Abstract
Primary arteritis of the central nervous system (CNS) comprises a heterogeneous group of CNS disorders, which is characterised by non-atheromatous inflammation and necrosis of the arterial wall. The clinical presentation is highly variable, with stroke being the most common manifestation. Conventional angiography is considered to be the best imaging tool for diagnosing the disease. However, angiographic findings, which usually show lumen irregularities and stenosis, are often unspecific and can occur with a variety of other vascular disorders, such as atherosclerosis and arterial dissection. Therefore, brain biopsies are often needed to confirm the diagnosis. Recent reports have shown that MRI is able to visualise contrast enhancement in subjects with known primary CNS arteritis.
This case report suggests that high-resolution contrast-enhanced, black-blood T1 weighted images with fat suppression might be useful for diagnosising intracranial arteritis. This MRI technique has the potential to replace invasive procedures, such as conventional angiography and/or brain biopsies. Furthermore, it provides information about the inflammatory activity of the disease and might be useful for monitoring anti-inflammatory therapy. Further studies are needed to confirm these initial promising results.
We report the case of a 63-year-old woman with right latent hemiparesis, dysarthria, ataxia and a neuropsychological disorder with a depressive syndrome. She had suffered from a stroke affecting the pons and the left thalamus 3 months before admission to our hospital. Furthermore, the patient complained of severe and frequent headaches, and chronic fatigue. A recent oral infection with herpes simplex virus (HSV), which was treated with acyclovir, was also reported. She presented with no cardiovascular risk factors. Blood tests showed no signs of systemic inflammation. Electrocardiogram and echocardiography were normal. Duplex sonography revealed no significant stenosis in the cervical arteries, although blood flow velocity was increased in the basilar artery (85/40 cm s–1). Analysis of cerebrospinal fluid (CSF) revealed an elevated cell count (51/3 mm–3) and an increased protein content (63 mg dl–1). Polymerase chain reaction (PCR) for HSV, varicella zoster virus (VZV), Epstein–Barr virus (EBV) and cytomegalovirus (CMV) were negative. Serological screening for vasculitis (rheumatic factors, complement C3/C4, anti-nuclear antibody (ANA), anti-neutrophil cytoplasmic antibody (ANCA) angiotensin converting enzyme (ACE) was negative.
For further diagnostic workup, the patient was referred to the radiology department for a magnetic resonance (MR) scan. All MR examinations were performed on a clinical high-field MR imager (3.0 Tesla Magnetom Verio, Siemens Healthcare, Erlangen, Germany).
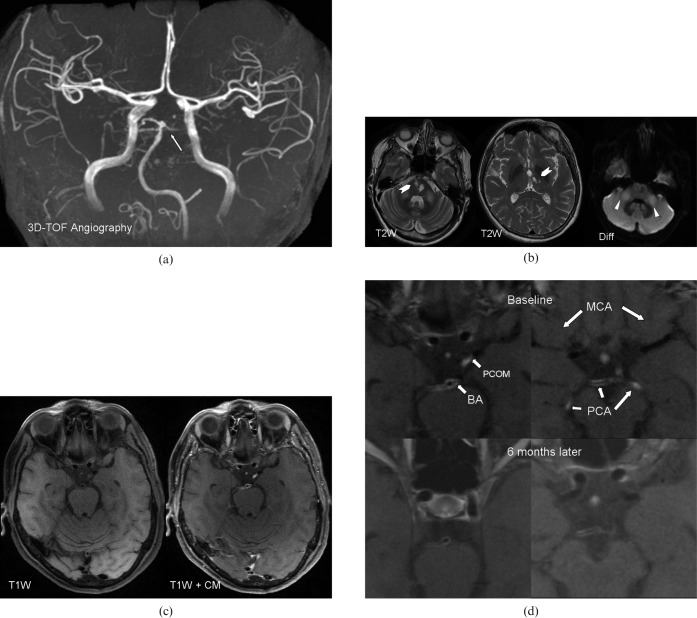
Time-of-flight intracranial MR angiography (Figure 1a) showed unspecific lumen irregularities in the basilar and both posterior cerebral arteries (PCA). T2 weighted turbo spin echoes of the brain (Figure 1b) showed old ischaemic infarcts in the right and left pons and in the left thalamus. Diffusion-weighted images revealed no recent ischaemic infarction or signs of encephalitis, although a slight hyperintensity was noted in both cerebellar peduncles, as an unspecific sign for cerebellitis.
Figure 1.
(a) Three-dimensional time-of-flight (TOF) MR angiography. The arrow points to lumen irregularities in the basilar artery and the posterior cerebral artery. These findings are unspecific and can be found in atherosclerotic disease as well as in central nervous system (CNS) arteritis. (b) Axial T2 weighted (T2W) MR images of the brain show hyperintense areas (chevron) in the left and right pons and in the left thalamus, consistent with ischaemic infarctions. The arrowheads point to hyperintense areas in both cerebellar peduncles, as an unspecific sign for cerebellitis. (c) Axial T1 weighted (T1W) images pre- and post-contrast show strong contrast enhancement in the basilar artery, both posterior cerebral arteries and in the left posterior communication artery, suggestive of CNS vasculitis. No contrast enhancement is seen in both middle cerebral arteries. CM, contrast media. (d) Magnified axial T1 weighted post-contrast images at baseline (first row) and 6 months after initiation of therapy (second row) show an absence of contrast enhancement in the left posterior cerebral artery (PCA) and in the left posterior communication artery (PCOM) and a decrease in the contrast enhancement in the basilar artery (BA) and the right PCA.
High-resolution, black-blood fat suppressed pre- and post-contrast T1 weighted images (double inversion recovery turbo spin echo) were performed using a 12-channel head coil (best in-plane interpolated resolution 0.2 × 0.2 mm2, slice thickness 2 mm). The delayed-enhancement T1 weighted sequence 5 min after the intravenous injection of 0.1 mmol kg–1 (0.2 ml kg–1) gadolinium-DTPA-BMA (Gadobutrol, Bayer Schering, Leverkusen, Germany) showed strong contrast enhancement in the vessel walls of the distal basilar artery, the posterior cerebral arteries and the left posterior communicating artery (Figure 1c), suggesting intracranial arteritis. No arterial contrast enhancement was seen in the middle and anterior cerebral arteries (Figure 1c). Owing to the high suspicion of intracranial arteritis on MRI, the clinical symptoms and the cerebrospinal fluid (CSF) results, a systemic therapy with endoxan and steroids was started immediately. Shortly after the initiation of the therapy, an improvement of the sensomotoric symptoms and of the dysphoric/depressive mental state of the patient were noted. A follow-up examination 3 months after the initiation of therapy (images not shown) revealed a slight decrease in contrast enhancement on the MR images. At the same time CSF showed a decrease in the cell count from 51 to 33/3 mm–3 while protein content decreased from 63 mg dl–1 to 50 mg dl–1. However, the patient still suffered from recurrent headaches and fatigue, and endoxan/steroid combination therapy was continued. 6 months after initiation of anti-inflammatory therapy the headaches and fatigue disappeared. At the same time, MRI showed a substantial decrease in the contrast enhancement of the arterial wall in the basilar artery and right cerebral artery (Figure 1d) and an absence of contrast enhancement in the left communication artery and left posterior cerebral artery. CSF showed a further decrease in the cell count to 24/3/mm3 while protein content remained at the same level seen after 3 months. These findings suggest that MRI is able to visualise the inflammatory activity of primary central nervous system (CNS) vasculitis with good correlation to the clinical status of the patient.
Primary arteritis of the CNS comprises a heterogeneous group of CNS disorders that is characterised by non-atheromatous inflammation and necrosis of the arterial wall [1]. The clinical presentation is highly variable, with stroke being the most common manifestation [2].
Conventional angiography is considered to be the best imaging tool to diagnose the disease. However, angiographic findings, which usually show lumen irregularities and stenosis, are often unspecific and can occur with a variety of other vascular disorders, such as atherosclerosis and arterial dissection. Therefore brain biopsies are often needed to confirm the diagnosis [3].
Black-blood pre- and post-contrast T1 weighted sequences with fat suppression enable the delineation of the arterial wall from the lumen and the surrounding perivascular tissue. Furthermore, post-contrast T1 weighted sequences allow visualising contrast enhancement of the arterial wall. To date, these sequences have been used successfully to evaluate the composition and morphology of the carotid atherosclerotic plaque [4] and to assess the mural enhancement in the superficial temporal artery in giant cell arteritis [5]. Recent reports have shown that MRI is able to visualise contrast enhancement in subjects with known primary CNS arteritis [6].
In our patient strong, mural contrast enhancement was seen in several intracranial arteries, which decreased substantially after 6 months of anti-inflammatory therapy. The extent of the contrast enhancement and the distribution of the enhancement was atypical of atherosclerotic disease, in which contrast enhancement is generally weaker, does not compromise the whole vessel wall and is commonly localised at the shoulder region of the atherosclerotic plaque [4].
This case report suggests that high-resolution contrast-enhanced, black-blood T1 weighted images with fat suppression might be useful for the diagnosis of intracranial arteritis. This may allow invasive procedures to be replaced, such as conventional angiography and/or brain biopsies. Furthermore, this MRI technique provides information about the inflammatory activity of the disease and might be useful for monitoring anti-inflammatory therapy. Further studies are needed to confirm these initial promising results.
References
- 1.Younger DS. Vasculitis of the nervous system. Curr Opin Neurol 2004;17:317–36 [DOI] [PubMed] [Google Scholar]
- 2.Hajj-Ali RA, Calabrese LH. Central nervous system vasculitis. Curr Opin Rheumatol 2009;21:10–8 [DOI] [PubMed] [Google Scholar]
- 3.Miller DV, Salvarani C, Hunder GG, Brown RD, Parisi JE, Christianson TJ, et al. Biopsy findings in primary angiitis of the central nervous system. Am J Surg Pathol 2009;33:35–43 [DOI] [PubMed] [Google Scholar]
- 4.Saam T, Hatsukami TS, Takaya N, Chu B, Underhill H, Kerwin WS, et al. The vulnerable, or high-risk, atherosclerotic plaque: noninvasive MR imaging for characterization and assessment. Radiology 2007;244:64–77 [DOI] [PubMed] [Google Scholar]
- 5.Bley TA, Wieben O, Uhl M, Thiel J, Schmidt D, Langer M. High-resolution MRI in giant cell arteritis: imaging of the wall of the superficial temporal artery. AJR Am J Roentgenol 2005;184:283–7 [DOI] [PubMed] [Google Scholar]
- 6.Küker W, Gaertner S, Nagele T, Dopfer C, Schoning M, Fiehler J, et al. Vessel wall contrast enhancement: a diagnostic sign of cerebral vasculitis. Cerebrovasc Dis 2008;26:23–9 [DOI] [PMC free article] [PubMed] [Google Scholar]