Abstract
Alimentary tract duplications are uncommon congenital anomalies containing a normal gastrointestinal mucosa and smooth muscle layer. Intestinal duplication in the jejunum is rare, and any malignancy arising in the jejunal duplication is extremely rare. In this report, we present the first case of papillary adenocarcinoma arising in a tubular duplication of the jejunum. Coronal reformatted images from contrast-enhanced CT revealed a well-enhanced tubular mass in the distal jejunum with small bowel obstruction. There were multiple enlarged lymph nodes in the small bowel mesentery around the superior mesenteric artery. The typical macroscopic and histological findings were present.
Alimentary tract duplications are uncommon congenital anomalies containing a normal gastrointestinal mucosa and smooth muscle layer that can occur anywhere throughout the digestive tract. Most patients present with pain and obstructive symptoms. Acute haemorrhage can be encountered in the case of a duplication cyst with gastric mucosa and ulceration. In addition, although rare, malignant change can occur within the intestinal duplication [1–10]. Papillary adenocarcinoma arising in an intestinal duplication is extremely rare and, to our knowledge, only two cases have been reported in the duplication cysts of the caecum and small bowel [2, 4]. In this report, we present the first case of papillary adenocarcinoma identified in a tubular duplication of jejunum on small bowel series, CT imaging and small bowel enteroscopy, with radiological–pathological correlation.
Case report
A 40-year-old man was admitted to our hospital with complaints of lower abdominal pain and vomiting for three days. On physical examination, direct tenderness was apparent in the left lower abdomen. Blood tests revealed elevated levels of C-reactive protein (17.79 mg dl−1) and serum tumour markers, such as carcinoembryonic antigen (CEA, 10.65 ng ml−1) and cancer antigen 19-9 (CA19-9, 29.44 U ml−1).
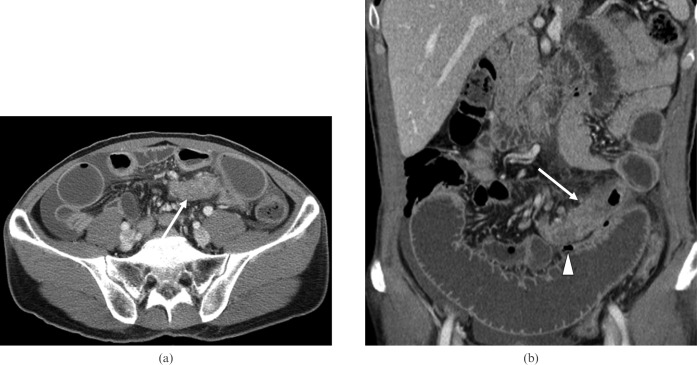
A small bowel series showed focal stricture in the distal jejunum with lobulated filling defect lesion and central barium collection (Figure 1). An axial image of contrast-enhanced CT showed an approximately 7.0 cm tubular mass in the left mid-abdomen, adjacent to the stricture site (arrow in Figure 2a). A coronal reformatted image revealed focal stricture and circumferential wall thickening of the distal jejunum and dilatation of the proximal small bowel loop (Figure 2b). A well-enhanced tubular mass was noted at the stricture site (arrow in Figure 2b), and collapsed distal small bowel was well visualised (arrowhead in Figure 2b). There were multiple enlarged lymph nodes in the small bowel mesentery around the superior mesenteric artery (SMA) root. On small bowel enteroscopy, severe stenosis was identified at the distal jejunum showing oedematous and hyperaemic mucosal irregularities (Figure 3). There was a small hole adjacent to the stricture; however, the orifice was so small that the enteroscope could not pass through it (arrow in Figure 3). Given these imaging characteristics and the high serum CEA and CA19-9, the differential diagnosis consisted of a small bowel adenocarcinoma with lymph node metastases, lymphoma or intestinal duplication with a high probability of malignancy.
Figure 1.

Small bowel series shows focal stenosis in the distal jejunum with lobulated filling defect lesion and central barium collection.
Figure 2.
Contrast-enhanced CT. (a) An axial image showed a 7.0 cm tubular mass in the left abdomen, adjacent to the stricture site (arrow). (b) A coronal reformatted image showed a focal stricture and circumferential wall thickening of the distal jejunum. A well-enhanced tubular mass was noted at the stricture site (arrow), and collapsed distal small bowel was well visualised (arrowhead).
Figure 3.

Small bowel enteroscopy reveals severe stenosis at the distal jejunum showing oedematous and hyperaemic mucosal irregularities. There is a small hole adjacent to the stricture (arrow).
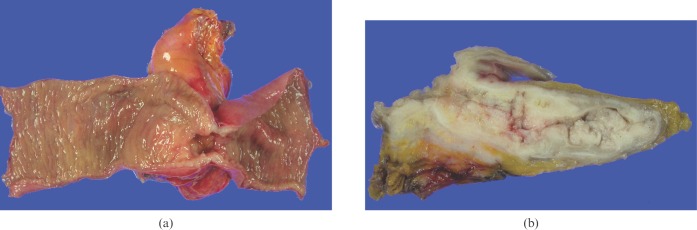
Segmental resection of small bowel was performed. The distal jejunal segment showed a 9.5 × 5.5 × 3 cm mass on the serosal side of the leaves of the mesentery (Figure 4). Histological examination revealed tubular duplication arising in the jejunum, which was composed of well-organised layers of smooth muscle typical of the gastrointestinal tract. A poorly differentiated papillary adenocarcinoma was found within the tubular duplication invading subserosa (Figure 5). There were metastases to regional lymph nodes and mesenteric lymph nodes of SMA.
Figure 4.
Macroscopic findings of the resected jejunum. (a) The tubular lesion is 9.5 × 5.5 × 3 cm in size and located in the jejunal serosal opposite the mesenterium. (b) The cut surface of the tubular lesion shows a grey friable mass with surrounding muscular wall.
Figure 5.
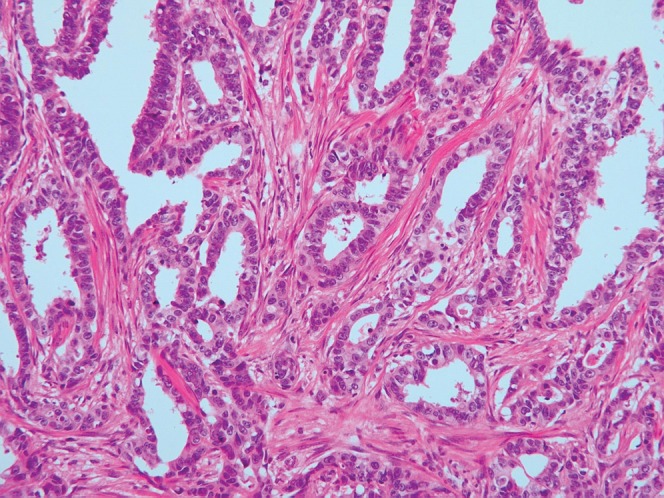
Photomicrograph (hematoxylin and eosin stain ×200) shows a poorly differentiated papillary adenocarcinoma arising in a duplication of the jejunum.
Follow-up CT eight months after surgery and chemotherapy showed a newly developed 1.0 cm mass in the rectal shelf, suggesting carcinomatosis. The patient started new chemotherapy and has been alive without disease progression.
Discussion
The aetiology of intestinal duplication remains unknown, and several theories have been proposed to explain their pathogenesis. The abnormal recanalisation after the solid epithelial stage of embryonic bowel development explains duplications in the oesophagus, small bowel and colon. The intrauterine vascular accident theory suggests that intestinal duplications arise from an intrauterine vascular accident during early foetal development [11]. The most common site is the ileum, followed by the oesophagus and duodenum [12]. Although intestinal duplication occurs most often in the ileum, it is uncommon in the jejunum. Carcinoma in a jejunal duplication is extremely rare, and only two cases have been reported [6, 8].
Various malignancies have been reported in enteric duplications, including adenocarcinoma, metastatic adenocarcinoma, carcinoid tumour and squamous cell carcinoma [1, 3, 5–10]. To our knowledge, only two cases of papillary adenocarcinomas in alimentary tract duplications have been reported, and these were found only in duplication cysts, not in tubular duplications [2, 4]. A previous study reported that 79% of alimentary tract duplications were spherical and 21% were tubular [13]. Thus, the patient presented here is extremely rare with respect to the location of duplication, showing of tubular duplication and rare histological type of papillary adenocarcinoma.
Papillary adenocarcinoma shows papillary growth of malignant epithelial cells with fibrovascular cores; it occurs commonly in the pancreas, gall bladder, ovary and thyroid gland. It is a rare histological subtype of the small bowel. Two previous studies [2, 4] reported CT and MRI findings of papillary adenocarcinoma in cystic duplications of the caecum and small bowel (Table 1); they presented as sharply marginated cystic masses with internal mural nodules. In our case, tubular duplication was perpendicular to the parent small bowel, and malignant cells filled the duplication lumen. There was no cystic portion or mucin component.
Table 1. Worldwide reported cases of papillary adenocarcinoma arising in gastrointestinal duplications.
| Author (year) | Age/sex | Symptoms and signs | Intestine | Tumour size (cm) | Duplication type |
| GA Radich et al. (2006) [4] | 39/F | Asymptomatic/pregnant | Small bowel | 14.8 × 8.5 × 8.0 | Cystic |
| J Lee et al. (2008) [2] | 40/F | Palpable mass | Caecum | 4.0 × 4.4 × 4.5 | Cystic |
| Present patient (2009) | 40/M | Pain, vomiting | Jejunum | 9.5 × 5.5 × 3 | Tubular |
The mode of metastasis in the malignancy of the duplication is similar to that of small bowel cancer, and surgical resection is required [6]. However, curative resection could not be performed in the present patient because of metastasis to the mesenteric lymph nodes of the SMA. Although our patient underwent segmental resection of the small bowel and chemotherapy following surgery, because of mesenteric lymph nodes metastases peritoneal seeding mass occurred in the rectal shelf. Thus, the prognosis is generally poor once malignancy has occurred in the intestinal duplication.
In conclusion, it is difficult to diagnose duplication of the gastrointestinal tract and cancer arising in the duplication pre-operatively. However, if a tubular structure ending as a blind pouch is located in or adjacent to the alimentary tract, one should include enteric duplication in the differential diagnosis. When an enhanced solid portion is seen within the duplication, the possibility of malignant change including papillary adenocarcinoma should be considered.
References
- 1.Hata H, Hiraoka N, Ojima H, Shimada K, Kosuge T, Shimoda T. Carcinoid tumor arising in a duplication cyst of the duodenum. Pathol Int 2006;56:272–8 [DOI] [PubMed] [Google Scholar]
- 2.Lee J, Jeon YH, Lee S. Papillary adenocarcinoma arising in a duplication of the cecum. Abdom Imaging 2008;33:601–3 [DOI] [PubMed] [Google Scholar]
- 3.Kuraoka K, Nakayama H, Kagawa T, Ichikawa T, Yasui W. Adenocarcinoma arising from a gastric duplication cyst with invasion to the stomach: a case report with literature review. J Clin Pathol 2004;57:428–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Radich GA, Altinok D, Adsay NV, Soulen RL. Papillary adenocarcinoma in a small-bowel duplication in a pregnant woman. AJR Am J Roentgenol 2006;186:895–7 [DOI] [PubMed] [Google Scholar]
- 5.de Tullio D, Rinaldi R, Pellegrini D, Stano R, Messina F, Cavazzini L, et al. Adenocarcinoma arising in an elderly patient's large ileal duplication. Int J Surg Pathol. 2008 (epub ahead of print) doi: 10.1177/1066896908319443. [DOI] [PubMed] [Google Scholar]
- 6.Kusunoki N, Shimada Y, Fukumoto S, Iwatani Y, Ohshima T, Arahi E, et al. Adenocarcinoma arising in a tubular duplication of the jejunum. J Gastroenterol 2003;38:781–5 [DOI] [PubMed] [Google Scholar]
- 7.Neal JW, Zuk RJ, Baithun SI. Squamous cell carcinoma in a duplicate large intestine. A case report. Virchows Arch A Pathol Anat Histopathol 1989;415:383–5 [DOI] [PubMed] [Google Scholar]
- 8.Fletcher DJ, Goodfellow PB, Bardsley D. Metastatic adenocarcinoma arising from a small bowel duplication cyst. Eur J Surg Oncol 2002;28:93–4 [DOI] [PubMed] [Google Scholar]
- 9.Hickey WF, Corson JM. Squamous cell carcinoma arising in a duplication of the colon: case report and literature review of squamous cell carcinoma of the colon and of malignancy complicating colonic duplication. Cancer 1981;47:602–9 [DOI] [PubMed] [Google Scholar]
- 10.Adair HM, Trowell JE. Squamous cell carcinoma arising in a duplication of the small bowel. J Pathol 1981;133:25–31 [DOI] [PubMed] [Google Scholar]
- 11.Favara BE, Franciosi RA, Akers DR. Enteric duplications. Thirty-seven cases: a vascular theory of pathogenesis. Am J Dis Child 1971;122:501–6 [PubMed] [Google Scholar]
- 12.Berrocal T, Lamas M, Gutieerrez J, Torres I, Prieto C, del Hoyo ML. Congenital anomalies of the small intestine, colon, and rectum. Radiographics 1999;19:1219–36 [DOI] [PubMed] [Google Scholar]
- 13.Karnak I, Ocal T, Senocak ME, Tanyel FC, Buyukpamukcu N. Alimentary tract duplications in children: report of 26 years' experience. Turk J Pediatr 2000;42:118–25 [PubMed] [Google Scholar]