Abstract
Objectives
The prompt identification of children in whom enema reduction of intussusception might fail and surgery is necessary is crucial in order to avoid futile repeat attempts and untoward complications. The purpose of this retrospective review was to determine whether air encircling the intussusceptum in the small bowel during air enema for intussusception reduction could serve as an indication for operation rather than repeat attempts at radiological reduction.
Methods
Imaging studies of 83 children aged 4 to 40 months with idiopathic intussusception who had air enema for intussusception reduction were reviewed for the presence of air encircling the intussusceptum in the distal small bowel. Findings were correlated with clinical course and surgical findings.
Results
In 12 of 83 patients, air was seen encircling the intussusceptum in the small bowel, and in 11 of these (88%) air enema failed to reduce the intussusception. In 8 of the 11, delayed repeated attempts using air enema failed to reduce intussusception. Clinical signs and their duration did not differ between those children without and those with air encircling the intussusceptum.
Conclusion
In the presence of air encircling the intussusceptum in the distal small bowel on air enema, delayed repeated attempts for intussusception reduction are unlikely to succeed, and surgery is indicated.
Since the advent of enemas for the treatment of idiopathic ileocolic intussusceptions, the rate of surgical reduction has fallen drastically and radiographically controlled reduction has become the mainstay of treatment [1,2]. Mass use of ultrasound as a diagnostic modality has led to earlier detection, with a higher success rate for enema reduction of intussusceptions [2]. While most cases of ileocolic intussusception are successfully reduced without surgery, there remains a subgroup of paediatric patients who require operative intervention [3,4]. The presence of shock, peritonitis or perforation with free air obviates the enema trial [5,6]. Most patients with ileoileal intussusception or intussusception with a pathological lead point on sonography can also be reduced by air enema in an acute situation [7]; surgical treatment may be indicated at a later date.
When complete reduction at the level of the caecum fails, repeat attempts using enema may be appropriate if the child's clinical status permits [2,8-12]. If repeat attempts fail, reduction is performed surgically. There is an ongoing quest for clinical and imaging criteria that can differentiate between patients who can benefit from repeat air enema after initial failure and those who require surgery [11-13]. This differentiation is important, since a delay in reduction may lead to a severe compromise of bowel viability [14].
There are currently very few clinical or imaging findings considered specific to predict irreducibility for the minority of patients in whom radiological reduction fails [2]. The “dissection sign” on barium enema has been reported as an indication of ileocolic or colocolic intussusception that requires surgery [15]; however, barium enema is currently not used as frequently as air enema for intussusception reduction [4]. In one report, an “appendix sign” on air enema has been reported as an indication for surgical intervention [16].
Over a 3 month period, 4 children aged 5–18 months presented to our emergency department with intermittent abdominal pain and vomiting of 1–2 days’ duration. The children were otherwise healthy, and on presentation had no clinical signs indicating bowel necrosis or peritonitis. Abdominal sonography showed ileocolic intussusception with vascular flow in the bowel wall in colour Doppler in all patients. Air enema reduction was attempted and the intussusception was reduced to the level of the caecum in all four patients, but failed to reduce into the small bowel. Instead, upon reaching the caecum, a mobile intussusception encircled by air, protruding into the caecum on a stalk, was noted (Figures 1 and 2). Reflux of air around the intussusceptum into the terminal ileum was observed in all cases. Despite the prolonged presence of air around the intussusceptum in the caecum and the terminal ileum, the intussusception could not be reduced. Repeat sonography was performed in two of these patients and confirmed the persistence of an ileocolic intussusception (Figures 2 and 3). Delayed repeated attempts to reduce the intussusception were unsuccessful, and each patient was ultimately transferred to the operating room for laparotomy.
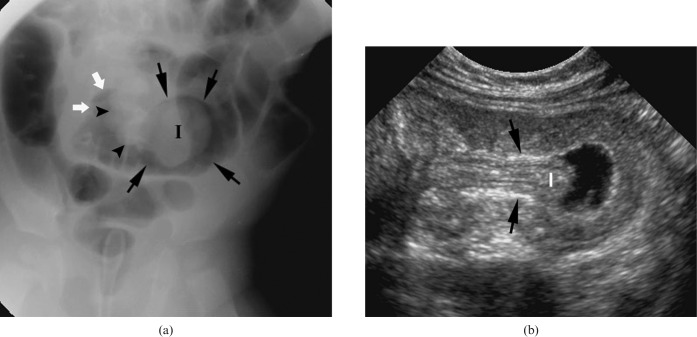
Figure 1.

Intussusception in a 12-month-old girl who presented with fever and restlessness for 48 h. Fluoroscopy image in the prone position demonstrates the intussusception (I), surrounded by air (arrows), protruding through the ileocaecal valve on a narrow stalk (arrowheads).
Figure 2.
Intussusception in a 14-month-old boy who presented with abdominal pain and bloody diarrhoea for 72 h. Fluoroscopy image in the prone position (a) demonstrates the intussusception (I), surrounded by air (arrows), protruding through the ileocaecal valve on a short stalk (arrowheads). A small amount of air is seen in the distal small bowel (white arrows). On sonography (b), the intussusceptum head (I) is surrounded by tiny echogenic dots (arrows), representing air between the intussusceptum and the intussuscipiens.
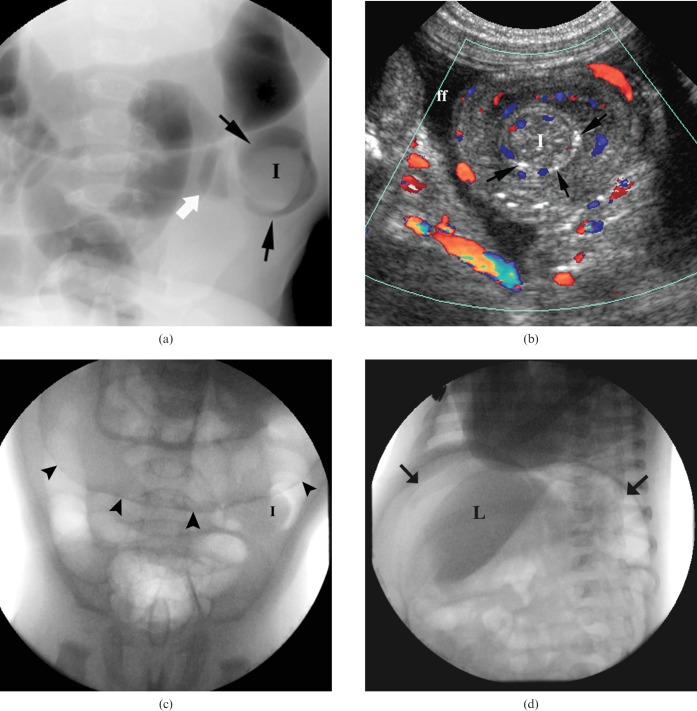
Figure 3.
Intussusception in a 4-month-old boy who presented with diarrhoea for 24 h. Fluoroscopy image in the prone position (a) demonstrates the intussusception (I), surrounded by air (arrows), protruding through the ileocaecal valve. A small amount of air can be seen in the distal small bowel (white arrow). Repeat sonography (b) confirmed the persistence of the intussusception and demonstrated tiny echogenic dots representing air (arrows) between the intussusceptum head (I) and the intussuscipiens mucosa. ff, free fluid. Fluoroscopy during a delayed reduction attempt (c) demonstrates the persisting intussusception (I) and free air, delineating the transverse colon (arrowheads), as confirmed in an oblique view (d), anterior and posterior to the liver (L) and under the diaphragm (arrows).
Operative findings in all four patients were similar: ileoileal intussusception starting proximal to the ileocaecal valve and protruding into the colon, leaving the caecum intact (ileo-ileocolic intussusception). No pathological lead point was found. Manual reduction was uneventful; there was no need for bowel resection in any of the patients.
In view of these findings, we reviewed imaging studies and patients’ records of all children treated for intussusception in our hospital over a 3.5 year period. The purpose of our study was to determine whether air encircling the intussusceptum in the distal small bowel during air enema for intussusception reduction could serve as a sign predicting necessity for operation rather than repeat attempts at radiological reduction.
Methods and materials
We performed a retrospective review of all children treated for intussusception in the two campuses of our hospital from November 2005 to April 2009. Imaging studies of all children with intussusception diagnosed by sonography, who were referred for air enema reduction, were reviewed through our common picture archiving and communication system (PACS) system. Air enema reduction attempts were performed under fluoroscopy guidance, without sedation, applying pressure of 90–120 mmHg, in the prone position. Presence of air encircling the intussusceptum within the distal small bowel (the intussuscipiens) was defined as a positive finding. Imaging studies from each campus were reviewed separately by a paediatric radiologist from the other campus; radiologists were thus blinded to the clinical outcome. Equivocal cases were jointly discussed in a consecutive session of combined reading by both radiologists, and diagnosis was established by consensus.
In addition, in order to avoid selection bias, hospital records and imaging studies of all children who needed operation for intussusception were separately reviewed in order to detect possible additional patients who might have been operated without having enema reduction first, or who might have had similar imaging findings that were missed. Data recorded included the patient’s age, sex, clinical symptoms and their duration, surgical findings when present and clinical outcome. Sensitivity, specificity, positive predictive value and negative predictive value of air encircling the intussusceptum in the caecum and terminal ileum for irreducibility were calculated. The study was approved by the institutional review board.
Results
83 patients who had 97 air enemas for intussusception reduction were identified. Eight patients had two separate events of intussusception, one patient had three events and one patient had five events. Air encircling the intussusceptum in the small bowel was clearly identified in 12 patients (our 4 index cases and 8 additional cases), and imaging findings were equivocal in 1. In 11 of the 12 patients (Table 1, patients 1–9, 11, 12) in whom this finding was present, air enema failed to reduce the intussusception; 6 of these were female and 5 were male, aged 4–40 months (mean 12 months). All children were operated on within 1–2 h from the attempted failed reduction. At operation, the intussusception was manually reduced in all 11 children. In one patient, a Meckel's diverticulum was identified and resected. In a second patient a distal ileal mass was palpated and ileocaecal resection was performed; lymphoid hyperplasia with necrosis was found in the resected bowel. In these two patients, sonography did not reveal the character of the leading point found at operation. In a third patient, a 4-month-old boy, the initial reduction attempt succeeded in reducing the intussusception from the splenic flexure to the caecum but failed to reduce it to the small bowel; air was seen in the distal small bowel (Figure 3a). Repeat sonography confirmed the persistence of the intussusception (Figure 3b) and a delayed repeated attempt was performed 4 h later. During this second attempt, free air was noted and the patient was rushed to theatre (Figure 3c,d). At operation, a tiny perforation was found in the transverse colon and was repaired. The intussusception was easily reduced from the caecum to the small bowel; no pathological leading point was identified. A fourth patient (patient 12), who presented with a fifth recurrent event of intussusception, had already been operated on twice before for irreducible ileocolic intussusception (without a pathological leading point or bowel resection; patients 4 and 12) and was later found to have intestinal lymphoid hyperplasia on small-bowel follow-through barium study. On two other occasions the intussusception was successfully reduced by air enema. On the fifth occasion, she had a long-segment ileo-ileocolic intussusception that could not be reduced by air enema, with air encircling the intussusceptum in the caecum and the distal small bowel (Figure 4a). At operation, a very long ileoileal intussusception was found protruding through the intact ileocaecal valve with focal areas of bowel wall necrosis (Figure 4b), which was fortunately reversible. There was marked submucosal and mesenteric lymphadenopathy, which was sampled and was found to be reactive lymph node enlargement. The intussusception was manually reduced without resection and the post-operative recovery was unremarkable.
Table 1. Clinical symptoms, sonographic findings and surgical findings in 13 patients with air encircling the intussusceptum on air enema.
| Patient | Age (months) | Gender | Clinical symptoms | Duration (h) | Sonographic findings |
Surgical findings |
|||
| Extension of intussusception | Mesenteric lymph nodes | Free fluid | IICI | Additional findings | |||||
| 1 | 5 | M | Restlessness, vomiting | 24 | RLQ to splenic flexure | − | − | Mesenteric lymph nodes, free fluid | |
| 2 | 6 | F | Fever, restlessness, vomiting, currant jelly stools | 24 | RLQ | + | − | + | |
| 3 | 8 | F | Fever, URTI 5 days, vomiting, currant jelly stools | 24 | RLQ to transverse colon | + | + | ||
| 4 | 20 | F | Restlessness/apathy, vomiting | 24 | RLQ to hepatic flexure | + | − | + | |
| 5 | 14 | M | Fever, bloody diarrhoea | 72 | RLQ to splenic flexure | + | − | + | Oedematous small bowel wall |
| 6 | 18 | M | Restlessness, vomiting | 24 | RLQ to descending colon | + | + | + | Meckel's diverticulum resected |
| 7 | 5 | M | Abdominal pain, vomiting, diarrhoea | 48 | RLQ to transverse colon | + | − | + | |
| 8 | 6 | F | Vomiting | 96 | RLQ to transverse colon | − | + | + | |
| 9 | 4 | M | Diarrhoea | 24 | RLQ to splenic flexure | + | − | Transverse colon perforation | |
| 10 | 24 | F | Vomiting | 36 | RLQ to transverse colon | + | − | NA | NA |
| 11 | 6 | F | Fever, restlessness, vomiting, currant jelly stools | 12 | RLQ | + | − | + | 5 cm flattened necrotic tissue in distal ileum wall |
| 12 | 40 | F | Abdominal pain, vomiting, lethargy | 10 | LUQ | + | − | + | Mesenteric and submucosal lymph nodes, moderate bowel wall necrosis |
IICI, ileo-ileocolic intussusception; NA, not applicable (patient did not undergo surgery); RLQ, right lower quadrant; URTI, upper respiratory tract infection; LUQ, left upper quadrant.
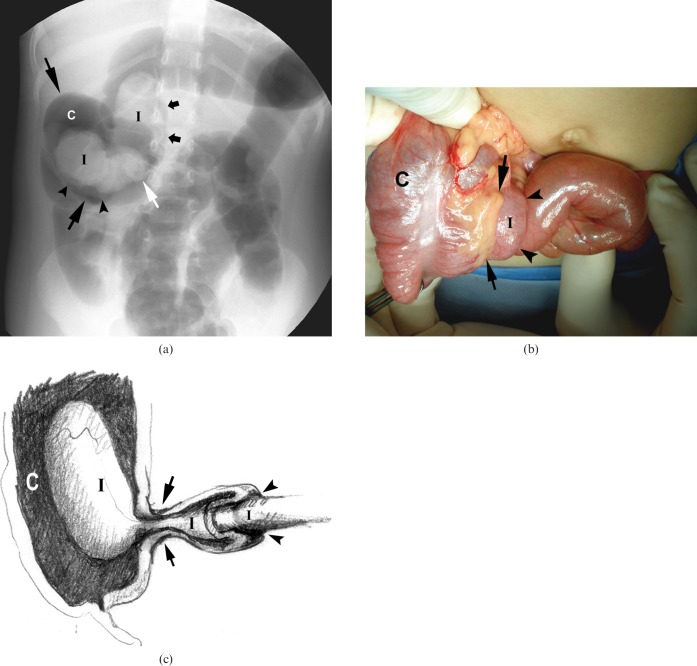
Figure 4.
Recurrent intussusception in a 36-month-old girl who presented with intermittent abdominal pain and lethargy for 10 h. Fluoroscopy image in the supine position (a) demonstrates the ileoileal intussusception (I), surrounded by air in the caecum (C, long arrows), protruding through the ileocaecal valve (long white arrow) on a short stalk (arrowheads). The double density of the ileum protruding into the caecum reflects the overlapping inner and outer layers of the intussusception. A small amount of air can be seen in the distal small bowel (short arrows). Intraoperative image (b) shows the ileoileal component (I), partially reduced from the caecum (C), the intact ileocaecal valve (arrows) and the point of intussusception (arrowheads). Discolouration along the serosal ileal margin reflects early necrosis (which proved to be reversible) of the bowel wall. (c) The ileoileal component (I) of an intussusception (arrowheads) protruding through an intact ileocaecal valve (long arrows) into the caecum (C).
In the other seven children who underwent operation, no pathological lead point could be identified and there was no need for bowel resection. In 8 of the 11 patients who were operated on (73%), ileoileal intussusception was found, protruding through an otherwise intact ileocaecal valve (ileo-ileocolic intussusception; Figure 4d). In the other three patients, ileocolic intussusception was reported. Clinical and surgical findings are presented in Table 1. Clinical symptoms and their duration did not differ between the 11 patients in whom reduction failed and the patients who had a successful reduction. None of these children was initially hospitalised elsewhere or transferred after being investigated in another institute. None of the children treated for intussusception in our institute during the study period was referred directly for surgery. All of the children are doing well following surgery, at a mean follow-up period of 18 months (range 2–40).
In a 24-month-old female (patient 10) with a positive finding, the intussusception was reduced in a delayed reduction attempt (4 h after the first attempt). In the other 8 children in whom delayed reduction was attempted (15 min in 2 patients, 1 h in 2 patients, 4 h in 3 patients and 12 h in 1 patient) air enema failed to reduce the intussusception.
In a 12-month-old female, imaging findings were equivocal. In this patient the intussusception was eventually reduced using air enema; however, the study contained more images and took more time than most of the other reductions, indicating increased difficulty in the reduction procedure.
Three children in whom air encircling the intussusceptum was not seen were also operated on. Two children were operated on following a partial air enema reduction of intussusception, one from the rectum to the sigmoid colon and one from the sigmoid to the transverse colon. One child was operated on for a recurrent ileoileal intussusception 5 h following successful air enema reduction of an ileocolic intussusception; a Meckel's diverticulum was recognised in the repeat sonography and was resected. A review of hospital records of children undergoing surgery for intussusception reduction without an initial attempt at enema reduction did not reveal any additional cases. In this series, the appearance of air encircling the intussusceptum had a sensitivity of 100% for identifying failure of an enema reduction attempt, a specificity of 98%, a positive predictive value of 92% and a negative predictive value of 100%.
Discussion
Reduction of intussusception by enema is the mainstay treatment for this condition in children. Although highly successful in most cases, there remains a subgroup of patients who require operative manual reduction. This subgroup consists of patients who have an ileoileal intussusception with or without a pathological lead point who do not undergo spontaneous reduction, patients presenting following a prolonged course with compromised bowel viability, and patients who have undergone failed repeat enema reduction attempts [1-4,7,17].
There is a growing tendency to attempt repeated delayed enema intussusception reduction if a progressive partial reduction was achieved during earlier attempts, as long as the child is clinically stable and is closely observed, in order to avoid unnecessary operation [1,2,7,10-12]. However, it is important to recognise which of these children will require prompt surgery, as delay may further compromise bowel viability and lead to necrosis, morbidity and sometimes even death [3,18]. This need is more pronounced in rural or remote areas where simple intussusception may be treated by air enema locally, but the delay associated with further reduction attempts may waste valuable time until the child is transferred to a tertiary hospital [14].
Air enema has become the preferred method for intussusception reduction in most centres [2-4,7]. It is thus important to characterise findings in this method that can predict irreducibility. We propose a radiological finding that seems to predict irreducibility of intussusception with air enema. In all our cases with this finding the intussusceptum was initially reduced to the level of the caecum or the terminal ileum but complete reduction into the small bowel was not achieved. Following partial reduction, a small amount of air became insinuated around the intussusceptum and could be detected alongside the intussusceptum within the distal small bowel (Figures 1a, 2a, 3a, 4a).
When air becomes insinuated between the intussusceptum and the intussuscipiens bowel wall, the surface area against which the air is inflated increases. As a result, the pressure pushing the intussusceptum within the bowel lumen decreases, lowering the probability of complete reduction via enema. Moreover, the air becoming insinuated between the intussusceptum and the intussuscipiens creates pressure around the intussusceptum, acts in opposition to the force created by the air pressure in the colon and further reduces the probability of successful reduction. The prolonged presence of air around the persistent filling defect delineating the intussusceptum creates the appearance of a highly mobile mass on a stalk (Figures 1a, 2a, 4a). This radiographic finding correlates with the surgical finding of an ileoileal intussusception that protrudes through the ileocaecal valve (ileo-ileocolic intussusception) while leaving the caecum intact, as occurred in eight of our patients (Figure 4). In one study, such ileo-ileocolic intussusception was the most likely type of intussusception to result in bowel wall necrosis [19]; hence, the importance of early recognition and appropriate management of these cases.
There is only one previous report of failure to reduce intussusception owing to reflux of air into the small bowel. Hedlund et al [20] described three cases in which air refluxed into the small bowel following low-pressure (30–50 mm Hg) air enema, initially without complete reduction of the intussusception. However, in these patients, the intussusception was completely reduced when higher pressure (80–120 mm Hg) was applied, as is the current practice [20].
Reflux of air into the proximal small bowel at low pressure can be explained by flow of air through, rather than around, the slightly open central lumen of the intussusceptum into the bowel loop proximal to the intussusception. This passage of air is possible as long as air pressure in the lumen is not yet high enough to achieve complete reduction. With continuous inflation of air, the intussusceptum enfolds inwards and the central lumen closes, thus enabling luminal pressure to increase and produce complete reduction [21].
The cases reported in our study emphasise the importance of careful examination of the caecum and the distal small bowel for the presence of a persistent filling defect despite some passage of air beyond the intussusceptum head towards the proximal small bowel loops. This is especially important in patients in whom a repeat attempt at air enema reduction is weighed against the option of surgical intervention. Of the nine patients with the finding of air encircling the intussusceptum in this series in whom delayed repeat reduction was attempted, eight eventually required surgery, including one who also had a transverse colon perforation (Figure 3).
We were able to find only one additional report of failure to reduce an ileocolic intussusception because of reflux of contrast around the intussusceptum; however, the authors of this report were using a barium enema. Fishman et al [15] described the dissection of barium between the intussusceptum and the intussuscipiens in 23 out of 43 cases of failed barium enema reduction (53%), as opposed to none among 43 cases of successful reduction. They therefore considered barium dissection as an indication for surgical management. Barium dissection may explain the “solar eclipse” appearance in a case reported by Raveenthiran [22]. However, in most paediatric centres, barium enema has been replaced by air enema as the preferred method for intussusception reduction. It is therefore important that radiologists are aware that air encircling the intussusceptum in the distal small bowel is a sign predicting irreducibility at air enema as well, and that they are able to recognise this.
Can the presence of air between the intussusceptum and the intussuscipiens also be demonstrated by sonography? Although the sonographic findings were not the focus of our study, we believe that we were able to identify and demonstrate this in two out of three patients in this series who had sonography following a failed air enema reduction attempt. The small amount of air is seen as tiny echogenic dots encircling the intussusceptum head, abutting the intussuscipiens mucosa (Figures 2b, 3b). This sonographic appearance can be useful when air enema findings are unclear or equivocal and repeat sonography is performed following air enema, and can be added to the other sonographic features that have been described as associated with decreased enema reduction rates [2,23]. It has to be emphasised that this particular sonographic sign is only seen after an air enema reduction attempt.
The major drawbacks of our study are its relatively small sample size and its retrospective nature. Nevertheless, ileo-ileocolic intussusception could not be reduced by air enema in 11 of 12 patients (92%) in whom air encircling the intussusceptum was found; moderate (fortunately reversible) bowel wall necrosis was found in 1 patient; and bowel perforation occurred in another patient in a 4 h delayed second reduction attempt. Of 14 patients who underwent surgery for irreducible intussusception in our institute in the study period, 11 (79%) had air encircling the intussusceptum on air enema; 2 were operated on for irreducible intussusception in the colon; and 1 for an ileoileal intussusception. Ileocolic intussusception was successfully reduced in 71 patients (who had 86 events of intussusception) in this series of 83 children (89% of 97 events). The incidence of lead point or bowel necrosis in this series was typical of reports in the literature: In two patients, a Meckel's diverticulum was found at surgery; in one case of lymphoid hyperplasia with necrosis was found; and there was one case of bowel perforation. The rate of successful enema reduction was similar to those reported elsewhere.
Conclusion
The presence of air encircling the intussusceptum within the distal small bowel on air enema implies that repeated attempts to reduce intussusception may fail; therefore, in order to minimise further compromise of bowel viability, further enema reduction attempts should be abandoned and the patient should undergo surgery without delay.
Acknowledgments
The authors thank Ms Shifra Fraifeld for her help in the preparation of this manuscript and Dr Yair Peled for his assistance with photography.
References
- 1.Daneman A, Navarro O. Intussusception. Part 1. A review of diagnostic approaches. Pediatr Radiol 2003;33:79–85 [DOI] [PubMed] [Google Scholar]
- 2.Daneman A, Navarro O. Intussusception. Part 2. An update on the evolution of management. Pediatr Radiol 2004;34:97–108; quiz 187 [DOI] [PubMed] [Google Scholar]
- 3.Kaiser AD, Applegate KE, Ladd AP. Current success in the treatment of intussusception in children. Surgery 2007;142:469–75; discussion 475–7 [DOI] [PubMed] [Google Scholar]
- 4.Ko HS, Schenk JP, Troger J, Rohrschneider WK. Current radiological management of intussusception in children. Eur Radiol 2007;17:2411–21 [DOI] [PubMed] [Google Scholar]
- 5.Barr LL, Stansberry SD, Swischuk LE. Significance of age, duration, obstruction and the dissection sign in intussusception. Pediatr Radiol 1990;20:454–6 [DOI] [PubMed] [Google Scholar]
- 6.Ramachandran P, Gupta A, Vincent P, Sridharan S. Air enema for intussusception: is predicting the outcome important? Pediatr Surg Int 2008;24:311–13 [DOI] [PubMed] [Google Scholar]
- 7.Navarro OM, Daneman A, Chae A. Intussusception: the use of delayed, repeated reduction attempts and the management of intussusceptions due to pathologic lead points in pediatric patients. AJR Am J Roentgenol 2004;182:1169–76 [DOI] [PubMed] [Google Scholar]
- 8.Connolly B, Alton DJ, Ein SH, Daneman A. Partially reduced intussusception: when are repeated delayed reduction attempts appropriate? Pediatr Radiol 1995;25:104–7 [DOI] [PubMed] [Google Scholar]
- 9.Gonzalez-Spinola J, Del Pozo G, Tejedor D, Blanco A. Intussusception: the accuracy of ultrasound-guided saline enema and the usefulness of a delayed attempt at reduction. J Pediatr Surg 1999;34:1016–20 [DOI] [PubMed] [Google Scholar]
- 10.Gorenstein A, Raucher A, Serour F, Witzling M, Katz R. Intussusception in children: reduction with repeated, delayed air enema. Radiology 1998;206:721–4 [DOI] [PubMed] [Google Scholar]
- 11.Sandler AD, Ein SH, Connolly B, Daneman A, Filler RM. Unsuccessful air-enema reduction of intussusception: is a second attempt worthwhile? Pediatr Surg Int 1999;15:214–16 [DOI] [PubMed] [Google Scholar]
- 12.Saxton V, Katz M, Phelan E, Beasley SW. Intussusception: a repeat delayed gas enema increases the nonoperative reduction rate. J Pediatr Surg 1994;29:588–9 [DOI] [PubMed] [Google Scholar]
- 13.Fragoso AC, Campos M, Tavares C, Costa-Pereira A, Estevao-Costa J. Pneumatic reduction of childhood intussusception. Is prediction of failure important? J Pediatr Surg 2007;42:1504–8 [DOI] [PubMed] [Google Scholar]
- 14.Beasley SW. Best practice management of intussusception in rural centres: how to minimise morbidity and mortality. ANZ J Surg 2007;77:A74 [Google Scholar]
- 15.Fishman MC, Borden S, Cooper A. The dissection sign of nonreducible ileocolic intussusception. AJR Am J Roentgenol 1984;143:5–8 [DOI] [PubMed] [Google Scholar]
- 16.Henry MC, Breuer CK, Tashjian DB, Moss RL, McKee M, Touloukian R, et al. The appendix sign: a radiographic marker for irreducible intussusception. J Pediatr Surg 2006;41:487–9 [DOI] [PubMed] [Google Scholar]
- 17.Koh EP, Chua JH, Chui CH, Jacobsen AS. A report of 6 children with small bowel intussusception that required surgical intervention. J Pediatr Surg 2006;41:817–20 [DOI] [PubMed] [Google Scholar]
- 18.Jen HC, Shew SB. The impact of hospital type and experience on the operative utilization in pediatric intussusception: a nationwide study. J Pediatr Surg 2009;44:241–6 [DOI] [PubMed] [Google Scholar]
- 19.Chen WJ, Zhang HR, Liu JQ, Hu Y, Chen J, Yang F. [Ultrasonographic findings of intussusception complicated by intestinal necrosis in children.] Zhongguo Dang Dai Er Ke Za Zhi 2008;10:161–2 [PubMed] [Google Scholar]
- 20.Hedlund GL, Johnson JF, Strife JL. Ileocolic intussusception: extensive reflux of air preceding pneumatic reduction. Radiology 1990;174:187–9 [DOI] [PubMed] [Google Scholar]
- 21.Sorantin E, Lindbichler F. Management of intussusception. Eur Radiol 2004:14 Suppl. 4:L146–54 [DOI] [PubMed] [Google Scholar]
- 22.Raveenthiran V. Solar eclipse sign of intussusception on barium enema. Pediatr Surg Int 2002;18:79–80 [DOI] [PubMed] [Google Scholar]
- 23.Stranzinger E, Dipietro MA, Yarram S, Khalatbari S, Strouse PJ. Intramural and subserosal echogenic foci on US in large-bowel intussusceptions: prognostic indicator for reducibility? Pediatr Radiol 2009;39:42–6 [DOI] [PMC free article] [PubMed] [Google Scholar]