Abstract
The purpose of this study was to assess the success of neurolinguistic programming in reducing the need for general anaesthesia in claustrophobic patients who require MRI and to consider the financial implications for health providers. This was a prospective study performed in 2006 and 2007 at a teaching hospital in England and comprised 50 adults who had unsuccessful MR examinations because of claustrophobia. The main outcome measures were the ability to tolerate a successful MR examination after neurolinguistic programming, the reduction of median anxiety scores produced by neurolinguistic programming, and models of costs for various imaging pathways. Neurolinguistic programming allowed 38/50 people (76%) to complete the MR examination successfully. Overall, the median anxiety score was significantly reduced following the session of neurolinguistic programming. In conclusion, neurolinguistic programming reduced anxiety and subsequently allowed MRI to be performed without resorting to general anaesthesia in a high proportion of claustrophobic adults. If these results are reproducible, there will be major advantages in terms of patient safety and costs.
Over the first 15 year period (1989–2003) of performing MRI for clinical indications in Sheffield, we observed a failure rate of approximately 3% because of patient claustrophobia. Currently, the failure rate is approximately 1.0–1.5%, with the improvement probably arising from improved magnetic design producing smaller scanners that appear less daunting for the patients [1]. Despite this, our present workload levels produce three scan failures per week because of claustrophobia. Some studies have shown that over 14% of patients require some form of sedation in order to tolerate MRI [2], and 37% of patients report moderate to high levels of anxiety brought about by the procedure [3]. This is usually in the form of feelings of isolation and threat to self-control [4].
Claustrophobia is common during MR scanning because of the enclosed nature of cylindrical whole-body MR scanners. In our experience, this is exacerbated further by the use of surface coils, particularly when imaging the head and neck, even though one study claims that the level of anxiety is unrelated to the use of surface coils [5]. The specific features that patients find most distressing are the spatial restriction, temperature, duration and the acoustic noise [6]. When a patient undergoes an unsuccessful MR examination, the clinical team must decide if the information can be gained from another procedure; however, in many cases, it is necessary to repeat the MR scan using sedation or general anaesthesia (GA). Local policy dictates that this may be administered only by an anaesthetist to ensure that no patient comes to harm during the diagnostic procedure [7]. Frequently, it is judged that sedation will not be sufficient and the claustrophobic patient will request to be “asleep” for the procedure. We perform approximately 150 MR procedures under GA per annum (excluding children) in a region that provides an MR service to approximately 1.5 million people. Those cases require substantial resources in terms of staff, scanner time and day care facilities. The small but finite risk of complications from the anaesthetic can also not be ignored [8].
It is a justifiable goal, therefore, to explore methods that could reduce the need for GA requirements for MRI. The purpose of this study is to evaluate the use of neurolinguistic programming (NLP) as a method to reduce anxiety in patients who have failed MR examinations because of claustrophobia to a level that allows them to remain in the scanner long enough to complete the examination.
Methods
Study design and population
The overall goal was to study 50 people who had failed a previous MR examination because of subjective claustrophobia. Patients who were unable to fully communicate verbally with the NLP practitioner (e.g. foreign language users, speech- or hearing-impaired patients) were not approached about the study. The anticipated success rate was a conservative estimate following discussion with NLP experts (H.L.) who predicted it would be far in excess of 60%.
Patients who had failed an MR examination were contacted by telephone and invited to take part in the study by the NLP-trained radiographer (J.B.). Those who agreed attended the MR department at the Sheffield Teaching Hospitals or at the University of Sheffield. 58 patients were approached and 8 declined, all of whom subsequently underwent an MR study under general anaesthesia. The 50 patients (24 males and 26 females) who agreed to enter the study had a median age of 52 years with a range of 58 years (17–75 years). A wide variety of body areas were planned to be imaged, and the expected duration of the scans was between 20 min and 30 min. The patient's level of anxiety was assessed by a questionnaire based on Spielberger's State–Trait Anxiety Inventory [9]. This was assessed on two occasions: (i) on the same day as NLP and (ii) after NLP but before the MR scan. A background to the principles of NLP is given in the discussion section but an outline of the methods used in the study is given here.
An MR radiographer (J.B.) underwent training in the fundamentals of NLP by way of an NLP practitioner course (accredited by the International NLP Trainers Association). The total training consisted of 20 days spread over a 6 month period. The main NLP technique used on our patients was “Clare's fast phobia cure” for phobias of unknown origin (adapted from Rushworth [10]), which has been used successfully to cure phobias [11]. The “Clare's fast phobia cure” process was developed by Clare Rushworth whilst working in the field of cancer care for neutralising phobias of unknown origin. It is a specific application of a collapsing anchors process, whereby an unresourceful anchor response to a particular stimulus is replaced by a more resourceful one. This process involves identifying the precise trigger for the unresourceful response. A visual anchor is created for the trigger (this may vary from person to person) and the precise “antidote” resources are selected (these too may vary from person to person). A positive stacked anchor containing multiple resources is created kinaesthetically by precise timed touch. The two anchors are fired simultaneously and held until the integration of the two states is complete. In brief, the patient was asked to describe the feelings they experience when they think about an MR scan. They were asked to associate (anchor) those feelings with something that they could see in the room. The patient was then asked to think about pleasant memories on other occasions when they were relaxed, happy or confident. As the patient thought about the good experiences, the NLP practitioner touched them on the hand or shoulder, thus anchoring the experience. By using the same touch and simultaneously looking at the object that they had chosen and holding both anchors until the previously phobic anchor has been “collapsed”, the previously anxious thoughts associated with MRI can become much more comfortable and positive. The main differences to a straight collapsing anchor are: two different systems are being used for the anchors (visual and kinaesthetic), a precise trigger for the phobic response is identified and then anchored, a precise and ecological mix of “antidote” states for the resource anchor is selected and a very powerful resource anchor is stacked with multiple resources. The amount of time that the NLP radiographer spent working with each patient before the scan varied depending on the patient's needs, but was usually in the order of 1 h.
Clinical outcome measures and statistical analysis
The success of the NLP was determined primarily by the success of the MRI procedure. The following assessment criteria were used:
1. Did the patient manage to have a complete examination?
2. Were the images adequate for clinical reporting as judged by a consultant radiologist not directly involved in the study?
3. Had the individual's anxiety levels reduced after the NLP counselling?
The primary analysis was simple proportion assessments for Criteria 1 and 2, whereas non-parametric statistics (Mann–Whitney test) were used to compare the changes in anxiety scores between patients who had successful MR examinations and those who had failed. A significance value of p<0.05 was used.
Financial considerations
An attempt was made to study the financial aspects of the study if they were applied to the general population. The unit costs of MR under general anaesthesia at our institution and the costs of applying NLP to a non-GA case were calculated as shown in Table 1. A financial model was created based on the associated costs in relation to the observed success rate of NLP.
Table 1. Breakdown of costs associated with GA examinations and non-GA examinations supplemented by NLP.
| General anaesthetic costs per patient | |
| Operating department practitioner | £22 |
| Recovery | £19 |
| Maintenance/preparation etc. | £10 |
| Anaesthetist | £95 |
| Anaesthesia and drugs | £40 |
| MRI scana | £302 |
| Total cost per patient of an MR under GA | £488 |
| Costs of non-GA MR examinations supplemented by NLP per patient | |
| Cost of NLP practitioner time (1 h) | £18 |
| Cost of non-GA MRI scana | £151 |
| Total cost for non-GA scan | £169 |
aThe Government 2007–08 Indicative Tariff to support Unbundling of Diagnostics puts the cost of a single MRI examination without contrast (RA MR1) at £151. On average, it would normally be possible to carry out two MRI examinations in the scanner time that it takes to carry out one under general anaesthesia (GA). It can therefore be assumed that this doubles the cost of a scan under anaesthetic to £302.
The GA-related costs are made on the assumption of four patients being scanned in a 4 h session. The overall difference in the unit cost of a GA and non-GA examination supplemented with neurolinguistic programming (NLP) is £319.
Ethics
This study was performed under the guidance and with the approval of Barnsley Research Ethics Committee, Ref. No: 06/Q2304/33. Written consent was obtained from all subjects after full explanation of the procedures.
Results
The 50 patients recruited into the study came from a group of 58 patients approached (eight did not agree to enter the study). Of the 50 patients who were recruited, 38 (76%) completed the MR examination and all of those examinations were of sufficient quality for clinical reporting. MR examinations were not completed in 12/50 patients (24%), including three who would not consider going onto the scanner and nine who went on the scanner bed but for whom no usable images were obtained.
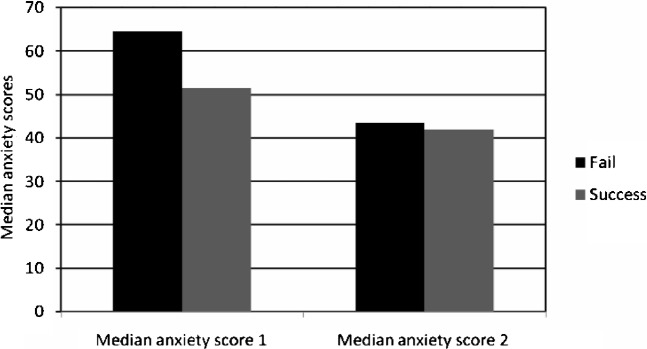
The data concerning anxiety levels are presented in Figure 1. When all patients are considered, there was a statistically significant reduction in anxiety following NLP. The 12 patients who subsequently failed to undergo the MR examination had statistically higher anxiety scores before NLP than the patients who tolerated the MRI (p _ 0.034, <0.05). After NLP, there was a significant reduction in anxiety scores in both “fail” and “succeed” groups, but the scale of the reduction between the two groups did not reach statistical significance. (p _ 0.172).
Figure 1.
Histograms of median anxiety scores before neurolinguistic programming (NLP) (left) and after NLP (right) in patients who subsequently had a successful MR (light grey) and those who failed (dark grey).
The success rate of the NLP process was studied further by looking at any potential effects in performance of the NLP practitioner as a result of increasing experience during the study. A graph of the success rate of NLP plotted against sequential groups of 10 patients is shown in Figure 2. This appears to show a considerable “experience” effect, as a consistent success rate of 90% was achieved for the last 30 patients as opposed to 30% for the first 10 patients.
Figure 2.
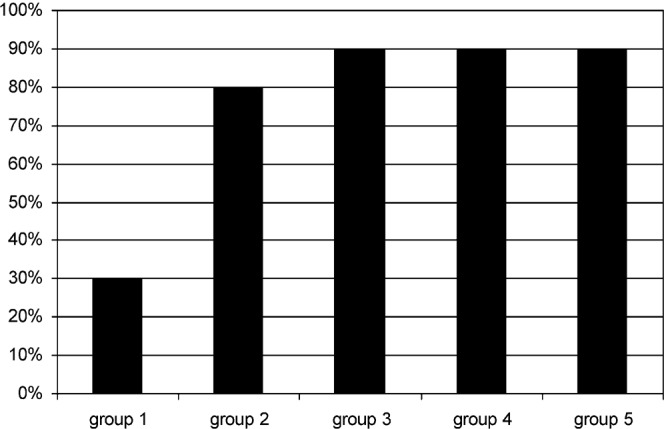
Success rates of neurolinguistic programming (NLP) in relation to sequential groups of 10 patients.
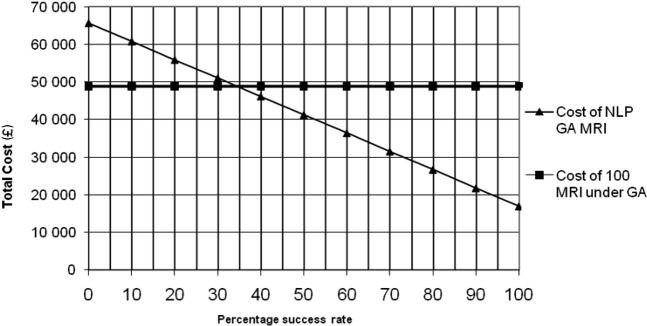
The overall cost of an MR examination under GA at our institution was calculated at £488, whereas the cost of standard MRI supplemented by an NLP practitioner was calculated at £169 (excluding the one-off cost of training at £1750). Figure 3 shows the sensitivity analysis of costs for 100 patients plotted against the NLP success rate. If NLP was successful in all cases, there would be an overall saving of £31 900 (65%), using the costs calculated for our department. If NLP was not successful in any patient, the costs would increase by £16 900 (35%) because the GA would be required as well as the NLP procedure. The financial breakeven point occurs at an NLP success rate of 35%. If our finding of a 76% success rate is generally applicable, we estimate an overall saving of £20 188 per 100 patients (a 41% saving overall).
Figure 3.
Sensitivity analysis of total costs for 100 patients against the percentage success rate of neurolinguistic programming (NLP). The horizontal line represents the costs if all patients with claustrophobia went directly to MR under general anaesthesia (GA). The sloping line represents total costs in relation to the percentage success rate of NLP. The financial breakeven point occurs if 35% of NLP cases are successful. At the current success rate of 76% there is an overall saving of £20 188 (41%).
Discussion
MRI is now the investigation of choice for a wide range of pathologies. There has been a major increase in the number of MR scanners in hospitals over the past few years, and the improved specifications of the scanners has increased patient throughput. As a result, a large number of patients undergo MR procedures and, in our experience, 1.0–1.5% of these patients will have claustrophobia to a level that prevents diagnostic imaging. GA is currently the main method for overcoming these problems at many institutions, despite the issues of patient safety, cost and availability. The increasing number of patients requiring GA has other deleterious effects on patient throughput and imaging targets for waiting times, as a smaller number of people can be scanned per unit time under GA. Any method, therefore, that can be used to reduce GA rates without using extra MR time is very attractive, and our current work with NLP shows great promise (Table 2).
Table 2. Summary of topic and results.
| What is already known on this topic? |
| MRI can be difficult for patients for many reasons |
| Claustrophobia is common during MRI and results in scan failure in at least 1% of cases |
| In such cases, many patients need to have the examination under general anaesthesia |
| What this study adds |
| Neurolinguistic programming can be used to help patients cope with MR scanning without recourse to general anaesthesia |
| Our success rate is 76% in a study group of 50 claustrophobic patients |
| If these results are generally applicable, there are major advantages to patient care in terms of safety and cost |
NLP was first introduced in the 1970s by Richard Bandler, an information scientist and mathematician, and John Grinder, a professor of linguistics. Their studies involved people who were excellent communicators and counsellors, and their results produced a model of human experience and communication that has been refined and expanded in subsequent years and used in many situations [12–14]. NLP recognises the influence of language, both internal and external, on behaviour and gathers both verbal and non-verbal information in order to study subjective experience. NLP allows us to recognise and enable change in less useful patterns of behaviour that were learnt previously but which are continually repeated [15, 16].
In our study, we found that 76% of patients who had previously failed an MR scan successfully completed a scan following the NLP intervention, although it should be appreciated that 8 of the 58 people approached refused to attempt NLP. A statistically significant reduction in anxiety levels was achieved in our patient group by NLP, even in those who went on to fail to complete the MR scan. Each patient had highly individualised anxieties that required a flexible approach and a wide range of NLP techniques to be used. As NLP principles would predict, simply using one technique in a “one size fits all” procedure is often not effective. Indeed, the “Clare's fast phobia cure” alone was probably not sufficient in many instances, as some individuals required specific work on neutralising previous experiences in which their phobia had a specific origin. Others required pacing and leading and the specific influencing and reassurance of certain language patterns. This resulted in the NLP practitioner being in the MR scanner room in over 60% of cases, which allowed continued use of NLP if the patient began to show a return to his/her anxious state. A radiographer does not stay with the patient in the scan room normally.
This raises two issues. First, it is possible (and indeed likely) that this introduced an important confounding factor. Consideration must be given to the possibility that additional time spent with the patient and the presence of a radiographer in the scan room contributed to the success of completing the MR examination [4]. Previous research comparing the effects of information, counselling and relaxation techniques on patients undergoing MRI, however, has not shown significant reductions in anxiety levels [17]. This confounding factor will need to be investigated in future studies. The second issue is a proposed EU directive on workers exposed to electromagnetic fields (Directive 2008/46/EC) [18]. This would outlaw staff remaining in the scan room while imaging is performed. The outcome of that proposed legislation is not known at present but potentially could have a major impact on the future role of studies such as ours.
It is also possible that the type of scanner used could have an effect on the overall failure rate [1]. Our work was performed on two different manufacturers' systems but they were both cylindrical 1.5 T superconducting systems. Our initial analysis does not show any apparent difference between the types of scanner used, but this would need to be confirmed by further research involving greater numbers of patients. It is assumed that the use of an “open” MR scanner would have a significant improvement on claustrophobia failure rates. It has been shown that 84% of patients who had previously failed an examination on a cylindrical system were able to tolerate a scan on an open system [19]. These systems are relatively rare and, because most operate at low field strength, image quality is often compromised.
In the current climate of tight budgets and waiting list pressures, there is always a search for new and innovative ways of cutting costs. The cost of training a radiographer to be an NLP practitioner is approximately £1750 at the time of writing. The NLP practitioner spends approximately 1 h with each patient before the scan at a cost of £18 per hour. The cost difference between an MR scan with and without GA is calculated to be £319 (Table 1). When the cost of the practitioner's time is taken into account, the breakeven point of offering an NLP service to patients is calculated to be a success rate of 35% (Figure 3). Assuming that all of the patients who fail to undergo an MRI scan go on to have GA with a success rate of 76% (as per our study), the 41% (£20 188) cost saving is a significant one.
Conclusions
In summary, we have shown that the use of NLP in patients who fail to tolerate MRI can greatly reduce the need for a repeat examination under GA. The positive effects of this are greater patient safety and reduced costs.
Footnotes
J.B. and P.D.G contributed equally to the study.
References
- 1.Dewey M, Schink T, Dewey CF. Claustrophobia during Magnetic Resonance imaging: Cohort study in over 55,000 patients. J Magn Reson Imaging 2007;26:1322–7 [DOI] [PubMed] [Google Scholar]
- 2.Murphy KJ, Brunberg JA. Adult claustrophobia, anxiety and sedation in MRI. Magn Reson Imaging 1997;15:51–4 [DOI] [PubMed] [Google Scholar]
- 3.Katz RC, Wilson L, Frazer N. Anxiety and its determinants in patients undergoing magnetic resonance imaging. J Behav Ther Exp Psychiatry 1994;25:131–4 [DOI] [PubMed] [Google Scholar]
- 4.Tornqvist E, Mansson A, Larsson EM, Hallstrom I. It's like being in another world-patients' lived experience of magnetic resonance imaging. J Clin Nurs 2006;15:954–61 [DOI] [PubMed] [Google Scholar]
- 5.Thorpe S, Salkovskis PM, Dittner A. Claustrophobia in MRI: the role of cognitions. Magn Reson Imaging 2008;26:1081–8 [DOI] [PubMed] [Google Scholar]
- 6.Quirk ME, Letendre AJ, Ciottone RA, Lingley JF. Anxiety in patients undergoing MR imaging. Radiology 1989;170:463–6 [DOI] [PubMed] [Google Scholar]
- 7.Laurence AS. Sedation, safety and MRI. Br J Radiol 2000;73:575–7 [DOI] [PubMed] [Google Scholar]
- 8.Jenkins K, Baker AB. Consent and anaesthetic risk. Anaesthesia 2003;5:962–94 [DOI] [PubMed] [Google Scholar]
- 9.Spielberger CD. State-trait anxiety inventory (Form Y). Redwood City, CA: Mind Garden, 2007 [Google Scholar]
- 10.Rushworth C. Making a difference in cancer care: practical techniques in palliative and curative treatment. London, UK: Souvenir Press, 1994 [Google Scholar]
- 11.Sharpe M. NLP in General Practice. NLP News (The Magazine of the International NLP Trainers Association Special Issue: NLP in the UK National Health Service 2005;67–6. [Google Scholar]
- 12.Bandler R, Grinder J. The structure of Magic I. Palo Alto, CA: Science and Behaviour Books Inc, 1975 [Google Scholar]
- 13.Bandler R, Grinder J. The structure of Magic II. Palo Alto, CA: Science and Behaviour Books Inc, 1975 [Google Scholar]
- 14.Grinder J, Bandler R. Tranceformations: NLP and the structure of hypnosis. Colorado, USA: Real People Press, 1981 [Google Scholar]
- 15.Bandler R, Grinder J. Frogs into princes: the introduction to NLP. Colorado, USA: Real People Press, 1979 [Google Scholar]
- 16.Bandler R. Using your brain for a change. Colorado, USA: Real People Press, 1985 [Google Scholar]
- 17.Quirk ME, Letendre AJ, Ciottone RA, Lingley JF. Evaluation of three psychologic interventions to reduce anxiety during MR imaging. Radiology 1989;173:759–62 [DOI] [PubMed] [Google Scholar]
- 18.Health andSafetyExecutive Physical Agents (Electromagnetic Fields) Directive (2008/46/EC). Available from: www.hse.gov.uk/aboutus/europe/euronews/dossiers/emf.htm [Accessed 3 June 2009] [Google Scholar]
- 19.Bangard C, Paszek J, Berg F, Eyl G, Kessler J, Lackner K, et al. MR imaging of claustrophobic patients in an open 1.0 T scanner: motion artifacts and patient acceptability compared with closed bore magnets. Eur J Radiol 2007;64:152–7 [DOI] [PubMed] [Google Scholar]