Abstract
Objective
This study evaluated the feasibility and safety of the transjugular intrahepatic portosystemic shunt (TIPS) procedure using the hepatic artery-targeting guidewire technique for the puncture step.
Methods
We retrospectively reviewed 11 consecutive patients (5 men and 6 women, aged 46–76 years (mean 64 years)) with portal hypertension in whom the TIPS procedure was performed. As the first step in the TIPS procedure in all cases, a micro-guidewire was inserted into the hepatic arterial branch accompanying the portal venous branch through a microcatheter coaxially advanced from a 5-French catheter positioned in the coeliac or common hepatic artery. At the puncture step, the tip of the metallic cannula was aimed 1 cm posterior to the distal part of this micro-guidewire, after which the TIPS procedure was performed. Success rate, number of punctures and complications were evaluated.
Results
The TIPS procedure was successfully performed in all 11 patients. The mean number of punctures until success in entering the targeted portal venous branch was 5 (range 1–14). In 3 patients (27%), the right portal venous branch was entered at the first puncture attempt. The hepatic artery was punctured once in one patient and the bile duct was punctured once in another patient. No serious procedure-induced complications occurred.
Conclusion
The TIPS procedure can be accomplished safely, precisely and relatively easily using the hepatic artery-targeting guidewire technique.
Transjugular intrahepatic portosystemic shunt (TIPS) placements have continued to increase since the first such procedure was performed in 1988 [1]. Currently, this procedure is accepted as an effective treatment for the complications of portal hypertension, such as variceal bleeding [2] and intractable ascites [2,3]. In many institutions, including ours, however, this procedure is rarely performed and it might be difficult to maintain the necessary skills.
During the TIPS procedure, the puncture from the proximal portion of the hepatic vein (usually a right hepatic vein) to the proximal portion of a branch of the intrahepatic portal vein (usually the right portal vein) is the most important and difficult step [1,2]. In 1994, Matsui et al [4] introduced a simple technique to assist in this puncture step. This technique was aided by a targeting guidewire in the hepatic arterial branch accompanying the portal venous branch to be punctured. To our knowledge, there has been no subsequent literature on the use of this simple technique, which we have adopted in our institution. This study evaluated the application of the hepatic artery-targeting guidewire technique for the puncture step of the TIPS procedure. We also assessed the occurrence of procedure-induced complications in order to clarify the value of this technique to inexperienced or infrequent operators such as those in our institution.
Methods and materials
Patients
Between January 2004 and July 2009, 11 consecutive patients (5 men and 6 women aged 46–76 years (mean 64 years)) with portal hypertension underwent the TIPS procedure at our institution. For these patients, the hepatic artery-targeting guidewire technique was utilised for the puncture step of the TIPS procedure.
Procedures
All procedures were performed after the patient provided written informed consent. The consent form included permission for the use of records, images and data for research purposes.
Immediately before the TIPS procedure, coeliac and superior mesenteric arteriography was performed via a 5-French catheter inserted from the femoral artery to delineate the portal vein and hepatic artery anatomy. A 0.016-inch guidewire was inserted through a micro-catheter coaxially advanced from the 5-French catheter positioned at the coeliac or common hepatic artery into the hepatic arterial branch accompanying the portal venous branch for which the puncture was planned.
After the right jugular vein was punctured under local anaesthesia, a Rösch–Uchida transjugular liver access set (Cook; Bloomington, IN) was used to catheterise the right (n = 10) or left (n = 1) hepatic vein and also to orientate and stabilise the needle for the puncture. Fluoroscopic images were rapidly obtained while the C-arm was rotated to different angles during screening to aid in directing the needle in the required direction. Meticulous care was taken to shorten the duration of each fluoroscopy session to minimise radiation dose. The tip of the 14-gauge metallic cannula was aimed 1 cm posterior to the distal part of the micro-guidewire inserted in the branch of the hepatic artery. In the majority of cases, contrast medium was not used during screening, but in some cases (n = 3) less than 3 ml of contrast medium was infused from the catheter to show the position of the needle tip clearly. A TIPS procedure was then performed either using the standard puncture technique, with devices included in the Rösch–Uchida transjugular liver access set (n = 9), or the coaxial needle puncture technique, using the thin-needle method as modified by Matsui et al [4] (n = 2). With the coaxial needle puncture technique, which is a modified puncture technique, a 21-gauge 70-cm-long percutaneous transhepatic cholangiography needle (inner diameter 0.018 inch; Hakko; Nagano, Japan), which was inside a 4-French, 60-cm-long Teflon dilator (inner diameter 0.035 inch; Hanako; Tokyo, Japan), was used in place of the 5-French catheter and trocar stylet, both of which are included in the Rösch–Uchida transjugular liver access set. Details of the rest of the TIPS procedure after a successful puncture have been described elsewhere [1,2,4]. Figure 1 shows an example of a TIPS that was created with assistance from the hepatic artery-targeting guidewire technique.
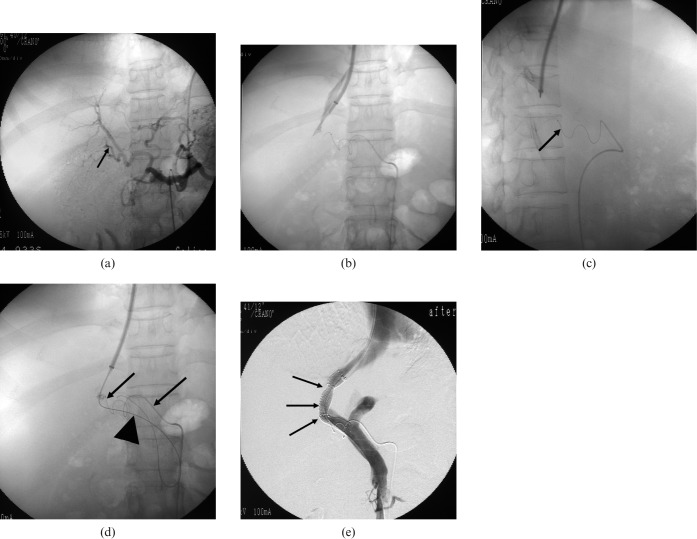
Figure 1.
(a) Coeliac arteriography shows all hepatic arterial branches. Note that the A7 hepatic arterial branch accompanies the portal venous branch (P5) that would be punctured (arrow). (b) Posteroanterior screening shows the tip of the 14-gauge curved metal cannula covered by a 10-French Teflon catheter advanced to the right hepatic vein. (c) Lateral-oblique screening shows that the tip of the cannula is directed 1 cm posterior to the tip of the target guidewire in the A7 hepatic arterial branch (arrow). (d) After success in puncturing the portal venous branch (P7), a guidewire (arrowhead) was advanced into the superior mesenteric vein through a 5-French catheter. Note that the micro-guidewire and micro-catheter for targeting is positioned in the right hepatic arterial branch (arrows). (e) Direct portography shows prompt blood flow from the portal vein to the hepatic vein through the transjugular intrahepatic portosystemic shunt tract (arrows) that has just been created. Sufficient patency of the TIPS tract remained on subsequent follow-up with images such as ultrasonography and computed tomography scan.
Parameters investigated
We collected data on the patients in whom the TIPS procedure with the hepatic artery-targeting guidewire technique was performed, the rate of success in the TIPS procedure and any complications related to the procedure.
Results
A TIPS procedure was successfully performed in all of the 11 patients (Table 1). The TIPS tract was created between the right hepatic vein and the right branch of the portal vein in all but one patient. In that patient, the TIPS tract was created between the left hepatic vein and the left branch of the portal vein after failure of the puncture between the right hepatic vein and the right branch of the portal vein. In three patients (27%), the right portal venous branch was entered on the first puncture attempt. Mean number of punctures until confirmation by immediate aspiration of portal venous blood and manual injection of contrast medium was 5 (range 1–14). The mean total duration of the procedure was 141 min (range 77–330 min).
Table 1. Transjugular intrahepatic portosystemic shunt procedures performed in 11 patients with portal hypertension.
| Case no. and sex (age in years) | Symptoms due to portal hypertension | Hepatic arterial branch into which tip of micro-catheter was inserted as target | Hepatic vein from which needle punctured | Number of punctures until successful cannulation into portal branch | Method of puncturing |
| 1. Female (67) | Intractable ascites | A8 | Right hepatic vein | 5 | Modified method |
| 2. Female (76) | Intractable ascites | A6 | Right hepatic vein | 8 | Modified method |
| 3. Male (61) | Oesophagogastric varices, intractable ascites | A8 | Right hepatic vein | 2 | Original method |
| 4. Male (46) | Intractable ascites | A7 | Right hepatic vein | 1 | Original method |
| 5. Female (69) | Duodenal varices | A8 | Right hepatic vein | 10 | Original method |
| 6. Female (76) | Oesophagogastric varices | A5 | Right hepatic vein | 3 | Original method |
| 7. Female (70) | Oesophagogastric varices, intractable ascites | A8 | Right hepatic vein | 10 | Original method |
| 8. Male (50) | Intractable ascites | A3 | Left hepatic vein | 5a | Original method |
| 9. Male (73) | Intractable ascites | A6 | Right hepatic vein | 1 | Original method |
| 10. Male (68) | Intractable ascites | A5 | Right hepatic vein | 14 | Original method |
| 11. Female (51) | Intractable ascites | A7 | Right hepatic vein | 1 | Original method |
aThe first four punctures were between the right hepatic vein and the right portal vein, all of which failed.
In one patient, the hepatic artery was punctured once during the procedure and in another patient the bile duct was punctured once during the procedure. In both of these patients, the fistula was so minor that it disappeared spontaneously, as demonstrated by hepatic arteriography, hepatic venography and direct portal venography while contrast medium was injected through the catheter advanced in the superior mesenteric vein after TIPS creation. No serious complications were induced by the procedure.
Discussion
Of the several steps in the TIPS procedure, transvenous access to the portal vein is by far the most crucial and, unfortunately, also the most unpredictable [4,5]. Attempts have been made to make this blind puncture more targeted in order to shorten the procedure time and enhance its safety.
A widely known technique to achieve this is the combined use of wedged hepatic venography for targeting the portal vein during TIPS [2,5]. In this method, after percutaneous access is obtained via an internal jugular vein, the right or middle hepatic vein from which the TIPS needle would make the puncture is cannulated. The position and patency of the portal vein are then confirmed by wedging a catheter into the hepatic vein and injecting carbon dioxide as a contrast medium to opacify the portal vein retrogradely. The reported rate of success in the visualisation of the portal vein with wedged hepatic venography is 87–91% [2,5,6]. Ideally, this rate could be improved.
If wedged venography fails, there are alternative techniques for portal vein localisation. On an anteroposterior projection, the mid right portal veins lie between the 10th and 12th posterior ribs in 87% of patients and the right portal trunks lie between 0.5 and 1.5 vertebral body widths lateral to the right margin of the spine in 90% of patients [7]. This knowledge enables the operator to pass the needle with some confidence using fluoroscopy alone [2]. The success in puncture using this technique is largely dependent on the experience of the operator. More invasive techniques include the use of a targeting guidewire or catheters inserted into the portal vein, placed via an enlarged umbilical vein or transhepatically [2,8]. This method is relatively invasive and should be avoided in patients with coagulopathy. The transhepatic approach should be avoided in patients who have ascites, which are occasionally seen in patients with portal hypertension [3].
In the present study, we evaluated 11 patients who received a TIPS in a procedure aided by a hepatic artery-targeting guidewire. This technique is a simple method based on the hepatic vascular anatomy in that the hepatic artery structures run close to the portal venous system in the liver [9]. Although the number of TIPS procedures performed in our institution in just over 5 years was low, 11 in all, the success rate was 100%. This suggests that this technique is helpful in successfully performing TIPS, despite lack of operator experience with the technique because of the small number of cases. This technique could be an additional alternative method when opacification of the portal vein fails retrogradely on wedged venography during a TIPS procedure. In addition, this technique can be used whether or not ascites exists.
Conclusion
The TIPS procedure can be accomplished safely, precisely and relatively easily with the aid of the hepatic artery-targeting guidewire technique.
References
- 1.Richter GM, Noldge G, Brado M, Scharf J, Simon C, Hansmann J, et al. TIPSS: 10 years of clinical experience. Rofo 1998;168:307–15 [DOI] [PubMed] [Google Scholar]
- 2.Owen AR, Stanley AJ, Vijayananthan A, Moss JG. The transjugular intrahepatic portosystemic shunt (TIPS). Clin Radiol 2009;64:664–74 [DOI] [PubMed] [Google Scholar]
- 3.Thalheimer U, Leandro G, Samonakis DN, Triantos CK, Senzolo M, Fung K, et al. TIPS for refractory ascites: a single-center experience. J Gastroenterol 2009;44:1089–95 [DOI] [PubMed] [Google Scholar]
- 4.Matsui O, Yoshikawa J, Kadoya M, Gabata T, Miyayama S, Takashima T. Transjugular intrahepatic portosystemic shunt after previous recanalization of a chronically thrombosed portal vein via a transmesenteric approach. Cardiovasc Intervent Radiol 1996;19:352–35 [DOI] [PubMed] [Google Scholar]
- 5.Krajina A, Lojik M, Chovanec V, Raupach J, Hulek P. Wedged hepatic venography for targeting the portal vein during TIPS: comparison of carbon dioxide and iodinated contrast agents. Cardiovasc Intervent Radiol 2002;25:171–5 [DOI] [PubMed] [Google Scholar]
- 6.Yang L, Bettmann MA. Identification of the portal vein: wedge hepatic venography with CO2 or iodinated contrast medium. Acad Radiol 1999;6:89–93 [DOI] [PubMed] [Google Scholar]
- 7.Darcy MD, Sterling KM. Comparison of portal vein anatomy and bony anatomic landmarks. Radiology 1996;200:707–10 [DOI] [PubMed] [Google Scholar]
- 8.Teitelbaum GP, Van Allan RJ, Reed RA, Hanks S, Katz MD. Portal venous branch targeting with a platinum-tipped wire to facilitate transjugular intrahepatic portosystemic shunt (TIPS) procedures. Cardiovasc Intervent Radiol 1993;16:198–200 [DOI] [PubMed] [Google Scholar]
- 9.Uflacker R. Hepatic veins and portal venous system. In: Uflacker R. Atlas of vascular anatomy. An angiographic approach. Baltimore, USA: Williams and Wilkins, 1997:639–44 [Google Scholar]