Abstract
The aim of this study was to present the simplified rules of delineation of lymph node (LN) volumes in breast irradiation. Practical rules of delineation of LN areas were developed in the Department of Radiation Oncology of the Institut Curie. These practical guidelines of delineation were based on different specific publications in the field of breast and LN anatomy. The principal characteristic of these rules is their clearly established relationship with anatomical structure, which is easy to find on CT slices. The simplified rules of delineation have been published in pocket format as the illustrated atlas “Help of delineation for breast cancer treatment”. In this small pocket guide, delineation using the practical rules is illustrated, with examples from anatomical CT slices. It is shown that there is an improvement in delineation after the use of these simplified rules and the guide. In conclusion, this small guide is useful for improving everyday practice and decreasing the differences in target delineation for breast irradiation between institutions and observers.
The value of lymph node irradiation has already been demonstrated by various studies and meta-analyses [1–3]. In the age of new conformal techniques, there is a real need for a clear definition of treated volumes, such as breast, tumour bed, lymph node areas and organs at risk (OAR) [4–10]. Many teams have been working for several years on the definition of treated volumes. Some delineation studies are exclusively theoretical and some provide a good anatomical atlas, but this information is difficult to use in everyday practice [4–15]. The treatment position has also been shown to be an important factor of variability in the depth and situation of lymph node volumes [5, 6]. Conformal and intensity-modulated radiotherapy (IMRT) require an exact definition of target volumes in terms of their anatomical limits for delineation on CT scans. Some authors have proposed anatomically based landmarks specific for breast cancer radiotherapy in order to delineate all regional lymph nodes and the breast [5, 6, 8, 10, 15, 16]. Despite this work, two recent papers have demonstrated the individual interobserver variability and differences in target and OAR delineation for breast irradiation, especially in lymph node areas [7, 8].
This study was designed to propose a practical method to improve and facilitate the everyday delineation process for the clinicians of our department.
Methods and materials
Lymph node anatomy was studied [4, 5, 10–15]. Three anatomical studies conducted in our department initially examined vessels such as the internal mammary artery, individual characteristics and the importance of the patient's position [6]. We then went on to investigate interobserver differences in delineation [8], followed by the definition of simplified rules for everyday delineation [16]. Simplified guidelines for lymph node and breast delineation and for the delineation of OAR, brachial plexus and so on were prepared.
Three CT scans of patients in the treatment position were delineated by different physicians. These delineations were initially compared using classic statistical methods and then using Aquilab Software (Lille, France) to evaluate interobserver differences. Despite the exact description of lymph node regions in high-quality papers [4, 5, 10], some physicians experience difficulties in the delineation process. We therefore tried to simplify this process and develop practical guidelines for delineation based not only on various specific publications in the field of breast and lymph node anatomy, but also on our experience following discussions between surgeons, radiologists and radiation oncologists.
We set out to evaluate anatomical findings, together with surgical and radiological opinions, and to define structures that are easy to identify on unenhanced CT scans in the treatment position. Our key aim was not to develop a new anatomical atlas, but instead to define useful everyday guidelines for delineation.
Results
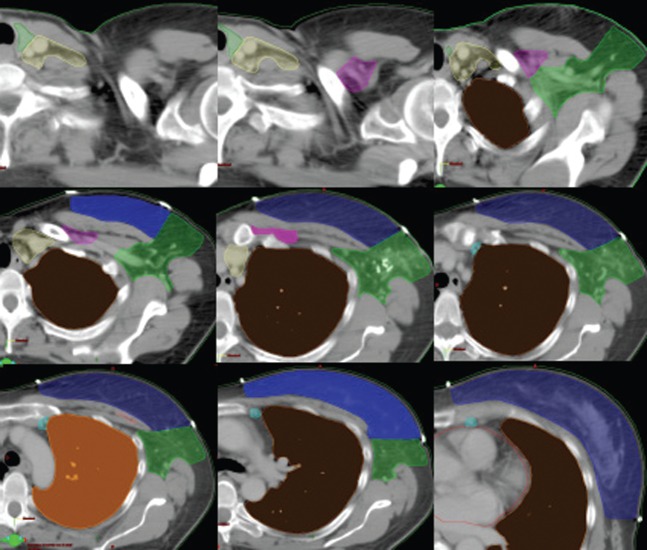
After two years' work on volume definition in breast cancer treatment, the simplified rules were published in pocket format as an illustrated atlas called “Guide to delineation for breast cancer treatment” (Figure 1). This booklet weighs 5 g and contains seven pages with pictures and explanations, as shown in Figures 1 and 2. This small pocket guide illustrates examples of delineation on anatomical CT slices using the simplified practical rules shown in Figure 1. The booklet has now been in use for two years. This guide was validated in routine practice by new residents, who were asked to delineate according to the guidelines published in the literature; they then received a training course and a copy of the pocket guide. Figure 3 presents an example of delineation before and after the use of these simplified rules for contouring of axillary volumes performed by the same residents. As previously reported, these anatomy refresher courses are beneficial. This free small guide is given not only to residents in training, but also to radiation oncologists specialised in breast radiotherapy and to radiation physicists in order to improve everyday practice and decrease the differences in target delineation for breast irradiation between radiation oncologists. This simple action, designed to improve the quality of delineation in our department, seems to be useful and very well accepted.
Figure 1.
Examples of delineation shown in the guide and simplified rules of delineation.
Supraclavicular region: contouring of the supraclavicular region is guided by the origin of the internal mammary artery.
Cranial: Thyroid cartilage
Caudal: Clavicular head
Medial (med): Trachea
Posterior (post)-lateral (lat): Anterior scalene muscle
Post-med: Carotid artery
Infra clavicular region: The infraclavicular region corresponds to the lymphatic drainage between axillary vertex, and the superior limit of the axillary LN dissection (LND).
Cranial: Pectoralis minor
Caudal: Sternoclavicular joint
Lat: Pectoralis minor (medial side)
Med: Clavicle
Ant: Pectoralis major
Post: Axillary artery
Internal mammary chain: The lymph nodes of the IMC are located within the anterior interspaces; they are located either medial or lateral to the vessels and are concentrated in the upper three interspaces.
Ant: Ant. part of the vascular area
Post: The pleura
Med: Medial limit of the vascular area
Lat: Lateral limit of the vascular area
Caudal: Superior side of the fourth rib
Cranial: Inferior limit of supraclavicular area
Rotter LN or intra pectoral node: situated between: pectoralis major and pectoralis minor at the second intercostal space
Axilla:
Ant: Pectoralis major and pectoralis minor
Post: Subscapularis, teres major and latissimus dorsi
Med: Seratus anteriorLat: 5 mm backward the skin
Caudal: fourth and fifth ribs
Cranial: Inferior limit of infraclavicular volume or “first clip”
Figure 2.
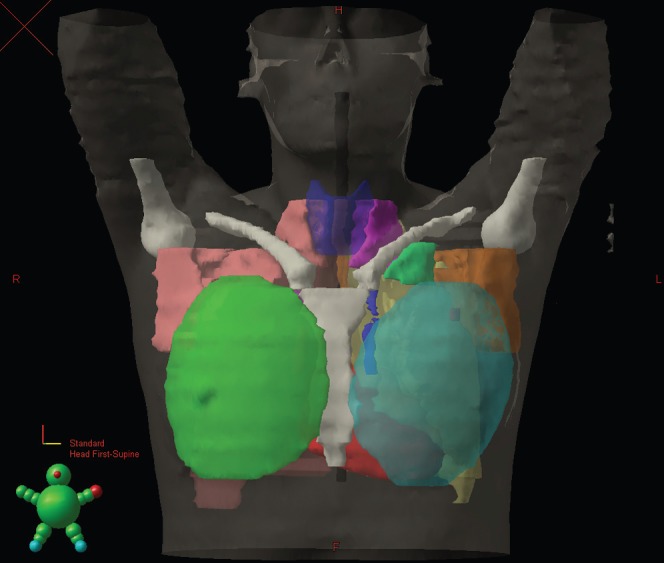
The final result of delineation with 3D volume reconstruction using Eclipse TPS of volumes delineated using the simplified rules.Supraclavicular region (fuchsia)Infraclavicular region (green)Internal mammary chain (dark blue)Rotter LN or intrapectoral node (red)Axilla (yellow-ochre)Brachial plexus is shown in yellow, thyroid in dark blue, bones in white, heart in red.
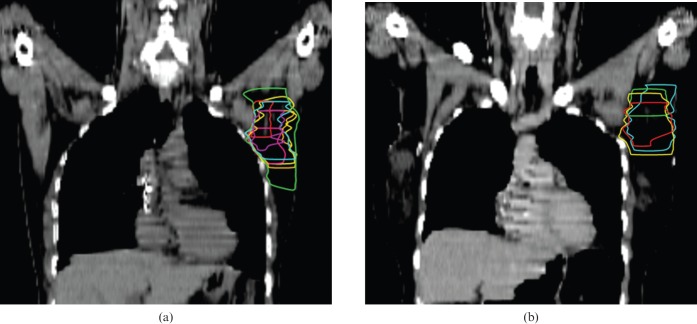
Figure 3.
Practical example of axillary delineation before and after continuing medical education (CME) and using the simplified practical rules: “how to delineate the lymph node areas?”. (a) Before training; (b) after training.
Discussion
The guide is an example of practical use of all information concerning the patient's anatomy, a review of the literature and practical experience in collaboration with surgeons and radiologists.
Many interesting and high-quality papers have been published in the specialised literature over recent years [4–6, 10, 14, 15]. Despite these interesting studies, two recent papers have highlighted the interobserver variability and differences in target and OAR delineation for breast irradiation, especially in lymph node areas [7, 8]. Pena et al [8] studied delineation differences in breast and lymph node volumes between radiation oncologists in the same department. After delineation exercises, comparative analysis and continuing medical education (CME) meetings, the authors concluded that written delineation protocols and training courses need to be developed. Li et al [9] compared independent target delineation by nine radiation oncologists specialised in breast radiotherapy from eight different institutions and found substantial variability in terms of target and OAR contouring between institutions and between observers. These interobserver differences resulted in substantial variations in dosimetric planning for breast radiotherapy [9]. The authors concluded that a systematic consensus is highly desirable, particularly in the age of intensity-modulated and image-guided radiotherapy, with a need for an atlas.
The proposed guide described in our paper is not an extensive anatomical atlas with exact definition of lymph node areas in relation to lymph node invasion [3]. It may not be perfect, but it is a useful tool to improve the everyday delineation process. In conclusion, more atlases and written recommendations need to move from articles and books to the physician′s pocket in order to improve everyday practice.
Acknowledgments
We thank AstraZeneca (France), who supported the publication and distribution of this pocket delineation guide, and Aquilab (France), who helped us to address the issue of interobserver variability of delineation.
Footnotes
This work was presented in part at the ESTRO Advanced Course of breast cancer treatment, Lisbon, Portugal 2009.
References
- 1.Early BreastCancerTrialistsCollaborativeGroup(EBCTCG) effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;366:2087–106 [DOI] [PubMed] [Google Scholar]
- 2.Kyndi M, Overgaard M, Nielsen HM, Sørensen FB, Knudsen H, Overgaard J. High local recurrence risk is not associated with large survival reduction after postmastectomy radiotherapy in high-risk breast cancer: a subgroup analysis of DBCG 82 b&c. Radiother Oncol 2009;90:74–9 [DOI] [PubMed] [Google Scholar]
- 3.Chang DT, Feigenberg SJ, Indelicato DJ, Morris CG, Lightsey J, Grobmyer SR, et al. Long-term outcomes in breast cancer patients with ten or more positive axillary nodes treated with combined-modality therapy: the importance of radiation field selection. Int J Radiat Oncol Biol Phys 2007;67:1043–51 [DOI] [PubMed] [Google Scholar]
- 4.Kiricuta IC, Götz U, Schwab F, Fehn M, Neumann HH. Target volume definition and target conformal irradiation technique for breast cancer patients. Acta Oncol 2000;39:429–36 [DOI] [PubMed] [Google Scholar]
- 5.Dijkema IM, Hofman P, Raaijmakers CP, Lagendijk JJ, Battermann JJ, Hillen B. Loco-regional conformal radiotherapy of the breast: delineation of the regional lymph node clinical target volumes in treatment position. Radiother Oncol 2004;71:287–95 [DOI] [PubMed] [Google Scholar]
- 6.Kirova YM, Servois V, Campana F, Dendale R, Bollet MA, Laki F, et al. CT-scan based localization of the internal mammary chain and supra clavicular nodes for breast cancer radiation therapy planning. Radiother Oncol 2006;79:310–15 [DOI] [PubMed] [Google Scholar]
- 7.Kirova YM, Fournier-Bidoz N, Servois V, Laki F, Pollet GA, Salmon R, et al. How to boost the breast tumor bed? A multidisciplinary approach in eight steps. Int J Radiat Oncol Biol Phys 2008;72:494–500 [DOI] [PubMed] [Google Scholar]
- 8.Castro Pena P, Kirova YM, Campana F, Dendale R, Bollet MA, Fournier-Bidoz N, Fourquet A. Anatomical, clinical and radiological delineation of target volumes in breast cancer radiotherapy planning: individual variability, questions and answers. Br J Radiol 2009;82:595–9 [DOI] [PubMed] [Google Scholar]
- 9.Li XA, Tai A, Arthur DW, Buchholz TA, Macdonald S, Marks LB, et al. Variability of target and normal structure delineation for breast cancer radiotherapy: an RTOG multi-institutional and multiobserver study. Int J Radiat Oncol Biol Phys 2009;73:944–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martinez-Monge R, Fernandes PS, Gupta N, Gahbauer R. Cross-sectional nodal atlas: a tool for the definition of clinical target volumes in 3D radiation therapy planning. Radiology 1999;211:815–28 [DOI] [PubMed] [Google Scholar]
- 11.Scatarige JC, Hamper UM, Sheth S, Allen HA., 3rd Parasternal sonography of the internal mammary vessels: technique, normal anatomy, and lymphadenopathy. Thoracic Radiology 1989;172:453–7 [DOI] [PubMed] [Google Scholar]
- 12.Ege GN. Internal mammary lymphoscintigraphy. Radiology 1976;118:101–17 [DOI] [PubMed] [Google Scholar]
- 13.Freedman GM, Fowble BL, Nicolaou N, Sigurdson ER, Torosian MH, Boraas MC, et al. Should internal mammary lymph nodes in breast cancer be a target for the radiation oncologist? Int J Radiat Oncol Biol Phys 2000;46:805–14 [DOI] [PubMed] [Google Scholar]
- 14.Lengelé B, Nyssen-Behets C, Scalliet P. Anatomical bases for the radiological delineation of lymph node areas. Upper limbs, chest and abdomen. Radiother Oncol 2007;84:335–47 [DOI] [PubMed] [Google Scholar]
- 15.Madu CN, Quint DJ, Normolle DP, Marsh RB, Wang EY, Pierce LJ. Definition of the supraclavicular and infraclavicular nodes: implications for three-dimensional CT-based conformal radiation therapy. Radiology 2001;221:333–9 [DOI] [PubMed] [Google Scholar]
- 16.Kirova YM, Castro Pena P, Dendale R, Bollet MA, Fournier-Bidoz N, Fourquet A. Definition of nodal volumes in breast cancer treatment and segmentation guidelines. J Radiol 2009; 90747–51 [DOI] [PubMed] [Google Scholar]