among college females [44]. In contrast, among college females, Marczinski [45] found that drinking behavior was more strongly related to cognitive or emotional reasons such as feeling anxious, nervous, or lonely. Capraro [46] concluded that alcohol use among males transitioning to young adulthood may reflect socialized beliefs about the role of alcohol in the lives of young men, whereas young women’s alcohol use may be more closely related to proximal emotions. Together, these studies suggest that elevated alcohol use in the early 20s may be differentially associated with depression for young men and women.
As noted, although the depression rate was higher among women than men in the increaser group, no significant gender difference was found among young adults in this group; that is, among those with fewer alcohol disorder symptoms in the early 20s but elevated symptoms later in the study period. One possible explanation for this is that the triggers for problem drinking become more similar for males and females in their late 20s and early 30s. Lemke [47] reported that adult men and women reported similar drinking reactivity to stressors, and another study found that males and females in their 30s experienced similar levels of stressful life events overall [48].
Limitations of the study should be noted. First, measures were based on participants’ self-reports, potentially raising concerns about response bias for alcohol use [49] and/or depression [50]. Second, the classes we have identified may be specific to our sample, potentially limiting the generalizability of the present findings. Finally, the increaser group had relatively few participants, potentially limiting power to detect gender differences within this trajectory group relative to other groups. However, the magnitude of the gender difference in depression in the increaser group was less than that in the decreaser or the chronic group.
This study also has important strengths. It used prospective data across 4 time points from ages 21 through 30 that included diagnostic assessments of major depressive episodes and alcohol use disorder symptoms in young adulthood. Dynamic changes in diagnostic criteria for alcohol use disorder were modeled across these time points, allowing for identification of unique subgroup trajectories of problem alcohol use. The gender-balanced sample provided opportunities to explore important differences between young adult men and women. We are aware of no other studies using prospective, longitudinal, diagnostic data and these dynamic modeling methods to examine the interrelationships of depression, symptoms of alcohol use disorders, and gender.
The present findings suggest that specific interventions targeting young women’s early problem drinking may be particularly indicated for prevention efforts addressing young adult depression. It should be noted that women with alcohol problems receive less services for these problems compared to men. For instance, Roeloffs [51] reported that of patients being involved in hazardous drinking, 25.5% of male patients and 4.5% of female patients received counseling about alcohol use. This disparity in services may partly reflect higher prevalence rates of problem drinking and alcohol use disorder symptoms among men. As a consequence, alcohol problems may be more readily recognized in men by clinical practitioners. The present study stresses the need for clinicians and other practitioners to pay particular attention to earlier signs of problem drinking among young women and associated risks of comorbid depression, as well as the need to develop appropriate preventive protocols that recognize unique risks for women and men.
Acknowledgments
Funding for this study was provided by the National Institute on Drug Abuse (NIDA; grant numbers R01DA021426-(10-11), R01DA009679-(01-13), and R01DA024411-01), the National Institute on Alcohol Abuse and Alcoholism (NIAAA; R01AA016960-01), and by grant 21548 from the Robert Wood Johnson Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
An earlier version of this paper was presented in May 2009 at the annual meeting of the Society for Prevention Research in Washington, DC.
References
- [1].Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder - Results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- [2].Murray C, Lopez A. The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Harvard School of Public Health; Cambridge, MA: 1996. [Google Scholar]
- [3].Conner KR, Pinquart M, Gamble SA. Meta-analysis of depression and substance use among individuals with alcohol use disorders. J Subst Abuse Treat. 2009;37:127–37. doi: 10.1016/j.jsat.2008.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States - Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:830–42. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- [5].Graham K, Massak A, Demers A, Rehm J. Does the association between alcohol consumption and depression depend on how they are measured? Alcoholism: Clin Exp Res. 2007;31:78–88. doi: 10.1111/j.1530-0277.2006.00274.x. [DOI] [PubMed] [Google Scholar]
- [6].Hasin DS, Grant BF. Major depression in 6050 former drinkers: Association with past alcohol dependence. Arch Gen Psychiatry. 2002;59:794–800. doi: 10.1001/archpsyc.59.9.794. [DOI] [PubMed] [Google Scholar]
- [7].Rodgers B, Korten AE, Jorm AF, et al. Non-linear relationships in associations of depression and anxiety with alcohol use. Psychol Med. 2000;30:421–32. doi: 10.1017/s0033291799001865. [DOI] [PubMed] [Google Scholar]
- [8].Skogen JC, Harvey SB, Henderson M, Stordal E, Mykletun A. Anxiety and depression among abstainers and low-level alcohol consumers. The Nord-Tr circle divide ndelag Health Study. Addiction. 2009;104:1519–29. doi: 10.1111/j.1360-0443.2009.02659.x. [DOI] [PubMed] [Google Scholar]
- [9].Schulenberg JE, O’Malley PM, Bachman JG, Wadsworth KN, Johnston LD. Getting drunk and growing up: Trajectories of frequent binge drinking during the transition to young adulthood. J Stud Alcohol. 1996;57:289–304. doi: 10.15288/jsa.1996.57.289. [DOI] [PubMed] [Google Scholar]
- [10].Substance Abuse and Mental Health Services Administration . Results from the 2005 National Survey on Drug Use and Health: National findings. Substance Abuse and Mental Health Services Administration, Office of Applied Studies; Rockville, MD: 2006. [Google Scholar]
- [11].Lee JO, Hill KG, Guttmannova K, et al. The effects of general and alcohol-specific peer factors in adolescence on trajectories of alcohol abuse disorder symptoms from 21 to 33 years. Drug Alcohol Depend. 2012;121:213–19. doi: 10.1016/j.drugalcdep.2011.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Jackson KM, Sher KJ. Similarities and differences of longitudinal phenotypes across alternate indices of alcohol involvement: a methodologic comparison of trajectory approaches. Psychol Addict Behav. 2005;19:339–51. doi: 10.1037/0893-164X.19.4.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Maggs JL, Schulenberg JE. Trajectories of alcohol use during the transition to adulthood Alcohol Res Health. 2004;28:195–201. [Google Scholar]
- [14].Chassin L, Pitts SC, Prost J. Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: Predictors and substance abuse outcomes. J Consult Clin Psychol. 2002;70:67–78. [PubMed] [Google Scholar]
- [15].Jessor R, Donovan JE, Costa FM. Beyond adolescence: Problem behavior and young adult development. Cambridge University Press; New York: 1991. [Google Scholar]
- [16].Arnett JJ. The developmental context of substance use in emerging adulthood. J Drug Issues. 2005;35:235–53. [Google Scholar]
- [17].Schulenberg JE, Maggs JL. A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. J Stud Alcohol. 2002;(Suppl. 14):54–70. doi: 10.15288/jsas.2002.s14.54. [DOI] [PubMed] [Google Scholar]
- [18].Jacob T, Koenig LB, Howell DN, Wood PK, Haber JR. Drinking trajectories from adolescence to the fifties among alcohol-dependent men. J Stud Alcohol Drugs. 2009;70:859–69. doi: 10.15288/jsad.2009.70.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Warner LA, White HR, Johnson V. Alcohol initiation experiences and family history of alcoholism as predictors of problem-drinking trajectories. J Stud Alcohol Drugs. 2007;68:56–65. doi: 10.15288/jsad.2007.68.56. [DOI] [PubMed] [Google Scholar]
- [20].Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder - Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- [21].Blanco C, Okuda M, Markowitz JC, et al. The epidemiology of chronic major depressive disorder and dysthymic disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2010;71:1645–56. doi: 10.4088/JCP.09m05663gry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Goldstein BI, Levitt AJ. Is current alcohol consumption associated with increased lifetime prevalence of major depression and suicidality? Results from a pilot community survey. Compr Psychiatry. 2006;47:330–33. doi: 10.1016/j.comppsych.2006.01.010. [DOI] [PubMed] [Google Scholar]
- [23].Robins L, Helzer JE, Croghan J, Williams JBW, Spitzer RL. NIMH Diagnostic Interview Schedule. Version III. National Institute of Mental Health; Rockville, MD: 1981. [Google Scholar]
- [24].Jaffee SR, Moffitt TE, Caspi A, et al. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Arch Gen Psychiatry. 2002;59:215–22. doi: 10.1001/archpsyc.59.3.215. [DOI] [PubMed] [Google Scholar]
- [25].Leaf PJ, Myers JK, McEvoy LT. Procedures used in the Epidemiological Catchment Area study. In: Robins LN, Reiger DA, editors. Psychiatric disorders in America. Free Press; New York: 1991. pp. 11–32. [Google Scholar]
- [26].Newman DL, Moffitt TE, Caspi A, et al. Psychiatric disorder in a birth cohort of young adults: Prevalence, comorbidity, clinical significance, and new case incidence from ages 11 to 21. J Consult Clin Psychol. 1996;64:552–62. [PubMed] [Google Scholar]
- [27].Reinherz HZ, Giaconia RM, Carmola Hauf AM, Wasserman MS, Paradis AD. General and specific childhood risk factors for depression and drug disorders by early adulthood. J Am Acad Child Adolesc Psychiatry. 2000;39:223–31. doi: 10.1097/00004583-200002000-00023. [DOI] [PubMed] [Google Scholar]
- [28].American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 4th ed American Psychiatric Association; Washington DC: 1994. [Google Scholar]
- [29].Hasin DS, Beseler CL. Dimensionality of lifetime alcohol abuse, dependence and binge drinking. Drug Alcohol Depend. 2009;101:53–61. doi: 10.1016/j.drugalcdep.2008.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Saha TD, Chou SP, Grant BF. Toward an alcohol use disorder continuum using item response theory: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2006;36:931–41. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- [31].Slade T, Grove R, Teesson M. A taxometric study of alcohol abuse and dependence in a general population sample: evidence of dimensional latent structure and implications for DSM-V. Addiction. 2009;104:742–51. doi: 10.1111/j.1360-0443.2009.02498.x. [DOI] [PubMed] [Google Scholar]
- [32].Muthen B, Muthen LK. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism: Clin Exp Res. 2000;24:882–91. [PubMed] [Google Scholar]
- [33].Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- [34].Hipp JR, Bauer DJ. Local solutions in the estimation of growth mixture models. Psychol Methods. 2006;11:36–53. doi: 10.1037/1082-989X.11.1.36. [DOI] [PubMed] [Google Scholar]
- [35].Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychol Methods. 2002;7:147–77. [PubMed] [Google Scholar]
- [36].Buhi ER, Goodson P, Neilands TB. Out of sight, not out of mind: strategies for handling missing data. Am J Health Behav. 2008;32:83–92. doi: 10.5555/ajhb.2008.32.1.83. [DOI] [PubMed] [Google Scholar]
- [37].Acock AC. Working with missing values. J Marriage Fam. 2005;67:1012–28. [Google Scholar]
- [38].Muthén B. Latent variable analysis: Growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of quantitative methodology for the social sciences. Sage; Newbury Park, CA: 2004. pp. 345–68. [Google Scholar]
- [39].Ram N, Grimm K. Growth mixture modeling: A method for identifying differences in longitudinal change among unobserved groups. Int J Behav Dev. 2009;33:565–76. doi: 10.1177/0165025409343765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Tofighi D, Enders CK. Identifying the correct number of classes in a growth mixture model. In: Hancock GR, editor. Mixture models in latent variable research. Information Age; Greenwich, CT: 2007. pp. 317–41. [Google Scholar]
- [41].Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equation Model. 2007;14:535–69. [Google Scholar]
- [42].Clark SL, Muthén B. [Accessed 2/18/2010];Relating latent class analysis results to variables not included in the analysis. Mplus. Available at: http://www.statmodel.com/download/relatinglca.pdf.
- [43].Wilson GS, Pritchard ME, Schaffer J. Athletic status and drinking behavior in college students: The influence of gender and coping styles. J Am Coll Health. 2004;52:269–73. doi: 10.3200/JACH.52.6.269-275. [DOI] [PubMed] [Google Scholar]
- [44].Harrell ZAT, Karim NM. Is gender relevant only for problem alcohol behaviors? An examination of correlates of alcohol use among college students. Addict Behav. 2008;33:359–65. doi: 10.1016/j.addbeh.2007.09.014. [DOI] [PubMed] [Google Scholar]
- [45].Marczinski CA, Bryant R, Fillmore MT. The relationship between cognitive preoccupation with alcohol and alcohol use in male and female college students. Addict Res Theory. 2005;13:383–94. [Google Scholar]
- [46].Capraro RL. Why college men drink: Alcohol, adventure, and the paradox of masculinity. J Am Coll Health. 2000;48:307–15. doi: 10.1080/07448480009596272. [DOI] [PubMed] [Google Scholar]
- [47].Lemke S, Schutte KK, Brennan PL, Moos RH. Gender differences in social influences and stressors linked to increased drinking. J Stud Alcohol Drugs. 2008;69:695–702. doi: 10.15288/jsad.2008.69.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Skaff MM, Finney JW, Moos RH. Gender differences in problem drinking and depression: Different “vulnerabilities?”. Am J Community Psychol. 1999;27:25–54. doi: 10.1023/A:1022813727823. [DOI] [PubMed] [Google Scholar]
- [49].Embree BG, Whitehead PC. Validity and reliability of self-reported drinking behavior - dealing with the problem of response bias. J Stud Alcohol. 1993;54:334–44. doi: 10.15288/jsa.1993.54.334. [DOI] [PubMed] [Google Scholar]
- [50].Hunt M, Auriemma J, Cashaw ACA. Self-report bias and underreporting of depression on the BDI-II. J Pers Assess. 2003;80:26–30. doi: 10.1207/S15327752JPA8001_10. [DOI] [PubMed] [Google Scholar]
- [51].Roeloffs CA, Fink A, Unutzer J, Tang LQ, Wells KB. Problematic substance use, depressive symptoms, and gender in primary care. Psychiatr Serv. 2001;52:1251–53. doi: 10.1176/appi.ps.52.9.1251. [DOI] [PubMed] [Google Scholar]
- [52].Raftery AE. Bayesian model selection in social research. Sociol Methodol. 1995;25:111–63. [Google Scholar]