Abstract
We report the first case of extensive involvement of isolated intracranial Rosai-Dorfman's disease (RDD) in a child. Our case is unique because it presents with involvement of the middle cranial fossa, cavernous sinus, pituitary gland, orbit, ethmoid and sphenoid sinuses. Previous cases of intracranial RDD in children have reported separate involvement of cavernous sinus, suprasellar region, and frontal and petroclival regions. Involvement of the pituitary gland has so far not been reported. A 14-year-old male presented with a medical history of loss of vision, raised erythrocyte sedimentation rate (ESR), and abnormal prolactin and cortisol levels. Radiologically the diagnosis was meningioma. The histopathological diagnosis was RDD with emperipolesis and S-100 positivity. RDD is a histiocytic proliferation of unknown aetiology, which commonly affects lymph nodes. Uncommonly it involves the extranodal sites and rarely the central nervous system (CNS). 80 cases of RDD involving CNS have been reported in the literature, and only 5 were in children. Although the definitive diagnosis of RDD disease is based on the histopathology report, it should be included in the differentials of a lesion mimicking meningioma especially in children.
Rosai and Dorfman first described this rare disease entity in 1969 [1]. Since then only a few cases have been reported worldwide. RDD commonly affects the lymph nodes of young adults [2]. Although extranodal involvement is known to occur, isolated intracranial RDD is very rare. Out of 80 reported intracranial RDD cases, only 5 were in children [3-8].
We report a case of isolated intracranial RDD in a 14-year-old male mimicking meningioma. This extra-axial lesion was predominantly noted in the floor of the left middle and anterior cranial fossa with involvement of the sella turcica, orbit, ethmoid sinuses, sphenoid sinus and cavernous sinus, encasing the internal carotid artery. To our knowledge, this is the sixth case of intracranial RDD in the paediatric age group, and the first case with pituitary involvement in a child to be reported in the literature.
Although intracranial RDD mimics a meningioma, extensive involvement in a child should raise other possibilities. Histopathology and immunohistochemistry are needed to confirm diagnosis [2].
Case report
A 14-year-old male presented with progressive loss of vision in the left eye for the past 1 year. Vital signs were normal with no lymphadenopathy or hepatosplenomegaly. Laboratory investigations revealed increased erythrocyte sedimentation rate, T4, prolactin and cortisol levels. The rest of the routine haematological and biochemical studies were normal.
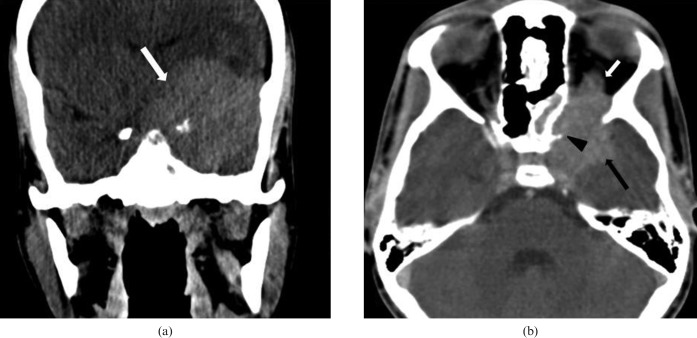
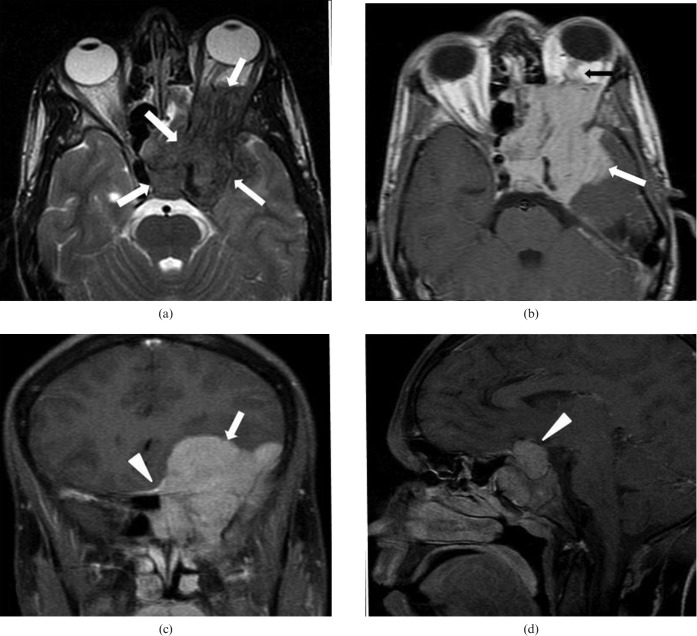
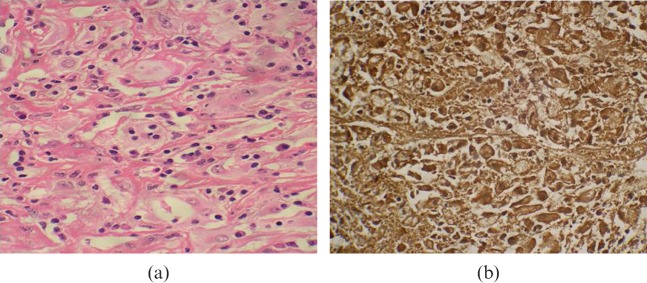
Coronal plain CT scan showed an extra-axial lesion which was relatively hyperdense, located in the left side of the skull base. No evidence of any calcification was noted within (Figure 1a). Axial T2 weighted MRI showed the lesion to be predominantly hypointense (Figure 1b). Mild peritumoural oedema was also noted (Figure 1b). On contrast administration the lesion showed homogeneous enhancement (Figure 2a–c). Destruction of the left sphenoid bone was noted with tumour extension into the left orbit causing buckling of the optic nerve and minimal proptosis. Bone erosion with tumour extension into the ipsilateral sphenoid and ethmoid sinuses was also noted (Figure 2a,b). Involvement of the left cavernous sinus encasing the left internal carotid artery was present (Figure 2b). Involvement of pituitary gland was also noted (Figure 2d). A dural tail was observed along the midline (Figure 2c). The radiological diagnosis was meningioma. The patient underwent left frontotemporal craniotomy and orbitotomy and subtotal decompression of the left middle cranial fossa mass. Pathological analysis revealed numerous histiocytes showing phagocytosed lymphocytes, plasma cells and red blood cells (emperipolesis). Immunohistochemistry for S-100 protein was strongly positive for the histiocytic cells (Figure 3a,b). Overall features were consistent with intracranial RDD.
Figure 1.
(a) Non-contrast coronal CT scan shows a homogeneously hyperdense extra-axial lesion (white arrow). (b) Contrast-enhanced axial CT scan shows a homogeneously enhancing extra-axial lesion (black arrow), with extension into the orbit (white arrow) and erosion of left sphenoid wing (black arrow head).
Figure 2.
(a) Axial T2 weighted MR image shows an extra-axial lesion hypointense to brain parenchyma (white arrows). (b) Gadolinium-enhanced axial T1 weighted MR image shows a homogeneously enhancing mass lesion (white arrow) with extension into the orbit causing buckling of the optic nerve (black arrow). (c) Gadolinium-enhanced fat-suppressed coronal T1 weighted MR image shows mass (white arrow) with dural tail along the midline (long arrowhead). (d) Gadolinium-enhanced fat-suppressed sagittal T1 weighted MR image showing involvement of the pituitary gland (long arrowhead).
Figure 3.
Paraffin section showing (a) histiocytes with emperipolesis (haematoxylin and eosin, ×400) with (b) immunopositivity for S-100 protein (avidin biotin complex immunoperoxidase method ×400).
Discussion
Rosai and Dorfman [1] first described a rare benign lymphoproliferative disorder in 1969, which was then known as sinus histiocytosis with massive lymphadenopathy, now primarily known as RDD. Although the pathogenesis is not clearly understood, some have proposed the role to be either infection or immunodeficiency [2]. RDD commonly involves cervical lymph nodes. Extranodal involvement is reported in up to 43% of cases of RDD involving paranasal sinuses, spine, orbit, skin and upper respiratory tract. Neurological involvement is rare and occurs in less than 5% of RDD patients [2]. Only 80 cases of RDD with CNS involvement have been reported in the literature [3].
Intracranial RDD predominantly affects males during their fourth or fifth decade [2]. To our knowledge only five paediatric cases of isolated intracranial RDD have been reported prior to the present case (Table 1).
Table 1. Summary of paediatric cases of isolated intracranial Rosai–Dorfman's disease.
| Author | Year | Gender | Age (years) | Site involved | Treatment | Follow-up |
| Shaver et al [4] | 1993 | M | 5 | Cavernous sinus | Surgery | Resolution post-surgery |
| Woodcook et al [5] | 1999 | F | 15 | Suprasellar | Biopsy, steroids | Slight interval increase in the residual lesion |
| Griffiths et al [6] | 2004 | M | 9 | Frontal | Surgery | No residual lesion |
| Gupta DK et al [7] | 2006 | M | 15 | Bilateral petroclival | Surgery | Residual tumour present |
| Lungren et al [8] | 2009 | F | 2 | Bilateral frontal | Surgery | Residual tumour present |
| Present case | 2009 | M | 14 | Cavernous sinus, orbit, sella, sphenoid and ethmoid sinus, middle fossa | Surgery | Residual component noted |
Presenting symptoms are usually focal deficits, seizures or headache owing to mass effect by the lesions. The typical imaging appearance of intracranial RDD is a dural-based enhancing mass mimicking meningioma [2,3]. Although it usually presents as a solitary lesion, multiple intracranial masses have also been reported [2]. Orbital involvement is rare and usually unilateral [9]. The common appearance is an infiltrative soft-tissue mass with variable contrast enhancement, as in our case. There may be extensive orbital involvement with pre-septal and post-septal or purely retrobulbar disease [9]. Suprasellar involvement is very rare and has been reported in six cases [2]. Although isolated involvement of cavernous sinus and suprasellar region has been reported in paediatrics by Shaver et al [4] and Woodcock et al [5], respectively, our case showed involvement of both cavernous sinus and suprasellar region with associated involvement of the orbit and pituitary gland. The abnormal levels of prolactin, cortisol and T4 are probably due to involvement of the adenohypophysis.
The differential diagnoses on imaging in our case include meningioma, metastasis, granulomatous infection like tuberculosis, lymphoma and Langerhans cell histiocytosis [5]. Extraxial location, homogeneously hyperdense on non-contrast CT scan, homogeneous enhancement on contrast administered scans and presence of dural tailing all suggest meningioma [10]. Signal intensities vary on T2 weighted imaging sequences depending on the histological type. Fibroblastic and the transitional variety of meningioms are usually hypointense to grey matter on T2 weighted imaging [11]. Intracranial RDD usually resembles meningioma on imaging and even intraoperatively. However, there are no histopathological similarities [2].
Histologically, sinus histiocytosis is characterised by nodal sinus dilatation with non-neoplastic proliferation of histiocytes. This histiocytic proliferation may cause effacement of normal nodal architecture and nodal capsular fibrosis. These histiocytes typically demonstrate a foamy eosinophilic cytoplasm and characteristically contain small, mature lymphocytes, known as lymphocytophagocytosis or emperipolesis. On immunohistochemistry, there is positive staining for S-100 [12].
Various treatment modalities such as surgery, steroids, chemotherapy and radiation therapy have been tried. Surgical resection has been found to be most effective [2,6,7]. However, in our case the lesion could not be resected completely owing to extensive involvement.
Conclusion
Although isolated intracranial RDD is a rare disease (especially in children), it should be included in the differential diagnosis of a dural-based mass mimicking meningioma in a child. Imaging modalities can help in characterisation and extent of the lesion, but histopathological examination and immunochemistry provides the definitive diagnosis.
References
- 1.Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy: a newly recognized benign clinicopathological entity. Arch Pathol 1969;87:63–70 [PubMed] [Google Scholar]
- 2.Wan S, Teng X, Zhan R, Yu J, Gu J, Zhang K. Isolated intracranial Rosai-Dorfman disease mimicking suprasellar meningioma: case repot with review of the literature. J Int Med Re 2008;36:1134–9 [DOI] [PubMed] [Google Scholar]
- 3.Theeler BJ, Keylock JB, Yoest SM. Teaching neuroimage: isolated intracranial Rosai-Dorfman disease mimicking a meningioma. Neurology 2008;70:e42. [DOI] [PubMed] [Google Scholar]
- 4.Shaver EG, Robsamem SL, Yachnis AT, Sutton LN. Isolated extranodal sinus histiocytosis in a 5 year old boy: a case report. J Neurosurg 1993;79:769–73 [DOI] [PubMed] [Google Scholar]
- 5.Woodcock R, Mandell J, Lipper M. Sinus histiocytosis (Rosai–Dorfman disease) of the suprasellar region: MR imaging findings—a case report. Radiology 1999;213:808–10 [DOI] [PubMed] [Google Scholar]
- 6.Griffiths SJ, Tang W, Parameswaran R, Kelsey, West CGH. Isolated intracranial Rosai Dorfman disease mimicking meningioma in a child. Br JNeurosurg 2004;18:293–7 [DOI] [PubMed] [Google Scholar]
- 7.Gupta DK, Suri A, Mahapatra AK, Mehta VS, Garg A, Sarkar C, et al. Intracranial Rosai–Dorfman disease in a child mimicking bilateral giant petroclival meningiomas: a case report and review of literature. Childs Nerv Syst 2006;22:1194–200 [DOI] [PubMed] [Google Scholar]
- 8.Lungren MP, Petrella JR, Cummings GA. Isolated Intracranial Rosai-Dorfman disease in a child. AJNR 2009;30:e148–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang E, Anzani Y, Paulino A, Wong J. Rosai–Dorfman disease presenting with bilateral orbital masses: report of two cases. AJNR 2001;22:1386–8 [PMC free article] [PubMed] [Google Scholar]
- 10.Buetow MP, Buetow PC, Smirniotopoulos JG. Typical, atypical and misleading features of Meningioma. RadioGraphics 1991;11:1087–106 [DOI] [PubMed] [Google Scholar]
- 11.Elster AD, Challa VR, Gilbert TH, Richardson DN, Contento JC. Meningiomas: MR and histopathologic features. Radiology 1989;170:857–62 [DOI] [PubMed] [Google Scholar]
- 12.Andriko JAW, Morrison A, Colegial CH, Davis BJ, Jones RV. Rosai-Dorfman disease isolated to the central nervous system: a report of 11 Cases. Mod Pathol 2001;14:172–8 [DOI] [PubMed] [Google Scholar]