Abstract
Renal angiomyolipoma is recognised as a benign hamartomatous lesion with no obvious malignant potential. However, the tumour may show extrarenal/perinephric extension at times. Rarely, the lesion may extend into the renal vein and inferior vena cava (IVC) indicating aggressive behaviour. We present a case of an angiomyolipoma of the kidney with sonographic, CT and MRI evidence of extension into the renal vein and IVC.
Renal angiomyolipomas are the most common mesenchymal tumours of the kidney; they occur sporadically or in association with tuberous sclerosis where they can be bilateral and multiple. These are usually detected incidentally presenting as echogenic masses on ultrasound or fat-containing lesions on CT or MRI. At times, they may show aggressive behaviour in the form of perinephric extension and invasion into the renal vein and inferior vena cava (IVC). Here we report a case of large aggressive angiomyolipoma (AML) growing into the renal vein and IVC.
Case report
A 40-year-old female presented with complaints of pain and stiffness in the right side of her abdomen for 1 year. She also complained of pain while passing urine. Pain was mild in intensity and did not interfere with her daily routine. No history of fever, weight loss, anorexia, decreased urine output, haematuria or burning micturation was present. She was diagnosed as hypothyroid 1 year ago and was on regular medication. No other relevant history was present. Physical examination revealed no significant abnormality. Routine laboratory investigations were within normal limits with haemoglobin of 12 g dl–1, total leukocyte count of 8 × 103 μl–1, urea of 21 mg dl–1 and creatinine of 0.8 mg dl–1. Urinalysis revealed 3+ protein. Ultrasonography of the abdomen was then carried out which showed an echogenic mass in the right kidney which extended into the IVC (Figure 1a,b). CT abdomen showed focal mass of fat attenuation (−48 HU to −80 HU) in the right renal pelvis extending into the renal vein and IVC. No calcification was seen in it (Figure 2a,b). MRI of the abdomen revealed mass in the renal pelvis appearing hyperintense on T1 weighted and T2 weighted images (Figure 3a,b) and showed suppression on fat saturated images (Figure 4a). The mass was extending into the right renal vein and IVC (Figure 4b). Inferiorly, the lesion was extending into the perinepheric space. No evidence of any hydronephrosis or locoregional lymphadenopathy was seen. No soft-tissue component was seen within the mass. Based on the above findings, a diagnosis of possible AML invading the right renal vein and IVC was made. A right radical nephrectomy and IVC thrombectomy was performed and the specimen was sent for histopathological examination which revealed triphasic tumour composed of a mixture of mature adipocytes, many thick blood vessels and smooth muscle components consistent with AML. No cytological atypia, mitosis or necrosis was seen.
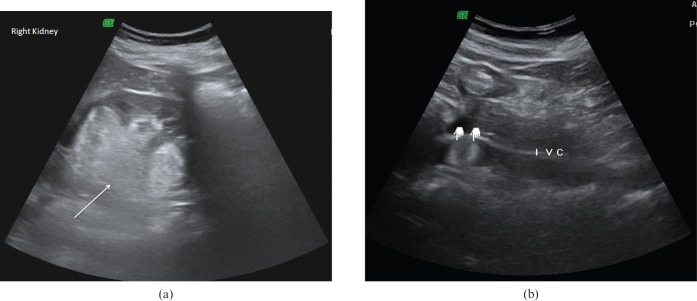
Figure 1.
Ultrasonography of the right lumbar region showing (a) an echogenic mass in the right kidney (arrow) and (b) mass extending into the inferior vena cava (marked).
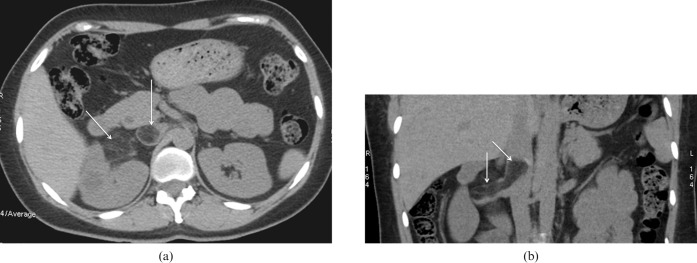
Figure 2.
(a) Axial CT section showing a focal mass of fat attenuation (−48 HU to −80 HU) in the right renal pelvis. (b) Coronal CT image showing extension of the lesion into the renal vein and inferior vena cava (arrows).
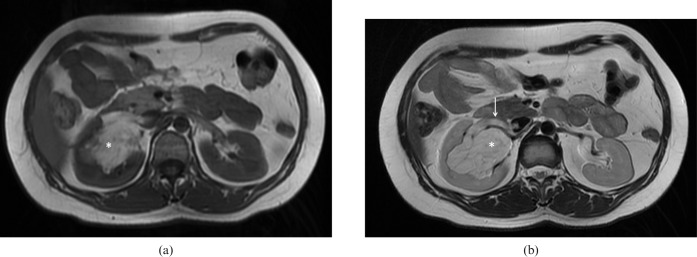
Figure 3.
(a) T1 weighted MRI of the abdomen showing a hyperintense mass (asterisk) in the renal pelvis. (b) T2 weighted MRI mass (asterisk) shows hyperintense signal with extension into renal vein (arrow).
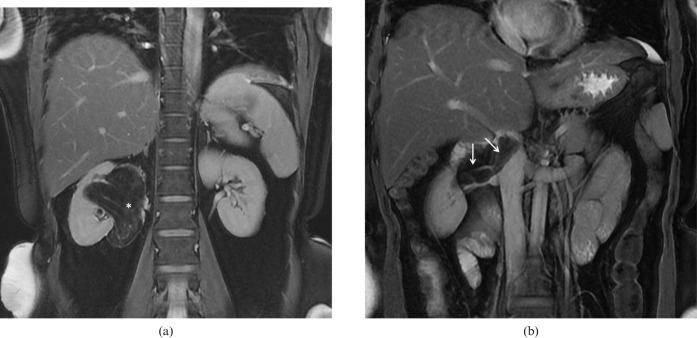
Figure 4.
(a) Coronal fat saturated MRI showing suppression of fatty lesion (asterisk). (b) Coronal fat saturated MRI showing extension of the mass into right renal vein and inferior vena cava (arrows).
Discussion
AML is the most common renal mesenchymal tumour composed of blood vessels, smooth muscles and adipose tissues. It can be sporadic or seen in association with tuberous sclerosis. Sporadic variety is the more common type and is typically seen in middle aged patients with a mean age of 43 years. Females are more commonly affected with a female-to-male ratio of 4:1 [1]. Tumours in this group are usually solitary. AMLs seen in association with tuberous sclerosis are frequently bilateral and multifocal. These can be seen in children as well as in adults [2].
AMLs <4 cm in size are usually incidentally detected during sonography or CT scan for some other indication. Tumours >4 cm in size can present with loin pain, anaemia or haematuria. Larger tumours also carry a significant risk of intratumoural and perinephric haemorrhage. On sonography, the lesion appears as a highly echogenic mass within the renal cortex. Echogenic appearance can be due to fat content of the lesion or complex interfaces produced by blood vessels and smooth muscles. Angiomyolipomas may also demonstrate mixed or reduced echogenicity. On CT, the lesion is seen as a well-defined, circumscribed hypodense focal lesion. HU value, typically that of fat (−10 HU or lower), is almost diagnostic. Lesions without any detectable fat cannot be distinguished from other renal neoplasms. Approximate 5% of AMLs do not show the fat attenuation on CT scan and hence cannot be differentiated from renal cell carcinoma (RCC).
Lesions vary in size from small nodules to large tumours. Larger tumours may show areas of haemorrhage on CT which may obscure the fat component. These tumours are supposed to be non-aggressive but may exhibit capsular invasion and perinephric extension. On rare occasions the tumour may show extension into venous structures indicating aggressive local invasion [3]. Intravascular extension of the lesion into the renal vein and IVC indicates an aggressive element [4,5]. The first case of such a tumour was reported in 1982 and only a few cases have been reported in the literature to date. Approximately 75% of all reported cases of aggressive AML occur as sporadic isolated cases with only 25% related to tuberous sclerosis [2]. MRI may also detect the presence of fat in AMLs which is highly specific for AML. The diagnosis can be confirmed with the use of fat saturation techniques [1].
Thus, various imaging modalities not only help in making the diagnosis of AML but also help in pre-operative evaluation. CT with reformatted images and MRI not only confirm the diagnosis but also clearly demonstrate the cephalic extent of tumour thrombus. Differentials of such a fat-containing lesion would include lipoma, liposarcoma and fat-containing RCC.
Biopsy is rarely needed in view of the typical imaging findings of AML. Tumours smaller in size (<4 cm) are followed annually with CT or ultrasonography. Larger tumours (>4 cm) presenting with intratumoural/perinephric haemorrhage can be treated conservatively with partial nephrectomy or selective catheter embolisation [2].
Conclusion
Renal AML at times can be aggressive and may show extension into renal vein and IVC. Such cases should be managed cautiously with prompt surgical intervention. Various imaging modalities play a pivotal role in confirming the diagnosis and in pre-operative evaluation of lesions.
References
- 1.Dogra V, Levine E. The kidney. Haaga's textbook on CT and MRI imaging of the whole body, 4th edition. St. Louis: Mosby, 2003: 1577–578 [Google Scholar]
- 2.Yiu WC, Chu SM, Collins RJ, Tam PC, Chan FL, Ooi GC. Aggressive renal angiomyolipoma: radiological and pathological correlation. JHK Coll Radiol 2002;5:240–2 [Google Scholar]
- 3.Aranson AM, Graham RT, Shaw P, Srigley J, Herschorn S. Angiomyolipoma of the kidney extending into the inferior vena cava: sonographic and CT findings. AJR Am J Roentgenol 1988;151:1159–61 [DOI] [PubMed] [Google Scholar]
- 4.Bosniak MA, Megibow AJ, Hulnik DH, Horii S, Raghavendra BN. CT diagnosis of renal angiomyolipoma: the importance of detecting small amounts of fat. AJR Am J Roentgenol 1988;151:497–501 [DOI] [PubMed] [Google Scholar]
- 5.Israel GM, Bosniak MH, Slywotzky CM, Rosen RJ. CT differentiation of large exophytic renal angiomyolipomas and perirenal liposarcomas. AJR Am J Roentgenol 2002;179:769–73 [DOI] [PubMed] [Google Scholar]