Abstract
Sciatica is the most frequently encountered symptom in neurosurgical practice and is observed in 40% of adults at some point in their lives. It is described as pain of the hip and the lower extremity secondary to pathologies affecting the sciatic nerve within its intraspinal or extraspinal course. The most frequent cause is a herniating lumbar disc pressing on the neural roots. Extraspinal causes of sciatic pain are usually overlooked because they are extremely rare and due to intraspinal causes (lumbar spinal stenosis, facet joint osteoarthritis, fracture, and tumors of the spinal cord and spinal column) being the main consideration. Early diagnosis of sciatica significantly improves the likelihood of relieving symptoms, as well as avoiding any additional neurologic injury and unnecessary surgery. We evaluate histolopathologically confirmed extraspinal causes of sciatica cases, accompanied by their presented computed tomography and/or magnetic resonance imaging findings.
Anatomy
Being familiar with the anatomy of the lumbosacral plexus and sciatic nerve is essential for the evaluation of extraspinal sciatica. The lumbar plexus is composed of the ventral rami of L1–L4 and is anatomically located behind the psoas muscle. A minor branch of L4 combines with the ventral ramus of L5 to form the lumbosacral cord or trunk. The lumbosacral trunk descends over the sacral ala and combines with the ventral rami of S1, S2 and S3 (and a branch of S4) to form the sacral plexus [1].
The sacral plexus is a thick triangular network, with its apex formed by the sciatic nerve, located anteriorly to the sacroiliac joint and the piriformis muscle. Its upper fibres form the sciatic nerve at the level of the inferior piriformis muscle, which then leaves the pelvis via the greater sciatic foramen. At that level, the sciatic nerve is anteriorly next to the ischium, posteriorly next to the piriformis muscle and medially next to the inferior gluteal vessels.
Within the gluteal region, the sciatic nerve travels superficial to other lateral rotator muscles of the thigh and deep to the gluteus maximus muscle. In the inferior gluteal region, the nerve passes between the ischial tuberosity and greater trochanter, typically in closer proximity to the ischial tuberosity. It then travels between the biceps femoris and the adductor magnus to enter the posterior compartment of the thigh, where it divides to give rise to the common peroneal and tibial nerves. In most individuals this division takes place just above knee level (Figure 1) [2].
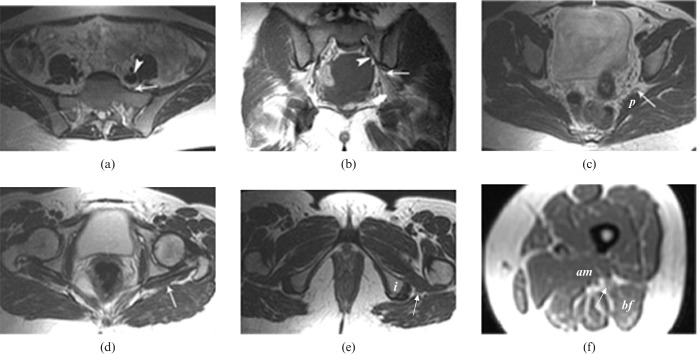
Figure 1.
Normal MRI appearance of the lumbosacral trunk, sacral plexus and sciatic nerve. Axial T1 weighted image (a) at the level of the sacral wings shows the lumbosacral trunk (arrow) anterior to the sacrum and posterior to the iliac vessels (arrowhead). Coronal T1 weighted image (b) shows the normal sacral plexus (arrowhead) passing anterior to the sacral wings and continuing inferolaterally to leave the pelvis through the greater sciatic foramen (thin arrow) as the sciatic nerve (thick arrow). Axial T2 weighted image (c) at the level of the greater sciatic foramen shows the sacral plexus (arrow) anterior to the piriformis (P) muscle and lateral to the inferior gluteal vessels. Axial T2 weighted image (d) at the level of the gluteal region shows the sciatic nerve (arrow) superficial to the lateral rotator muscles and deep to the gluteus maximus muscle. Axial T2 weighted image (e) at the level of the infragluteal region shows the sciatic nerve (arrow) between the ischial tuberosity (i) and the greater trochanter. Axial T1 weighted image (f) at the mid-femoral level shows the sciatic nerve (arrow) between the adductor magnus (am) and biceps femoris (bf) muscles.
Traumatic, infective, inflammatory, tumoral, vascular and other causes constitute the aetiology of extraspinal sciatica (Table 1).
Table 1. Causes of extraspinal sciatic neurapathy.
| Traumatic causes | Intramuscular injection, abdominal surgical procedures, fracture, haematoma |
| Infective causes | Abscess (e.g. psoas abscess, tubo-ovarian abscess and pelvic abscess) |
| Inflammatory causes | Sacroiliitis |
| Tumoral causes | |
| Primary tumours of the sciatic nerve | Schwannoma, neurofibromatosis, neurolymphomatosis and malignant neurofibrosarcoma |
| Tumours causing compression or invasion of the sciatic nerve | Intra-abdominal or intrapelvic benign or malignant masses, primary (benign or malign) or secondary tumours originating from neighbouring soft tissues and osseous structures along the course of the sciatic nerve and lymphoma |
| Tumours causing infiltration of the sciatic nerve | Endoneural metastasis and lymphoma |
| Vascular causes | Aneurysma, arteriovenous malformation and arteriovenous fistulae |
| Other causes | Endometriosis, leiomyoma, adenomyosis, retroverted uterus, endosalpingitis, haematocolpos, piriformis syndrome, pregnancy, radiotherapy, osteoarthritis |
Traumatic causes
Traumatic nerve injury findings may vary extensively from disruption of axonal conduction with preservation of anatomical continuity to complete loss of continuity of the nerve trunk. Post-traumatically, sciatic nerve injury may be caused by laceration, stretching or compression in the early period, or later on by heterotropic ossification encasing the nerve (Figure 2). MRI exactly demonstrates both the location and the severity of the injury. The T2 weighted MR images may demonstrate (depending on the severity of the injury) high signal intensity in the nerve fibres and/or increased nerve dimension, deformation of the nerve or total loss of nerve integrity (Figure 3) [3].
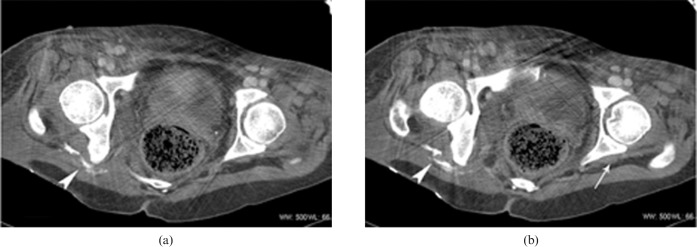
Figure 2.
Post-traumatic heterotropic ossification in a 35-year-old female patient with a history of trauma sustained 6 years previously, and complaining of persistent numbness and pain in the right lower limb. Axial CT images (a,b) show a gluteus-level heterotropic ossification (with a lucent central portion) surrounding the right sciatic nerve (arrowhead). The left sciatic nerve appears normal (arrow).
Figure 3.
Post-traumatic oedema in a 54-year-old female patient complaining of right foot numbness and pain radiating to the back of her right thigh following trauma. Coronal fat suppression T2 weighted image shows a right lumbosacral plexus oedema at the level of the greater sciatic foramen (arrows). The left lumbosacral plexus appears normal.
Intramuscular injection
Peripheral nerve injury related to intramuscular injection is caused either by injection close to the nerve or by accumulation of the injected drug within the spaces where the sciatic nerve travels and which are formed between the piriformis, gemellus, quadratus and obturator muscles (Figure 4). Other possible mechanisms are direct needle trauma, secondary compression by scar tissue and direct nerve fibre damage caused by neurotoxic chemicals in the injected drug [4].
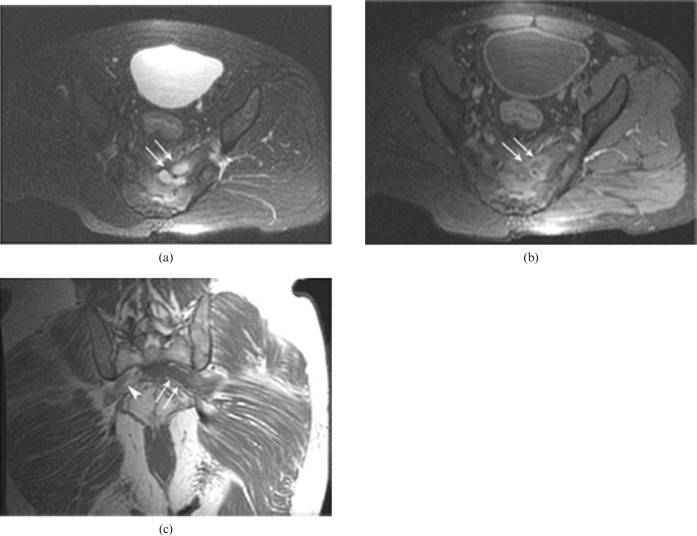
Figure 4.
Footdrop in a 45-year-old female patient with an intramuscular injection history 3 days previously; axial fat suppression T2 weighted images (a,b) reveal oedema in the course of the sciatic nerve (arrowheads) The right sciatic nerve appears normal (arrow).
Surgical interventions
These are the most common cause of extraspinal sciatica. Extraspinal sciatica is most commonly seen following hip joint surgery. The sciatic nerve may be injured during pelvic surgery as a result of poor positioning of the patient, surgical dissection or excessive pressure exerted by the surgeons.
Fracture
Quite often, sciatica develops following fracture of the sacrum and the sacroiliac joint because of the anatomical proximity of the lumbosacral plexus to these structures (Figure 5). In addition, the sciatic nerve may be injured in cases of fractures of the acetabulum and femur or femoral head dislocation.
Figure 5.

Sacral fracture in a 52-year-old male patient with a post-traumatic right footdrop. Axial CT image reveals a separation fracture affecting the neural foramina in the right half of the sacrum.
Haematoma
A gluteal region haematoma is usually related to trauma, hip operation, haemophilia or anticoagulation therapy. Haematoma can damage the nerve either directly (increased pressure on the nerve) or indirectly (ischaemia as a result of vasa vasorum compression). The MRI signal characteristics of the mass vary according to its contents of haemoglobin degradation products. Acute haematoma (1–4 days) has low signal intensity in all sequences and may be surrounded by oedema. A mass in its early (2–7 days) and late (1–3 weeks) subacute phases is hyperintense on the T1 weighted images owing to its methaemoglobin content. The signal intensity on the T2 weighted images is low during the early subacute period but high during the late subacute period. The wall of a chronic haematoma has a hypointense signal on both sequences owing to haemosiderin accumulation. A mass that has appeared following (usually) a trauma, stage-related signal changes and size reduction over time are pathognomonic for haematoma (Figure 6) [5].
Figure 6.
Intramuscular haematoma in a 51-year-old female patient with left-side sciatica, following a penetrating trauma. Axial T1 weighted (a) and T2 weighted (b) images show a large haematoma at the level of the greater sciatic foramen involving the left piriformis muscle, lumbosacral plexus and sciatic nerve (arrowheads). The right sciatic nerve appears normal (arrows).
Infection-related causes
Abscess
An abscess is a focal collection of pus and necrotic material walled off by a fibrovascular rim. Gluteal and pelvic region abscesses are seldom encountered. They are usually related to gastrointestinal and urinary tract infections and may affect the sacral plexus by spreading via normal anatomical routes. The psoas and iliac muscles, and the iliac vessels, are the potential routes along which abdominal infections spread into the pelvis. A gluteal abscess and presacral abscess also related to sacral osteomyelitis may directly affect the lumbosacral plexus and sciatic nerve, and thus cause sciatica. The abscess content has a low T1 weighted and high T2 weighted signal intensity. The peripheral fibrovascular rim signal, on the other hand, is hyperintense on the T1 weighted and hypointense on the T2 weighted images when compared with the signal of the abscess content. Inflammatory changes are present around the abscess, and peripheral contrast enhancement is typically observed following intravenous contrast administration (Figure 7) [5].
Figure 7.
Presacral abscess in a 55-year-old male patient with a left lumbosacral plexopath. A contrast-enhancing signal increase consistent with sacral osteomyelitis is observed on the fat suppression axial T1 weighted images following intravenous Gd administration (a) and on the axial fat suppression T2 weighted images (b). In addition, a presacral region cystic mass affecting the left lumbosacral plexus and consistent with an abscess is seen, demonstrating peripheral contrast attenuation (arrows). The right lumbosacral plexus appears normal (arrowhead) on the coronal T1 weighted images (c). The presacral abscess effect on the left lumbosacral plexus is clearly observable (arrows).
Inflammatory causes
Sacroiliitis
Sacroiliitis is a frequently encountered finding among seronegative spondyloarthropathies. Patients typically have an insidious-onset pain, which is relieved with physical activity and worsens during late night time. Sciatica may be the result of referred pain or the inflammatory changes in the immediate vicinity of the sacroiliac joint directly affecting the nerve [6]. Although the patient's symptoms have a guiding role, CT and MRI findings are pathognomonic. CT images of the sacroiliac joint demonstrate cortical erosion and subcortical sclerosis in the early course, and narrowing and ankylosis of the joint in the later course of the disease. On the other hand, by demonstrating the related acute inflammatory changes, MRI can provide information about the activity of the disease and for making an early diagnosis of sacroiliitis (Figure 8) [7].
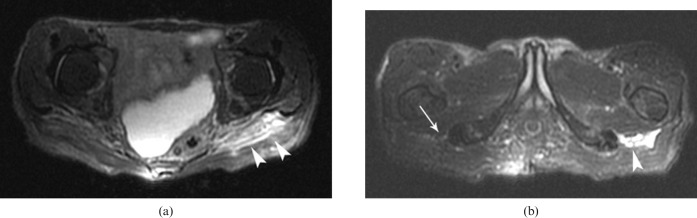
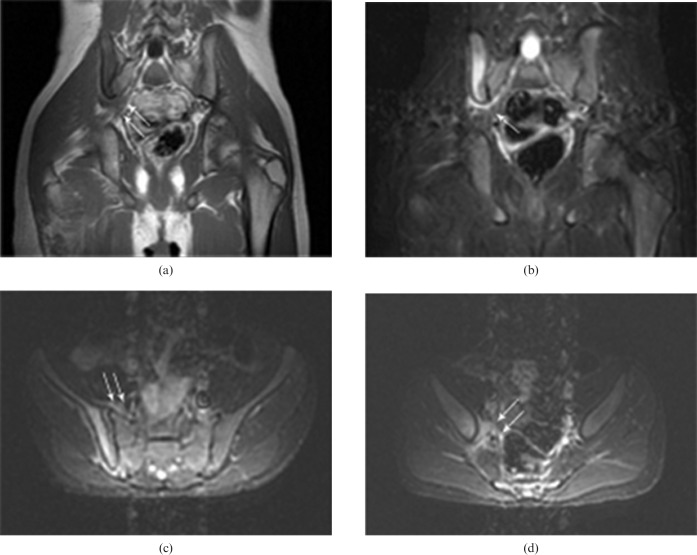
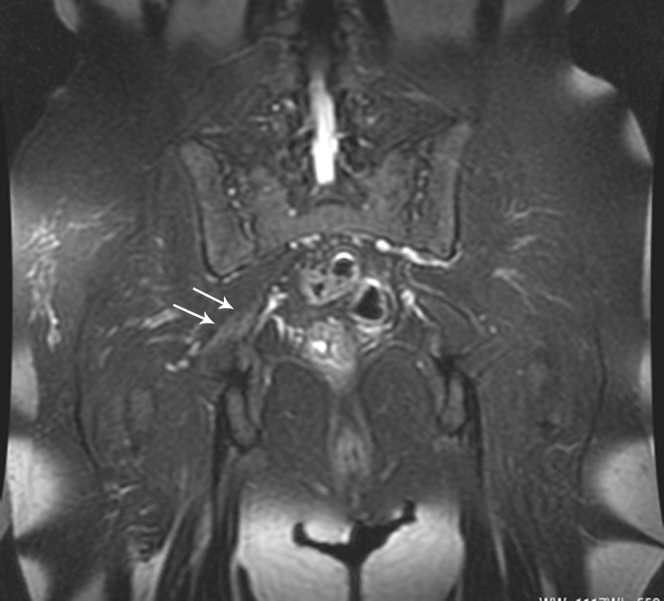
Figure 8.
Sacroiliitis in a 19-year-old male patient with right-side sciatica. Coronal T1 weighted (a) and T2 weighted fat suppression (b) and axial T2 weighted fat suppression (c,d) MR images reveal sacroiliitis of the right sacroiliac joint and neighbouring oedema pressing on the lumbosacral plexus (arrows).
Tumoral causes
Tumoral involvement of the sciatic nerve is quite rare and is usually observed with primary tumours of the nerve (schwannoma, neurofibromatosis, neurolymphomatosis and malignant neurofibrosarcoma) [8, 9].
Primary tumours of the sciatic nerve
Schwannoma is the most common primary tumour of the sciatic nerve. It originates from the Schwann cells forming the sheath of the nerve. It is mostly encountered in head and neck regions and originates from the eighth nerve. Pelvic region schwannomas are quite rare.
The imaging features of a schwannoma overlap those of a solitary neurofibroma (originating from nerve fibres), and often they are indistinguishable. The CT image attenuation of both neurofibromas and schwannomas is similar to that of muscle, and neurofibromas and schwannomas have various degrees of contrast enhancement following intravenous contrast administration. Both lesions are isohypointense on the T1 weighted and hyperintense on the T2 weighted MRI images when compared with muscle, and a central area of low-intensity signal may be observed (more frequently with neurofibromas), called the target sign (Figure 9).
Figure 9.
Schwannoma in a 37-year-old female patient complaining of right radicular leg pain. Coronal T1 weighted (a), axial T2 weighted images (b) and fat suppression T1 weighted images (c) following intravenous contrast administration reveals a smooth-contoured solid mass with significant contrast enhancement in the right sciatic nerve (arrowheads). The left sciatic nerve appears normal (arrow).
Despite two-thirds of neurofibroma cases being encountered sporadically, the remaining one-third of cases are associated with neurofibromatosis type 1. These tumours are characteristically multiple and plexiform in appearance, with diffuse involvement of the lumbosacral plexus in patients with neurofibromatosis.
Malignant peripheral nerve sheath tumours occur most often in patients with neurofibromatosis type 1, especially after radiation therapy [10]. The imaging features of malignant neural tumours overlap those of their benign counterparts, making differentiation between the two challenging. Findings that favour a malignant neural tumour include large size, irregular margins and heterogeneity. Clinically, the finding of a progressively enlarging mass in a patient suggests a malignant nerve sheath tumour.
Tumours causing compression or invasion of the sciatic nerve
Intra-abdominal or intrapelvic benign or malignant masses, primary (benign or malign) or secondary tumours originating from neighbouring soft tissues and osseous structures along the course of the sciatic nerve, or lymphomas may affect the sciatic nerve and cause sciatic pain.
Intra-abdominal and intrapelvic benign and malignant tumours
The lumbosacral plexus may be affected as a result of compression or invasion by intra-abdominal or intrapelvic masses, with colorectal carcinoma (Figure 10) and endometriosis being the most frequently encountered malignant and benign causes, respectively. In addition, the sciatic nerve may be locally invaded by uterine, prostatic and ovarian tumours, or compressed by uterine leiomyoma, adenomyosis or a retroverted uterus.
Figure 10.

Colorectal carcinoma in a 64-year-old female patient with lumbosacral plexopathy. Axial CT image demonstrating a rectal carcinoma invading the left half of sacrum, the left S3 neural root and the left piriformis muscle.
Malignant soft-tissue tumours
Metastasis to muscle
Despite constituting about 50% of body mass and having a significant blood supply, metastatic tumour involvement of skeletal muscle is quite rare. The frequency of this metastasis is reported to be 0.8–16% in autopsy studies. Lung carcinomas are usually the primary source of metastasis, and the most frequently affected muscles are the diaphragm, rectus abdominis, deltoid, psoas and the intercostal muscles. Rarely, metastatic involvement of muscles neighbouring the sciatic nerve may also be observed (Figure 11) [11].
Figure 11.
Intramuscular metastasis in a 52-year-old male patient with a history of advanced stage gastric carcinoma complaining of waist pain, bilateral thigh pain (more severe on the left thigh), radiating to both legs, numbness and left leg cramps. (a) Pelvic CT image showing a solid left gluteal mass containing diffuse necrosis and calcification and peripheral contrast attenuation. (b) Axial fat suppression contrast-enhanced T1 weighted MR image demonstrating a well-demarcated solid mass in the left gluteal and right piriformis muscles with significant contrast enhancement. In addition, the sciatic nerves fibres are seen to be surrounded by tumour masses and appear thickened with no contrast enhancement (arrows).
Intramuscular metastasis is seen as a low-attenuation mass in contrast CT images, often demonstrating peripheral contrast attenuation. On the other hand, intramuscular metastatic lesions are isohypointense on the T1 weighted and hyperintense on the T2 weighted MRI images when compared with surrounding muscle tissues. The mass causes expansion of the involved muscle, and accompanying peritumoral oedema may be noticeable. In addition, haemorrhage, necrosis and calcification within the mass may be observable [12].
Soft-tissue sarcomas
Similar to intramuscular metastases, soft-tissue sarcomas are seen as isohypointense T1 weighted and hyperintense T2 weighted MRI lesions (Figure 12). However, necrosis, peritumoral oedema and lobulation are less frequently encountered in soft-tissue sarcomas than in metastatic lesions [13]. Histopathological examination is mandatory for a definitive diagnosis.
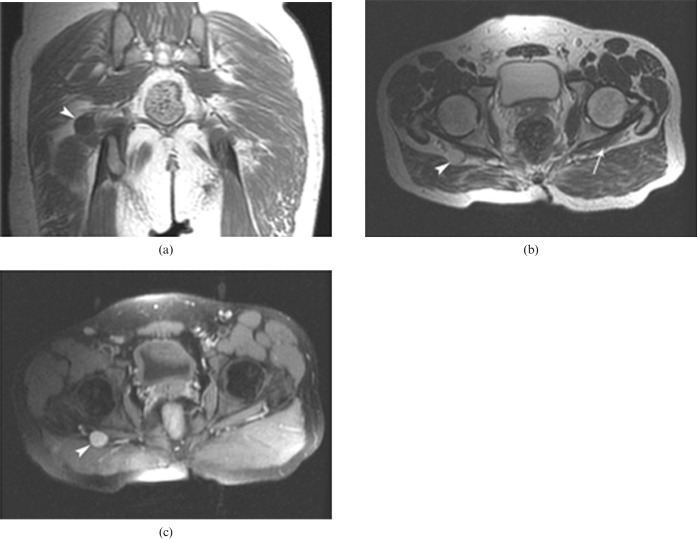
Figure 12.
Soft-tissue sarcoma in a 39-year-old female patient with left-side sciatica. Axial T1 weighted (a), T2 weighted (b) and T1 weighted images following intravenous contrast administration (c) demonstrating a soft-tissue mass with significant contrast enhancement in the posterior femoral compartment; the close relation of the mass to the sciatic nerve is seen (arrowheads). The right sciatic nerve appears normal (arrows).
Malignant tumours originating from bones
The pain of these tumours is similar to that caused by malignant soft-tissue tumours in having an insidious onset, being persistent, progressive, worsening at night and not being relieved by changing position. The characteristics of the pain are usually of utmost importance in the diagnosis of tumour-related sciatica. Most of the osseous tumours causing sciatica are located in the pelvis and proximal femur [14]. In addition to clearly visualising the lesion, CT and MRI also show in detail its relation to the sciatic nerve (Figure 13).
Figure 13.
Malignant osseous tumour in a 57-year-old male patient complaining of persistent left leg pain and numbness in the left foot. Axial T2 weighted (a), fat suppression contrast-enhanced T1 weighted (b) and fat suppression T2 weighted (c) MR images demonstrate a solid mass causing left acetabular destruction and have a soft-tissue component surrounding the infragluteal portion of the sciatic nerve (arrows). The right sciatic nerve appears normal (arrowhead).
Benign tumours of bones and soft tissues
Many benign tumours occur along the course of the lumbosacral plexus and involve or impinge on its various components. Lipoma (Figure 14), osteochondroma (Figure 15) and ganglion cyst (Figure 16) are the most common benign tumours causing sciatica. But a wide range of other benign tumours has been reported in the literature. Although the appearance of many benign processes is non-specific, some offer imaging characteristics that suggest the exact diagnosis.
Figure 14.

Intramuscular lipoma in a 64-year-old male patient complaining of left foot numbness. Axial CT image shows a lipoma within the left external obturator muscle pressing on the left sciatic nerve (arrow). The right sciatic nerve appears normal (arrowhead).
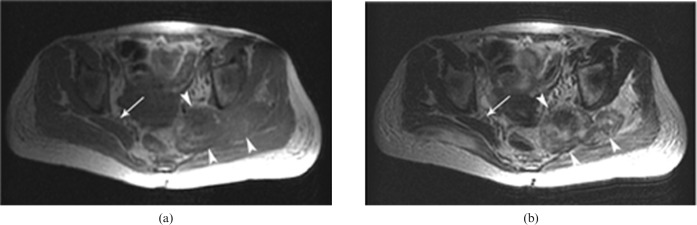
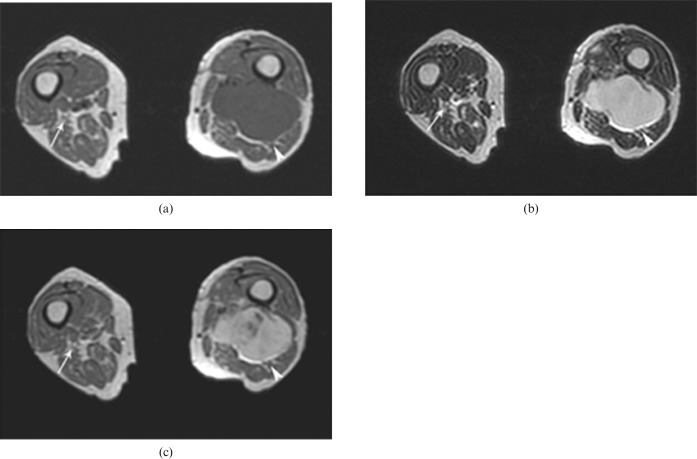
Figure 15.
Osteochondroma in a 35-year-old female patient complaining of right foot numbness. Axial T1 weighted images (a,b) showing a pedunculated osteochondroma located in the posterior portion of the femur and pressing on the sciatic nerve (arrowheads). The left sciatic nerve appears normal (arrows).
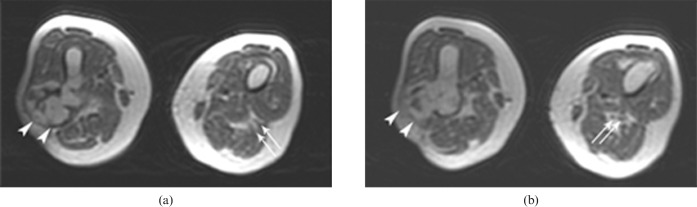
Figure 16.
Ganglion cyst in a 51-year-old female patient with left-side sciatica; Axial T2 weighted (a) and fat-suppression T2 weighted (b) MR images demonstrating a round hyperintense mass along the course of the sciatic nerve at the posterior femoral compartment (arrow).
Lymphoma
There are three ways in which lymphomas may affect the sciatic nerve. The most frequent cause of lymphoma-related sciatica is compression of the nerve by the enlarged lymph nodes (Figure 17). Secondly, extranodal involvement of soft tissues such as muscle (e.g. piriformis and gluteus muscles) may affect the sciatic nerve. In such cases, asymmetrical muscle expansion, heterogeneous or low focal density on the CT images, or focal or diffuse low T1 weighted signal intensity or high T2 weighted signal intensity on the MRI images are radiologically observed. A uniform or ring-form contrast attenuation may be seen or the lesion may not attenuate contrast at all. And lastly, although very rare, direct lymphoma invasion of the sciatic nerve has also been reported [15].
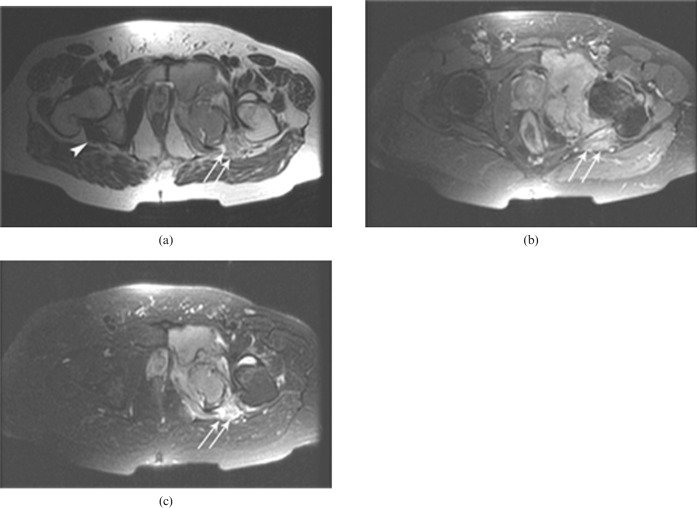
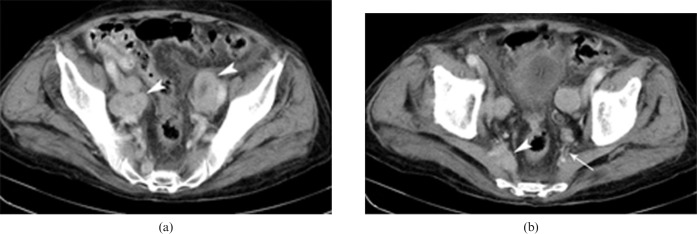
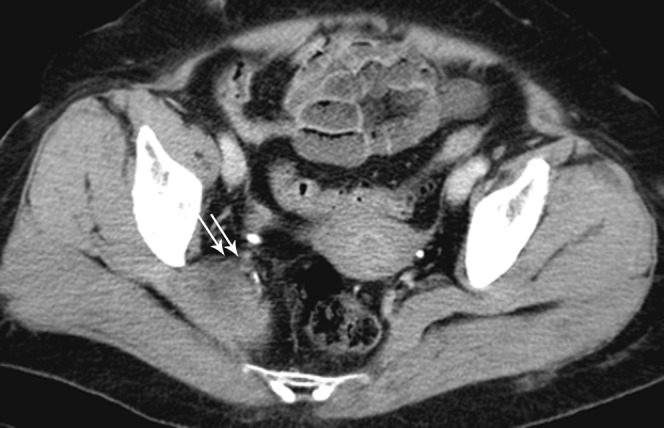
Figure 17.
Lymphoma in a 35-year-old female patient with right buttock pain and normal lumbar MRI. Axial CT images (a) reveal multiple bilateral parailiac lymphadenopathies (arrowheads). At the level of the lower sacrum, CT (b) reveals enlarged lymph nodes pressing on the sciatic nerve in the vicinity of the right piriformis muscle (arrowhead). The left lumbosacral plexus appears normal (arrow).
Tumours causing infiltration of the sciatic nerve
Endoneural metastasis of tumour cells into the sciatic nerve or its primary lymphomatous involvement may cause sciatic pain.
Vascular causes
The lumbosacral trunk is anterior to the sacrum and posterior to the iliac vessels, and any aneurysmal or pseudoaneurysmal expansion of the iliac artery (especially the internal iliac artery) and its branches may affect the sciatic nerve (Figure 18). The basic mechanism of aneurysm-related sciatica is compression to the nerve. Although nerves are fairly resistant to ischaemia and the lumbosacral plexus is rich in vascular supply, ischaemia may play an additional role (secondary to vasa vasorum compression) in the formation of aneurysm-related sciatic pain [16]. In addition, although quite rarey, direct pressure on the sciatic nerve by an arteriovenous malformation or arteriovenous fistula may also cause sciatica (Figure 19).
Figure 18.
A right internal iliac artery aneurysm in a 43-year-old male patient with lower back pain radiating to the right leg. Axial CT image demonstrating a partially thrombosed aneurysmal dilation of the right iliac artery pressing on the right lumbosacral plexus (arrow).
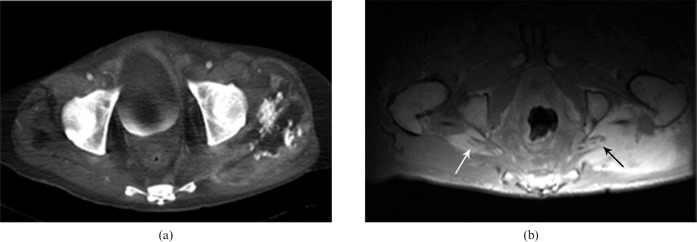
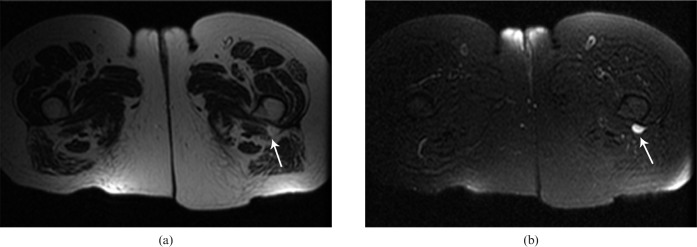
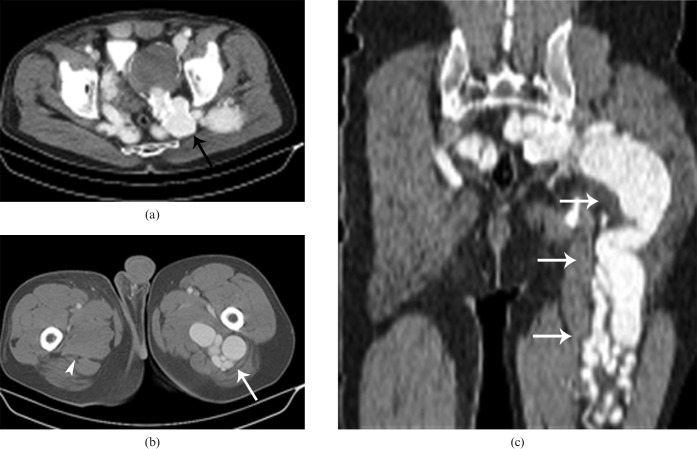
Figure 19.
Arteriovenous fistula in a 49-year-old male patient with left sciatica and a history of penetrating trauma 2 years previously. Axial (a,b) and coronal reformatted (c) CT images demonstrating a thrombosed aneurysm (black arrow) and diffuse varicose veins (white arrows) related to the arteriovenous fistula pressing on the left lumbosacral plexus and sciatic nerve. The right sciatic nerve appears normal (arrowhead).
Other causes
Endometriosis
Endometriosis may compress the sciatic nerve within the pelvis, sciatic notch or gluteal region distal to the notch, the compression being most frequent at the level of the sciatic notch and on the right [17]. Sciatic pain typically starts a few days before menstruation, intensifies progressively and shows some relief a week after menstruation is over. The focal mass is classically seen as high signal intensity on both T2 and T1 weighted images, suggesting acute haemorrhage; however, signal intensities can vary depending on the nature of the haemoglobin breakdown products.
Piriformis syndrome
Piriformis syndrome is sciatic nerve entrapment at the greater sciatic notch caused by an abnormal condition of the piriformis muscle (e.g. traumatic injury (most often), hypertrophy, inflammation, anatomic variations). It accounts for about 6% of sciatica cases. Typically, enlargement of the piriformis muscle is observed on the CT and MR images [18]. In addition, anterior displacement of the sciatic nerve or high T2 weighted signal intensity may be observed (Figure 20).
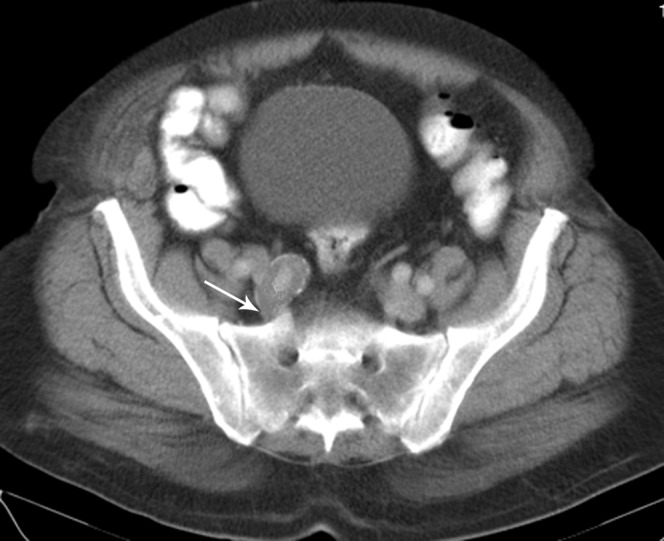
Figure 20.
Piriformis syndrome in a 35-year-old female patient with a history of a traffic accident involvement 7 days previously, and complaining of persistent hip pain radiating to the posterior of her right thigh, as well as numbness in the right foot. Axial CT image reveals an intramuscular piriformis haematoma causing enlargement of the muscle. In addition, thickening and anterior displacement of the right sciatic nerve are seen (arrows).
Pregnancy
Pregnancy-related sciatica may be caused by the direct compression of the nerve roots or secondary to the possible ischaemia of the neural elements caused by compression of the aorta or vena cava by the gravid uterus [19].
Secondary to radiotherapy
Post-radiation neuropathy is a rare condition and has usually been reported with involvements of the cervical and brachial plexus. It is most frequently observed following higher doses of radiation (>5000 rads). Peripheral nerves may be damaged following radiotherapy either directly (by the harmful effects of radiation itself) or indirectly (by diffuse fibrosis of tissues surrounding the nerve caused by radiation). Imaging reveals diffuse nerve thickening with no observable mass. Rarely, however, focal mass-like lesions similar to those of tumour recurrence may be observed, being hypointense on the T1 weighted and hyperintense on the T2 weighted MR images [20]. Contrast enhancement following intravenous administration of gadolinium may also be observed.
Osteoarthritis-related sciatica
Sciatica can be seen as a result of mechanical compression of the sciatic nerve related to degenerative changes (osteophyte formation) in the sacroiliac and hip joints, especially in elderly patients.
References
- 1.Pick T, Howden R. Anatomy, descriptive and surgical (Gray's anatomy). Philadelphia, PA: Running Press, 1974: 781–93 [Google Scholar]
- 2.Moore KL, Dalley AF. Clinically oriented anatomy. Philadelphia, PA: Lippincott, Williams & Wilkins, 1999 [Google Scholar]
- 3.Maravilla KR, Bowen BC. Imaging of the peripheral nervous system: evaluation of peripheral neuropathy and plexopathy. AJNR Am J Neuroradiol 1998;19:1011–23 [PMC free article] [PubMed] [Google Scholar]
- 4.Villarejo FJ, Pascual AM. Injection injury of the sciatic nerve (370 cases). Childs Nerv Syst 1993;9:229–32 [DOI] [PubMed] [Google Scholar]
- 5.Ergun T, Lakadamyali H, Derincek A, Cagla Tarhan N, Ozturk A. Magnetic resonance imaging in the visualization of benign tumors and tumor-like lesions of hand and wrist. Curr Probl Diagn Radiol 2010;39:1–16 [DOI] [PubMed] [Google Scholar]
- 6.Wong M, Vijayanathan S, Kirkham B. Sacroiliitis presenting as sciatica. Rheumatology 2005;44:1323–4 [DOI] [PubMed] [Google Scholar]
- 7.Bredella MA, Steinbach LS, Morgan S, Ward M, Davis JC. MRI of the sacroiliac joints in patients with moderate to severe ankylosing spondylitis. AJR Am J Roentgenol 2006;187:1420–6 [DOI] [PubMed] [Google Scholar]
- 8.Benzel EC, Morris DM, Fowler MR. Nerve sheath tumors of the sciatic nerve and sacral plexus. J Surg Oncol 1988;39:8–16 [DOI] [PubMed] [Google Scholar]
- 9.Maini A, Tripathi M, Shekar NC, Malhotra A. Sciatic schwannoma of the thigh detected on bone scan: a case report. Clin Imaging 2003;27:191–3 [DOI] [PubMed] [Google Scholar]
- 10.Foley KM, Woodruff JM, Ellis FT, Posner JB. Radiation-induced malignant and atypical peripheral nerve sheath tumors. Ann Neurol 1980;7:311–18 [DOI] [PubMed] [Google Scholar]
- 11.Ergun T. Bilateral sciatica secondary to mass lesions in the gluteal muscles. Intramuscular metastasis. J Clin Neurosci 2008;15:1388–426 [DOI] [PubMed] [Google Scholar]
- 12.Beşe NS, Ozgüroğlu M, Dervişoğlu S, Kanberoğlu K, Ober A. Skeletal muscle: an unusual site of distant metastasis in gastric carcinoma. Radiat Med 2006;24:150–3 [DOI] [PubMed] [Google Scholar]
- 13.Williams JB, Youngberg RA, Bui-Mansfield LT, Pitcher JD. MR imaging of skeletal muscle metastases. AJR Am J Roentgenol 1997;168:555–7 [DOI] [PubMed] [Google Scholar]
- 14.Bickels J, Kahanovitz N, Rubert CK, Henshaw RM, Moss DP, Meller I, et al. Extraspinal bone and soft-tissue tumors as a cause of sciatica. Clinical diagnosis and recommendations: analysis of 32 cases. Spine 1999;24:1611–16 [DOI] [PubMed] [Google Scholar]
- 15.Roncaroli F, Poppi M, Riccioni L, Frank F. Primary non-Hodgkin's lymphoma of the sciatic nerve followed by localization in the central nervous system: case report and review of the literature. Neurosurgery 1997;40:618–21 [DOI] [PubMed] [Google Scholar]
- 16.Wider C, Kuntzer T, Von Segesser LK, Qanadli SD, Bogousslavsky J, Vingerhoets F. Bilateral compressive lumbosacral plexopathy due to internal iliac artery aneurysms. J Neurol 2006;253:809–10 [DOI] [PubMed] [Google Scholar]
- 17.Vilos GA, Vilos AW, Haebe JJ. Laparoscopic findings, management, histopathology, and outcome of 25 women with cyclic leg pain. J Am Assoc Gynecol Laparosc 2002;9:145–51 [DOI] [PubMed] [Google Scholar]
- 18.Rossi P, Cardinali P, Serrao M, Parisi L, Bianco F, De Bac S. Magnetic resonance imaging findings in piriformis syndrome: a case report. Arch Phys Med Rehabil 2001;82:519–21 [DOI] [PubMed] [Google Scholar]
- 19.Ashkan K, Casey AT, Powell M, Crockard HA. Back pain during pregnancy and after childbirth: an unusual cause not to miss. J R Soc Med 1998;91:88–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wouter vanEs H, Engelen AM, Witkamp TD, Ramos LM, Feldberg MA. Radiation-induced brachial plexopathy: MR imaging. Skeletal Radiol 1997;26:284–8 [DOI] [PubMed] [Google Scholar]